As a smoking cessation strategy, a quitline service has been known to be effective in helping smokers in several countries (e.g., Australia, Sweden, United States, New Zealand, United Kingdom, and Hong Kong) quit smoking.1–6 It can provide convenient smoking cessation services to smokers who need help and are reluctant to undergo face-to-face counseling, is effective with diverse populations, and has a broad reach.3,7 Also, a randomized controlled trial showed that telephone counseling as an adjunct to nicotine replacement therapy by transdermal patch significantly increased 90-day continuous abstinence rates at six months compared with pharmacological treatment alone.8
In general, a quitline service uses two approaches. In a proactive approach, a trained counselor telephones the smoker to provide support in initiating a quit attempt and maintaining prolonged abstinence. In a reactive approach, users obtain information or assistance by telephoning the quitline.9,10 A meta-analysis of telephone counseling for smoking cessation reported that three or more calls of intensive, proactive telephone counseling increased the odds of quitting, compared with minimal intervention such as brief advice or the provision of self-help materials.9
A quitline service could be especially effective for helping smokers in Korea quit smoking. Korea is a country with a very high smoking prevalence among men—one of the highest worldwide—with 46.6% of Korean men compared with 4.6% of Korean women smoking in 2005.11 The total population of smokers in Korea is estimated to be about 10 million. No quitline service or research was implemented in Korea until 2005. A preliminary proactive quitline service was offered by the National Cancer Center (NCC) and the Korean Ministry of Health and Welfare (KMHW) from November 1, 2005, to January 31, 2006, from which the 30-day continuous abstinence rate of the participants was reportedly 38.3% based on an intention-to-treat analysis.12
We examined the continuous abstinence rates of smoking at each follow-up of the proactive quitline service and explored the factors of successful smoking cessation, using data from the proactive quitline service implemented by the NCC and the KMHW.
METHODS
Overview of the Korean proactive quitline service
Before implementation of the Korean proactive quitline service, the NCC had operated a preliminary proactive quitline service granted by the KMHW for three months, from November 2005 to January 2006. The NCC reported the effects of a 30-day smoking cessation period for 649 smoking subjects. Based on the effects of the preliminary service, the NCC and the KMHW have been operating the Korean proactive quitline service nationwide since April 17, 2006. We used a single, representative nationwide telephone number, 1544-9030. (The Korean pronunciation of “9030” is similar to that for the Korean term for “success in smoking cessation;” thus, it was easy to memorize.) After a user called at his/her own charge and enrolled in the quitline service, a trained counselor for smoking cessation called him/her back and provided up to 14 consecutive counseling calls for 12 months, free of charge. In addition to telephone counseling, more information services were provided for those hoping to quit smoking, through an interactive voice response (IVR) system and the Korean quitline website (http://www.quitline.hp.go.kr). Counseling services were available from 8 a.m. to 10 p.m. on weekdays and from 8 a.m. to noon on Saturdays by 30 trained counselors on a two-shift basis. If the users failed to quit smoking, they were allowed to repeat the program, without limitations.
Participants
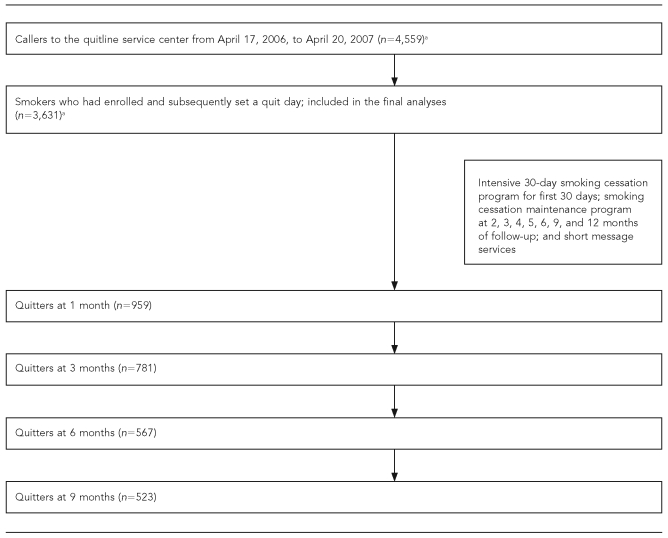
The Korean quitline service was advertised and promoted nationwide via a media release, television and radio commercials, messages in subway stations, 248 community health centers, 135 family medicine clinics at the university hospital, and smoking cessation-related organizations and their websites. As shown in Figure 1, 4,559 people called the quitline service center from April 17, 2006, to April 20, 2007. Of those callers, we included in the final analyses 3,631 participants who had enrolled and subsequently set a quit day.
Figure 1.
Overview of a study of the Korean quitline service data: South Korea, 2006–2007
aAmong the 4,559 callers, those who did not set a quit day were excluded in the final analyses.
The first call
At the participants' first enrollment, counselors collected the following baseline data: sociodemographic characteristics (gender, age, occupational status, education level, type of medical security, and frequency of alcohol use per week) and smoking-related characteristics (number of cigarettes per day, age at smoking initiation, smoking duration, previous quit attempts, and Fagerstrom Test for Nicotine Dependence [FTND] score). The Korean version of the FTND questionnaire, which had been previously validated, was used during the first call counseling.13 Also, counselors set a quit date with each participant, explained counseling plans, and boosted self-efficacy. The duration of this first interview was about 25 minutes (range: 15–40 minutes).
Smoking cessation programs
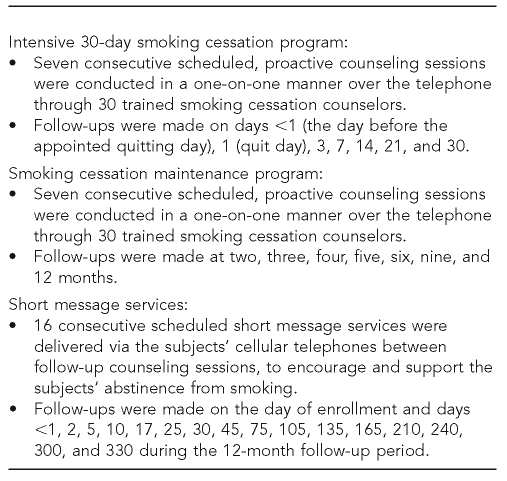
As shown in Figure 2, we introduced a unique, intensive, and proactive smoking cessation program for the quitline service, comprising an intensive 30-day smoking cessation program and a smoking cessation maintenance program, with scheduled short-message services (SMSs) being sent to a subject's cellular phone between follow-up counseling sessions, to remind and encourage the subject to quit smoking.
Figure 2.
Smoking cessation programs provided to participants in the Korean quitline service: South Korea, 2006–2007
The intensive 30-day smoking cessation program consisted of seven consecutive scheduled counseling sessions conducted on day <1 (the day before the appointed quit day), day 1 (the quit day), day 3, day 7, day 14, day 21, and day 30. When a scheduled day for this counseling session was a holiday, a subject received counseling before or after the scheduled day. The subjects who successfully completed the intensive 30-day smoking cessation program were provided with a smoking cessation maintenance program, comprising another seven consecutive scheduled counseling sessions conducted at two, three, four, five, six, nine, and 12 months of follow-up. These counseling sessions covered the following to prevent relapse: assessing the participant's progress, examining relapse situations, discussing coping strategies, and encouraging and supporting the participant's quit behavior. The duration of each follow-up call was about 5 minutes (range: 2–10 minutes).
All the counseling days were appointed at the subjects' convenience, and all the counseling sessions were conducted in a one-on-one manner over the telephone through 30 trained smoking cessation counselors. The counselors were students and -graduates who had completed a special 44-hour training program for smoking cessation counseling at the quitline service center, after having studied psychology, clinical psychology, the science of public health, or the science of nursing at the university level.
In addition to these programs, we also used scheduled SMSs delivered via the subjects' cellular phones between follow-up counseling sessions to encourage and support the subjects' abstinence from smoking. These SMSs consisted of a total of 17 consecutive scheduled messages delivered on the day of enrollment and days <1, 2, 5, 10, 17, 25, 30, 45, 75, 105, 135, 165, 210, 240, 300, and 330 during the 12-month follow-up period.Messages included: “Congratulations on your resolution to quit smoking'” on day <1; “Can you feel the changes in your body after quitting? It's now beginning'” on day 2; “Congratulations on your successful 30-day abstinence'” on day 30; and “It's a month until your successful one-year abstinence' Stay cheerful until your success'” on day 330.
Outcome measures
Counselors collected all the participants' quit status information at each of the follow-up counseling sessions. The main outcome measure was self-reported continuous abstinence rate at each of the follow-up sessions, which was defined as the percentage of participants who reported not having smoked even one cigarette since the preceding counseling session among all the participants who had set a quit day, based on an intention-to-treat analysis. Because only those who had been abstinent received the next counseling session in this quitline service, “continuous abstinence at each of the follow-ups” implied “continuous abstinence since a quit day at each of the follow-ups.” Also, participants could be classified as an “abstinence failure,” which included both “failure to maintain abstinence” (smoking even one cigarette since day 1, or refusing to participate further in the program) and “loss to follow-up” (no response to three telephone calls, refusal to participate in the program on day <1, or inability to participate in the program, due to certain diseases or death). In addition, we calculated the self-reported continuous abstinence rate at each of the follow-up sessions, according to additional number of quit attempts (i.e., abstinence rate on the second, third, fourth, and fifth quit attempts).
Statistical analyses
We estimated the self-reported continuous abstinence rate at each follow-up session based on an intention-to-treat analysis. Among the callers, those who did not set a quit day were excluded in the final analyses. All the participants who had set a quit day were included in the denominator, and those who reported not having smoked even one cigarette since the preceding follow-up were included in the numerator; those lost to follow-up were considered to be abstinence failures.
We used Pearson's Chi-square test and p-values for trend to identify the factors of successful abstinence in a univariable analysis. We performed multiple logistic regression analyses to assess the factors for abstinence with adjustments for main independent variables using odds ratios (ORs) with 95% confidence intervals (CIs). Among the independent variables, those variables that showed p<0.3 in univariable analyses were included in the multiple logistic regression analyses. Also, considering the multicollinearity between age and age at smoking initiation, only the variable of age showing a stronger association with smoking cessation was included in the final model.
All the statistical tests were two-sided, and we considered values of p≤0.05 to be statistically significant. We conducted data analyses using SPSS® version 12.0.14
RESULTS
Baseline characteristics of the participants
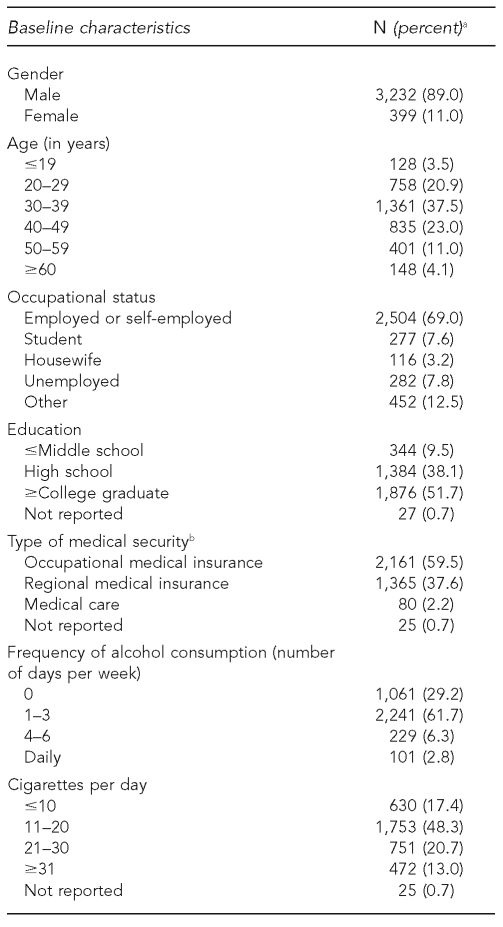
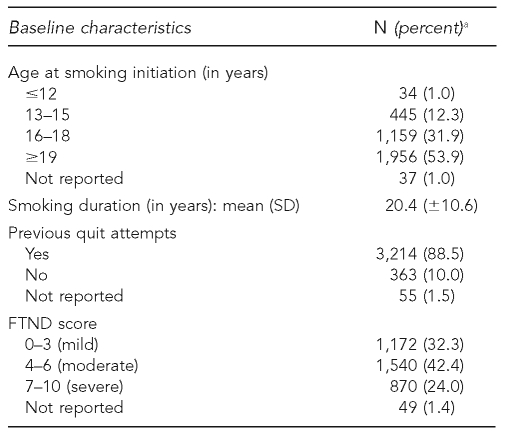
As shown in Table 1, of the 3,631 participants who had set a quit day and whose quit day had elapsed in the previous 12 months, 89.0% (n=3,232) were male, 37.5% (n=1,361) were aged 30–39 years, and 69.0% (n=2,504) were employed or self-employed. Also, 51.7% (n=1,876) had at least a college degree, 59.5% (n=2,161) held occupational medical insurance, and 61.7% (n=2,241) reported drinking alcohol one to three days per week. Regarding smoking behavior, 48.3% (n=1,753) smoked 11–20 cigarettes per day, 53.9% (n=1,956) had started smoking at ≥19 years of age, 88.5% (n=3,214) had previously attempted to quit smoking, and 42.4% (n=1,540) had an FTND score of 4–6. The mean smoking duration was 20.4 ± 10.6 years.
Table 1.
Baseline sociodemographic and smoking-related characteristics of participants in the Korean quitline service who had set a quit day and whose quit day had elapsed in the previous 12 months (n=3,631): South Korea, 2006–2007
aBecause of rounding, not all percentages add up to 100.
bThe medical security system in Korea, which is compulsory, comprises two major programs: medical insurance and medical care. Medical insurance is divided into occupational medical insurance for the employed, and regional medical insurance for the unemployed or the self-employed. Medical care is sponsored by the Korean government for low-income people.
SD = standard deviation
FTND = Fagerstrom Test for Nicotine Dependence
Self-reported continuous abstinence rates
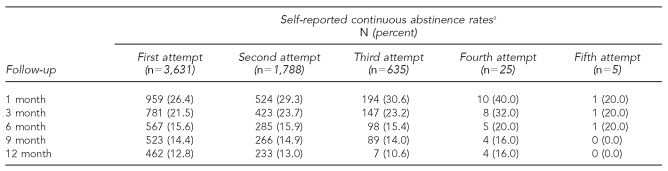
Table 2 shows the self-reported continuous abstinence rates. Among the 3,631 participants, the self-reported continuous abstinence rates were 26.4%, 21.5%, 15.6%, 14.4%, and 12.8% at one, three, six, nine, and 12 months, respectively. The abstinence rates of the subjects who attempted to quit a second time ranged from 29.3% at one month to 13.0% at 12 months.
Table 2.
Self-reported continuous abstinence rates by number of smoking quit attempts among participants in the Korean quitline service (n=3,631): South Korea, 2006–2007
aSelf-reported continuous abstinence rate is defined as the percentage of participants who have not smoked even one cigarette since their quit day at each of the follow-up counseling sessions among all the participants who set a quit day, based on an intention-to-treat analysis.
Differences in characteristics of quitters and non-quitters, in univariable analysis
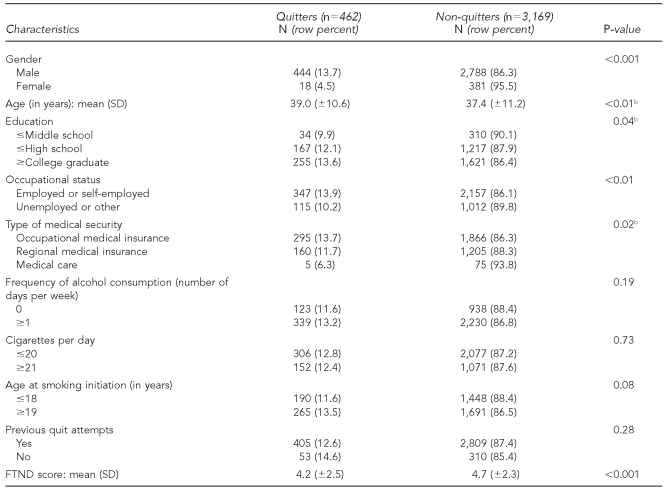
As shown in Table 3, the factors of successful smoking cessation at 12-month follow-up by univariable analyses were as follows: male gender, older age, high education level, employed, holder of occupational medical insurance or regional medical insurance rather than medical care, and low FTND scores. No significant differences vis-à-vis frequency of alcohol consumption per week, number of cigarettes per day, or age at smoking initiation were noted between quitters and non-quitters.
Table 3.
Baseline characteristics of quitters and non-quitters at 12-month follow-up in univariable analyses among participants in the Korean quitline service (n=3,631)a: South Korea, 2006–2007
aNot all the sums in each of the 2×2 tables total 3,631 due to missing values.
bP-value for trend
SD = standard deviation
FTND = Fagerstrom Test for Nicotine Dependence
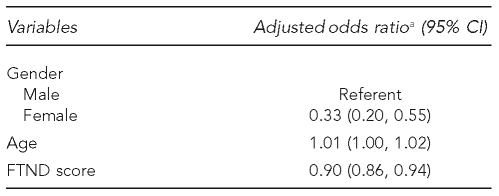
Factors of smoking cessation in multiple logistic regression analyses
In multiple logistic regression analyses, the factors of smoking cessation at 12-month follow-up were male gender, older age, and low FTND scores after adjusting for main independent variables such as gender, age, education level, occupational status, type of medical security, frequency of alcohol consumption per week, previous quit attempts, and FTND score (Table 4).
Table 4.
Factors of successful smoking cessation at 12-month follow-up in multiple logistic regression analyses among participants in the Korean quitline service (n=3,631): South Korea, 2006–2007
aAdjusted for gender, age, education level, occupational status, type of medical security, frequency of alcohol consumption per week, previous quit attempts, and FTND score. Age and FTND scores are continuous variables.
CI = confidence interval
FTND = Fagerstrom Test for Nicotine Dependence
DISCUSSION
We conducted the Korean proactive quitline service for smoking cessation; based on literature published to date, it is only the second quitline service operating in the Far East, following one in Hong Kong. Our study showed a self-reported 12.8% continuous abstinence rate at 12 months among the 3,631 subjects. In comparison, the California Smoker's Helpline reported an abstinence rate at 12 months of 9.1% for those in the treatment group (n=1,973) who had been registered to receive up to seven counseling sessions.15 The Australian telephone quitline service also reported that only 5.0% of the cohort who had been smoking at baseline had quitt for an entire year.1 Meanwhile, the Swedish quitline reported that the point-prevalence abstinence rate at 12 months of the proactive treatment group was 32.6% (205/629).2 Although there were difficulties in comparing the abstinence rates of the various studies—owing to differences in the definitions, criteria, study designs, and populations involved therein—the 12-month abstinence rate in our study was similar to or slightly higher than those of other studies.
The high abstinence rate uncovered by this study is thought to be associated with the more intensive, proactive counseling sessions conducted in this study vs. other studies, as well as the SMSs. A meta-analysis of the effect of telephone counseling on smoking cessation reported that 19 trials offering between three and six sessions showed a significant effect compared with the control group, while seven trials providing one or two counseling calls showed no significant effect.9 Moreover, proactive counseling has been considered more effective than reactive counseling in encouraging participants to quit smoking.9,10 The SMSs via cellular phone might have contributed to the subjects' successful smoking cessation, as they encouraged and supported abstinence from smoking. SMSs through cellular phones, as part of the quitline service protocol, can be effective in countries such as Korea where cellular phones are commonly used. Korea has 90.2 cellular phone subscribers per 100 inhabitants, based on the Information and Communication Technology Statistics 2007 of the International Telecommunication Union.16
We estimated abstinence rates without using biochemical validation techniques such as urinary cotinine concentration or expired carbon monoxide. However, a biochemical validation is considered to be uninformative in low-intensity interventions, such as those in the quitline service.17,18 Moreover, several previous studies have suggested that self-reported smoking status is considerably accurate.19,20
Previous studies have reported that the factors of smoking cessation are as follows: age, gender, cigarette consumption per day, readiness to quit smoking, follow-up time, education level, perceived ease or difficulty in quitting, presence of smokers at home, helpful support while quitting, previous history of abstinence, and the use of clinical help and/or nicotine replacement therapy.3,12,21,22
The factors of successful smoking cessation in this study were male gender, older age, high education level, employment, holder of occupational medical insurance, and a low FTND score. Regarding types of medical insurance, one possible explanation could be associated with the fact that the smokers with occupational medical insurance had difficulties in maintaining a smoking habit, due to smoking bans in the workplace—a circumstance not likely applicable to those with regional medical insurance.
Our study showed no significant association between previous quit attempts and abstinence. According to the literature, the association between them is controversial. Some studies reported that the number of previous quit attempts or the quit days during the previous quit attempts were positively associated with successful abstinence among users of a quitline service3,21 and among smokers of a cohort survey not using a quitline service.23 In the meantime, other studies not using a quitline service reported that the number of previous quit attempts had no significant association with successful abstinence;24,25 on the contrary, several clinical trials using pharmacologic treatments such as nicotine patches or bupropion reported that smokers who relapsed and attempted to quit again had poorer abstinence outcomes than smokers who tried to quit only once.26,27
Limitations
Our study had several limitations. First, we had no control group for comparison. Further study using a randomized controlled design is needed. Second, the proportion of female subjects in our study was extremely low compared with that of other studies, which is strongly associated with an extremely low smoking prevalence among Korean women. As mentioned previously, the smoking prevalence was 46.6% among Korean men but only 4.6% among Korean women in 2005.11 Third, we did not evaluate the participants' use of pharmacologic products such as nicotine patches, bupropion, and other forms of smoking cessation drugs, which might affect the abstinence rates. Lastly, information bias could have occurred because all follow-up information was collected by counselors, and this might have affected the reported quit rates. That is, we could not rule out the possibility that the actual smoking cessation rates might be lower than the ones reported.
CONCLUSION
This study confirmed that the proactive quitline service for smoking cessation in Korea had abstinence rates similar to or higher than the previous reported quitline programs and determined the factors of successful smoking cessation. Further studies should be considered to determine the cost-benefit effect of the Korean proactive quitline service.
Acknowledgments
The authors thank those who supported and helped this study, including the National Cancer Center; Ministry of Health and Welfare, Korea; Sang-Wha Shin, a data manager, and 30 smoking cessation counselors at the Korean proactive quitline service center; and Diana McDonnell, PhD, a research epidemiologist at the Center for Family and Community Health at the University of California, Berkeley School of Public Health in Berkeley, California.
Footnotes
This study was supported by the Funds for Health Promotion provided by the Ministry of Health and Welfare of Korea for the implementation of the smoking cessation policy of the Korean government.
REFERENCES
- 1.Miller CL, Wakefield M, Roberts L. Uptake and effect of the Australian telephone quitline service in the context of a mass media campaign. Tob Control. 2003;12(Suppl 2):ii53–8. doi: 10.1136/tc.12.suppl_2.ii53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Helgason AR, Tomson T, Lund KE, Galanti R, Ahnve S, Gilljam H. Factors related to abstinence in a telephone helpline for smoking cessation. Eur J Public Health. 2004;14:306–10. doi: 10.1093/eurpub/14.3.306. [DOI] [PubMed] [Google Scholar]
- 3.Abdullah ASM, Lam TH, Chan SSC, Hedley AJ. Which smokers use the smoking cessation quitline in Hong Kong, and how effective is the quitline? Tob Control. 2004;13:415–21. doi: 10.1136/tc.2003.006460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.HHS “quitline” helps Americans stop smoking. FDA Consumer. 2005;39:4–5. [PubMed] [Google Scholar]
- 5.Wilson N, Thomas G, Grigg M, Afzal R. New smoke-free environments legislation stimulates calls to a national quitline. Tob Control. 2005;14:287–8. doi: 10.1136/tc.2005.011726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gilbert H, Sutton S. Evaluating the effectiveness of proactive telephone counseling for smoking cessation in a randomized controlled trial. Addiction. 2006;101:590–8. doi: 10.1111/j.1360-0443.2006.01398.x. [DOI] [PubMed] [Google Scholar]
- 7.Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ. Clinical practice guideline. Rockville (MD): Department of Health and Human Services, Public Health Service (US); 2008. May, Treating tobacco use and dependence: 2008 update. [Google Scholar]
- 8.Macleod ZR, Charles MA, Arnaldi VC, Adams IM. Telephone counseling as an adjunct to nicotine patches in smoking cessation: a randomized controlled trial. Med J Aust. 2003;179:349–52. doi: 10.5694/j.1326-5377.2003.tb05590.x. [DOI] [PubMed] [Google Scholar]
- 9.Stead LF, Perera R, Lancaster T. Telephone counseling for smoking cessation. Cochrane Database Syst Rev. 2006;3:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Pan W. Proactive telephone counseling as an adjunct to minimal intervention to for smoking cessation: a meta-analysis. Health Educ Res. 2006;21:416–27. doi: 10.1093/her/cyl040. [DOI] [PubMed] [Google Scholar]
- 11.Organization for Economic Co-Operation and Development. OECD health data 2010. [cited 2011 Mar 18]. Available from: URL: http://stats.oecd.org/wbos/Index.aspx?DatasetCode=HEALTH.
- 12.Myung SK, Park JG, Bae WK, Yeon JL, Kim Y, Hong GS. Effectiveness of proactive quitline service and predictors of successful smoking cessation: findings from a preliminary study of quitline service for smoking cessation in Korea. J Korean Med Sci. 2008;23:888–94. doi: 10.3346/jkms.2008.23.5.888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park SM, Son KY, Lee YJ, Lee HC, Kang JH, Lee YJ, et al. A preliminary investigation of early smoking initiation and nicotine dependence in Korean adults. Drug Alcohol Depend. 2004;74:197–203. doi: 10.1016/j.drugalcdep.2004.01.001. [DOI] [PubMed] [Google Scholar]
- 14.SPSS, Inc. SPSS®. Version 12.0. Chicago: SPSS, Inc.; 2005. [Google Scholar]
- 15.Zhu SH, Anderson CM, Tedeschi GJ, Rosbrook B, Johnson CE, Byrd M, et al. Evidence of real-world effect of a telephone quitline for smokers. N Engl J Med. 2002;347:1087–93. doi: 10.1056/NEJMsa020660. [DOI] [PubMed] [Google Scholar]
- 16.International Telecommunication Union. ITU ICT Eye: ICT statistics 2009. [cited 2011 Mar 18]. Available from: URL: http://www.itu.int/ITU-D/icteye/Reporting/ShowReportFrame.aspx?ReportName=/WTI/CellularSubscribersPublic&ReportFormat=HTML4.0&RP_intYear=2007&RP_intLanguageID=1&RP_bitLiveData=False.
- 17.Velicer WF, Prochaska JO, Rossi JS, Snow MG. Assessing outcome in smoking cessation studies. Psychol Bull. 1992;111:23–41. doi: 10.1037/0033-2909.111.1.23. [DOI] [PubMed] [Google Scholar]
- 18.SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4:149–59. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- 19.Glasgow RE, Mullooly JP, Vogt TM, Stevens VJ, Lichtenstein E, Hollis JF, et al. Biochemical validation of smoking status: pros, cons, and data from four low-intensity intervention trials. Addict Behav. 1993;18:511–27. doi: 10.1016/0306-4603(93)90068-k. [DOI] [PubMed] [Google Scholar]
- 20.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking; a review and meta-analysis. Am J Public Health. 1994;84:1086–93. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaen CR, Cummings KM, Zielezny M, O'Shea R. Patterns and predictors of smoking cessation among users of a telephone hotline. Public Health Rep. 1993;108:772–8. [PMC free article] [PubMed] [Google Scholar]
- 22.Balanda KP, Lowe JB, O'Connor-Fleming ML. Comparison of two self-help smoking cessation booklets. Tob Control. 1999;8:57–61. doi: 10.1136/tc.8.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tob Control. 1997;6(Suppl):S57–62. doi: 10.1136/tc.6.suppl_2.s57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. 2004;6(Suppl 3):S363–9. doi: 10.1080/14622200412331320761. [DOI] [PubMed] [Google Scholar]
- 25.Ferguson JA, Patten CA, Schroeder DR, Offord KP, Eberman KM, Hurt RD. Predictors of 6-month tobacco abstinence among 1,224 cigarette smokers treated for nicotine dependence. Addict Behav. 2003;28:1203–18. doi: 10.1016/s0306-4603(02)00260-5. [DOI] [PubMed] [Google Scholar]
- 26.Gourlay SG, Forbes A, Marriner T, Pethica D, McNeil JJ. Double blind trial of repeated treatment with transdermal nicotine for relapsed smokers. BMJ. 1995;311:363–6. doi: 10.1136/bmj.311.7001.363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gonzales DH, Nides MA, Ferry LH, Kustra RP, Jamerson BD, Segall N, et al. Bupropion SR as an aid to smoking cessation in smokers treated previously with bupropion: a randomized placebo-controlled study. Clin Pharmacol Ther. 2001;69:438–44. doi: 10.1067/mcp.2001.115750. [DOI] [PubMed] [Google Scholar]