Abstract
Objectives
The public has long been encouraged to engage in sun-safe practices to minimize exposure to sunlight, the major cause of nonmelanoma skin cancer. More recently, some have advocated unprotected sun exposure to increase cutaneous synthesis of vitamin D as a way to promote health. We assessed the net result of these conflicting messages.
Methods
In a cross-sectional survey in 2007, questionnaires were mailed to participants of an ongoing cohort study in Washington County, Maryland. The study population consisted of 8,027 adults (55% response rate).
Results
Thirty percent of respondents were aware that unprotected sun exposure increased endogenous vitamin D levels. Among those who were aware of this benefit, 42% reported going out into the sun to increase vitamin D levels. Sun-seeking to increase vitamin D production did not significantly differ according to self-reported personal history of skin cancer, but was significantly higher among women, older age groups, those with less education, and vitamin D supplement users.
Conclusion
A substantial proportion of respondents reported sun-seeking behavior expressly to increase endogenous vitamin D levels. The message about sun exposure and vitamin D is reaching the general public; however, this finding poses challenges to skin cancer prevention efforts.
Among all human malignancies, skin cancers are by far the most common1,2 and in the U.S. are among the most costly.3 With exposure to solar ultraviolet (UV) radiation as the major cause of nonmelanoma skin cancer,2 prevention strategies have emphasized sun avoidance and skin-protection behaviors such as use of sunscreen and skin-protective clothing. Longstanding public education campaigns have sought to reduce sunlight exposure with the goal of reducing skin cancer incidence rates.4,5
In addition to being the primary cause of human skin cancer, solar UV radiation is also responsible for stimulating cutaneous vitamin D synthesis. In turn, vitamin D is critical for calcium homeostasis and skeletal maintenance.6 The observation that hypovitaminosis D was common in general medical inpatients, even in those with vitamin D intakes exceeding the recommended daily allowance and those without apparent risk factors for vitamin D deficiency, led to the hypothesis that the general population may have suboptimal levels of vitamin D.6,7 As understanding of this topic progressed, it gradually gave rise to the observation that sun avoidance, with the goal of preventing skin cancer, may compromise vitamin D sufficiency.7 For bone health, consensus has been achieved concerning the definition of vitamin D deficiency (<25 nanograms per milliliter [ng/ml] 25-hydroxyvitamin D [25(OH)D]). For overall health, however, the general definition of vitamin D insufficiency varies.6,7
Both interest and concern regarding vitamin D has increased as evidence has accumulated that its potential health benefits may extend beyond skeletal health. The public's concerns about vitamin D insufficiency have been raised as studies reporting health benefits have received media coverage, touting the health benefits of the “sunshine vitamin.”4,8,9 Based on the premise that vitamin D is important to overall health and well-being, some reports have extolled the benefits of regular sun exposure6,10 and even tanning bed use.10 For example, vitamin D deficiency and decreased exposure to sunlight have been hypothesized to increase the risks of many common cancers, type 1 diabetes, rheumatoid arthritis, and multiple sclerosis.6,10 Based on these potentially wide-ranging health benefits of vitamin D, some have suggested that the benefits of sun exposure to increase cutaneous vitamin D synthesis may outweigh the risks (e.g., skin cancer) associated with unprotected exposure to solar UV radiation.6,10
The importance of understanding the public's perceptions of these issues is accentuated by the fact that the actual relationship between sun exposure and cutaneous vitamin D synthesis and metabolism is complex and incompletely understood even by the scientific community. In a study of highly sun-exposed (average weekly sun exposure of 29 hours) young adults in Hawaii, approximately one-half had 25(OH)D concentrations <30 ng/ml, and 9% had concentrations <20 ng/ml.11 Under tightly controlled experimental conditions among adults in the United Kingdom, UV radiation exposure of approximately 35% of the total skin surface area at doses similar to summer sunlight three days a week for 13 minutes per day resulted in 25(OH)D concentrations of ≥20 ng/ml (“sufficient”) in 10% and concentrations of ≥32 ng/ml (“optimal”) in 74% of the adults.12 Thus, in addition to factors affecting UV radiation dose, such as season of year, time of day, latitude, altitude, and atmospheric conditions,13,14 results such as these suggest there is considerable inter-individual variability in cutaneous vitamin D synthesis in response to sunlight. The determinants of these inter-individual differences in vitamin D synthesis and metabolism are undoubtedly complex and multifactorial, but contributors appear to be factors such as age, race, vitamin D supplement use, calcium intake, body mass index (BMI), skin type, and genetic characteristics.7,8,13,15 Advances are being made in understanding how genetic variants contribute to inter-individual differences in vitamin D status; for example, the results of a recent genome-wide association study revealed variants at three loci that were associated with a significantly higher likelihood of vitamin D insufficiency.16
Further complicating matters, some researchers currently recommend lower-level sun exposure of approximately 15 minutes per day with face and hands exposed,13,17 but the evidence described previously adds uncertainty with respect to the extent to which this level of sun exposure results in the desired increase in circulating vitamin D concentrations. Furthermore, application of this recommendation is controversial given that solar UV radiation is the major cause of skin cancer.2 Additionally, even those who engage in sun-protective behaviors (e.g., sunscreen use) may not apply the sunscreen in a manner that would prevent vitamin D synthesis to the degree theoretically possible on the basis of the sun protection factor.14,15,18
The small but growing body of evidence on this topic indicates that lack of attention to this issue may lead to further escalation in the incidence of skin cancer. Few studies have examined the impact on the general population of the mixed medical and media messages that range from sun avoidance for skin cancer prevention to the sun-seeking, pro-vitamin D message. We addressed this evidence gap by describing the prevalence of (1) awareness of unprotected sun exposure to increase vitamin D and (2) the extent to which concerns about vitamin D may be influencing sun exposure behaviors.
METHODS
We conducted a cross-sectional survey as part of the longitudinal follow-up of the CLUE II (Give Us a Clue to Cancer and Heart Disease) prospective cohort study. The CLUE II cohort was established with baseline data collection that took place from May through October 1989 in Washington County, Maryland.19 Washington County is a semirural community located in western Maryland. The baseline data collection was designed to collect blood samples from as many adult residents as possible in the Washington County and surrounding (30-mile radius) area to provide specimens for a serum bank. Mobile trailers operated in all areas of the county and at all times of day except between 1 a.m. and 6 a.m. Brief medical histories were taken and blood was drawn in a baseline cohort comprising 32,894 participants. Based on 1990 U.S. Census figures, approximately 30% of adult Washington County residents participated. Overall, participation was highest in the 45- to 65-year age group and was slightly higher among females, more educated people, and nonsmokers. The CLUE II cohort has been a fertile resource for epidemiologic studies across a wide range of research questions.
The cohort has been periodically followed up with self-administered, mailed questionnaires. Relevant to this study was the most recent follow-up, which took place in 2007 and contained the questionnaire items upon which this study was based. For the 2007 survey, a self-administered follow-up questionnaire was mailed to CLUE II cohort members who had completed and returned at least one previous follow-up questionnaire (target n=14,822). Of these, 8,183 responded for a response rate of 55%. The specific questionnaire items most relevant to our study were those added to determine the extent to which respondents were aware of the message that going out into the sun increases endogenous vitamin D levels (“Have you heard about going out into the sun without sunscreen or skin-protective clothing so that your body would make more vitamin D?”) and acted upon this advice by going out into the sun to increase vitamin D production (“Do you ever go out into the sun so that your body will make more vitamin D?”). A total of 8,027 respondents provided valid responses to both of these items and comprised the study population for our study. All data collection activities took place with the approval of the Institutional Review Boards of the Medical University of South Carolina and Johns Hopkins University.
For these two questions, we assessed the overall prevalence of awareness as well as awareness according to sociodemographic characteristics and BMI, lifestyle characteristics (e.g., cigarette smoking and vitamin D supplement use), skin cancer risk factors (e.g., complexion, skin type, and history of sunburns), and self-reported history of skin cancer. We did not include race/ethnicity in the analyses because the predominantly (99%) Caucasian population left too little diversity to provide reasonable inferences for racial/ethnic groups other than Caucasians.
Statistical analyses
We compared respondents who reported awareness of unprotected sun exposure to increase endogenous vitamin D production with those who were not aware of this assertion. Among those who were aware, we compared those who reported going out into the sun to increase vitamin D levels with those who reported never going out into the sun to increase vitamin D levels. We used Chi-square tests to determine associations between participant characteristics. We considered p≤0.05 statistically significant.
RESULTS
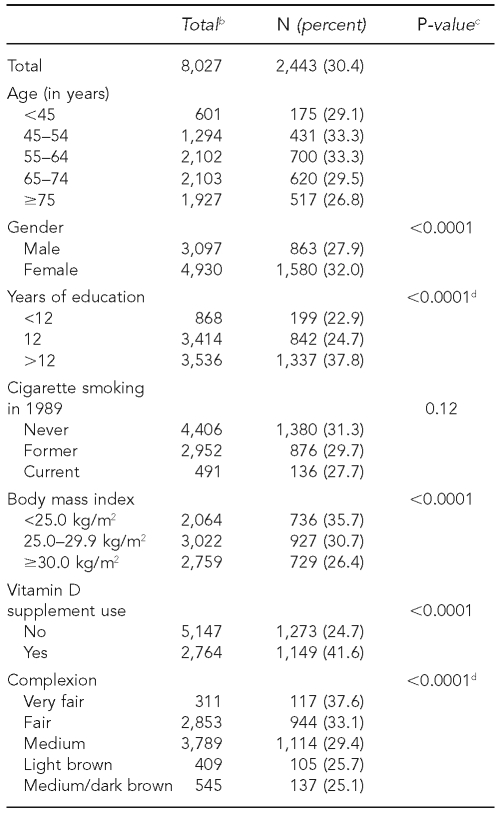
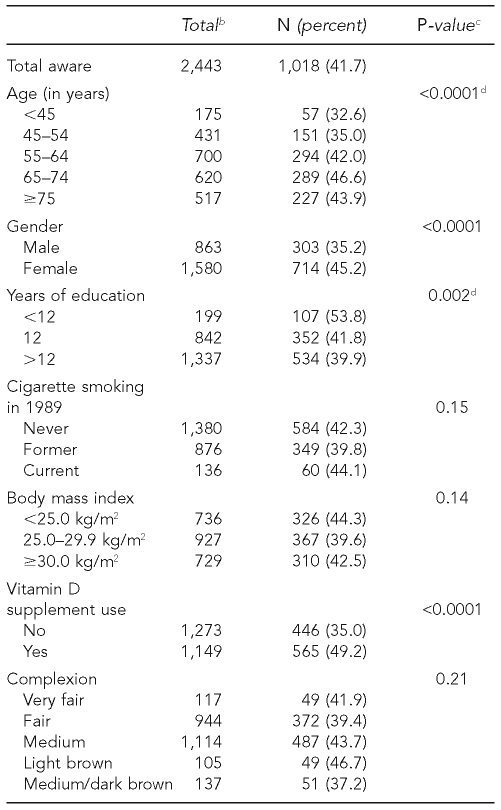
Thirty percent (95% confidence interval [CI] 29, 31) of respondents were aware that unprotected sun exposure increased endogenous vitamin D levels (Table 1). Several demographic characteristics and skin cancer risk factors were associated with awareness. The prevalence of awareness was higher among those aged 45–64 years (33%) than among those who were either older or younger (<30%). Awareness was significantly higher in women than men (32% vs. 28%, p<0.0001), and prevalence of awareness increased with higher education, from 23% to 25% to 38% among those with <12, 12, and >12 years of education, respectively (p<0.0001). Awareness was higher in those with a BMI of <25.0 kilograms per meter squared (kg/m2) (36%) compared with those with a BMI of 25.0–29.9 kg/m2 (31%) or ≥30 kg/m2 (26%) (p<0.0001). Compared with nonusers, vitamin D supplement users were substantially more likely to be aware that unprotected sun exposure increased endogenous vitamin D levels (42% vs. 25%, p<0.0001).
Table 1.
Prevalence of awareness of sun exposure without sunscreen or skin-protective clothinga to increase vitamin D levels: CLUE II Study, Washington County, Maryland, 2007
aPrevalence of “yes” responses to the question, “Have you heard about going out into the sun without sunscreen or skin-protective clothing so that your body would make more vitamin D?”
bDue to missing data, the totals for some variables do not add up to 8,027.
cChi-square test
dp-value for trend
eNonmelanoma or melanoma skin cancer
kg/m2 = kilograms per meter squared
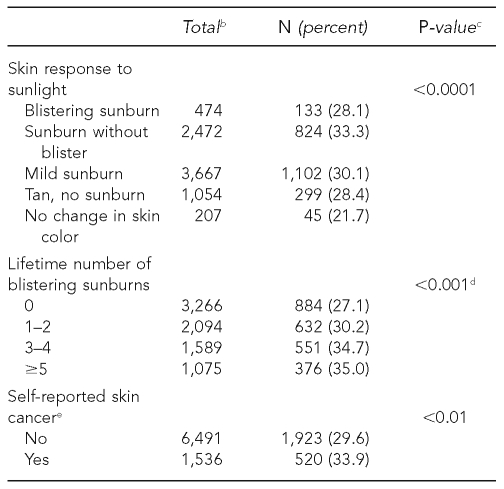
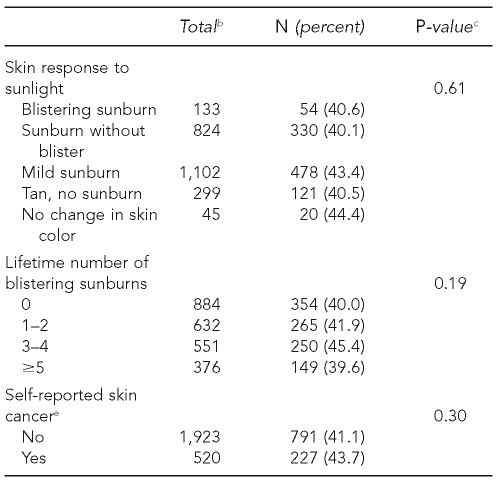
With respect to skin cancer risk factors, there was a marked gradient in awareness of unprotected sun exposure to increase vitamin D levels between those with very fair complexion compared with those who had a medium/dark brown complexion (38% vs. 25%, p<0.0001). No consistent trend was seen for the skin phenotypic characteristic of sensitivity to sunburn, but there was a statistically significant trend in increased awareness according to lifetime number of blistering sunburns (p<0.001). Consistent with the results for skin cancer risk factors, the prevalence of awareness was significantly higher among those with a self-reported history of skin cancer compared with those with no previous skin cancer (34% vs. 30%, p<0.01) (Table 2).
Table 2.
Among those aware of unprotected sun exposure to increase cutaneous vitamin D synthesisa (n=2,443), the prevalence of seeking sun exposure to increase vitamin D levels: CLUE II Study, Washington County, Maryland, 2007
aAmong those who were aware that sun exposure increased vitamin D, prevalence of “yes” responses to the question, “Do you ever go out into the sun so that your body will make more vitamin D?”
bDue to missing data, the totals for some variables do not add up to 2,443.
cChi-square test
dp-value for trend
eNonmelanoma or melanoma skin cancer
kg/m2 = kilograms per meter squared
Among the respondents who were aware that unprotected sun exposure increased endogenous vitamin D levels, 1,018 (42%) reported going out into the sun to increase vitamin D production (Table 2). Among this group, several factors were significantly associated with sun-seeking behavior for vitamin D. There was a significant trend of increased sun-seeking behavior with older age (p<0.0001). Women were significantly more likely than men to engage in sun-seeking for vitamin D (45% vs. 35%, p<0.0001). The association between education and sun-seeking behavior ran counter to the association observed with awareness, with a statistically significant inverse trend of decreased sun-seeking behavior with more education (p=0.002). Vitamin D supplement users were significantly more likely than nonusers to report going out in the sun for vitamin D (49% vs. 35%, p<0.0001). Sun-seeking behavior for vitamin D did not differ significantly according to skin phenotypic characteristics or self-reported history of skin cancer.
DISCUSSION
This study provides information about the extent to which the debate within the biomedical community surrounding vitamin D has permeated to the general public. The study findings indicate that a substantial proportion, almost one-third of the study population, was aware of the idea of engaging in sun-seeking behavior to enhance cutaneous vitamin D synthesis. Furthermore, approximately 40% of those who were aware of this issue actually engaged in sun-seeking behavior to stimulate cutaneous vitamin D production.
Awareness of sun exposure to increase vitamin D levels was greater among those who had a personal history of skin cancer or who had a high risk of skin cancer by virtue of complexion and more extensive sun exposure/sunburn history. It is not surprising that those who may have heightened concern about their skin's susceptibility to the sun were also most aware of engaging in sun exposure to increase vitamin D levels. However, it was disconcerting that among those who were aware, those at greatest risk of skin cancer due to fair complexion, susceptibility to sunburn, sunburn history, and preexisting personal history of skin cancer were no less likely than others to engage in sun-seeking behaviors for vitamin D. This finding is of acute concern because the skin cancer risks associated with unprotected sun exposure are largely concentrated within this group. The reasons why those with high-risk skin cancer phenotypes due to factors such as fair complexion, susceptibility to sunburn, sunburn history, or a preexisting personal history of skin cancer would have similar likelihood of sun-seeking for vitamin D as those without these characteristics is not known, but could potentially be due to incongruence between an individual's perceived and actual skin cancer risk, or possibly the perception that the health benefits of vitamin D outweigh the risks associated with skin cancer.
This interpretation of the prevalence estimates is corroborated by the few previous studies to address this topic. In a 2004 survey in Queensland, Australia, 15% of respondents agreed that sun protection may result in insufficient vitamin D, and another 39% were uncertain.21 In a 2006 survey by this same research group, 21% of adults had reduced their sun-protective behaviors due to concern about vitamin D levels, and 16% had future intentions to do so.8 Revealing an increasing trend over time, 32% felt that regularly protecting skin from the sun raised dangers about insufficient vitamin D levels.8 In a survey of Chinese women >50 years of age in Hong Kong, 53% responded yes to the question, “Do you know that sun exposure can give you vitamin D?”22 In a different, open-ended question about sources of vitamin D, however, only 23% of respondents listed sunlight as a source of vitamin D.22 Taken together with our findings, the evidence to date indicates that prevalence estimates vary, but substantial proportions of the populations investigated have consistently reported awareness that sun exposure increases vitamin D levels. Evidence from our study in the U.S. suggests that this awareness was associated with sun-seeking expressly for the purpose of increasing vitamin D levels.
Limitations
This study had several limitations. One limitation was the lack of detailed questionnaire items to better characterize the extent of the study respondents' specific sun-seeking behaviors and their specific understanding of the important underlying issues concerning vitamin D. Greater insights will be gained from future studies that more thoroughly characterize the extent of the sun-seeking behavior to increase cutaneous vitamin D synthesis, including the frequency and duration of intentional sun exposure and the proportion of the skin surface area exposed to the sun. Further, the study inferences would be strengthened if more were known about respondents' understanding of vitamin D photosynthesis. For example, it would enrich our understanding of this question if more was known about perceptions of the duration/time of day and body coverage of sun exposure required to achieve optimal vitamin D levels, or the impact of sunscreens on vitamin D photosynthesis. For example, a study in Australia8 revealed that respondents often believed extended sun exposure was necessary to achieve the benefits of vitamin D. Future research that includes more detailed questions will allow these issues to be explored in greater depth, and may help shed light on the underlying explanations for the associations observed in our study. This will, in turn, provide a refined characterization of how formidable a challenge to skin cancer prevention efforts this issue presently poses.
A limitation to the generalizability of the study findings is that the study population was not randomly sampled, but, rather, was a select group of participants in a long-term prospective cohort study. Washington County is a community in western Maryland. To the extent that those who reside in more urban areas may have greater awareness of vitamin D, the prevalence estimates in our study may actually represent underestimates. On the other hand, our response rate was 55%. Compared with nonparticipants in the 2007 survey that formed the basis of this investigation, those who participated may be more health conscious and, therefore, have greater awareness that sun exposure increases endogenous vitamin D levels. To the extent that this is true, our results may represent overestimates of the prevalence of awareness of vitamin D and sun-seeking behavior to raise vitamin D levels.
Our prevalence estimate was unlikely to be prone to extreme error, making it safe to infer that the penetration of the messages about vitamin D to the general public has been substantial. The lack of racial/ethnic diversity in our predominantly (99%) Caucasian study population was another limitation. It will be important to characterize these questions in more diverse samples in future studies; for example, African Americans have lower circulating vitamin D concentrations than Caucasians and may have different perceptions and knowledge about vitamin D and sun-seeking behavior for vitamin D.
CONCLUSIONS
The heightened awareness of vitamin D in the general population and apparent population interest in this topic accentuate the need to work to resolve controversies in the field. There are several important and challenging issues in this regard. One issue is whether to advise sun avoidance/sun-protective behaviors and complete reliance on vitamin D supplements to maintain optimal vitamin D levels. Considering that UV radiation is a skin carcinogen and associated with photoaging,8,13 sun avoidance and vitamin D supplementation are clearly the most prudent strategies for individuals with sun-sensitive phenotypes.7 Thus, if a universal recommendation was not a viable public health option, tailored messaging that accounts for age and complexion would be indicated.
Another controversial topic is what constitutes optimal target levels of the primary serum biomarker of vitamin D, 25(OH)D.7,13 While consensus has been achieved regarding the vitamin D level needed for bone health, there is still controversy over what constitutes optimal target vitamin D levels for overall health.7,13,17,20 Further, it will be important to have an evidence-based framework when assessing and communicating what the potential health benefits of vitamin D may be—that is, for a particular health outcome—the extent to which the existing evidence is convincing, merely suggestive, or offers no evidence of benefit.
Importantly, this framework for assessing the evidence would be further complicated by accounting for the issue of health benefits for given target vitamin D levels. This framework makes accurately characterizing the dose-response relationship between vitamin D and a putative health outcome a key consideration. These issues have been addressed with respect to bone health, but many of the additional hypothesized health benefits of vitamin D remain to be proven to the extent that they reach the threshold of evidence-based recommendations.7,13 A desired end-product of this research would be to generate the evidence base to developing a cohesive message with consensus from the various medical and public health constituencies.23 Future patient-focused skin cancer prevention interventions would likely benefit from directly addressing population interest in this topic by explaining the balance between the risks and benefits of sun exposure and promoting proper dietary vitamin D supplementation as a sensible approach.
REFERENCES
- 1.Rogers HW, Weinstock MA, Harris AR, Hinckley MR, Feldman SR, Fleischer AB, et al. Incidence estimate of nonmelanoma skin cancer in the United States, 2006. Arch Dermatol. 2010;146:283–7. doi: 10.1001/archdermatol.2010.19. [DOI] [PubMed] [Google Scholar]
- 2.Karagas MR, Weinstock MA, Nelson HH. Keratinocyte carcinomas (basal and squamous cell carcinomas of the skin). Chapter 64. In: Schottenfeld D, Fraumeni JF Jr, editors. Cancer epidemiology and prevention. 3rd ed. New York: Oxford University Press; 2006. pp. p. 1230–50. [Google Scholar]
- 3.Housman TS, Feldman SR, Williford PM, Flesicher AB, Jr, Goldman ND, Acostamadiedo JM, et al. Skin cancer is among the most costly of all cancers to treat for the Medicare population. J Am Acad Dermatol. 2003;48:425–9. doi: 10.1067/mjd.2003.186. [DOI] [PubMed] [Google Scholar]
- 4.Hiom S. Public awareness regarding UV risks and vitamin D—the challenges for UK skin cancer prevention campaigns. Prog Biophys Mol Biol. 2006;92:161–6. doi: 10.1016/j.pbiomolbio.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 5.Sinclair C, Foley P. Skin cancer prevention in Australia. Br J Dermatol. 2009;161(Suppl 3):116–23. doi: 10.1111/j.1365-2133.2009.09459.x. [DOI] [PubMed] [Google Scholar]
- 6.Holick MF. Sunlight, UV-radiation, vitamin D and skin cancer: how much sunlight do we need? Adv Exp Med Biol. 2008;624:1–15. doi: 10.1007/978-0-387-77574-6_1. [DOI] [PubMed] [Google Scholar]
- 7.Gilchrest BA. Sun exposure and vitamin D sufficiency. Am J Clin Nutr. 2008;88:570S–7S. doi: 10.1093/ajcn/88.2.570S. [DOI] [PubMed] [Google Scholar]
- 8.Youl PH, Janda M, Kimlin M. Vitamin D and sun protection: the impact of mixed public health messages in Australia. Int J Cancer. 2009;124:1963–70. doi: 10.1002/ijc.24154. [DOI] [PubMed] [Google Scholar]
- 9.Scully M, Wakefield M, Dixon H. Trends in news coverage about skin cancer prevention, 1993–2006: increasingly mixed messages for the public. Aust N Z J Public Health. 2008;32:461–6. doi: 10.1111/j.1753-6405.2008.00280.x. [DOI] [PubMed] [Google Scholar]
- 10.Grant WB, Cross HS, Garland CF, Gorham ED, Moan J, Peterlik M, et al. Estimated benefit of increased vitamin D status in reducing economic burden of disease in Western Europe. Prog Biophys Mol Biol. 2009;99:104–13. doi: 10.1016/j.pbiomolbio.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 11.Binkley N, Novotny R, Krueger D, Kawahara T, Daida YG, Lensmeyer G, et al. Low vitamin D status despite abundant sun exposure. J Clin Endocrinol Metab. 2007;92:2130–5. doi: 10.1210/jc.2006-2250. [DOI] [PubMed] [Google Scholar]
- 12.Rhodes LE, Webb AR, Fraser HI, Kift R, Durkin MT, Allan D, et al. Recommended summer sunlight exposure levels can produce sufficient (≥20 ng/ml(–1)) but not proposed optimal (≥32 ng/ml(21)) 25(OH)D levels at UK latitudes. J Invest Dermatol. 2010;130:1411–8. doi: 10.1038/jid.2009.417. [DOI] [PubMed] [Google Scholar]
- 13.Borradale D, Kimlin M. Vitamin D in health and disease: an insight into traditional functions and new roles for the “sunshine vitamin”. Nutr Res Rev. 2009;22:118–36. doi: 10.1017/S0954422409990102. [DOI] [PubMed] [Google Scholar]
- 14.Diehl JW, Chiu MW. Effects of ambient sunlight and photoprotection on vitamin D status. Dermatol Ther. 2010;23:48–60. doi: 10.1111/j.1529-8019.2009.01290.x. [DOI] [PubMed] [Google Scholar]
- 15.Stechschulte SA, Kirsner RS, Federman DG. Vitamin D: bone and beyond, rationale and recommendations for supplementation. Am J Med. 2009;122:793–802. doi: 10.1016/j.amjmed.2009.02.029. [DOI] [PubMed] [Google Scholar]
- 16.Wang TJ, Zhang F, Richards JB, Kestenbaum B, van Meurs JB, Berry D, et al. Common genetic determinants of vitamin D insufficiency: a genome-wide association study. Lancet. 2010;376:180–8. doi: 10.1016/S0140-6736(10)60588-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reichrath J. Skin cancer prevention and UV-protection: how to avoid vitamin D-deficiency? Br J Dermatol. 2009;161(Suppl 3):54–60. doi: 10.1111/j.1365-2133.2009.09450.x. [DOI] [PubMed] [Google Scholar]
- 18.Norval M, Wulf HC. Does chronic sunscreen use reduce vitamin D production to insufficient levels? Br J Dermatol. 2009;161:732–6. doi: 10.1111/j.1365-2133.2009.09332.x. [DOI] [PubMed] [Google Scholar]
- 19.Comstock GW, Alberg AJ, Huang HY, Wu K, Burke A, Hoffman SC, et al. The risk of developing lung cancer associated with antioxidants in the blood: ascorbic acid, carotenoids, alpha-tocopherol, selenium, and total peroxyl radical absorbing capacity. Cancer Epidemiol Biomarkers Prev. 1997;6:907–16. [PubMed] [Google Scholar]
- 20.Hollis BW, Wagner CL, Drezner MK, Binkley NC. Circulating vitamin D3 and 25-hydroxyvitamin D in humans: an important tool to define adequate nutritional vitamin D status. J Steroid Biochem Mol Biol. 2007;103:631–4. doi: 10.1016/j.jsbmb.2006.12.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Janda M, Kimlin M, Whiteman D, Aitken J, Neale R. Sun protection and low levels of vitamin D: are people concerned? Cancer Causes Control. 2007;18:1015–9. doi: 10.1007/s10552-007-9042-4. [DOI] [PubMed] [Google Scholar]
- 22.Kung AW, Lee KK. Knowledge of vitamin D and perceptions and attitudes toward sunlight among Chinese middle-aged and elderly women: a population survey in Hong Kong. BMC Public Health. 2006;6:226. doi: 10.1186/1471-2458-6-226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Martin JM, Ghaferi JM, Cummins DL, Mamelak AJ, Schmults CD, Parikh M, et al. Changes in skin tanning attitudes: fashion articles and advertisements in the early 20th century. Am J Public Health. 2009;99:2140–6. doi: 10.2105/AJPH.2008.144352. [DOI] [PMC free article] [PubMed] [Google Scholar]