Oral health conditions in parts of Appalachia—a region of the United States spanning 13 states across the Appalachian Mountains from southern New York to Northern Mississippi and including 24.8 million people—are considered severe.1–3 In particular, Kentucky, a highly Appalachian state containing the highest proportion of economically distressed counties across all of Appalachia,4 has some of the worst oral health outcomes in the nation.5–7 Kentucky ranks seventh nationwide in the number of completely edentulous older adults,5 ninth in adults with any permanent teeth extracted,6 and eighth in the prevalence of individuals not having visited a dentist or dental clinic within the past year for any reason.7 Though Kentucky does have a high rate of water fluoridation,8 teeth cleanings, and dental sealants as compared with the rest of the nation, it still has a higher rate of caries and untreated caries among children.9
In addition, rural inhabitants in the U.S. have been shown to experience worse oral health outcomes compared with urban inhabitants. Vargas et al. found that adults living in rural areas in the U.S. were less likely to visit a dentist in the past year and more likely to be edentulous than their urban counterparts.10 About 30% of Kentuckians live in Appalachian-designated counties. These counties reflect high levels of rurality and some of the poorest populations in the U.S., contributing to the acute condition of oral health in the region.1 Further, as reported by their parents, rural Kentucky children are less likely to have teeth in excellent condition and to have dental insurance than their urban counterparts.11 These indicators seem to suggest the existence of geographic disparities with higher rates of oral health problems and lower use of dental care in Appalachian Kentucky—a predominantly rural region—than in non-Appalachian Kentucky. Unfortunately, tabular presentations of oral health data to policy makers can fail to convey both the relative magnitude and location of disparities.
To clearly illustrate the geographic differences in an oral health outcome in Kentucky, we proposed the use of two geospatial techniques: (1) a cartographic construction technique called the bivariate cartogram and (2) hot-spot cluster analysis. We chose to present these data with cartograms due to the limitations associated with the more commonly encountered choropleth map and tabular presentation displays. For example, tabular presentations of spatial data do not display data according to the context of space, thereby limiting the results and interpretation. Choropleth maps (i.e., thematic maps in which regions are shaded according to the distribution of data values) can often lead to misinterpretation by displaying larger regions more prominently than smaller ones. Cartograms are maps that proportionally scale the area of a geographic entity (e.g., counties, states, and countries) according to a given (i.e., nonspatial) attribute (e.g., population),12,13 thereby reducing the effect of the previously mentioned size-prominence limitation of choropleth maps. Bivariate cartograms use one attribute (e.g., county population) to proportionally rescale the area of each county polygon, and a second attribute (e.g., percentage of adults aged 18 years and older with six or more teeth removed because of tooth decay or gum disease) as a traditional choropleth-type thematic map.
A hot-spot cluster analysis is useful for investigating clusters of health events, such as the percentage of adults with six or more teeth removed by county in the Appalachian and non-Appalachian regions of Kentucky. Using hot-spot analysis for geospatial visualization can readily show the locations of significant hot spots or clusters of health events and, hence, help in identifying disparities. Individually, cartograms transform regions relative to an underlying variable, while a hot-spot analysis finds areas with statistical clusters at the county level. When used in conjunction, as performed in this study, the techniques produce a highly informative and visually compelling understanding of oral health disparities in the state.
These geographic techniques have been useful in assessing and investigating clustering patterns for other health events. For example, Mandal et al. found that breast and prostate cancers cluster spatially in the U.S., with clusters of counties with high cancer rates found in the North and clusters with low cancer rates found in the South.14 Studies with similar methodology have also used hot-spot analysis to identify elevated clusters of mosquito breeding,15 respiratory infection incidence rates,16 and typhoid outbreaks from 1906 to 1909.17 Moreover, cartograms have been used to visualize disparities in obesity prevalence by state,18 map the global burden of malaria,19 and map crime rates.20
To our knowledge, however, there are no extant examples of the use of these two techniques—bivariate cartograms and hot-spot analysis—in the relevant literature for examining oral health-related disparities. As an example of the intersection between oral health and geographic analysis, this study was intended to bridge that gap in the literature and highlight the use of a geographic information system (GIS) as a novel tool when analyzing regional-based oral health disparities. The findings from this study will be useful in guiding health planning, resource allocation, and policy decisions aimed at reducing oral health disparities and improving oral health for all Kentuckians.
METHODS
Cartogram analysis
We created cartograms using ArcGIS® version 9.321 that visualized 2006 population estimates,22 2007 dental workforce,23 and an oral health outcome across Kentucky by county. We calculated the dental workforce by county, defined as dentists per 10,000 population, by geocoding the physical practice addresses of all Kentucky dentists and calculating the rate as a point-in-polygon count of dentists divided by the respective county population. County polygon areas were then transformed by the resulting county populations and dentist-per-10,000 population ratio using the Gastner-Newman diffusion algorithm,24 available as a downloadable script for ArcGIS.25 Next, the newly transformed county polygons were shaded as a choropleth map using the percentage, by county, of adults aged 18 years and older with six or more permanent teeth removed because of tooth decay or gum disease. The data for this variable were taken from a 2007 report by the Kentucky Institute of Medicine,26 which compiled data from the Kentucky Behavioral Risk Factor Surveillance System in the years 1997, 1999, 2002, and 2004.27 County polygons were shaded by the relative values of the oral health outcome variable as categorized into five classes using the Natural Breaks algorithm,28 with a monochromatic color scheme provided by ColorBrewer.org.29,30
Appalachian county designations were identified from the Appalachian Regional Commission.1 We downloaded the Kentucky county polygon data from the Kentucky Division of Geographic Information.31 We also created a table to offer a brief descriptive understanding of the cartograms. We performed student's two-sample t-tests on the variables in the Table comparing Appalachia with non-Appalachia using SAS® version 9.1.32
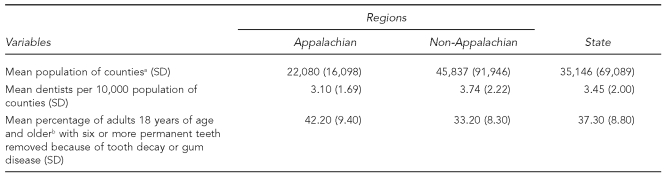
Table.
Descriptive statistics for variables of interest in a study of oral health in Appalachian and non-Appalachian regions in Kentucky
ap<0.05; two-sample t-test assuming unequal variances
bp<0.0001; two-sample t-test assuming equal variances
SD = standard deviation
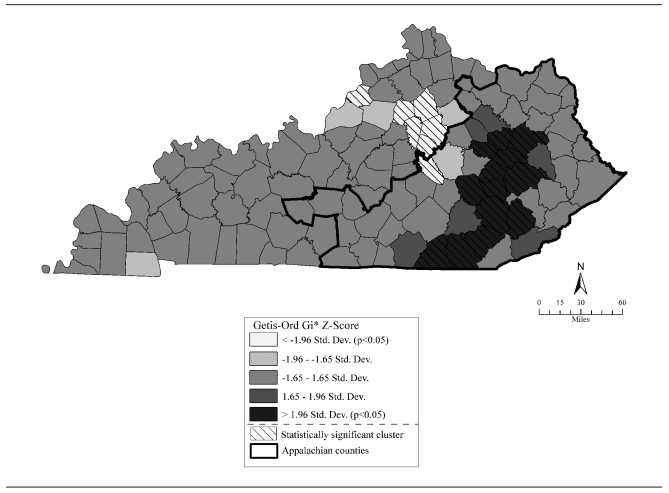
Hot-spot analysis
We performed a hot-spot analysis using the hot-spot analysis tool in ArcGIS, based on the Getis-Ord Gi* statistic,33 to identify counties with statistically significant (p<0.05) clusters of high or low rates of the percentage of adults with six or more teeth removed because of tooth decay or gum disease. Extreme (high or low) values of the Getis-Ord Gi* statistic indicated an increasing intensity of clusters of high or low values (i.e., a nonrandom distribution of the oral health outcome by county). The output statistic of the hot-spot analysis, the Z-score, measures the standard deviation (SD). Counties with statistically significantly higher Z-scores (darker counties) indicate a cluster of counties with a higher percentage of adults with six or more teeth removed because of tooth decay or gum disease, and counties with statistically significantly lower Z-scores (lighter counties) indicate a cluster of counties with a lower percentage of adults with six or more teeth removed because of tooth decay or gum disease (Figure 1).
Figure 1.
Higha and lowb hot-spot GI* analysis of the percentage of adults 18 years of age and older with six or more permanent teeth removed because of tooth decay or gum disease in Kentucky
aHigh clusters (darker counties): 13 out of the 54 Appalachian counties were nonrandom clusters (p<0.05) with respect to oral health outcome (i.e., higher percentage of adults with teeth removed). One of the 13 Appalachian counties had a low cluster. This county was relatively close to lower Z-score cluster counties and just within the border of the Appalachian region.
bLow clusters (lighter counties): six non-Appalachian counties were nonrandom clusters (p<0.05) with respect to oral health outcome (i.e., lower percentage of adults with teeth removed).
Std. dev. = standard deviation
RESULTS
As shown in Figure 2a, an untransformed choropleth map of Kentucky highlights the concentration of darker counties—those with a higher percentage of adults with six or more teeth removed—in the Appalachian region. Nine of the 10 counties in the bottom oral health class—51%–65%—are located in the Appalachian region. The cartogram in Figure 2b, as transformed by county population, depicts counties with the largest populations as also having the largest areas, and typically better oral health per the oral health outcome. The cartogram in Figure 2c, as transformed by dentists per 10,000 population, shows a similar trend as Figure 2b in that counties with the largest areas—i.e., higher ratios of dentists per 10,000 population—also had the lowest percentage of adults with six or more teeth removed. Counties with lower ratios of dentists per 10,000 population tend to be Appalachian and have worse oral health as measured by our oral health outcome. Thus, Figure 2 illustrates three spatial disparities: an oral health disparity between Appalachian and non-Appalachian Kentucky, between higher and lower population counties, and between counties with higher and lower numbers of dentists per 10,000 population.
Figure 2.
Percentage of adults 18 years of age or older with six or more permanent teeth removed because of tooth decay or gum disease in Kentucky shown in (a) an untransformed choropleth map, (b) a 2006 county population cartogram, and (c) a 2007 dental workforce cartograma
aKentucky counties transformed proportional to county populations for 2006 (b) and proportional to the ratio of dentists per 10,000 population within each county (c). Two Appalachian counties (Robertson and Owsley) have zero dentists and are distorted enough not to be visible (c).
The Table shows that the mean population and mean number of dentists per 10,000 population in Appalachia were lower than in non-Appalachian Kentucky and Kentucky, and the mean percentage of adults with six or more teeth removed was higher in Appalachia than in non-Appalachia and Kentucky. We found no significant differences between Appalachia and non-Appalachia for the number of dentists per 10,000 population, but we did find significant differences between the two regions for the oral health outcome (p<.0001) and population variables (p<0.05).
Figure 1 shows that counties with a higher percentage of adults with six or more teeth removed because of tooth decay or gum disease (darker counties: >1.96 SD) were statistically significantly clustered (i.e., non-randomly distributed) in the Appalachian region, thus confirming the results of an oral health spatial-based disparity between Appalachian and non-Appalachian Kentucky. The map also shows that counties with a lower percentage of adults with six or more teeth removed because of tooth decay or gum disease (lighter counties: <1.96 SD) were statistically significantly clustered in the non-Appalachian region. We repeated this analysis for the ratio of dentists per 10,000 population variable with some similar results: high clusters (>1.96 SD ratios of dentists per 10,000 population) were found in five non-Appalachian counties, and one Appalachian county was a statistically significant low cluster (<1.96 SD) (data not shown).
DISCUSSION
The depictions of a distorted, or rescaled, Kentucky via cartograms in addition to the hot-spot analysis provide policy makers with evidence of spatially and statistically based oral health disparities between Appalachian and non-Appalachian Kentucky and some evidence of a dental workforce misdistribution. These two geographic analytical techniques were useful in conjunction because, while the results in Figure 2 show the effect that dentist and population density have on the oral health outcome (i.e., generally worse oral health in counties with lower dentist and population densities), Figure 1 pinpoints specific clusters of counties with significantly high rates of the percentage of adults with six or more teeth removed because of tooth decay or gum disease. Both figures offer policy makers a clear guide to county-level funding allocation for the improvement of oral health. Together, these geographic techniques present an informative visualization of the state by oral health and a thorough and accurate depiction of the spatial component of oral health disparities with respect to our outcome. This study also brought light to the importance of accounting for place of residence in dental public health research through the use of spatial statistical techniques and GIS.
The public health significance of these findings is broad. The implications of these results can drive policy-making and funding allocation, and provide a basis for further investigation into the causes of these patterns. Specifically, this study provides policy makers with a visualization of the oral health burden faced in Appalachian Kentucky to direct efforts in that region and improve overall oral health. Also, the use of carto-grams coupled with a hot-spot analysis offers a unique way of visualizing health-related disparities to policy makers, the lay public, and researchers.
In addition, these findings are important to the field of public health because oral health is often an overlooked component of general health and well-being. In 2000, the Surgeon General called oral disease a “silent epidemic” because of its ubiquitous nature and disproportionate effect on “… our most vulnerable citizens—poor children, the elderly, and many members of racial and ethnic minority groups.”34 Moreover, poor oral health has been associated with an elevated risk of heart disease.35,36 Among adults, poor oral health has also been associated with absences from work34 and low self-esteem.37,38
The hot-spot analysis showed counties with a higher percentage of adults with six or more teeth removed because of tooth decay or gum disease clustered in the Appalachian region—a region characterized by low population densities, low dentist densities, and high poverty rates. These variables inextricably define much of Appalachian Kentucky39,40 and may explain why an oral health disparity exists. Future studies should seek to perform regression analyses to try to more thoroughly explain why much of Appalachian Kentucky is experiencing poorer oral health relative to non-Appalachian Kentucky. Moreover, although not every county with a high percentage (51%–65%) of the oral health outcome is shown as being part of a significantly high cluster, policy makers should not neglect those counties simply because they are not part of a high cluster. Counties that were not high clusters but had a high percentage of adults with six or more teeth removed because of tooth decay or gum disease still represent areas in which funding should be focused.
Limitations
This study had several limitations. One limitation was the artificially abrupt change in the oral health outcome that occurred from county boundary to county boundary and the use of county-level choropleth thematic mapping that depicted a synthetic uniformity (ecological fallacy) of the oral health outcome across counties. In addition, the oral health outcome used in this study was limited to adults aged 18 years and older with six or more permanent teeth removed because of tooth decay or gum disease. While it was necessary to be specific for the sake of this research, this outcome does not sufficiently provide an exhaustive understanding of oral health in Kentucky. Future studies should seek to offer a more rounded assessment of oral health by examining more oral health outcomes and indicators using geospatially based methods. In addition, although cartograms represent an important visual tool in oral health epidemiology and health geography, they may at first seem difficult to interpret. It has been shown, however, that providing a basic briefing on cartograms allows for a better understanding of the maps.41
CONCLUSIONS
Cartograms and hot-spot analysis, though only two elements in the spectrum of geography and spatial statistics, provide a more novel representation of spatial disparities than classic tabular presentations, minimize limitations associated with choropleth maps, add a dimension of data (i.e., spatial weighting) beyond the typical map, and identify nonrandom clusters of health events. These two tools can be used by policy makers to determine where oral health disparities exist and pinpoint specific areas of need when allocating funds for and improving oral health across entire populations. Finally, this study highlights certain areas in a predominantly rural state that are experiencing oral health-related disparities and demonstrates the need to account for place of residence when performing public health research.
Footnotes
This article was presented orally as a poster session at the American Public Health Association Conference in Philadelphia in November 2009.
REFERENCES
- 1.Appalachian Regional Commission. Counties in Appalachia. [cited 2010 Mar 20]. Available from: URL: http://www.arc.gov/counties.
- 2.University of Pittsburgh School of Dental Medicine. Center for Oral Health Research in Appalachia. [cited 2011 Jan 15]. Available from: URL: http://www.dental.pitt.edu/research/research_oralhealth.php.
- 3.Martin CA, McNeil DW, Crout RJ, Ngan PW, Weyant RJ, Heady HR, et al. Oral health disparities in Appalachia: orthodontic treatment need and demand. JADA. 2008;139:598–604. doi: 10.14219/jada.archive.2008.0221. [DOI] [PubMed] [Google Scholar]
- 4.Appalachian Regional Commission. County economic status in Appalachia, FY 2011. [cited 2011 Jan 15]. Available from: URL: http://www.arc.gov/research/MapsofAppalachia.asp?MAP_ID=54.
- 5.Centers for Disease Control and Prevention, Office of Surveillance, Epidemiology, and Laboratory Services (US). Behavioral Risk Factor Surveillance System prevalence and trends data: oral health—2008: adults aged 65+ who have had all their natural teeth extracted. [cited 2011 Jan 15]. Available from: URL: http://apps.nccd.cdc.gov/brfss/list.asp?cat=OH&yr=2008&qkey=6606&state=All.
- 6.CDC, Office of Surveillance, Epidemiology, and Laboratory Services (US). Behavioral Risk Factor Surveillance System prevalence and trends data: oral health—2008: adults that have had any permanent teeth extracted. [cited 2011 Jan 15]. Available from: URL: http://apps.nccd.cdc.gov/brfss/list.asp?cat=OH&yr=2008&qkey=6607&state=All.
- 7.CDC, Office of Surveillance, Epidemiology, and Laboratory Services (US). Behavioral Risk Factor Surveillance System prevalence and trends data: oral health—2008: visited the dentist or dental clinic within the past year for any reason. [cited 2011 Jan 15]. Available from: URL: http://apps.nccd.cdc.gov/brfss/list.asp?cat=OH&yr=2008&qkey=6610&state=All.
- 8.Populations receiving optimally fluoridated public drinking water—United States, 2000. MMWR Morb Mortal Wkly Rep. 2002;51(7):144–7. [PubMed] [Google Scholar]
- 9.Chattopadhyay A, Arevalo O, Cecil JC., III Kentucky's oral health indicators and progress towards Healthy People 2010 objectives. J Ky Med Assoc. 2008;106:165–74. [PubMed] [Google Scholar]
- 10.Vargas CM, Dye BA, Hayes KL. Oral health status of rural adults in the United States. J Am Dent Assoc. 2002;133:1672–81. doi: 10.14219/jada.archive.2002.0120. [DOI] [PubMed] [Google Scholar]
- 11.Martin AB, Wang E, Probst JC, Hale N, Johnson AO. Dental health and access to care among rural children: a national and state portrait. Columbia (SC): South Carolina Rural Health Research Center; 2008. [cited 2011 Jan 15]. Also available from: URL: http://rhr.sph.sc.edu/report/(7-2)%20Dental%20Health%20and%20Access%20to%20Care%20Among%20Rural%20Children.pdf.
- 12.Jackel CB. Using ArcView to create contiguous and noncontiguous area cartograms. CaGIS. 1997;24:101–9. [Google Scholar]
- 13.Bortins I, Demers S. Cartogram types: what is a cartogram? [cited 2010 Mar 20]. Available from: URL: http://www.ncgia.ucsb.edu/projects/Cartogram_Central/types.html.
- 14.Mandal R, St-Hilaire S, Kie JG, Derryberry D. Spatial trends of breast and prostate cancers in the United States between 2000 and 2005. Int J Health Geogr. 2009;8:53. doi: 10.1186/1476-072X-8-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rochlin I, Iwanejko T, Dempsey ME, Ninivaggi DV. Geostatistical evaluation of integrated marsh management impact of mosquito vectors using before-after-control-impact (BACI) design. Int J Health Geogr. 2009;8:35. doi: 10.1186/1476-072X-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rojas F. Poverty determinants of acute respiratory infections among Mapuche indigenous peoples in Chile's Ninth Region of Araucania, using GIS and spatial statistics to identify health disparities. Int J Health Geogr. 2007;6:26–1. doi: 10.1186/1476-072X-6-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hinman SE, Blackburn JK, Curtis A. Spatial and temporal structure of typhoid outbreaks in Washington, D.C., 1906–1909: evaluating local clustering with the Gi* statistic. Int J Health Geogr. 2006;5:13. doi: 10.1186/1476-072X-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Houle B, Holt J, Gillespie C, Freedman DS, Reyes M. Use of density-equalizing cartograms to visualize trends and disparities in state-specific prevalence of obesity: 1996–2006. Am J Public Health. 2009;99:308–12. doi: 10.2105/AJPH.2008.138750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Guerra CA, Snow RW, Hay SI. Mapping the global extent of malaria in 2005. Trends Parasitol. 2006;22:353–8. doi: 10.1016/j.pt.2006.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andresen MA, Wuschke K, Kinney JB, Brantingham PJ, Brantingham PL. Cartograms, crime, and location quotients. Crime Patterns and Analysis. 2009;2:31–46. [Google Scholar]
- 21.Environmental Systems Research Institute, Inc. ArcGIS®: Version 9.3. Redlands (CA): ESRI; 2009. [Google Scholar]
- 22.Kentucky State Data Center. School of Urban and Public Affairs, University of Louisville. Population and housing unit estimates for 2006. [cited 2008 Jan 12]. Available from: URL: http://ksdc.louisville.edu/kpr/popest/est.htm.
- 23.Kentucky Board of Dentistry. Dental license search. [cited 2007 Sep 12]. Available from: URL: http://web1.ky.gov/gensearch/LicenseSearch.aspx?AGY=9.
- 24.Gastner MT, Newman MEJ. Diffusion-based method for producing density-equalizing maps. Proc Natl Acad Sci U S A. 2004;101:7499–504. doi: 10.1073/pnas.0400280101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Environmental Systems Research Institute, Inc. Support: cartogram geoprocessing tool version 2. [cited 2011 Mar 1]. Available from: URL: http://arcscripts.esri.com/details.asp?dbid=15638.
- 26.Kentucky Institute of Medicine. The health of Kentucky: a county assessment. 2007. [cited 2011 Mar 1]. Available from: URL: http://kyiom.org/pdf/healthy2007a.pdf.
- 27.CDC (US). Behavioral Risk Factor Surveillance System annual survey data. [cited 2011 Mar 1]. Available from: URL: http://www.cdc.gov/brfss/technical_infodata/surveydata.htm.
- 28.Jenks GF, Caspall FC. Error on choropleth maps: definition, measurement, reduction. Ann Assoc Am Geogr. 1971;61:217–44. [Google Scholar]
- 29.Brewer CA. Color use guidelines for mapping and visualization. In: MacEachren AM, Taylor DRF, editors. Visualization in modern cartography. Tarrytown (NY): Elsevier Science; 1994. pp. 123–47. [Google Scholar]
- 30.Brewer C, Harrower M Pennsylvania State University. ColorBrewer 2.0: color advice for cartography. [cited 2011 Mar 1]. Available from: URL: http://colorbrewer2.org.
- 31.Kentucky Geography Network. Explore the Commonwealth. [cited 2011 Mar 1]. Available from: URL: http://kygeonet.ky.gov.
- 32.SAS Institute, Inc. SAS®: Version 9.1 for Windows. Cary (NC): SAS Institute, Inc.; 2009. [Google Scholar]
- 33.Ord JK, Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geogr Analysis. 1995;27:286–306. [Google Scholar]
- 34.Department of Health and Human Services (US). Oral health in America: a report of the Surgeon General. Rockville (MD): HHS, National Institute of Dental and Craniofacial Research, National Institutes of Health (US); 2000. [cited 2010 May 30]. Also available from: URL: http://www.surgeongeneral.gov/library/oralhealth. [Google Scholar]
- 35.Joshipura KJ, Rimm EB, Douglass CW, Trichopoulos D, Ascherio A, Willett WC. Poor oral health and coronary heart disease. J Dent Res. 1996;75:1631–6. doi: 10.1177/00220345960750090301. [DOI] [PubMed] [Google Scholar]
- 36.Janket SJ, Qvarnstrom M, Meurman JH, Baird AE, Nuutinen P, Jones JA. Asymptotic dental score and prevalent coronary heart disease. Circulation. 2004;109:1095–100. doi: 10.1161/01.CIR.0000118497.44961.1E. [DOI] [PubMed] [Google Scholar]
- 37.Cushing AM, Sheiham A, Maizels J. Developing socio-dental indicators—the social impact of dental disease. Community Dent Health. 1986;3:3–17. [PubMed] [Google Scholar]
- 38.Benyamini Y, Leventhal H, Leventhal EA. Self-rated oral health as an independent predictor of self-rated general health, self-esteem and life satisfaction. Soc Sci Med. 2004;59:1109–16. doi: 10.1016/j.socscimed.2003.12.021. [DOI] [PubMed] [Google Scholar]
- 39.Appalachian Regional Commission. County economic status in Appalachia, FY 2010. [cited 2011 Mar 1]. Available from: URL: http://www.arc.gov/research/MapsofAppalachia.asp?MAP_ID=53.
- 40.Saman DM, Arevalo O, Johnson AO. The dental workforce in Kentucky: current status and future needs. J Public Health Dent. 2010;70:188–96. doi: 10.1111/j.1752-7325.2010.00164.x. [DOI] [PubMed] [Google Scholar]
- 41.Sui DZ, Holt JB. Visualizing and analyzing public-health data using value-by-area cartograms: toward a new synthetic framework. Cartographica. 2008;43:3–20. [Google Scholar]