Abstract
Family planning is hailed as one of the great public health achievements of the last century, and worldwide acceptance has risen to three-fifths of exposed couples. In many countries, however, uptake of modern contraception is constrained by limited access and weak service delivery, and the burden of unintended pregnancy is still large. This review focuses on family planning's efficacy in preventing unintended pregnancies and their health burden. The authors first describe an epidemiologic framework for reproductive behavior and pregnancy intendedness and use it to guide the review of 21 recent, individual-level studies of pregnancy intentions, health outcomes, and contraception. They then review population-level studies of family planning's relation to reproductive, maternal, and newborn health benefits. Family planning is documented to prevent mother-child transmission of human immunodeficiency virus, contribute to birth spacing, lower infant mortality risk, and reduce the number of abortions, especially unsafe ones. It is also shown to significantly lower maternal mortality and maternal morbidity associated with unintended pregnancy. Still, a new generation of research is needed to investigate the modest correlation between unintended pregnancy and contraceptive use rates to derive the full health benefits of a proven and cost-effective reproductive technology.
Keywords: contraception; contraceptive behavior; family planning services; pregnancy outcome; pregnancy, unplanned; reproduction
INTRODUCTION
In 1999, the Centers for Disease Control and Prevention identified family planning as one of 10 great public health achievements in the United States during the 20th century (1). Alongside other achievements, such as vaccination and control of infectious diseases, access to family planning and contraceptive services was cited for social, economic, and health benefits conferred through “smaller family size and longer interval between the birth of children; increased opportunities for preconceptional counseling and screening; fewer infant, child, and maternal deaths; and the use of barrier contraceptives to prevent pregnancy and transmission of human immunodeficiency virus and other STDs [sexually transmitted diseases]” (1, p. 241). In the United States, contraceptive use among all women 15–44 years of age in 2002 was 61.9% in 2002 and considerably higher (72.9%) among married women. More than 45 million US women use contraception, relying primarily on the pill, female and male sterilization, and condoms.
The prevalence of contraceptive use is similarly high in European, many Latin American, and east and southeast Asian countries. Contraceptive use among partnered women aged 15–49 years in the developing world rose from 14% in the mid-1960s (2) to 62% in 2008 (3) and from protecting approximately 70 million to more than 600 million couples from unintended pregnancies. Rapid adoption of contraception has been documented in countries as diverse as Thailand, Iran, Egypt, and Colombia between the mid-1980s and mid-2000s (4). In low-income countries in sub-Saharan Africa, south Asia, and Central America, use of modern contraception is more modest and is constrained by limited access to services and weak government programs. While types of contraceptive methods used vary across regions, the health and social benefits of family planning are widely accepted across much of the world. Public sponsorship has launched most national family planning programs targeting low-income users, but modern contraceptive use has risen through sustained individual demand often met by an expansion of care from private providers.
Globally, the strength of government commitment tends to be greater than actual funding levels or program implementation efforts. Family planning has been cited as essential to the achievement of Millennium Development Goals (5) by former United Nations Secretary General Kofi Annan (6), and, as such, part of the fifth Millennium Development Goal targets universal access to family planning as a key strategy for improving maternal health. The proportion of governments in less-developed countries that provide direct or indirect support for contraceptive access grew from 64% in 1976 to 87% in 2009 (7). Global domestic spending on population activities—which includes family planning, reproductive health, sexually transmitted diseases/human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome, and basic research—by governments, nongovernmental organizations, and consumers reached $18.5 billion in 2006, but nearly half (45%) was allocated to sexually transmitted diseases/HIV/acquired immunodeficiency syndrome (8). Estimates of donor assistance in 2008 for this sector total $10.6 billion, but only $0.25 billion (2.4%) is directed toward supporting family planning (9), or approximately US $0.17 per woman of childbearing age in developing countries.
The term “family planning” has been used synonymously with contraceptive practice, although the ability to decide the number and timing of births can be achieved by a range of means, including contraception and assisted-reproductive technologies. Voluntary abstinence—either permanent or intermittent—elective abortion, and artificial insemination are other means commonly used by individuals to achieve reproductive intentions. In this review, we focus on contraception and address unsafe abortion as a preventable outcome of failed contraceptive behavior or methods.
Our review incorporates both population-level and individual-level perspectives in assessing the research evidence of contraceptive practice's relation to the burden of unintended pregnancies. The review has 4 parts. After framing the behavioral epidemiology that links sexual, reproductive, maternal, and newborn health outcomes, we briefly detail the measurement of unintended pregnancy and contraceptive practice. Next, we review findings from recent individual-level studies of 1) fertility intentions and pregnancy and maternal outcomes, 2) fertility intentions and contraceptive behaviors, and 3) contraceptive behaviors and unintended pregnancy outcomes. In the fourth part, we review research on the population-level health implications of family planning need.
A reproductive behavioral epidemiology framework
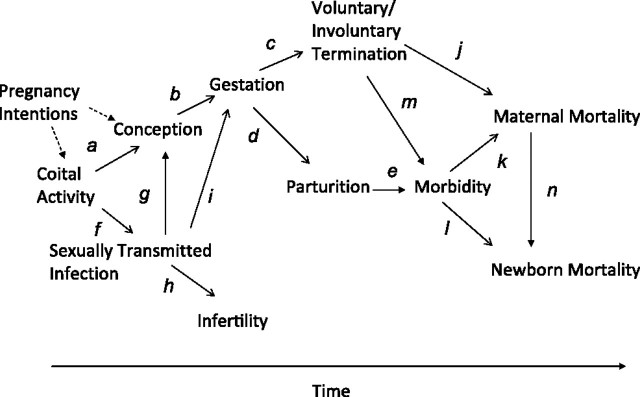
With broad acceptance of contraception as a modern health technology, why do unintended pregnancies still constitute a health burden for women and their partners? The answers lie in the health risks associated with sexual activity and reproduction. Coition, conception, viable pregnancy, fetal growth, parturition, and the puerperium separately carry health risks or undesirable outcomes, such as sexually transmitted infection, unintended pregnancy, fetal wastage, stillbirth, and maternal and neonatal mortality. Successful progression through these events can be measured by postpartum health and survival of mothers and infants. Many health technologies, including contraception, increase the likelihood that each transition occurs successfully. Table 1 and Figure 1 convey the epidemiologic links among the events and the key interventions, particularly family planning, associated with the pathways.
Table 1.
Common Measures for Reproductive Epidemiology Outcomes and Range of Values
| Outcome and Measure | Numerator | Denominator | Constant | Observed Average or Range (Study Source)a | Geographic Reference | Pathway(s)b | Illustrative Key Intervention |
| Coital activity | |||||||
| Coition rate | Coitions | Day | 100 | 0.12–0.27 per day (Brown, 2000 (86)) | Across 9 sub-Saharan African countries | a | Contraception, sexuality education |
| f | Consistent condom use | ||||||
| Conception | |||||||
| Conception rate | Conception | Coitions | 100 | 2%–4% (Tietze, 1960 (10)); 3.1% (Wilcox et al., 2001 (11)) | Wilcox et al.: North Carolina | a | Contraception |
| b | Fetal nutrition supplementation | ||||||
| Pregnancy rate | Pregnancies | Exposed women | 1,000 | 137 per 1,000 women aged 15–44 years (Singh et al., 2009 (14)) | Worldwide | a | Contraception |
| b | Fetal nutrition supplementation | ||||||
| Unintended pregnancy rate | Unintended pregnancy | Exposed women | 1,000 | 57 per 1,000 women aged 15–44 years (Singh et al., 2009 (14)) | Developing countries | a | Contraception |
| c | Elective pregnancy termination | ||||||
| Sexually transmitted infection | |||||||
| Type-specific infection rate | Type of acquired infection | Coitions | 1,000 | 0.0082 (95% CI: 0.0039, 0.0150) (Wawer et al., 2005 (12)) | HIV-1 transmission rate per coital act in Rakai, Uganda | g | Antibiotics, sexual abstinence |
| h | Antibiotics | ||||||
| f and i | Consistent condom use with pregnant partner, ART | ||||||
| Fetal growth | |||||||
| Preterm birth rate | Livebirths occurring at <37 weeks of gestation | Births | 100 | 9.6% (95% CI: 6.2–11.9) births (Beck et al., 2010 (87)) | Worldwide | d | Maternal and fetal nutrition during current and prior pregnancies (contraception for birth spacing) |
| Fetal mortality ratio | Fetal deaths | Pregnancies | 100 | 14.7% (Ventura et al., 2009 (88)) | United States in 2005 | d | Smoking cessation, elimination of alcohol and other drug use in pregnancy |
| Pregnancy termination | |||||||
| Miscarriage rate | Spontaneous fetal losses | Exposed women | 1,000 | 19.4 per 1,000 women aged 15–44 years (Ventura et al., 2009 (88)) | United States in 2005 | d | Smoking cessation, elimination of alcohol and other drug use in pregnancy |
| Induced abortion rate | Induced abortions | Exposed women | 1,000 | 29 per 1,000 women aged 15–44 years (Singh et al., 2009 (14)) | Worldwide | a | Contraception to prevent unwanted pregnancies, before and after abortion |
| j, m | Safe abortion procedures, postabortion complications management | ||||||
| Induced abortion ratio | Induced abortions | Pregnancies | 100 | 41 in developed and 23 in developing regions in 1995 (Guttmacher Institute, 1999 (89)) | Worldwide | a | Contraception to prevent unwanted pregnancies |
| j, m | Safe abortion procedures, postabortion complications management | ||||||
| Parturition | |||||||
| Birth rate (general fertility rate) | Livebirths | Exposed women | 1,000 | 39 (Ukraine) to 245 (Niger) (Measure DHS StatCompiler (47)) | Worldwide | a | Contraception to avoid unintended pregnancies |
| d | Prenatal and delivery care, maternal and fetal nutrition, postpartum family planning | ||||||
| Maternal mortality ratio | Maternal deaths | Livebirths | 100,000 | 3 (Denmark) to 2,100 (Sierra Leone) per 100,000 livebirths (WHO, 2007 (90)) | Worldwide | e/k | Management of complications (hemorrhage, toxemia, sepsis); provision of emergency obstetric services, skilled birth attendance |
| n | Cesarean section | ||||||
| Stillbirth rate | Stillbirths (fetal deaths in the last 12 weeks of pregnancy) | Deliveries | 1,000 | 5 in developed countries to 32 in Africa and South Asia (Stanton et al., 2006 (91)) | Worldwide | a | Consistent condom use |
| e | Treatment of syphilis infection | ||||||
| Infant mortality | |||||||
| Infant mortality rate | Deaths of infants at <12 months of age | Livebirths | 1,000 | 4 in western European to 95 in middle African countries (Population Reference Bureau, 2009 (92)) | Worldwide | l | Infection prevention, immunization, breastfeeding, rehydration; contraception for birth spacing |
| Perinatal mortality rate | Deaths of infants within the first 7 days | Livebirths | 1,000 | 6 in western Europe to 76 in western Africa (WHO, 2006 (93)) | Worldwide | l | Infection prevention, immunization, breastfeeding, rehydration; contraception for birth spacing |
| Neonatal mortality | Deaths of infants within the first 28 days | Livebirths | 1,000 | 3 in western Europe to 49 in western Africa (WHO, 2006 (93)) | Worldwide | l | Infection prevention, immunization, breastfeeding, rehydration; contraception for birth spacing |
| Postneonatal mortality | Deaths of infants at between 28 days and 1 year of life | Livebirths | 1,000 | 2.2 in the United States in 2006 (NCHS), 4.3 in Georgia in 2005, 63.5 in Swaziland in 2006 (MEASURE DHS StatCompiler (47)) | Worldwide | l | Infection prevention, immunization, breastfeeding, rehydration |
Abbreviations: ART, antiretroviral therapy; CI, confidence interval; DHS, Demographic and Health Surveys; HIV, human immunodeficiency virus; NCHS, National Center for Health Statistics; WHO, World Health Organization.
Observed average or range as given in the cited source (author(s), year, (reference no.)) of cross-national variation.
Italic letters refer to pathways identified in Figure 1.
Figure 1.
Pathways between sexual, reproductive, maternal, and newborn health outcomes. Motivational pathways are represented by dashed lines, behavioral pathways by solid lines.
Starting with coital activity, the probability of conception during any random act of intercourse is thought to range between 3% and 5% (10). A recent study of conception risk by menstrual cycle day among a small sample of North Carolina women found a likelihood of 3.1% per coition overall (11). In addition to pregnancy, coital activity also carries the risk of sexually transmitted infection. The probability of acquiring an infection will depend on multiple factors, including exposure to a partner infected with an offending organism as well as number of partners and condom use. For example, Wawer et al. (12) found the probability of HIV-1 transmission to be 0.0082 (95% confidence interval (CI): 0.0039, 0.0150) per coital act in Rakai, Uganda. Sex protected by contraception and consistent condom use addresses both pathways a and f in Figure 1 and reduces pregnancies that are unplanned and/or exposed to sexually transmitted infections. Sexually transmitted infection, such as chlamydia, gonorrhea, and syphilis, increases the risk of preterm birth, low birth weight, and stillbirth (i, d). Recurrent infections cause subfecundity (g) and infertility (h).
The probability that conceptions become viable fetuses (b) and progress to term (d) is enhanced by maternal nutritional well-being before pregnancy and nutritional status during gestation (13). The prevalence of spontaneous abortion can range from 5% to 70% of pregnancies, depending on stage of development. Worldwide, 22% of pregnancies, or about 42 million, are electively terminated (c), of which 20 million terminations happen under unsafe conditions, mostly in the developing world (14). Contraception plays a key role in reducing reliance on elective abortions and can avert as many as 13%–15% of the maternal deaths that result from unsafe abortions (a-b-c-m). Figure 1 highlights the significance of protected coitus not only in preventing unintended pregnancy and sexually transmitted infection but also in lowering exposure to subsequent morbidity and mortality risks.
Terminology and definitions in unintended pregnancy research
Fertility-intention measures implicitly require individual cognition of the ability to control the timing and number of pregnancies. This recognition is near, but not completely, universal in the world. Santelli et al. rightly describe pregnancy intendedness as a “complex concept … encompassing affective, cognitive, cultural and contextual dimensions” (15, p. 94). The persistence and stability of individual fertility intentions, and thus their predictive value, have been questioned in a number of studies (16–18).
Because population-level measures are primarily assessed through cross-sectional, national household surveys, such as the National Survey of Family Growth, the Demographic and Health Surveys (DHS), and the Reproductive Health Surveys, pregnancy intendedness is based on female respondents’ retrospective, potentially biased recall of the planned status of the last or a recent pregnancy: Right before you became pregnant with your (nth, last) pregnancy … , Thinking back to just before you got pregnant with [name of child] … , or At the time you became pregnant with [name of child] … . Prospective studies assess women's future pregnancy intentions and their strength: Are you trying to get (or keep from getting) pregnant now? How important is avoiding a pregnancy to you? Furthermore, in most studies, pregnancy intendedness is dichotomized (intended/unintended, wanted/unwanted), despite recognition that it is a complex and nuanced concept. This dichotomization may be due to the limitations of data collection or measurement instruments, but it does raise questions about what is being missed in current analyses.
The desired timing of the next pregnancy is used to assess unintendedness. Generally, a pregnancy that follows a woman's report of not wanting any additional births is classified as “unwanted,” whereas one that happens before a desired point in time for her is “mistimed.” A pregnancy desired at the time is considered “wanted.” Some pregnancies to women who are unsure of their intendedness are classified as being of “unsure” or “ambivalent” status. Most studies reviewed here adopt a 3-level classification, with “unsure” combined with “wanted” intendedness.
Pregnancy-intention measures provide the denominator for unmet contraceptive-need measures in the developing world (19). The most widely used concept of unmet contraceptive need is a woman exposed to the risk of pregnancy and not currently using contraception who wants to space or limit future childbearing. The standard DHS definition for unmet need means that a woman 1) is married or in a consensual union, 2) is between the ages of 15 of 49 years, 3) is capable of becoming pregnant, 4) wants to have no more children or no children for at least 2 years, and 5) is using neither a traditional nor a modern method of contraception (20, 21). One obvious limitation of this definition is that unmarried women, and especially adolescents, may not be included.
Terminology and definitions in family planning research
Modern contraceptive methods can be categorized in several ways. Hormonal methods include such products as oral contraceptives, patches, vaginal rings, injectables, implants, and levonorgestrel intrauterine contraception. Nonhormonal methods include male and female condoms and other barrier methods, as well as copper intrauterine devices (IUDs). Implants and intrauterine contraception, and sometimes injectables, are also categorized as long-acting, reversible contraceptive methods. Surgical sterilization is a permanent method of family planning.
Contraceptive effectiveness is a measure of the success of typical use of a method. It incorporates efficacy, that is, how well a method works when used consistently and correctly, and a host of other factors, such as ease of compliance. Generally, long-acting, reversible methods and sterilization are the most effective (>99% protection against pregnancy over a year of use), with very low pregnancy rates among typical users that approach perfect-use rates. Once initiated, these methods are relatively user independent. Shorter-acting hormonal contraceptives are generally in the next tier of effectiveness. Included are such methods as pills, patches, and vaginal rings. These methods have high efficacy, but potential problems with compliance (missed doses, unreliable supply) result in higher real-world pregnancy rates. For example, the typical pregnancy rate for the combined oral contraceptive pill is 8% in the first year of use (22). Barrier methods are somewhat less effective (pregnancy rates of 15%–32%), followed by contraception that relies on timed intercourse, such as withdrawal or fertility-awareness methods.
Perhaps one of the best-measured reproductive behaviors, contraceptive practice has been assessed extensively at the population level for more than 4 decades by using the “contraceptive prevalence rate.” Technically, this is not a rate but a proportion—the percentage of exposed women reporting current use of any contraception, including male methods. Exposure involves being of reproductive age (15 years to 44 or 49 years) and sexually active or in a marital or stable union. Contraceptive “method mix” is also a measure of much interest because it is a proxy for method availability and client choice (23). It may reflect preferences of women or couples or it may reflect limits regarding supply or provider bias (24).
MATERIALS AND METHODS
Guided by the framework in Figure 1, we reviewed the recent research literature on the magnitude and strength of the relation between pregnancy intentions and reproductive, maternal, and newborn health outcomes first (Table 2) and then contraception. Table 3 summarizes studies of pregnancy intentions and contraception behaviors, and Table 4 includes studies of contraceptive behaviors and pregnancy outcomes, specifically the incidence of unintended pregnancy and elective pregnancy termination. Nearly all studies are observational and most cross-sectional, limiting the rigor of the evidence and the reliability of further synthesis.
Table 2.
Results From Key Studies of Fertility Intentions and Pregnancy and Maternal Outcomes
| Author(s), Year (Reference No.) | Study Location/Design/Year(s) | Study Population | Analytic Sample Size | Fertility Intention Measure | Definition | Confounders Controlled | Comparison Group(s) | Outcome(s) Assessed | Multivariate Analysis Resultsa | Summary of Findings |
| Pregnancy Outcomes | ||||||||||
| Afable-Munsuz and Braveman, 2008 (28) | California Maternal and Infant Health Assessment, pooled 5 rounds of cross-sectional survey data, 1999–2003 | Women with livebirths in February–May; California resident, English or Spanish speaking, aged ≥15 years; addresses on birth certificate | 15,331 women | “At the time you got pregnant, how did you feel about getting pregnant?” | “I wanted to get pregnant then” (intended), “I wanted to get pregnant later” (mistimed), “I didn't want to get pregnant then or in the future” (unwanted), and “I wasn't sure what I wanted” (unsure). | Family income, respondent's education, paternal education, age, parity, marital status, socioeconomic factors that affected preterm birth | Intended vs. unsure, mistimed, unwanted (4 groups) | Preterm birth (<37 weeks of gestation) | White: unsure, OR = 1.44 (95% CI: 1.08, 1.92); unwanted, OR = 1.31 (95% CI: 0.89, 1.91); mistimed, OR = 1.08 (95% CI: 0.83, 1.41). Immigrant Latina: unsure, OR = 1.49 (95% CI: 1.08, 2.06); unwanted, OR = 1.24 (95% CI: 0.87, 1.76), mistimed, OR = 1.03 (95% CI: 0.80, 1.34). No association among black or US-born Latina women. | Relation between pregnancy intention and preterm birth varies by women's racial or ethnic group. After adjustment for the socioeconomic and demographic variables, being unsure about pregnancy intention significantly elevated odds of preterm birth among immigrant Latinas but not among white, black, or US-born Latina women. |
| Keeton and Hayward, 2007 (29) | CDC (Atlanta, Georgia) PRAMS data, 1993–2001 | US federal/state cooperative questionnaire of women with a recent livebirth drawn from each state's birth certificate file | 47,956 women with singleton birth from 10 states | “Thinking back to just before you got pregnant, how did you feel about becoming pregnant?” | Unintended pregnancies: “I didn't want to be pregnant then or at any time in the future, or I wanted to be pregnant later.” Intended pregnancies: “I wanted to be pregnant sooner, or I wanted to be pregnant then.” | Maternal age, marital status, tobacco use, alcohol use, receipt of prenatal care in the first trimester, total number of prenatal care visits, medical complications of pregnancy (hypertension or diabetes), and birth history (a combination of parity and history of prior preterm or low birth weight births) | Intended vs. unintended | 1) Composite measure of VLBW (<1,500 g) and VPT birth (<32 weeks’ completed gestational age) and 2) admission to the NICU | Relative risk for intended pregnancy: VLBW/VPT, black: OR = 1.19 (95% CI: 1.02, 1.38); white: OR = 1.08 (95% CI: 0.92, 1.30). NICU admission, black: OR = 0.93 (95% CI: 0.81, 1.07); white: OR = 1.08 (95% CI: 0.96, 1.21). | Intended pregnancy at a young age was associated with higher risk of poor birth outcomes (VLBW/VPT and NICU admission) for both whites and blacks. Intended pregnancy was protective against NICU admission with advancing maternal age. |
| Mohllajee et al., 2007 (30) | CDC (Atlanta, Georgia) PRAMS data, 1996–1999 | US federal/state cooperative questionnaire of women with a recent livebirth drawn from each state's birth certificate file | 87,087 women who gave birth between 1996 and 1999 in 18 states | “Thinking back to just before you got pregnant, how did you feel about becoming pregnant?” | Unintended: mistimed (“I wanted to be pregnant later”), unwanted (“I didn't want to be pregnant then or at any time in the future”), or ambivalent (“I don't know”). Intended: “I wanted to be pregnant sooner” or “I wanted to be pregnant then.” | Maternal age, maternal race, maternal ethnicity, maternal education, marital status, parity, prenatal care, previous low birth weight infant or premature delivery, smoking during the pregnancy, drinking during the pregnancy, and previous low birth weight or preterm birth infant | Intended vs. ambivalent, mistimed, unwanted | Birth outcomes: low birth weight (<2,500 g), preterm delivery (<37 weeks), and small for gestational age (birth weight <10th percentile for the infant's gestational age based on race and parity) | Ambivalence: low birth weight, OR = 1.15 (95% CI: 1.02, 1.29). Mistimed: low birth weight, OR = 0.92 (95% CI: 0.86, 0.97). Unwanted: preterm delivery, OR = 1.16 (95% CI: 1.01, 1.33). No other associations found. | Women with unwanted pregnancies had an increased likelihood of preterm delivery and compared with women with intended pregnancies. Women who were ambivalent toward their pregnancies had increased odds of delivering a low birth weight infant; in contrast, women with mistimed pregnancies had a lower likelihood. |
| Maternal Outcomes | ||||||||||
| Hardee et al., 2004 (94) | Indonesia, cross-sectional survey data, 1996 | Random and quota sample of women aged 15–49 years with at least 1 child | 796 | Ever experienced unintended pregnancy | Subjective (respondent report) | Background characteristics associated in bivariate analysis with psychological well-being | Ever vs. never had an unintended pregnancy | Low, medium, and high measures of psychological well-being | For being in low (vs. high) psychological well-being: OR = 2.8 (95% CI: 1.5, 5.1; in medium (vs. high) psychological well-being: OR = 2.1 (95% CI: 1.2, 3.8). | Women with a prior unintended pregnancy were more likely to report lower measures of psychological well-being. |
| Cheng et al., 2009 (32) | Maryland PRAMS database (births in 2001–2006) | Random sample of postpartum mothers | 9,048 | “Thinking back to just before you got pregnant, how did you feel about becoming pregnant?” | Unintended: mistimed (“I wanted to be pregnant later”), unwanted (“I didn't want to be pregnant then or at any time in the future”). Intended: “I wanted to be pregnant sooner” or “I wanted to be pregnant then.” | Sociodemographic factors | Intended vs. mistimed and unwanted | Inadequate folic acid use, cigarette use, alcohol use, postpartum depression, postpartum contraceptive use, early prenatal care | Folic acid use: mistimed, OR = 2.17 (95% CI: 1.78, 2.64); unwanted, OR = 2.33 (95% 1.71, 3.19). Early prenatal care: mistimed, OR = 0.54 (95% CI: 0.44, 0.67); unwanted, OR = 0.34 (95% CI: 0.26, 0.45). Cigarette use (prenatal): unwanted, OR = 2.07 (95% CI: 1.47, 2.92); (postpartum): unwanted, OR = 1.86 (95% CI: 1.35, 2.55). Breastfeeding for >8 weeks: unwanted, OR = 0.74 (95% CI: 0.57, 0.97). Postpartum depression: mistimed, OR = 1.34 (95% CI: 1.08, 1.68); unwanted, OR = 1.98 (95% CI: 1.48, 2.64). | Unintended pregnancy had a statistically significant association with some negative prenatal care behaviors and with postpartum depression. |
| Mohllajee et al., 2007 (30) | CDC (Atlanta, Georgia) PRAMS data, 1996–1999 | US federal/state cooperative questionnaire of women with a recent livebirth drawn from each state's birth certificate file | 87,087 women who gave birth between 1996 and 1999 in 18 states | “Thinking back to just before you got pregnant, how did you feel about becoming pregnant?” | Unintended: mistimed (“I wanted to be pregnant later”), unwanted (“I didn't want to be pregnant then or at any time in the future”), or ambivalent (“I don't know”). Intended: “I wanted to be pregnant sooner” or “I wanted to be pregnant then.” | Maternal age, maternal race, maternal ethnicity, maternal education, marital status, parity, prenatal care, previous low birth weight infant or premature delivery, smoking during the pregnancy, and drinking during the pregnancy | Intended vs. ambivalent, mistimed, unwanted | Maternal outcomes: nausea, kidney or bladder infections, premature rupture of membranes, vaginal bleeding, diabetes, high blood pressure, and premature labor | No associations with pregnancy intention found by authors. Premature rupture of membranes: adjusted OR = 1.37 (unintended), adjusted OR = 1.03 (mistimed), adjusted OR = 1.06 (ambivalent) compared with intended. | All adjusted odds ratios for unintended, mistimed, and ambivalent were linearly related and greater than 1 (intended) but were not statistically significant. |
| Shapiro-Mendoza et al., 2007 (33) | 1990 Paraguay and 1994 Bolivia DHSs, 3-year retrospective survey data | Most recent births to women of reproductive age in the 3 years prior to surveys | 2,845 children <3 years of age in Bolivia and 1,837 children <3 years of age in Paraguay | “At the time you became pregnant with [name of last-born child], did you want to become pregnant then, did you want to wait until later, or did you want no more children at all?” | Intended: “I wanted to get pregnant then.” Mistimed: “I wanted to get pregnant later.” Unwanted: “I did not want any more children.” | Child's sex, maternal age, maternal education, mother's marital status, residence, currently working, presence/type of toilet facility, parity, currently pregnant, modern contraceptive user | Unwanted and mistimed vs. intended | Discontinued breastfeeding status at the time of the survey (or 36 months of age) | Unwanted vs. intended: Bolivia, OR = 0.87 (95% CI: 0.7, 1.0); Paraguay, OR = 0.90 (95% CI: 0.7, 1.2). Mistimed vs. intended: Bolivia, OR = 0.91 (95% CI: 0.8, 1.1); Paraguay: OR = 0.91 (95% CI: 0.8, 1.1). | Compared with intended pregnancies, unwanted and mistimed pregnancies were marginally associated with longer duration of breastfeeding in both Bolivia and Paraguay, but associations were not statistically significant; parity did not modify the association. |
Abbreviations: CDC, Centers for Disease Control and Prevention; CI, confidence interval; NICU, neonatal intensive care unit; OR, odds ratio; PRAMS, Pregnancy Risk Assessment Monitoring System; VLBW, very low birth weight; VPT, very preterm.
Unless otherwise indicated, adjusted odds ratios and 95% confidence intervals are presented.
Table 3.
Results From Key Studies of Fertility Intentions and Contraceptive Behaviors
| Author(s), Year (Reference No.) | Study Location/Design/Year(s) | Study Population | Analytic Sample Size | Fertility Intention Measure | Definition | Confounders Controlled | Comparison Group(s) | Contraceptive Outcome(s) Assessed | Multivariate Analysis Resultsa | Summary of Findings |
| Bartz et al., 2007 (34) | Moderately large US city, longitudinal, 2004 | Adolescent females recruited from 3 primary care adolescent clinics | 289 sexually experienced females in 2004 follow-up of the original cohort of 287 enrolled subjects | Trying to get pregnant, trying not to get pregnant, intensity of commitment, importance of partner's desire that she get pregnant | Yes or no answers to, Are you trying to get pregnant now? Are you trying to keep from getting pregnant now? Importance of not getting pregnant at this time in my life; importance of partner wanting her to get pregnant | Age, previous pregnancy; random intercept for person-specific correlations | “No” answer to intention measure; unimportance of commitment and partner's desire | Use of contraception at time of coitus, measured 3 months later | Trying to get pregnant: OR = 0.17 (95% CI: 0.12, 0.23); trying not to get pregnant: OR = 7.84 (95% CI: 6.36, 9.68); committed to not getting pregnant, OR = 9.12 (95% CI: 6.75, 12.30); partner wants me to get pregnant, OR = 0.46 (95% CI: 0.35, 0.61) | Half of coital events for adolescent females committed to not getting pregnant were unprotected. Contraceptive protection during sex was significantly associated with intention to avoid getting pregnant. |
| O'Rourke et al., 2008 (35) | United States, cross-sectional, 2003–2004 | US Army recruits at Fort Bliss, Texas, and Fort Gordon, Georgia | 1,095 male and female first-term soldiers, sexually active but not pregnant or an expectant father | Pregnancy intention | PRAMS-based multidimensional assessment codes: 1 = plan a baby in the next 6 months, 2 = ambivalent (don't know), 3 = no intent in the next 6 months, 4 = no intent ever | Gender, age, education, ethnicity, binge drinking in the past month | Other levels of pregnancy intention score | Contraceptive efficacy (highest level of birth control used at last sexual intercourse) | Pregnancy nonintention score (1–4); adjusted OR = 1.14 (95% CI: 1.09, 1.20) with each unit increase in pregnancy intention score | On the basis of multivariate ordinal regression analysis of 845 men and women, pregnancy/paternity intention was found to be significantly associated with choice of efficacious contraceptive method. One-third of the population attempting to avoid pregnancy used no birth control at the last sexual intercourse. |
| Frost and Darroch, 2008 (36) | United States, cross-sectional telephone survey, 2004 | Nationally representative sample of 1,978 women aged 18–44 years | 1,641 women using reversible contraception at risk of unintended pregnancy (heterosexually active in the past year, not pregnant, up to 2 months postpartum, trying to become pregnant, and not sterile for either contraceptive or noncontraceptive reasons) | 1) Number of unintended pregnancies, 2) importance of avoiding pregnancy | 1) Number of unintended pregnancies ever experienced, 2) how important it is to avoid pregnancy (very, somewhat, a little/not important) | Parity, fatalistic attitude about contraception, reason for method use, would change method if cost was not an issue, type of provider | 1) 0 unintended pregnancies, 2) very important | Specific use of a reversible method: pill, long acting (injectable, patch, IUD, ring, and implant), condom, and other (withdrawal, periodic abstinence, spermicides, and other barrier) | ≥1 unintended pregnancies(vs. 0): pill = 0.73, P < 0.05 (standard error not reported); long acting = 2.10, P < 0.001; condom = 0.66, P < 0.01. Somewhat (vs. very) important: pill = 0.96, not significant/long acting = 0.91, not significant/condom = 0.83, not significant/other = 2.01, P < 0.001; a little/not (vs. very) important: pill = 0.38, P < 0.001/long acting = 0.77, not significant/condom = 1.14, not significant/other = 4.42, P < 0.001 | Women experiencing ≥1 unintended pregnancies had higher odds (2.1) of using long-acting methods and reduced odds for pill and condom use (0.7). Women reporting little or no importance about avoiding pregnancy had reduced odds of using the pill (0.4) and elevated odds of using other methods such as rhythm or withdrawal (2.6). |
| Wu et al., 2008 (5) | United States, NSFG 2002, retrospective survey data on contraceptive use | Nationally representative sample of 7,643 women aged 15–44 years | 3,687 women at risk of unintended pregnancy (heterosexually active in the past year, not pregnant, trying to become pregnant, and they or their partner not sterile or do not suspect being sterile | Wants a baby in the future | Yes answer to, Do you want a (another) baby some time in the future? | Age, race/ethnicity, education, parity, insurance coverage, number of sexual partners, months of sexual activity | No (another baby not wanted) | Consistent use (use of contraception in the past year during all months at risk of pregnancy), inconsistent use (use of contraception in the past year during some months when at risk of pregnancy), nonuse (no use of contraception during all months of pregnancy risk) | Multinomial logistic adjusted relative risk ratio with consistent use as the reference outcome: nonuse = 1.1 (95% CI: 0.8, 1.7), inconsistent use = 1.2 (95% CI: 0.88, 1.7) | 10% of women at risk of an unplanned pregnancy persistently did not use birth control over a 1-year period. No significant association was found between future pregnancy intentions and contraceptive behavior. |
| Vaughn et al., 2008 (37) | United States, NSFG 2002, retrospective survey data on contraceptive use | Nationally representative sample of 7,643 women aged 15–44 years | 7,106 episodes of use | Wants no more children | Yes answer | Nulliparous, married or cohabiting, previous method used is hormonal, previous method failed, covered by private insurance | Wants more children | Resumption of contraceptive use within 12 months after discontinuation | Cox proportional hazards model adjusted hazard ratio and 95% CI; wants no more children = 1.10 (95% CI: 1.04, 1.67) | Women wanting no more children have a higher probability of resuming contraceptive use within 12 months of discontinuation (1.10) than those wanting more children. |
Abbreviations: CI, confidence interval; IUD, intrauterine device; NSFG, National Survey of Family Growth; OR, odds ratio; PRAMS, Pregnancy Risk Assessment Monitoring System.
Unless otherwise indicated, adjusted odds ratios and 95% confidence intervals are presented.
Table 4.
Results From Key Studies of Contraceptive Behaviors and Fertility Outcomes
| Author(s), Year (Reference No.) | Study Location/Design/Year(s) | Study Population | Analytic Sample Size | Contraceptive Behavior Measure | Definition | Confounders Controlled | Comparison Group(s) | Fertility Outcome(s) Assessed | Multivariate Analysis Resultsa | Summary of Findings |
| Barden-O'Fallon et al., 2008 (38) | Guatemala, retrospective birth and contraceptive use history covering 1999–2002 | Pregnancies to reproductive-aged women in the 3 years prior to survey | 5,400 pregnancies to 4,118 women aged 15–49 years | Contraceptive discontinuation any time in the 12 months preceding livebirth | No method use reported after at least 1 month (episode) of use | Residence, age, education, religion, indigenous ethnicity, household socioeconomic status, parity, currently pregnant; survey clustering | Discontinued for wanted pregnancy; discontinued for other reason | Whether pregnancy was wanted at that time, wanted later (mistimed), or not wanted at all (unwanted) | Multinomial logistic adjusted relative risk ratios; mistimed vs. intended: nonuser = 3.94 (95% CI: 3.03, 5.10), discontinued for other reason = 8.58 (95% CI: 6.55,11.25); unwanted vs. intended: nonuser = 6.17 (95% CI: 4.39, 8.67), discontinued for other reason = 9.78 (95% CI: 10.07, 21.12) | Discontinuation for reasons other than pregnancy carries a higher and statistically significant relative risk of being reported as mistimed or unwanted than intended pregnancy. Nonuse in the year prior to pregnancy carries a higher relative risk of leading to a mistimed or unwanted than an intended pregnancy. |
| Sedgh et al., 2006 (43) | Nigeria (8 states), cross-sectional household survey in 2002–2003, weighted to population levels | 3,020 women aged 15–49 years systematically sampled from households in enumeration areas in 1 urban and 1 rural local government area in each state | 2,978 women | Ever used contraception | Used a modern method; used a traditional method only; never used | Age, marital status, parity, education, socioeconomic status, religion, residence, region | Never used | Had an unwanted pregnancy | Traditional only = 2.62, P < 0.001 (no standard error reported); modern = 3.86, P < 0.001 | Women who ever used a modern or traditional method have higher odds (3.9 and 2.6, respectively) of experiencing an unwanted pregnancy than those who never used. |
| Frank-Hermann et al., 2007 (40) | Germany, observational prospective cohort study | 1,599 women using the symptothermal method enrolled in 1985–2005 | 900 women with 17,638 cycles motivated to avoid pregnancy, starting to use the symptothermal method, and using only this or a barrier method, aged 19–46 years, with an average cycle length of 22–35 days, no previous history of infertility, ovulating, contributing at least 12 cycles of data | Protected intercourse (with barrier method) | Abstinence in the fertile period, protected intercourse in the fertile period, unprotected intercourse in the fertile period | None | Abstinent; unprotected intercourse | Rates of unintended pregnancies per 100 women | Descriptive: rates and 95% CIs; protected = 0.59% (95% CI: 0.07, 2.13), abstinence = 0.43% (95% CI: 0.05, 1.55), unprotected = 7.46% (95% CI: 4.15, 10.23) | The effectiveness of using the symptothermal method is comparable to abstinence practice and is superior to unprotected intercourse. |
| Kuroki et al., 2008 (42) | United States (Rhode Island), randomized clinical trial of dual protection intervention, 1999–2003 | 542 clients attending primary care, gynecology, and family planning clinics; aged 14–35 years; English speaking | 542 women, of 1,112 screened, consenting to the trial (both arms combined) | Using a hormonal contraceptive at baseline | Reported use of hormonal contraception at baseline | History of unplanned pregnancy, age, race/ethnicity, education, annual household income, parity, number of sexual partners in the past month, coping score, intervention arm | Not using a hormonal contraceptive | Incident unplanned pregnancy | 0.69 (95% CI: 0.41, 1.14) | Previous unplanned pregnancy is significantly associated with a subsequent unplanned pregnancy. Use of hormonal contraception at baseline lowers the incidence of unplanned pregnancy (adjusted odds = 0.69) but is not statistically significant. |
| Shlay et al., 2009 (44) | United States (Denver, Colorado), analysis of medical records for STD clinic clients, 2003–2006 | Medical records for 5,478 women seen at the Denver Metro Health Clinic | 642 women aged 12–44 years provided with contraception at the initial STD clinic visit, no intention to become pregnant, complete baseline and follow-up pregnancy history information, not pregnant at the initial visit, seen at least twice during the study period | Did not use birth control at the last sexual encounter; effective birth control provided at the initial visit | Whether any birth control was used at the last sexual encounter; received a 3-month supply of contraception free of charge | Age, race, poverty level, number of previous pregnancies, any history of abortion, education, first pregnancy before age 17 years, number of sexual partners in the past month, frequency of sexual encounters over the past 4 months | Used birth control at the last sexual encounter; not provided with birth control at the first visit | Incident unintended pregnancy | Did not use birth control = 1.67 (95% CI: 1.11, 2.52); received birth control at the initial visit = 1.03 (95% CI: 0.68, 1.58) | Nonuse of birth control at the last sexual encounter significantly increases the odds of unintended pregnancy (odds = 1.67). Receiving birth control at the initial clinic visit is not statistically significantly associated with odds of incident pregnancy. |
| Goldsmith et al., 2008 (41) | Oregon 2001 PRAMS survey data, cross-sectional analysis | US federal/state cooperative questionnaire of women with a recent livebirth drawn from each state's birth certificate file | 1,795 women (of 2,490) who gave birth in 2001 and completed and returned the survey | Prepregnancy knowledge of emergency contraception | Before you got pregnant … had you ever read or heard about emergency birth control (the “morning-after” pill)? | Maternal age, maternal race/ethnicity, maternal education, marital status, family income, prepregnancy insurance coverage | Yes, know of emergency contraception | Unintended birth (either mistimed or unwanted) vs. intended birth | Don't know; emergency contraception = 1.43 (95% CI: 1.0, 2.1) | Oregon women unaware of emergency contraception before pregnancy have higher odds of having an unintended birth than women who know. |
| Bradley et al., 2009 (39) | Kenya 2003, Zimbabwe 2005, Armenia 2005, Egypt 2005, Bangladesh 2004, Indonesia 2002, Colombia 2005, Dominican Republic 2002; multilevel hazard regression analysis of calendar data on contraceptive use and pregnancy events | Use episodes for women aged 15–49 years using reversible contraception in the 5 years before survey | Kenya = 2,597, Zimbabwe = 4,692, Armenia = 2,386, Egypt = 15,025, Bangladesh = 10,359, Indonesia = 17,563, Colombia = 20,714, Dominican Republic = 11,935 | Type of method used | Traditional, pill, injectable, condom, IUD, and other modern method | Age and parity at discontinuation, worked in the past year, years of education, aware of contraception, partner's desired fertility, media exposure, community-level contraceptive prevalence rate, residence, wealth status, region, interval of use, and cluster-level variance | Each modern method vs. traditional method | Contraceptive failure (accidental pregnancy while using method) | Range for adjusted hazard ratios: pill, 0.19 in Zimbabwe to 1.24 in Indonesia; injectable, 0.05 in Bangladesh to 0.42 in Colombia; condom, 0.22 in the Dominican Republic to 0.94 in Indonesia; IUD, 0.04 in Egypt to 0.26 in Indonesia; other: modern, 0.03 in Bangladesh to 0.71 in Colombia | Compared with traditional method use, in general, use of modern contraceptives, particularly the IUD and injectable methods, is significantly associated with lower odds of accidental pregnancy. |
| Goodman et al., 2008 (45) | Northern California, case-control, 2002–2005 | Aspiration abortion clients at 8 northern California Planned Parenthood clinics over a 3-year period | 2,019: 673 cases and 1,346 controls | Immediate postabortal insertion of IUD | Same-day postabortal insertion of IUD | Cases matched on date of abortion; multivariate hazards model controlled for woman's age, marital status, race/ethnicity, family size | Controls who accepted non-IUD contraception; women who declined contraception or received emergency contraception only excluded from controls | Rates of repeat abortion per 1,000 woman-years in the first year following the index abortion and in the entire follow-up period (at the agency clinic) | Hazard ratio = 0.37 (95% CI: 0.26, 0.52), P < 0.001 | 6.1% of postabortal IUD insertion cases had a repeat abortion compared with 15.3% of controls; repeat abortion rates = 34.6 (95% CI: 24.8, 47.0) and 91.3 (95% CI: 79.4, 104.9), respectively, per 1,000 woman-years (P < 0.001). Immediate postabortion IUD contraception significantly reduces repeat abortion incidence. |
| Regushevskaya et al., 2009 (46) | St. Petersburg, Russia; cross-sectional data; 2003–2004 | Women aged 18–44 years in 2 districts who consented to participate in an in-clinic survey of reproductive health and reproductive health services | 1,147 participants (67% of 1,718 reachable by phone of the 2,501 contacted by mail) | Reliability of contraceptive method at last intercourse | What kind of contraceptive method did you use at your last sexual intercourse? Reliable = IUD, pill, condom; unreliable = calendar, spermicide, emergency contraception, withdrawal, or douching (no reported use of injectable, implant, patch, or ring) | Age, marital status, education, employment, personal income, parity, age at first intercourse, use of contraception at first intercourse | Reliable method used | Had 2 or more abortions | Unreliable: 1.83 (95% CI: 1.28, 2.62); no method: 1.71 (95% CI: 1.23, 2.38) | Nearly 60% of women at risk of unintended pregnancy used reliable contraception at the last intercourse; 31% used an unreliable method. Odds of having ≥2 abortions were significantly elevated if unreliable or no contraception was used. |
Abbreviations: CI, confidence interval; IUD, intrauterine device; OR, odds ratio; PRAMS, Pregnancy Risk Assessment Monitoring System; STD, sexually transmitted disease.
Unless otherwise indicated, adjusted odds ratios and 95% confidence intervals are presented.
To investigate the association of pregnancy intentions with birth and maternal outcomes, we conducted an initial search by using the PubMed and Embase databases. The initial search included the terms ((pregnancy intention) OR (unplanned pregnancy) OR (unintended childbearing) OR (unintended fertility) OR (unwanted pregnancy)). Searches for studies on birth outcomes were identified by using the search terms (birth outcome OR neonatal outcome OR prematurity OR preterm birth OR low birth weight) OR (maternal outcome OR maternal health OR maternal morbidity OR maternal mortality). These searches were then combined. Abstracts of retrieved results were then reviewed to identify relevant articles. We also reviewed bibliographies from selected articles to aid with complete review. Given previously published reviews of a related nature (25, 26), we limited searches to articles published in English in 2004 or later. We also limited our review to studies that were prospective or longitudinal, were population based, and included multivariate analyses.
To evaluate recent studies of the relation between pregnancy intentions and contraceptive use, we conducted a second search of the PubMed and Embase databases with the search terms (“pregnancy, unplanned”[MeSH Terms] OR (“pregnancy”[All Fields] AND “unplanned”[All Fields]) OR “unplanned pregnancy”[All Fields] OR (“unintended”[All Fields] AND “pregnancy”[All Fields]) OR “unintended pregnancy”[All Fields]) AND (“contraception”[MeSH Terms] OR “contraception”[All Fields]). Between 2004 and 2009, 256 English-language studies were published. Abstracts of retrieved results were reviewed to identify eligible studies. We again limited our review to studies that were prospective or longitudinal, were population based, and included multivariate analyses.
RESULTS OF INDIVIDUAL-LEVEL STUDIES
Pregnancy intentions and birth outcomes
Rigorous research on the relation between pregnancy intentions and pregnancy outcomes is limited. What has been published generally focuses on short-term neonatal outcomes, such as prematurity. Many of the studies are older and are methodologically limited. A recent systematic review (27) concluded that unintended pregnancies, compared with intended pregnancies, were associated with higher odds of such neonatal outcomes as low birth weight (odds ratio (OR) = 1.36, 95% CI: 1.25, 1.48) and preterm birth (OR = 1.31, 95% CI: 1.09, 1.58). However, because of heterogeneity among studies—some studies adjusted for potential confounding variables such as race, maternal age, and prior low birth weight, while other studies did not present adjusted results—the authors chose to incorporate only unadjusted odds ratios so as to include as many of these studies as they could. Findings from previously published studies are inconsistent, with some showing a negative influence of intendedness on neonatal outcomes and others showing no difference (25). Much of the available literature is from developed countries.
We identified 3 studies, all in the United States, that included multivariable analyses of population-based data, and one prospective survey. “Birth outcomes” were primarily preterm birth and low birth weight, although the definitions of these outcomes varied somewhat across studies. The results are inconclusive. Two studies found that associations between unintended pregnancy and birth outcomes varied by race or ethnicity, with black women and Latinas having increased odds of negative outcomes if the pregnancy was unintended versus intended (28, 29). A third study (30) found higher odds of low birth weight if the pregnancy was unwanted (vs. wanted; adjusted OR = 1.16, 95% CI: 1.01, 1.33). These 3 studies assessed pregnancy intentions retrospectively, and all used a similar question to do so (Table 2). Results on fertility intentions and birth outcomes for developing countries are more difficult to find. A World Health Organization report analyzed DHS data from 5 developing countries (Bolivia, Egypt, Kenya, Peru, and the Philippines). The authors concluded that the effects of unintendedness on the child's subsequent immunization status and growth were inconsistent across countries (31).
Pregnancy intentions and maternal behaviors and health outcomes
Research findings on fertility intentions’ effects on maternal behaviors and health outcomes are even sparser than for pregnancy outcomes. We identified 4 studies that met our search criteria (Table 2). The strength of our review is limited by the different maternal outcomes selected by each group of authors, ranging from antepartum behaviors such as smoking, to pregnancy complications such as hypertension, to postpartum depression and breastfeeding. One study (30) found no association between pregnancy intention and maternal outcomes, while another (32) found unintendedness associated with decreased odds of early prenatal care (vs. intended: adjusted OR = 0.54 for mistimed and OR = 0.34 for unwanted) and significantly increased odds of postpartum depression (adjusted OR = 1.34 and OR = 1.98, respectively). Shapiro-Mendoza et al. (33) found that, compared with intended pregnancies, unwanted and mistimed pregnancies were marginally, but not significantly associated with longer durations of breastfeeding of infants born in the 3 years prior to the 1990 Paraguay and 1994 Bolivia DHSs (adjusted hazard ratio = 0.90, 95% CI: 0.7, 1.2 and adjusted hazard ratio = 0.87, 95% CI: 0.7, 1.0, respectively). What most of these studies have in common is their focus on immediate outcomes. Data on long-term maternal or child outcomes are lacking.
Pregnancy intentions and contraceptive use
Five studies meeting our inclusion criteria were identified (Table 3), all of which were US based. Only one used a prospective cohort design following up adolescent clinic patients, whereas another analyzed survey data on recruits at 2 US Army bases. The remaining 3 relied on data from a nationally representative telephone survey or the 2002 National Survey of Family Growth. Assessed contraceptive behaviors ranged from use at last sex, to consistent use, to resumed use following discontinuation, to type of method used. Fertility intentions were assessed in terms of wanting another pregnancy in the future, number of unintended pregnancies, and importance of avoiding a future pregnancy.
A number of studies reported a high percentage of women who did not intend to become pregnant but did not use contraception (5, 34, 35). On the other hand, adolescent clients committed to not becoming pregnant had higher odds of using contraception 3 months later (adjusted OR = 9.12, 95% CI: 7.75, 12.30), and US Army recruits, irrespective of gender, not intending to have a baby in the next 6 months had higher odds of using an efficacious contraceptive method (adjusted OR = 1.14, 95% CI: 1.09, 1.20). Women who had experienced 1 or more unintended pregnancies had notably higher odds (2.1 times) of using long-acting methods compared with those with no such pregnancies and reduced odds (OR = 0.7) of using the pill or condom (36). Somewhat surprisingly, with 2002 National Survey of Family Growth data, Wu et al. (5) found no association between wanting to avoid a pregnancy in the future and consistent use of contraception during months at risk in the past year. However, Vaughn et al. (37), with the same data, found that the probability of resuming contraceptive use among women who achieved their desired family size was significantly higher than for those discontinuing use when more children were wanted (adjusted hazard ratio = 1.10, 95% CI: 1.04, 1.67). These empirical analyses suggest that intentions to avoid pregnancy are associated with the use of contraception, but far from perfectly.
Contraceptive behaviors and fertility outcomes
Another set of studies examined the association of contraceptive behaviors with subsequent pregnancy outcomes. Nine studies published since 2004 met our inclusion criteria, 7 of which focused on the incidence of unintended pregnancy (38–44) and 2 (45, 46) on repeat abortion as outcomes (Table 4). Of the studies, 4 were US-state based (Rhode Island, Colorado, Oregon, and California), while the others were conducted in international settings. Heterogeneity in study design across studies limited our synthesizing the findings in a concise way. Contraceptive behaviors of interest range from general types of methods used, to specific use of symptom-thermal or hormonal methods, to prepregnancy knowledge of emergency contraception.
The studies located in developing countries utilized contraceptive calendar data and related respondent use patterns to the subsequent incidence of unintended pregnancy. A Guatemalan study (38) examined the influence of women's contraceptive discontinuation on unintended pregnancy, finding that those who used contraception but discontinued for a reason other than a desired pregnancy had a high relative risk ratio of 14.58 (95% CI: 10.07, 21.12) of having an unwanted (vs. intended) pregnancy. Those who did not use contraception also had a higher relative risk ratio of 3.94 (95% CI: 3.03, 5.10) of having a mistimed pregnancy and a relative risk ratio of 6.17 (95% CI: 4.39, 8.67) of having an unwanted pregnancy.
A Nigerian study (43) found that women who have ever used traditional or modern contraceptives have higher odds of experiencing an unwanted pregnancy than those who never used them. An extensive comparative analysis of 8 countries (39) assessed contraceptive failure rates for different reversible contraceptive methods. Adjusting for potential confounders, the authors found the probability of an accidental pregnancy among contraceptive pill users to range from 0.19 in Zimbabwe to 1.24 in Indonesia, from 0.05 for injectable users in Bangladesh to 0.42 in Colombia, and for IUD users from 0.04 in Egypt to 0.26 in Indonesia. These results, of which most are statistically significant at P < 0.01, are akin to typical-use failure rates found for modern reversible contraceptives.
Three US-state-based studies (41, 42, 44) similarly demonstrated that some contraceptive use or knowledge is advantageous in comparison to nonuse in reducing the incidence of unplanned pregnancy, but the measured protection is not as high as one might expect. For example, in the Colorado study, women having unprotected sex, compared with those using birth control, had an adjusted odds ratio of 1.67 (95% CI: 1.11, 2.52) of having an unintended pregnancy within a 3-year follow-up period. The magnitude of the adjusted odds ratio value, although statistically significant, is not substantial considering what should be a higher efficacy level from contraceptive protection.
Two studies on contraception and repeat abortion incidence (45, 46) showed that reliable contraception is significantly associated with reduced odds of repeat abortion. In Goodman et al.’s study (45), 6.1% of postabortion IUD insertion cases had repeat abortions compared with 15.3% of controls; the adjusted hazard ratio was 0.37 (95% CI: 0.26, 0.52). Although only 60% of participants at risk of unintended pregnancy in the St. Petersburg study (46) used reliable contraception at last sex, the odds of having 2 or more abortions was significantly higher for those using unreliable methods or no protection.
RESULTS OF POPULATION-LEVEL STUDIES
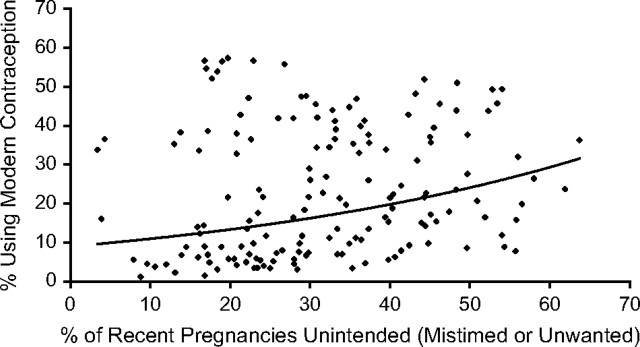
Contraception benefits for reproductive health
Demographers have long studied the relation between family planning and fertility at the population level and have drawn implications about satisfying contraceptive need on fertility, abortion, and mortality rates in the developing world. In this section, we review study findings from cross-national survey analyses that project the impact of lowering unintended pregnancy on reproductive and child health outcomes. As background, we use the StatCompiler tool (47) to compile DHS-based national estimates of the proportion of pregnancies that are unintended, either mistimed or unwanted, and the proportion of women of reproductive age using modern contraception. Figure 2 shows that the values from 158 DHSs conducted in 68 African, Asian, Latin American, and Caribbean countries between 1991 and 2007 do not closely fit either a linear or curvilinear trend because levels of unintended pregnancy tend to be higher than use of effective contraception. In fact, the relatively flat, curvilinear, and positive trend line suggests that unintended pregnancy levels rise, rather than fall, with modern birth control use. Only a few country data points show high use and low levels of unintendedness.
Figure 2.
Relation between national rates of unintended pregnancy and modern contraceptive prevalence among women aged 15–49 years across 158 Demographic and Health Surveys in developing countries, 1991–2007 (47).
Reasons for this apparent contradiction may vary from country to country. It is worth recalling that the definition of “contraceptive prevalence” does not presume correct and consistent use. For example, reported prevalence of condoms may not account for the often sporadic nature of their use. Similarly, high rates of contraceptive discontinuation (also not captured in the contraceptive prevalence rate) could counteract the potential impact of contraceptive use on unintended pregnancies. There may also be supply-side determinants of contraceptive use, such as availability of method choice or restricted access, that contribute to high unintended pregnancy rates. Women may be better able to articulate an unintended pregnancy than they are to avail themselves of and practice the means to prevent one with contraception.
Coitus, conception, infection, and contraception
The scale of sexual activity, reproduction, and their potential risks at the population level are challenging to visualize. With a majority of the 1.74 billion reproductive-age females being sexually active and a probability of conception during unprotected coition of 3 in 100 (11), each year as many as 720 million conceptions may occur. The majority of conceptions (60%–70%) will be spontaneously miscarried, leaving approximately 239 million identified pregnancies, of which 136.2 million will progress to livebirths, 33 million being unwanted. Another 46 million pregnancies will be electively terminated.
The Guttmacher Institute (14) estimates a pregnancy rate of 137 per 1,000 women aged 15–44 years in the developing world and an unintended pregnancy rate of 57 per 1,000, or 82.3 million mistimed or unwanted pregnancies. The unintended pregnancy rate has declined since the mid-1990s, largely because of increases in contraceptive use, proportionately faster in the developed than the developing world.
Preventing sexually transmitted infection and HIV transmission, as well as unplanned pregnancies, during coition is a priority in many low-income countries. HIV research has only recently acknowledged the importance of integrating family planning into HIV prevention and care programs. For HIV-positive women who seek to postpone or delay a pregnancy, family planning is a proven and cost-effective method for preventing mother-to-child transmission of HIV (48). A study of 14 developing countries (49) reports that, for 1.342 million HIV-positive women in need of perinatal HIV prevention, a potential 71,945 infant HIV infections and 423,211 births can be averted through increased family planning use. As the client load in need of HIV diagnosis and antiretroviral therapy increases, the financial and service burden for programs to meet that demand elevates the importance of responding to clients interested in spacing and limiting childbearing (50, 51). It is estimated that family planning can avert as many or more vertical pediatric infections and HIV deaths as scaling up antiretroviral efforts to prevent mother-to-child transmission (52).
Contraception, conception, and parturition
While safe, legal induced abortion has few health consequences for the woman, the need for abortion is an indication of unintended pregnancy. Although abortion rates are similar across developed and developing regions, many abortions that take place in the latter areas are unsafe (53, 54). Two-thirds of pregnancies in the developing world occur to women not using contraception (55). If contraception can reduce the incidence of unintended pregnancies, it will lower the risk of death and disability due to unsafe abortions. In Uganda, for example, current use of contraception, compared with no contraceptive use at all, has resulted in 150,000 fewer abortions (56). Meeting the existing level of 41% unmet need there would further reduce this number. In Guatemala, where 32% of pregnancies are unintended and abortion is illegal, 12% of pregnancies end in induced abortion. Eight of 1,000 women of reproductive age were hospitalized in 2003 because of complications of unsafe abortion, a figure that may well underestimate the magnitude of the problem. The relatively low prevalence of modern contraceptives (43%) and high unmet need (28%) are acknowledged to contribute to abortions and related morbidity (57).
Often, however, ineffective contraceptive use, rather than nonuse, contributes to unintended pregnancy: for many eastern European and south Asian countries, as many as two-thirds of abortions are due to contraceptive failure, mostly from traditional method use, and one-third are due to unmet need for contraception (58). In developed countries, it has been reported that most abortions occur as a result of contraceptive failure and a small proportion are due to nonuse of contraception. One study found that 84% of women seeking abortion reported recent contraceptive use about the time they conceived, compared with 16% reporting nonuse (59).
Increased contraceptive uptake is generally associated with reduced numbers of abortions. Since 1995, abortion rates have decreased worldwide. The greatest declines are in eastern Europe, concurrent with an increase in access to modern contraceptive methods (60). Westoff's (58) analysis of contraceptive use and abortion rates for 12 eastern European and south Asian countries shows a strong negative correlation between prevalence of contraceptive methods and abortion rates. That is, with some exceptions, countries with the highest uptake of modern contraceptive methods generally also have the lowest abortion rates. Westoff (58) estimates that, if unmet need in those countries were reduced to zero and traditional contraceptive methods were replaced by modern ones, the number of induced abortions would be lowered by 55%. Satisfying unmet need results in an average 23% reduction in abortions.
Contraception in relation to gestation and birth intervals
Elevated risks of neonatal, infant, and child mortality and of child malnutrition were statistically linked to short birth intervals (less than 30 months) in an analysis of DHS data from 17 developing countries (61). The adjusted odds of neonatal, infant, and under-age-5-years child deaths were 1.67, 1.85, and 1.91 times significantly higher if the birth interval was 18–23 months compared with 36–47 months. Conde-Agudelo et al. (62) found, with Latin American data, greater risk of preterm, low birth weight, and small-for-gestational-age infants associated with short interpregnancy intervals of less than 6 months compared with 18–23 months. In terms of maternal health, 2 studies (63, 64) reported higher risks of premature rupture of membranes, preeclampsia, high blood pressure, and anemia with interpregnancy intervals of less than 6 months in Latin America (in comparison to 18–23–month intervals) and Bangladesh (in comparison to 27–50–month intervals).
The interval between pregnancies is an important window during which contraceptive benefits for maternal health can be experienced. Although the empirical evidence on birth spacing and maternal and newborn outcomes is strong, that for contraceptive use between pregnancies is weak (65). Contraception's benefits need to be empirically differentiated from those of lactation and other protective behaviors in the birth interval. Since breastfeeding can extend over many months, particularly in sub-Saharan African countries, overlap with contraceptive use confounds estimates of the latter's effects. One multicountry analysis of pregnancy outcomes found that 12 months of contraception-only coverage in the preceding birth interval can reduce the mortality risk for the next newborn by 31.2%, while 12 months of contraceptive use overlapping with breastfeeding reduces the risk by 68.4% (66). This same study of DHS data for 19 developing countries found an average of 3–4 months of contraceptive use overlapping with breastfeeding.
Family-planning-averted births and maternal morbidity and mortality
Liu et al. (67) estimated that nearly 230 million births are averted annually by global contraceptive use, or 1.7 times the current number of livebirths. Averted births and pregnancies reduce the size of the denominator of maternal and infant mortality rates. Although it is difficult to attribute change in the maternal mortality ratio to a particular cause, evidence exists that meeting the need for family planning can reduce maternal mortality. An analysis of DHS data indicated a strong negative correlation between maternal mortality ratios and contraceptive prevalence rates (49). Another study (68) estimated that, without contraception, the number of maternal deaths would be 19% higher. A recent Guttmacher Institute study (14) found that fulfilling unmet contraceptive need can prevent an additional 150,000 maternal deaths annually; a study in rural Bangladesh (69) found that, between 1979 and 2005, the fertility decline was responsible for a 30% reduction in maternal deaths. In Uganda, even with substantial unmet need for contraception, current use of contraception has resulted in 490,000 fewer maternal deaths compared with no contraceptive use (56). Similarly, Egypt's maternal mortality ratio was reduced 50% between 1992 and 2000, a development concurrent with increased uptake of family planning and other maternal health improvements (70). Stover and Ross’ (71) recent analysis suggested that declines in total fertility rates between 1990 and 2005 in developing countries, attributable to contraceptive use, likely averted 1.2 million maternal deaths.
Contraceptive use in particular may also disproportionately impact women's risk of maternal mortality at either end of the reproductive age span. Adolescence and older reproductive age elevate maternal mortality risk, as does parity greater than 4 births (31). Providing contraceptive services to these groups can reduce the maternal mortality ratio by as much as 58% (55).
For every maternal death, as many as 30 more women may suffer disability or injury due to complications from pregnancy, childbirth, or abortion (72). Levine et al. (73) estimated that unwanted fertility and unsafe abortion account for 12%–30% of maternal disability-adjusted life years across the developing regions of the world. As many as 1.27 million years of life are lost and another 0.76 million years of life with disability are due to this maternal burden of disease in sub-Saharan Africa alone. The global disease burden associated with unmet family planning need among reproductive-aged women is one of the greatest contributors to disability-adjusted life years in the developing world, accounting for 7.4 million disability-adjusted life years among women aged 15–44 years, according to 2006 estimates (74). This issue trumps other risk factors such as anemia (4.7 million disability-adjusted life years) and smoking (1.6 million). Anemia itself is often due to pregnancy, which suggests that the all-cause burden of unmet need is even higher.
Maternal disability is also due to complications of unsafe abortion and childbirth, such as prolonged or obstructed labor resulting in vesicovaginal fistula. A recent prospective study evaluated morbidity in Mombasa, Kenya, among women in the first year postpartum. The authors observed a 50% incidence of anemia, an 11% incidence of HIV, and 39% with an unmet need for family planning (75). The same authors previously found that postpartum morbidity among HIV-positive women was higher in uninfected women (76). In Kenya, where 44% of births are unplanned (77) and contraceptive prevalence is 39%, it is logical to assert that those postpartum women who delivered children from an unintended pregnancy, due to unmet need for family planning, suffered unnecessary and completely preventable disability.
A Mexican study evaluating the impact of family planning on maternal morbidity (78) used historical data and generated comparisons between the current standard of care there and a model in which World Health Organization benchmarks for care would be met (Mother-Baby Package). The study concluded that increasing family planning prevalence from 59% to 74% among women older than age 20 years and from 18% to 33% among women younger than age 20 years (both Mother-Baby Package goals) would avert 1,324 disability events per 100,000 women annually—a 32% reduction compared with the current level of 4,149 disabling events.
Although high-quality published evidence is limited, the conclusions are consistent at the population level. Optimization of family planning can prevent maternal disability. Beyond physical disability, one study suggests that unintended pregnancy can adversely impact women's quality of life, with 94% of those surveyed saying they would experience negative health effects. In the same study, 16% of women also stated they would accept an “immediate risk of death” to avoid an unintended pregnancy (79).
Cost-effectiveness of family planning
International studies confirm that family planning is among the most cost-effective of all health interventions (80, 81). The cost savings stem from a reduction in unintended pregnancy, as well as a reduction in transmission of sexually transmitted infections, including HIV. It has been consistently documented that all contraceptive methods are cost-effective in comparison to no method (82, 83). An analysis of a publicly funded family planning program calculated that long-acting contraceptives (implants and IUDs), in particular, save US $7 in costs from unintended pregnancy for every US $1 spent (84). A recent study examining the cost effectiveness of contraception over 5 years in the United States showed the copper-T IUD, the levonorgestrel-containing IUD, and vasectomy to be the most cost-effective options (83). Although data show differences among individual developing countries, the measured savings are substantial everywhere. One US dollar spent on family planning can avert from US $2 (in Ethiopia) to US $9 (in Bolivia) in health costs, with an average of US $8 annually for all women using all methods of modern contraception (14, 81). The previously cited cost-effectiveness models for Mexico calculate lifetime savings of US $10.5 million with increased contraceptive prevalence (77). However, discontinuation of contraception, which often results from dissatisfaction, negatively impacts cost-effectiveness. Thus, having many contraceptive choices available is likely to increase overall cost-effectiveness (79, 84).
DISCUSSION
This review has focused on recent empirical studies of associations between pregnancy intentions and pregnancy and maternal outcomes and then examined the intermediate role of contraception as a health intervention. In the pathways of the behavioral epidemiology that link coital activity, conception, viable pregnancy, fetal growth, parturition, and the puerperium, protected sex is an important early juncture for preventing unhealthy sequelae, such as sexually transmitted infection, unintended pregnancy, fetal wastage, stillbirth, and maternal and neonatal morbidity and mortality. Modern contraceptive use and consistent condom use are highly effective means of preventing unplanned pregnancies and sexually transmitted infections.
We located and reviewed 21 eligible studies in the literature between 2004 and 2009, a time frame not covered by recent reviews. All involved individual-level, multivariate analyses; nearly all were observational; and 16 were US based. Three examined the association between pregnancy intentions and birth outcomes and 3 with maternal health behaviors and outcomes. Evidence of the effect of unintended pregnancies was inconclusive. We examined 5 other studies, again all US based, of pregnancy intentions’ relation with contraceptive use, one that should have been straightforward and substantial but was not. The bivariate results showed a surprisingly high percentage of study participants not using contraception despite intentions to defer or limit further childbearing. We next reviewed findings of 9 studies, 4 based in the United States, of contraceptive use and pregnancy incidence, particularly unplanned and electively terminated pregnancies. Here, we found more consistent results, generally of the order observed for 1-year contraceptive efficacy under typical use conditions.
The limited number of rigorous studies, particularly outside the United States and beyond individual risk factors, prompted us to look at studies adopting a population or demographic methods approach. Many of these analyses are cross-national, using standardized data and measures from the DHS. The identified studies often applied statistical models or forecasting methods with multiple country surveys to generate aggregate estimates of health benefits, such as averted unplanned pregnancies, pregnancy terminations, and maternal and infant deaths. In contrast to risk ratios from individual-level studies, the population-level studies provide counts of contraception-averted events that affect the pregnancy denominators of maternal and infant morbidity and mortality rates. Reviewing the demographic evidence of the contraceptive use–attributable impact on the burden of unintended pregnancies offers a complementary perspective and a more comprehensive understanding of the underlying structure of behavioral linkages.
By assessing study findings with population-level rates and ratios, we observed the scale and recurring probability of enabling and disabling sexual and reproductive health practices and events. Global contraceptive use prevents more than 200 million unintended births annually, which lowers rates of both unintended pregnancy and abortion. Some studies found that it significantly impacted maternal and infant mortality rates as well. Other studies have measured contraception's benefits in lowering the number of vertical HIV transmission cases among infected mothers interested in postponing or delaying future pregnancies. More research is needed to differentiate contraception's direct effect in reducing the number of (unintended) pregnancies from its indirect effect on the prevalence and incidence of unfavorable outcomes. Rising contraceptive practice in a population can coincide with favorable shifts in the distribution of pregnancy-related risks because of such common influences as gains in female education or household income, but prolonged contraceptive practice in the interpregnancy interval can also confer health benefits of maternal nutrition repletion on fetal growth and newborn survival. A reduction in unintended pregnancies reduces the number of events exposed to poor pregnancy outcomes and can make planned events healthier. An integrated understanding of family planning–attributable change in pregnancy events and change in epidemiologic risk-associated ratios deserves priority in future research efforts.
Understanding the effect of pregnancy intentions on contraceptive and reproductive behaviors is also requisite for strengthening the evidence base that informs maternal and child health policies and programs. Implicitly, it requires improving the measurement of fertility intentions both in the United States and abroad. Santelli et al. (85) identified affective, cognitive, and partner-specific dimensions as promising directions for future improvements. The modest empirical connections observed here among pregnancy intentions, contraceptive use, and health outcomes challenge the assumed reliability of unmet contraceptive need, a widely used measure that depends on a woman's reported desire to time future pregnancies. The gap between intentions and behavior, likely due to a combination of individual preferences and contextual factors of service access and of cultural and personal relationships, demands appropriate research designs to assess the causal relevance of pregnancy intentions to reproductive behavior and more focused research on family planning's health benefits when used before, after, and between pregnancies. The potential of contraception-facilitated birth spacing for preventing preterm and low birth weight infants to avert chronic disease in later adulthood is intriguing and warrants robust investigation with cohort data.
Demographic growth in the developing world will continue to exert upward pressure on the population base of women of reproductive age for several decades. Considerable momentum is built into population age structures as a consequence of past high fertility. At current rates, the number of unintended pregnancies will rise to 92 million globally by 2015. In many countries, where contraceptive prevalence is low and 40% to 50% of the population is under age 15 years, the entry of these cohorts into sexual activity and reproductive age will expose large numbers to the risk of unintended pregnancy. Access to quality contraceptive services will need to be expanded to avoid a rise in the volume of unplanned births and improve preconceptional health. Perhaps even more critical is to mount a substantial research effort that can address the implications of elevated sexual and reproductive health risks among adolescents and youth and the demographic import for future generations’ health and well-being.
Acknowledgments
Author affiliations: Department of Population, Family and Reproductive Health, Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland (Amy O. Tsui); and Department of Gynecology and Obstetrics, The Johns Hopkins University School of Medicine, Baltimore, Maryland (Raegan McDonald-Mosley, Anne E. Burke).
This review was supported in part by funding from the Bill and Melinda Gates Foundation to the Bill and Melinda Gates Institute for Population and Reproductive Health at the Johns Hopkins Bloomberg School of Public Health.
Conflict of interest: none declared.
Glossary
Abbreviations
- CI
confidence interval
- DHS
Demographic and Health Surveys
- HIV
human immunodeficiency virus
- IUD
intrauterine device
- OR
odds ratio
References
- 1.Ten great public health achievements—United States, 1900–1999. MMWR Morb Mortal Wkly Rep. 1999;48(12):241–243. [PubMed] [Google Scholar]
- 2.United Nations. Levels and Trends of Contraceptive Use as Assessed in 1988. New York, NY: Department of International Economic and Social Affairs, United Nations; 1989. (ST/ESA/SER.A/110) [Google Scholar]
- 3.Population Reference Bureau. Family Planning Worldwide 2008 Data Sheet. Washington, DC: Population Reference Bureau; 2008. [Google Scholar]
- 4.Robinson WC, Ross JA. The Global Family Planning Revolution: Three Decades of Population Policies and Programs. Washington, DC: World Bank; 2007. [Google Scholar]
- 5.Wu J, Meldrum S, Dozier A, et al. Contraceptive nonuse among US women at risk for unplanned pregnancy. Contraception. 2008;78(4):284–289. doi: 10.1016/j.contraception.2008.04.124. [DOI] [PubMed] [Google Scholar]
- 6.United Nations Population Fund. New York, NY: UNFPA; How the ICPD Programme of Action supports the MDGs. ( www.unfpa.org/public/cache/offonce/icpd/pid/5072#mdg5). (Accessed January 11, 2010) [Google Scholar]
- 7.United Nations. New York, NY: United Nations Department of Economic and Social Affairs/Population Division; 2009. World population policies 2009. ( http://www.un.org/esa/population/publications/wpp2009/Publication_highlights.pdf). (Accessed January 13, 2010) [Google Scholar]
- 8.The Hague, the Netherlands: Netherlands Interdisciplinary Demographic Institute; 2009. Financial resource flows for population activities in 2007. ( http://www.resourceflows.org/index.php/articles/c87/). (Accessed December 15, 2009) [Google Scholar]
- 9.United Nations Population Fund. Financing the ICPD programme of action: data for 2006. New York, NY. ( www.unfpa.org/public/cache/offonce/publications/pid/3935). (Accessed December 15, 2009) [Google Scholar]
- 10.Tietze C. Probability of pregnancy resulting from a single unprotected coitus. Fertil Steril. 1960;11:485–488. [Google Scholar]
- 11.Wilcox AJ, Dunson DB, Weinberg CR, et al. Likelihood of conception with a single act of intercourse: providing benchmark rates for assessment of post-coital contraceptives. Contraception. 2001;6(4):211–215. doi: 10.1016/s0010-7824(01)00191-3. [DOI] [PubMed] [Google Scholar]
- 12.Wawer MJ, Gray RH, Sewankambo NK, et al. Rates of HIV-1 transmission per coital act, by stage of HIV-1 infection, in Rakai, Uganda. J Infect Dis. 2005;191(9):1403–1409. doi: 10.1086/429411. [DOI] [PubMed] [Google Scholar]
- 13.King JC. The risk of maternal nutritional depletion and poor outcomes increases in early or closely spaced pregnancies. J Nutr. 2003;133(5 suppl 2):1732S–1736S. doi: 10.1093/jn/133.5.1732S. [DOI] [PubMed] [Google Scholar]
- 14.Singh S, Darroch JE, Ashford L, et al. Meeting the need for modern family planning services. In: Singh S, Darroch JE, Ashford L, et al., editors. Adding It Up: The Costs and Benefits of Investing in Family Planning and Maternal and Newborn Health. New York, NY: Guttmacher Institute and United Nations Population Fund; 2009. pp. 16–20. [Google Scholar]
- 15.Santelli J, Rochat R, Hatfield-Timajchy K, et al. The measurement and meaning of unintended pregnancy. Perspect Sex Reprod Health. 2003;35(2):94–101. doi: 10.1363/3509403. [DOI] [PubMed] [Google Scholar]
- 16.Koenig MA, Acharya R, Singh S, et al. Do current measurement approaches underestimate levels of unwanted childbearing? Evidence from rural India. Popul Stud (Camb) 2006;60(3):243–256. doi: 10.1080/00324720600895819. [DOI] [PubMed] [Google Scholar]
- 17.Klerman LV. The intendedness of pregnancy: a concept in transition. Matern Child Health J. 2000;4(3):155–162. doi: 10.1023/a:1009534612388. [DOI] [PubMed] [Google Scholar]
- 18.Bankole A, Westoff CF. The consistency and validity of reproductive attitudes: evidence from Morocco. J Biosoc Sci. 1998;30(4):439–455. doi: 10.1017/s0021932098004398. [DOI] [PubMed] [Google Scholar]
- 19.Westoff C. New Estimates of Unmet Need and the Demand for Family Planning. Calverton, MD: Macro International Inc; 2006. (DHS comparative reports no. 14) [Google Scholar]
- 20.Westoff C, Bankole A. Unmet Need: 1990–1994. Calverton, MD: Macro International Inc; 1995. (DHS Comparative Studies no. 16) [Google Scholar]
- 21.Sonfield A. Working to eliminate the world's unmet need for contraception. Guttmacher Policy Rev. 2006;9(1):10–13. [Google Scholar]
- 22.Trussell J. Contraceptive failure in the United States. Contraception. 2004;70(2):89–96. doi: 10.1016/j.contraception.2004.03.009. [DOI] [PubMed] [Google Scholar]
- 23.Seiber EE, Bertrand JT, Sullivan TM. Changes in contraceptive method mix in developing countries. Int Fam Plan Perspect. 2007;33(3):117–123. doi: 10.1363/3311707. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan TM, Bertrand JT, Rice J, et al. Skewed contraceptive method mix: why it happens, why it matters. J Biosoc Sci. 2006;38(4):501–521. doi: 10.1017/S0021932005026647. [DOI] [PubMed] [Google Scholar]
- 25.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann. 2008;39(1):18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 26.Cleland J, Bernstein S, Ezeh A, et al. Family planning: the unfinished agenda. Lancet. 2006;368(9549):1810–1827. doi: 10.1016/S0140-6736(06)69480-4. [DOI] [PubMed] [Google Scholar]
- 27.Shah PS, Balkhair T, Ohlsson A, et al. Intention to become pregnant and low birth weight and preterm birth: a systematic review [published online December 10, 2009] Matern Child Health J. doi: 10.1007/s10995-009-0546-2. (doi:10.1007/s10995-009-0546-2) [DOI] [PubMed] [Google Scholar]
- 28.Afable-Munsuz A, Braveman P. Pregnancy intention and preterm birth: differential associations among a diverse population of women. Perspect Sex Reprod Health. 2008;40(2):66–73. doi: 10.1363/4006608. [DOI] [PubMed] [Google Scholar]
- 29.Keeton K, Hayward RA. Pregnancy intention and birth outcomes: does the relationship differ by age or race? J Womens Health (Larchmt) 2007;16(4):510–516. doi: 10.1089/jwh.2006.M710. [DOI] [PubMed] [Google Scholar]
- 30.Mohllajee AP, Curtis KM, Morrow B, et al. Pregnancy intention and its relationship to birth and maternal outcomes. Obstet Gynecol. 2007;109(3):678–686. doi: 10.1097/01.AOG.0000255666.78427.c5. [DOI] [PubMed] [Google Scholar]
- 31.Marston C, Cleland J. The Effects of Contraception on Obstetric Outcomes. Geneva, Switzerland: Department of Reproductive Health and Research, World Health Organization; 2004. [Google Scholar]
- 32.Cheng D, Schwarz EB, Douglas E, et al. Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors. Contraception. 2009;79(3):194–198. doi: 10.1016/j.contraception.2008.09.009. [DOI] [PubMed] [Google Scholar]
- 33.Shapiro-Mendoza CK, Selwyn BJ, Smith DP, et al. The impact of pregnancy intention on breastfeeding duration in Bolivia and Paraguay. Stud Fam Plann. 2007;38(3):198–205. doi: 10.1111/j.1728-4465.2007.00131.x. [DOI] [PubMed] [Google Scholar]
- 34.Bartz D, Shew M, Ofner S, et al. Pregnancy intentions and contraceptive behaviors among adolescent women: a coital event level analysis. J Adolesc Health. 2007;41(3):271–276. doi: 10.1016/j.jadohealth.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 35.O'Rourke K, Richman A, Roddy M, et al. Does pregnancy/paternity intention predict contraception use? A study among US soldiers who have completed initial entry training. J Fam Plann Reprod Health Care. 2008;34(3):165–168. doi: 10.1783/147118908784734891. [DOI] [PubMed] [Google Scholar]
- 36.Frost JJ, Darroch JE. Factors associated with contraceptive choice and inconsistent method use, United States, 2004. Perspect Sex Reprod Health. 2008;40(2):94–104. doi: 10.1363/4009408. [DOI] [PubMed] [Google Scholar]
- 37.Vaughan B, Trussell J, Kost K, et al. Discontinuation and resumption of contraceptive use: results from the 2002 National Survey of Family Growth. Contraception. 2008;78(4):271–283. doi: 10.1016/j.contraception.2008.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Barden-O'Fallon JL, Speizer IS, White JS. Association between contraceptive discontinuation and pregnancy intentions in Guatemala. Rev Panam Salud Publica. 2008;23(6):410–417. doi: 10.1590/s1020-49892008000600006. [DOI] [PubMed] [Google Scholar]
- 39.Bradley SEK, Schwandt HM, Khan S. Levels, Trends, and Reasons for Contraceptive Discontinuation. Calverton, MD: ICF Macro; 2009. (DHS analytical studies 20) [Google Scholar]
- 40.Frank-Herrmann P, Heil J, Gnoth C, et al. The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple's sexual behaviour during the fertile time: a prospective longitudinal study. Hum Reprod. 2007;22(5):1310–1319. doi: 10.1093/humrep/dem003. [DOI] [PubMed] [Google Scholar]
- 41.Goodman S, Hendlish SK, Reeves MF, et al. Impact of immediate postabortal insertion of intrauterine contraception on repeat abortion. Contraception. 2008;78(2):143–148. doi: 10.1016/j.contraception.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 42.Kuroki LM, Allsworth JE, Redding CA, et al. Is a previous unplanned pregnancy a risk factor for a subsequent unplanned pregnancy? Am J Obstet Gynecol. 2008;199(5):517.e1–517.e7.. doi: 10.1016/j.ajog.2008.03.049. (doi:10.1016/j.ajog.2008.03.049) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sedgh G, Bankole A, Oye-Adeniran B, et al. Unwanted pregnancy and associated factors among Nigerian women. Int Fam Plan Perspect. 2006;32(4):175–184. doi: 10.1363/3217506. [DOI] [PubMed] [Google Scholar]
- 44.Shlay JC, Zolot L, Bell D, et al. Association between provision of initial family planning services and unintended pregnancy among women attending an STD clinic. J Womens Health (Larchmt) 2009;18(10):1693–1699. doi: 10.1089/jwh.2008.0966. [DOI] [PubMed] [Google Scholar]
- 45.Goldsmith KA, Kasehagen LJ, Rosenberg KD, et al. Unintended childbearing and knowledge of emergency contraception in a population-based survey of postpartum women. Matern Child Health J. 2008;12(3):332–341. doi: 10.1007/s10995-007-0252-x. [DOI] [PubMed] [Google Scholar]
- 46.Regushevskaya E, Dubikaytis T, Nikula M, et al. Contraceptive use and abortion among women of reproductive age in St. Petersburg, Russia. Perspect Sex Reprod Health. 2009;41(1):51–58. doi: 10.1111/j.1931-2393.2009.04115109.x. [DOI] [PubMed] [Google Scholar]
- 47.MEASURE Demographic and Health Surveys. StatCompiler. Calverton, MD: Measure DHS, ICF Macro; ( http://www.statcompiler.com). (Accessed January 12, 2010) [Google Scholar]
- 48.Wilcher R, Cates W, Jr., Gregson S. Family planning and HIV: strange bedfellows no longer. AIDS. 2009;23(suppl 1):S1–S6. doi: 10.1097/01.aids.0000363772.45635.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Halperin DT, Stover J, Reynolds HW. Benefits and costs of expanding access to family planning programs to women living with HIV. AIDS. 2009;23(suppl 1):S123–S130. doi: 10.1097/01.aids.0000363785.73450.5a. [DOI] [PubMed] [Google Scholar]
- 50.Bradley H, Bedada A, Tsui A, et al. HIV and family planning service integration and voluntary HIV counselling and testing client composition in Ethiopia. AIDS Care. 2008;20(1):61–71. doi: 10.1080/09540120701449112. [DOI] [PubMed] [Google Scholar]
- 51.Hoffman IF, Martinson FE, Powers KA, et al. The year-long effect of HIV-positive test results on pregnancy intentions, contraceptive use, and pregnancy incidence among Malawian women. J Acquir Immune Defic Syndr. 2008;47(4):477–483. doi: 10.1097/QAI.0b013e318165dc52. [DOI] [PubMed] [Google Scholar]
- 52.Hladik W, Stover J, Esiru G, et al. The contribution of family planning towards the prevention of vertical HIV transmission in Uganda. PLoS One. 2009;4(11):e7691. doi: 10.1371/journal.pone.0007691. (doi:10.1371/journal.pone.0007691) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Grimes DA, Benson J, Singh S, et al. Unsafe abortion: the preventable pandemic. Lancet. 2006;368(9550):1908–1919. doi: 10.1016/S0140-6736(06)69481-6. [DOI] [PubMed] [Google Scholar]
- 54.World Health Organization. Unsafe Abortion: Global and Regional Estimates of the Incidence of Unsafe Abortion and Associated Mortality in 2003. 5th ed. Geneva, Switzerland: WHO; 2007. [Google Scholar]
- 55.Prata N, Sreenivas A, Vahidnia F, et al. Saving maternal lives in resource-poor settings: facing reality. Health Policy. 2009;89(2):131–148. doi: 10.1016/j.healthpol.2008.05.007. [DOI] [PubMed] [Google Scholar]
- 56.Vlassoff M, Sundaram A, Bankole A, et al. Benefits of meeting the contraceptive needs of Ugandan women. Issues Brief (Alan Guttmacher Inst) 2009;4:1–8. [PubMed] [Google Scholar]
- 57.Singh S, Prada E, Kestler E. Induced abortion and unintended pregnancy in Guatemala. Int Fam Plan Perspect. 2006;32(3):136–145. doi: 10.1363/3213606. [DOI] [PubMed] [Google Scholar]
- 58.Westoff C. Recent Trends in Abortion and Contraception in 12 Countries. Calverton, MD: Macro International Inc; 2005. (DHS analytic studies no. 8) [Google Scholar]
- 59.Schünmann C, Glasier A. Measuring pregnancy intention and its relationship with contraceptive use among women undergoing therapeutic abortion. Contraception. 2006;73(5):520–524. doi: 10.1016/j.contraception.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 60.Sedgh G, Henshaw S, Singh S, et al. Induced abortion: estimated rates and trends worldwide. Lancet. 2007;370(9595):1338–1345. doi: 10.1016/S0140-6736(07)61575-X. [DOI] [PubMed] [Google Scholar]
- 61.Rutstein SO. Effects of preceding birth intervals on neonatal, infant and under-five years mortality and nutritional status in developing countries: evidence from the demographic and health surveys. Int J Gynaecol Obstet. 2005;89(suppl 1):S7–S24. doi: 10.1016/j.ijgo.2004.11.012. [DOI] [PubMed] [Google Scholar]
- 62.Conde-Agudelo A, Belizán JM, Norton MH, et al. Effect of the interpregnancy interval on perinatal outcomes in Latin America. Obstet Gynecol. 2005;106(2):359–366. doi: 10.1097/01.AOG.0000171118.79529.a3. [DOI] [PubMed] [Google Scholar]
- 63.Conde-Agudelo A, Belizán JM. Maternal morbidity and mortality associated with interpregnancy interval: cross sectional study. BMJ. 2000;321(7271):1255–1259. doi: 10.1136/bmj.321.7271.1255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Razzaque A, Da Vanzo J, Rahman M, et al. Pregnancy spacing and maternal morbidity in Matlab, Bangladesh. Int J Gynaecol Obstet. 2005;89(suppl 1):S41–S49. doi: 10.1016/j.ijgo.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 65.Yeakey MP, Muntifering CJ, Ramachandran DV, et al. How contraceptive use affects birth intervals: results of a literature review. Stud Fam Plann. 2009;40(3):205–214. doi: 10.1111/j.1728-4465.2009.00203.x. [DOI] [PubMed] [Google Scholar]
- 66.Tsui A, Creanga A. Does contraceptive use reduce neonatal and infant mortality? Findings from a multi-country analysis. Paper presented at the 2009 Annual Meeting of the Population Association of America, Detroit, Michigan, April 30–May 2. [Google Scholar]
- 67.Liu L, Becker S, Tsui A, et al. Three methods of estimating births averted nationally by contraception. Popul Stud (Camb) 2008;62(2):191–210. doi: 10.1080/00324720801897796. [DOI] [PubMed] [Google Scholar]
- 68.Ross J, Blanc A. The contribution of family planning to reducing maternal deaths. Presentation at the International Family Planning Conference: Research and Best Practices, Kampala, Uganda, November 15–18, 2009. [Google Scholar]
- 69.Chowdhury ME, Ahmed A, Kalim N, et al. Causes of maternal mortality decline in Matlab, Bangladesh. J Health Popul Nutr. 2009;27(2):108–123. doi: 10.3329/jhpn.v27i2.3325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Khadr Z. Monitoring socioeconomic inequity in maternal health indicators in Egypt: 1995–2005. Int J Equity Health. 2009;8:38. doi: 10.1186/1475-9276-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stover J, Ross J. How increased contraceptive use has reduced maternal mortality [published online September 17, 2009] Mater Child Health J. doi: 10.1007/s10995-009-0505-y. (doi:10.1007/s10995-009-0521-y) [DOI] [PubMed] [Google Scholar]
- 72.Sciarra JJ. Global issues in women's health. Int J Gynaecol Obstet. 2009;104(1):77–79. doi: 10.1016/j.ijgo.2008.09.001. [DOI] [PubMed] [Google Scholar]
- 73.Levine R, Langer A, Birdsall N, et al. Contraception. In: Jamieson DT, Breman JG, Measham AR, et al., editors. Disease Control Priorities in Developing Countries. 2nd ed. Washington, DC: World Bank; 2006. pp. 1075–1090. [PubMed] [Google Scholar]
- 74.Ezzati M, Vander Hoom S, Lopez AD, et al. Global Burden of Disease and Risk Factors. Washington, DC: World Bank; 2006. Comparative quantification of mortality and burden of disease attributable to selected risk factors. ( http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gbd&part=A592) [PubMed] [Google Scholar]
- 75.Chersich MF, Luchters SM, Yard E, et al. Morbidity in the first year postpartum among HIV-infected women in Kenya. Int J Gynaecol Obstet. 2008;100(1):45–51. doi: 10.1016/j.ijgo.2007.06.053. [DOI] [PubMed] [Google Scholar]
- 76.Chersich MF, Kley N, Luchters SM, et al. Maternal morbidity in the first year after childbirth in Mombasa, Kenya: a needs assessment. BMC Pregnancy Childbirth. 2009;9:51. doi: 10.1186/1471-2393-9-51. (doi:10.1186/1471-2393-9-51) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Biddlecom A. Unsafe Abortion in Kenya. In brief, 2008 series, no. 4. New York, NY: Guttmacher Institute; 2008. [PubMed] [Google Scholar]
- 78.Hu D, Bertozzi SM, Gakidou E, et al. The costs, benefits, and cost-effectiveness of interventions to reduce maternal morbidity and mortality in Mexico. PLoS One. 2007;2(1):e750. doi: 10.1371/journal.pone.0000750. (doi:10.1371/journal.pone.0000750.g002) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Schwarz EB, Smith R, Steinauer J, et al. Measuring the effects of unintended pregnancy on women's quality of life. Contraception. 2008;78(3):204–210. doi: 10.1016/j.contraception.2008.04.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Burkman RT, Sonnenberg FA. Health economics of contraception. Obstet Gynecol Clin North Am. 2000;27(4):917–931. doi: 10.1016/s0889-8545(05)70177-7. viii. [DOI] [PubMed] [Google Scholar]
- 81.Smith R, Ashford L, Gribble J, et al. Family Planning Saves Lives. 4th ed. Washington, DC: Population Reference Bureau; 2009. [Google Scholar]
- 82.Trussell J, Leveque JA, Koenig JD, et al. The economic value of contraception: a comparison of 15 methods. Am J Public Health. 1995;85(4):494–503. doi: 10.2105/ajph.85.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Trussell J, Lalla AM, Doan QV, et al. Cost effectiveness of contraceptives in the United States. Contraception. 2009;79(1):5–14. doi: 10.1016/j.contraception.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Foster DG, Rostovtseva DP, Brindis CD, et al. Cost savings from the provision of specific methods of contraception in a publicly funded program. Am J Public Health. 2009;99(3):446–451. doi: 10.2105/AJPH.2007.129353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Santelli JS, Lindberg LD, Orr MG, et al. Toward a multidimensional measure of pregnancy intentions: evidence from the United States. Stud Fam Plann. 2009 doi: 10.1111/j.1728-4465.2009.00192.x. 40(2):40(2):87–100. [DOI] [PubMed] [Google Scholar]
- 86.Brown MS. Coitus, the proximate determinant of conception: inter-country variance in sub-Saharan Africa. J Biosoc Sci. 2000;32(2):145–159. doi: 10.1017/s0021932000001450. [DOI] [PubMed] [Google Scholar]
- 87.Beck S, Wojdyla D, Say L, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88(1):31–38. doi: 10.2471/BLT.08.062554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ventura SJ, Abma JC, Mosher WD. Estimated pregnancy rates for the United States, 1990–2005: an update. Natl Vital Stat Rep. 2009;58(4):1–14. [PubMed] [Google Scholar]
- 89.Alan Guttmacher Institute. Sharing Responsibility: Women, Society and Abortion Worldwide. New York, NY: Alan Guttmacher Institute; 1999. [Google Scholar]
- 90.World Health Organization. Maternal Mortality in 2005: Estimates Developed by WHO, UNICEF, UNFPA and the World Bank. Geneva, Switzerland: WHO; 2007. [Google Scholar]
- 91.Stanton C, Lawn JE, Rahman H, et al. Stillbirth rates: delivering estimates in 190 countries. Lancet. 2006;367(9521):1487–1494. doi: 10.1016/S0140-6736(06)68586-3. [DOI] [PubMed] [Google Scholar]
- 92.Population Reference Bureau. Washington, DC: Population Reference Bureau; 2009. 2009 World population data sheet. ( http://www.prb.org/pdf09/09wpds_eng.pdf). (Accessed April 28, 2010) [Google Scholar]
- 93.World Health Organization. Neonatal and Perinatal Mortality: Country, Regional and Global Estimates. Geneva, Switzerland: WHO; 2006. [Google Scholar]
- 94.Hardee K, Eggleston E, Wong EL, et al. Unintended pregnancy and women's psychological well-being in Indonesia. J Biosoc Sci. 2004;36(5):617–626. doi: 10.1017/s0021932003006321. [DOI] [PubMed] [Google Scholar]