Abstract
This paper investigates the state-sponsored low cost housing provided to previously disadvantaged communities in the City of Cape Town. The strain imposed on municipal services by informal densification of unofficial backyard shacks was found to create unintended public health risks. Four subsidized low-cost housing communities were selected within the City of Cape Town in this cross-sectional survey. Data was obtained from 1080 persons with a response rate of 100%. Illegal electrical connections to backyard shacks that are made of flimsy materials posed increased fire risks. A high proportion of main house owners did not pay for water but sold water to backyard dwellers. The design of state-subsidised houses and the unplanned housing in the backyard added enormous pressure on the existing municipal infrastructure and the environment. Municipal water and sewerage systems and solid waste disposal cannot cope with the increased population density and poor sanitation behaviour of the inhabitants of these settlements. The low-cost housing program in South Africa requires improved management and prudent policies to cope with the densification of state-funded low-cost housing settlements.
Keywords: low-cost houses, backyard dwellings, service delivery, public health, environment, sanitation, diarrhoeal disease
Introduction
Housing and its relationship to health has long been one of the core areas of public health research.1 Housing affects health through a range of factors, acting directly or indirectly at different levels.1 The assumption that provision of improved housing to previously disadvantaged urban slum dwellers may improve their health is still being debated.2 This premise however forms one of the six principles of the state-funded low-cost housing scheme in South Africa, referred to as the Breaking New Ground initiative, formerly known as the Reconstruction and Development Programme.3
The exact association between housing and the maintenance of health and well-being remain elusive.4 It is intuitively accepted that affordable housing that is appropriate for environmental and social conditions; will protect people from hazards and will promote good health and wellbeing, but definitive proof has not been published.5 Deficient housing on the other hand could compromise basic human needs such as water, sanitation, safe food preparation and storage as well as assisting in the rapid spread of communicable and food borne diseases.6 According to the World Health Organisation (WHO), the developing world records 98% of deaths resulting from unsafe water, sanitation and hygiene.7 The WHO report identified infectious diarrhoea as the largest single contributor to ill health associated with water, hygiene and sanitation inadequacies.7
In South Africa, like in Mexico, the accelerated migration of indigent rural people into urban areas caused informal settlements to grow beyond the coping capacity of city infrastructure. This resulted in the deterioration of living conditions and the surrounding environment.8–11 In theory, living in urban areas potentially offers improved access to health care, education, better housing and improved economic opportunities.8 In reality however, the growth of urban slum areas in developing countries brought about an increase in poverty as many poor, often illiterate and unskilled people leave rural areas to try and find employment in cities.8
A consequence of the housing backlog in South Africa is that nearly one-fifth of households live in informal dwellings and in response to this need, there had been a large roll-out of government-sponsored low-cost housing.9 The South African housing policy is centered around the provision of fully state-funded home-ownership for the poor and seeks to eradicate informal housing, including backyard shacks.10 The new owners of such subsidized houses acquired their houses for free, but the improvement in their living conditions in most cases was not accompanied by an improvement in their financial status. Most of these inhabitants remained unemployed or with insecure or intermittent employment.
The new home owners soon exploited one of the few resources at their disposal, namely space, by erecting informal or makeshift dwellings in their backyard which were constructed from inadequate building materials (eg, corrugated iron sheets, wood and cardboard). Most of these informal dwellings are used for rental by other poorly housed families. Backyard dwellings in such formal housing communities caused the slum conditions of their former existence to follow them.11,12 These informal dwellings (called shacks by the inhabitants) have no sanitation, water, electricity and waste disposal facilities. The subsequent overcrowding and failures of the existing sanitation infrastructure causes severe pressure on municipal services with accompanying environmental pollution. This paper investigates the facilities provided to previously disadvantages communities and the strain posed on municipal services by densified low cost housing communities in the City of Cape Town, thereby creating unintended public health risks.
Methods
This study was approved by the Committee for Human Research at the Faculty of Health Sciences of Stellenbosch University and was conducted according to the ethical guidelines and principles of the International Declaration of Helsinki,13 the South African Guidelines for Good Clinical Practice and the Ethical Guidelines for Research of the Medical Research Council of South Africa.14 All respondents were informed of the objective of the study in their home language (English, Afrikaans or isiXhosa) and signed informed consent. A copy of the informed consent was provided to all participating households. The survey was conducted anonymously. All participants could inspect the completed questionnaire answer sheet for anonymity. They then posted the form into a sealed box with a postal slot. The box was only unsealed at the end of the study.
Four subsidized housing communities were selected within the City of Cape Town Metropole (CCTM) to participate in this cross-sectional survey. The government subsidized low-cost housing communities identified as study sites were: Driftsands, Greenfields, Masipumelela and Tafelsig. These sites were selected to represent the best spatial coverage of all the subsidized housing settlements within the city. The settlements were selected regardless of the local or central authority under whose jurisdiction the housing schemes were originally erected. They had to be older than three years. This was important because in some of the newer settlements structural wear and tear of the houses had not yet become evident to the same extent as in the older settlements. The settlements selected had to have distinct boundaries that did not blend into informal settlement areas ( so-called squatter settlements) in order to avoid infection pressure in the form of garbage and water pollution introduced from neighbouring areas. All four settlements had numerous low-cost houses (referred to as main house from this point forward) with informal dwellings made of temporary building materials in the back yard (referred to as shacks by the inhabitants and so called in this paper).
A legacy of the previous spatial disparities in the City resulted in communities with predominantly only one ethnic group. There were three settlements with predominantly black inhabitants and one settlement with predominantly coloured (mixed ancestry) inhabitants. This selection was representative of the overall demographic profile of the settlements in the city. No questions or annotations on race were included in the questionnaire.
The sampling strategy was based on a systematic sampling technique with random starting points so as to cover the entire community in a non-biased and representative sample. This sampling strategy is a probabilistic sampling technique when spatial randomness is required. It comprises a selection of elements from an ‘ordered list’ (such as a street plan) in a specific way. A random starting point (plot number) is selected eg, along every street and pathway in the community and in the case of the present study every 10th dwelling after that was selected to participate in the study.
Data were collected by means of structured interview questionnaires during home visits to all selected dwellings by the senior author, assisted by a qualified registered nurse who spoke all three languages prevalent in the area. All dwellings on a selected plot (main house and informal dwellings in the back yard) were included but recorded separately. Overall, 321 dwellings on 165 plots were selected for participation in the study. A systematic randomized sampling procedure was used to select the plots in the four study sites. Data were obtained from 1020 persons in total with a response rate of 100%. All households elegible for inclusion into the study by the sampling strategy participated and no one in any of the selected dwellings refused to provide data. The field work for this study was conducted over a period of 16 days and interviews took a median time of 40 minutes per household.
The questionnaires were piloted in two different settlements (predominantly coloured and predominantly black) in the CCTM. The pilot study sites were situated in Mfuleni and Westbank and four plots were randomly selected from each of the sites. From these eight plots the survey was administered to 15 dwellings with data obtained from 60 persons. The results from the pilot sites met the same criteria as the study sites. No problems or confusing questions were encountered and these interviews were carried out under the same conditions as the main study. The data from the dwellings in these pilot sites were therefore included in the total group, ie, 1080 participants living in 336 dwellings (173 main houses and 163 shacks).
The questionnaire was designed to record data from all dwellings on a plot. These questionnaires were available in all three languages and administered in the language of preference during an onsite interview with the head of the household. The questionnaire comprised sections on demographic, health and home ownership as well as a section to note the condition of the dwelling and its surrounding yard. The inspection of the dwelling and yard concentrated on the sanitation infrastructure and condition of the premises. The toilet was classified as non-operational when one of the following was noted: toilet blocked, could not flush, had serious leaks or had a severely cracked cistern or bowl. The sanitary condition of the yard was classified as poor when one or more of the following was noted: presence of broken glass, solid waste, excreta, puddles of dirty water, overflowing waste bins, overflowing or dirty drains.
Demographic and socio-economic variables included age, gender, physical challenges, educational attainment, citizenship, social grant recipients, employment status and household monthly income. The household monthly income was arrived at by adding the income of all employed members of the dwelling. Health variables included HIV and TB status, as well as ailments suffered in the preceding two weeks of the survey. Respondents were given an option of disclosing their HIV and TB status. All medication in the dwelling that was issued by the clinic was inspected and the reported diagnoses verified from that.
A fully qualified community health nursing sister administered a questionnaire (available in three languages) regarding various aspects of health, including 20 questions on symptoms relating to sanitation and waterborne diseases. When respondents reported that they were on medication (either acute or chronic), the nurse asked to see the medication and confirmed the illness by cross-checking the reported illness with the prescribed medication. Only the illnesses confirmed by prescription medication from the clinic were entered into the study data base. This was done in order to enter only verifiable illnesses into the study. This was necessitated by inaccurate reporting of illnesses by respondents due to the poor understanding of disease in general and specific symptoms in particular in these communities mainly as a result of low levels of education.
Data were recorded in a database created in Statistica version 9.0 (StatSoft Inc. 2009, USA). Descriptive statistics mainly means and standard deviations for continuous variables and frequency distributions for categorical variables were computed. Bivariate analysis testing for differences in proportions of low-cost housing and backyard shacks were performed using the test for probability values.
Results
Income and education status
Significantly more of the occupants of the shacks were employed than the occupants of the main houses (χ2 test, P = 0.0000). Almost 42% of households in the total group had a combined household income per month of less than R1200 (about US$160). The reported incomes of the inhabitants of the main houses were statistically significantly lower than those of the occupants of the shacks (Mann-Whitney U-test, P < 0.01). Approximately 28% of main households and 20% backyard shack dwellers received a government social grant (Table 1). The occupants of the shacks had a significantly higher education status that the occupants of the main houses (Mann-Whitney U-test, P = 0.01).
Table 1.
Sociodemographic characteristics of the study population.
| Characteristic | Main house (n = 173 dwellings) | % | Shack (n = 163 dwellings) | % | Total group (n = 336 dwellings) | % | P-value |
|---|---|---|---|---|---|---|---|
| Study population | 710 | 66 | 370 | 34 | 1080 | 100 | |
| Gender | |||||||
| Male | 322 | 64 | 184 | 36 | 506 | 47 | 0.17 |
| Female | 388 | 68 | 186 | 32 | 574 | 53 | |
| Disabled individuals | 18 | 90 | 2 | 10 | 20 | 2 | <0.01 |
| Nationality | |||||||
| South African | 695 | 68 | 329 | 32 | 1024 | 95 | <0.01 |
| Non-South African | 18 | 32 | 38 | 68 | 56 | 5 | |
| Highest education level | |||||||
| No schooling | 103 | 59 | 73 | 41 | 176 | 16 | 0.01 |
| Grade 0–4 | 152 | 83 | 32 | 17 | 184 | 17 | |
| Grade 5–7 | 154 | 70 | 65 | 30 | 219 | 20 | |
| Grade 8–10 | 138 | 61 | 90 | 39 | 228 | 21 | |
| Grade 9–12 | 158 | 61 | 100 | 39 | 258 | 24 | |
| Tertiary level | 5 | 33 | 10 | 67 | 15 | 1 | |
| Employment status | |||||||
| Full time employed | 122 | 62 | 76 | 38 | 198 | 18 | <0.01 |
| Part time employed | 8 | 20 | 33 | 80 | 41 | 4 | |
| Irregular employed | 50 | 61 | 32 | 39 | 82 | 8 | |
| Unemployed | 210 | 65 | 112 | 35 | 322 | 30 | |
| Pensioner | 14 | 52 | 13 | 48 | 27 | 3 | |
| Child at home | 104 | 61 | 66 | 39 | 170 | 16 | |
| Scholar | 202 | 84 | 38 | 16 | 240 | 22 | |
| Household monthly income | |||||||
| <R600 per month | 25 | 48 | 27 | 52 | 52 | 15 | <0.01 |
| R600-R1200 per month | 29 | 33 | 59 | 67 | 88 | 26 | |
| R1200-R2500 per month | 58 | 53 | 52 | 47 | 110 | 33 | |
| >R2500 per month | 23 | 28 | 60 | 72 | 83 | 25 | |
| Unsure | 1 | 33 | 2 | 67 | 3 | 1 | |
| Households receiving a social grant | 93 | 58 | 66 | 42 | 159 | 48 | <0.01 |
Housing infrastructure
All of the main houses have been equipped with a flush toilet, either inside or outside the house. In all cases backyard dwellers were allowed to use the toilet on the property. If however the toilet inside the home was not available, then the neighbour’s toilet may be used or any receptacle that could act as a chamber pot was used. The contents of such receptacles were often disposed of in the storm water drain. On the day of the home visit, 58% of toilets were found to be non-operational (Table 2).
Table 2.
Distribution of observations of poor condition of low-cost (main) houses.
| Observation | Number (n = 173) | % |
|---|---|---|
| Outside walls not painted | 82 | 47 |
| Inside walls not painted | 88 | 51 |
| Cracked walls | 117 | 68 |
| Door not well fitted | 103 | 60 |
| Broken windows | 60 | 35 |
| Toilet not operational | 101 | 58 |
| Toilet leaking | 69 | 40 |
| Tap leaking | 63 | 36 |
| Roof leaking | 136 | 79 |
| Structural damage | 11 | 6 |
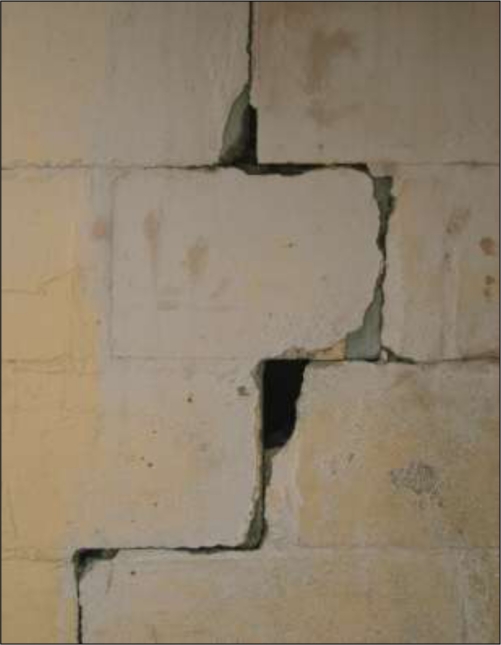
The main houses were in a state of disrepair (Table 2). The majority of the houses had cracked walls and/or visibly leaking roofs (walls streaked with previous leak damage). About half of the houses had unpainted walls, allowing wind-driven rain to seep through. A common occurrence was the use of softened bar soap to fill holes in leaking roofs. Some households had reported the structural problems (Table 2) to the City Council, but stated that they eventually “fixed the problem themselves or learnt to live with it.” This was fruitless as Council does not own these structures and could not be expected to maintain them.
Electricity and water services
All of the main houses had an operational prepaid electricity connection. Backyard dwellings created illegal connections from the main house, and paid between R50 to R200 per month for electricity usage. Of the main houses interviewed in the survey, only seven (4%) of the 173 houses timeously paid the local municipality for water usage (approximately R500 paid in total by the seven houses for a month). A total of 66% of backyard dwellers pay the landlord between R20 and R100 per month for water, in spite of the City providing the first 6000 litres of water for free each month to all households. The 97 backyard shack dwellers paid R6080 (about US$811) in total per month to landlords who themselves did not pay for this water. Backyard inhabitants fetched water from the main house and stored the water in a bucket in the shack.
Waste disposal
The disposal of household waste was unsatisfactory. The sanitary state of the yard outside the dwelling was classified as poor in 76% of the premises inspected. In 68% of cases there was no waste bin inside the dwelling. Household disposal of sewage from chamber pots and soiled baby diapers was inappropriate in 21% of cases (mainly into the storm water drain and in the street). In addition, 22% of households disposed of their solid refuse on the street. Fifteen percent of respondents said that nothing will happen if rubbish is thrown into the toilet.
All of the respondents in the survey complained of pests carrying potential health risks within their immediate home environment. The respondents from all four communities reported their most prominent pest problem was rats by 50%, cockroaches by 30%, fleas by 16% and flies by 4%. Flies were observed in all homes, indicating the presence of flies were under-reported.
Only one of the four sites had access to a drain leading to the sewerage system for the disposal of grey water (Table 3). Storm water drains were mostly used by families who lived in close proximity to such an opening in the kerb, while others preferred to use the toilet or open ground as disposal points. The storm water volume generated in built-up areas is related to the extent of the hardened surfaces in those areas. The total roof area for main houses was 5550 m2 while for backyard dwellings the total roof area was 1587 m2. Therefore the shacks added an extra 29% of roof area with resultant increase in stormwater during rain events. The inhabitants reported frequent flooding in the settlements.
Table 3.
The percentage of dwellings who dispose of household waste water inappropriately (n = 336).
| Waste water source | Open land | Toilet | Storm-water drain |
|---|---|---|---|
| Bathing/washing | 14.9 | 41.7 | 4.5 |
| Kitchen* | 23.2 | 20.2 | 2.7 |
| Laundry | 13.1 | 47.9 | 1.5 |
Notes:
Includes waste water from food preparation, dishes and cleaning.
Health profile
Over the two weeks preceding the survey 38% of dwellings reported one or more persons suffering from diarrhoea (Table 4).
Table 4.
Gender and age group of reported cases of diarrhea.
| Number of cases (n = 153) | % | |
|---|---|---|
| Dwelling type | ||
| Main house | 70 | 40 |
| Shack | 38 | 23 |
| Gender | ||
| Male | 74 | 48 |
| Female | 79 | 52 |
| Age | ||
| <10 | 50 | 33 |
| 11–20 | 23 | 15 |
| 21–30 | 38 | 25 |
| 31–40 | 26 | 17 |
| 41–50 | 10 | 7 |
| 51–60 | 3 | 2 |
| >60 | 3 | 2 |
Five percent of the participants willingly disclosed that they were HIV positive, while 11% reported that they were TB positive, one of whom reported being diagnosed with Multiple Drug Resistant (MDR) TB. None of those who reported suffering from TB or who were HIV positive had any medication for their condition in the dwelling. Furthermore, none of the TB or HIV infected individuals had visited the clinic in the preceding two months. The use of chronic medication was reported by 165 (15%) respondents. In many instances, respondents did not know what disease the medication was intended for. The five most common diseases diagnosed at the clinic and reported by the respondents are summarised in Table 5. Of the main houses, 51% had one or more inhabitants who smoked, while 49% of the shack dwellings had one or more smokers (Table 5).
Table 5.
Five most frequent illnesses diagnosed at a clinic* and treated by medication as reported by participants, differentiated by housing type.
| Diagnoses reported |
Main house occupants (n = 710) |
Shack dwellers (n = 370) |
P-value (Chi-square test) | ||
|---|---|---|---|---|---|
| Number | % | Number | % | ||
| Hypertension* | 42 | 5.9 | 9 | 2.4 | 0.01 |
| Asthma* | 32 | 4.5 | 17 | 4.6 | 0.95 |
| Diabetes* | 28 | 3.9 | 7 | 1.9 | 0.07 |
| Arthritis* | 25 | 3.5 | 2 | 0.5 | <0.01 |
| Epilepsy* | 7 | 1.0 | 4 | 1.1 | 0.88 |
| Substance use | 89 | 53 | 80 | 47 | 0.66 |
| Smoke cigarettes | 106 | 49 | 110 | 51 | 0.23 |
| Consume alcohol | 23 | 56 | 18 | 44 | 0.03 |
| Use drugs† | 89 | 53 | 80 | 47 | 0.66 |
Notes:
These diagnoses were verified by inspecting the medication issued by the clinic in each home;
The nature of the drugs were not explored.
Primary health care services
Three of the four low cost housing communities had access to a state clinic in their community. The Driftsands community used other healthcare facilities in neighbouring communities. Of the 400 signs and symptoms of illness reported by the participants, only 35% (140 symptoms) were treated by visiting the local clinic (Table 6).
Table 6.
Reported ailments and treatment.
|
Main house |
Shack |
Total |
P-value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Ailments reported | 249 | 35 | 151 | 41 | 400 | 37 | 0.06 |
| Participants suffering from ailment | 198 | 28 | 117 | 32 | 315 | 29 | 0.20 |
| Treatment of ailment | |||||||
| Visited clinic | 89 | 12 | 51 | 14 | 140 | 13 | 0.79 |
| Home treatment | 170 | 24 | 90 | 24 | 260 | 24 | |
| Participants still suffering from ailment | 158 | 22 | 96 | 82 | 254 | 24 | 0.62 |
Sixty percent of the participants walked to their primary health care clinic, while 39% used a ‘communal taxi’ and one percent utilized private transport. The amount paid for a return trip per person to a health care facility varied from R5.00 to R35.00 (about US$1–$5). This was a significant amount of the total household earnings as the mean reported total monthly income per household was R1353 (about US$180). The cost of transport mounted considerably for those on chronic medication who had to visit the clinic regularly. Thirty-five percent of the households reported that there had been one or more occasions during the preceding year when a family member needed to visit a clinic, but did not have money to pay for transport. A large percentage (71%) of the households were not satisfied with the services provided by the clinic and 86% thought that private health care facilities would offer better services than a state clinic.
Discussion
Despite commendable efforts, the housing backlog for South Africa’s urban poor has grown from 1.5 million units in 1994 to about 2.1 million in 2010, according to the Minister of Human Settlements. Taking into account the pace of delivery and the resources available, as well as continued economic and population growth and the rapid pace of urbanisation, it could take decades to beat the backlog.15
Income and education status
The economic implications of the creation of shacks for subletting can be seen not only in the direct rent charged but also the water that was sold to backyard dwellers. Only 4% of formal home owners paid the municipality for their water usage, but all sold water to the back yard dwellers. The amount of rent charged was not exorbitant and constituted a basic service rendered rather than an exploitative one. Very few of the dwellers living in the shacks were relatives of the dwellers in the main house. These shacks are rented out for income and/or to relieve the pressing housing need in the city. The situation therefore represents predominantly a landlord-renter relationship.
Contrary to common belief, the present survey found that backyard dwellers were better educated and had a higher employment rate and income when compared with the inhabitants of the main houses. Backyard dwellers have to seek employment and generate an income as they have to pay rent and water and electricity usage to the owner of the main house or otherwise face eviction. There is an inherent contradiction in this situation as the persons better able to pay (shack dwellers) are actually living in poorer housing conditions. When analysing the total distribution of education categories as included in the survey, the educational level attained by the inhabitants of the main houses were significantly lower than those of the shack dwellers. Of all the adults in the total group, 8% were illiterate or functionally illiterate (defined as schooling only up to Grade 4 or four years of primary school education). The lack of education among adults in the study contributed to the homeowners’ lack of knowledge on how to maintain their new home. This lack of knowing how to keep their homes clean and how to fix broken infrastructure were strongly verbally communicated by the respondents. In addition, their acquisition of an improved home was not accompanied by an improvement in employment status and that resulted in many being unable to afford the repairs or the cleaning materials required to keep the home clean. Within a short space of time, the sanitation facilities in their new home fell into a state of disrepair and were left uncleaned because of lack of both awareness and resources.
Housing infrastructure
The condition of the state-funded main houses in the present study was poor and a cause for concern. These houses are not ‘owned’ by the state or the local authority any longer and the present indigent owner does not have the financial ability or skills to maintain the house. Few of the owners actually exhibit a realistic awareness of what home ownership actually entails. Almost all of them wanted the “government” or the “municipality” to repair their homes. The situation has now deteriorated to the point that the failing sanitation infrastructure is impacting on municipal service delivery as well as causing huge pollution risks to the inhabitants and the environment. This looming crisis will need huge financial and other resources to redress. The improvements in living standards envisaged by the low-cost housing schemes are fast being lost. There is an urgent need for education of these home owners to improve their ability to maintain the infrastructure of their homes. In some cases small defects would have cost little to remedy at the time, but left untended, the cumulative cost for renovation in these settlements is by now very large.
Electricity and water services
All the formal and informal houses in this study had access to electricity. The shacks accessed electricity by means of illegal connections such as extension cords. When these electrical wires, many of which are of the wrong technical specifications for building to building connections, come into contact with corrugated metal roof material, sparks fly in windy conditions. In wet weather the ungrounded connections can cause severe electrical shocks. The high number of smokers and illegal electrical connections in the presence of flimsy building materials of the shacks (wood, corrugated iron sheets and even cardboard) increased the risk of structural fires considerably.
An analysis of burn injuries in Cape Town showed that shack fire burns were the second most frequent reason for admission to a Burns Unit in a secondary hospital in Cape Town.16 Thus the insecure nature of electricity supply to shacks in the backyard has implications for health care and fire services in the City. The damage to property and injuries caused by these frequent settlement fires are potentially preventable if municipal bylaws are strictly followed. At present the majority of efforts are aimed at speedier response to fires rather than prevention. It is however an extremely difficult situation for the municipal services, because eviction of backyard dwellers are not a political option in South Africa at present.
Waste disposal
Managing waste disposal in developing countries is one of the most costly services as it takes up to 1% of the gross national product and typically absorbs between 20% and 40% of municipal revenues.17 Improved technology can only be a partial solution to this problem.17 Successful implementation of proper waste management strategies strongly depend on an enabling social and economic environment that supports the services rendered. In the present study both the infrastructure enabling the inhabitants of these communities to follow safe disposal practices and their level of knowledge of such practices fall far short of even the most lenient definition of user co-operation. No education programs to redress this situation were encountered during the study.
The consequences of this disastrous lack of infrastructure and awareness can be seen from the worrisome results in this study. The levels of environmental pollution, the visible deterioration of the surroundings of these houses and the disease profiles of the inhabitants all indicate a looming crisis. These settlements are creating favourable conditions for disease outbreaks because of the easy transmission of particularly oral-faecal, water or food related pathogens. The lack of adequate and timely removal of solid waste causes seepage from bins and bulk rubbish containers and inappropriate rubbish disposal contributes to the environmental pollution. Improper waste disposal at the household and community level led to problems such as fly and rodent infestation, as reported by all four communities in the present study. These aspects of the re-housing of urban poor should receive attention by disaster-risk planning authorities.
Even though low-cost housing settlements provided access to an onsite toilet and water facilities for backyard shack dwellers to use, there are insufficient waste disposal facilities in those settlements. Direct discharges of untreated sewage from such settlements into the environment—notably the urban rivers—greatly increased the risk of disease transmission and environmental degradation, adding to the pressures on the urban poor. With a reported 21% of households admitting to the unsafe disposal of human excreta; waste water and raw sewage makes its way into yards, sidewalks and streets and into the storm water drains.18 The rationale behind the provision of free improved housing and free basic water allocation, namely increased hygiene and improved living conditions are thus negated by the lack of provision for adequate disposal of sewage, solid waste and waste water. Armitage et al (2009) warned that in settlements the waste streams of storm water, sanitation and refuse removal cannot be considered separately as the contamination is so effectively intermingled under these circumstances.19
Armitage et al (2009) found that grey water management had a low priority amongst inhabitants of settlements.19 Without adequate waterborne sanitation, the disposal of household waste water becomes a problem.20 Although the main houses in the present study had waterborne sanitation, the design of the facilities and the low level of proper sanitation behaviour of the inhabitants caused widespread disposal of waste water in two inappropriate ways. The City of Cape Town faces periodic water shortages that are set to increase with the advancement of climate change. Using potable water on such a large scale to dispose of waste water and other solid waste by flushing down the toilet is a wasteful habit that needs urgent educational remediation. Any community outreach to change this habit will ultimately fail, however, if user-friendly alternatives to this way of disposal are not provided. Unfortunately, retrofitting such user-friendly alternatives have cost and engineering implications for the City and this dilemma should be avoided by amending the planning in future housing settlements.
Storm water runoff in urban areas is increased by impermeable urban surfaces such roofs and as hard-topping of streets and driveways.21 Unfortunately settlements are often constructed with little consideration for storm water drainage.21 Even formal storm water drains are ‘passive’ systems simply receiving any water and solid matter discarded in or near them and are thus vulnerable to blocking-up or misuse. Storm water systems in low-cost settlements are used for the disposal of unwanted waste water, solid waste and even dead animals as was readily apparent in the present study areas. Apart from the risk of flooding because of blocked storm water systems, the other major impact of this unfortunate situation is the major contamination of rivers flowing past urban areas.22,23 The implications of this widespread pollution of surface water in the City for future water resources and environmental health should receive urgent attention by the City planners and engineers. Strategies that can be considered include: constructed wetlands, swales, passive infiltration systems and tactically placed impoundments.
Primary health care services
The reported HIV positivity of 5% was almost certainly an undercount. The prevalence of HIV for the Cape Town metropolitan area for 2008 was reported by the National Department of Health (2008) as 16.1% (95% confidence interval 14.7%–17.5%).24 The lack of any antiretroviral medication present in the dwellings was an equally worrisome finding. This indicates a need for better monitoring and evaluation along with a more incisive public health approach to support HIV positive persons. This unmet need has implications for the burgeoning HIV/AIDS epidemic in South Africa. Improved housing can theoretically improve the health of HIV positive persons,25 but under the present state of sanitation failures and polluted environments, these improvements will not materialize due to high infection pressure.
In spite of the reported TB and HIV positivity in this survey, no form of public health support or preventative programme regarding these diseases was visible in these communities. Education programmes need to be initiated and sustained over a long period, otherwise the relapse into old and unhelpful ways will simply overtake all progress made. Community health workers are needed to keep the programme operational. Without community-based health care ‘ advisors’ or community members who can keep an eye on the situation regarding cleanliness and disease status in the community, no lasting improvements will be seen. These community workers should be recruited from the communities they serve. With rudimentary training they can fulfill a useful function to bridge the gap between the health needs of the inhabitants and the City health services. Such a service will need some administrative support, but could be maintained at a relatively low cost.
TB or HIV positive persons or those who are malnourished need clean living environments because of their lowered immunity. The present living conditions in this study add significant infection pressure to the already poor health suffered by these persons. This in turn added to the patient load at the already overburdened and underfunded local health clinics, as well as higher up the referral chain of health services. The public health measures to tackle TB in these communities were wholly inadequate. The self-reported prevalence of TB was a source of great concern, notably the existence of a case of MDR-TB. The fact that none of these patients, including the case of MDR-TB, was on any TB medication has serious implications for the future management of this potentially preventable disease. None of the TB-positive persons visited the clinic in the preceding two months either, which indicated a serious lack of involvement of the primary health care services in the area.
If one in 1080 dwellers of these low-cost housing communities are already MDR-TB positive, then the City can expect a substantial increase in these difficult-to-treat cases, with a serious knock-on effect on the already overburdened health care system. The development of MDR may be related to poor compliance with drug treatment, poor treatment drug choices, poor access to primary health care facilities along with patient factors such as poor absorption of drugs and general poor health.26 Many of these factors are at play in these communities and the meticulous execution of TB control programmes in such environments should be a high priority. This need is clearly unmet at present.
Moraes et al (2005) showed that in three poor communities in Salvador, Brazil the incidence of diarrhoea in children in neighbourhoods with drainage and sewerage was one-third of the incidence in neighbourhoods with neither service.26 They also found that improving community sanitation—even in the absence of hygiene-promoting behaviour—can have an impact on diarrhoeal disease. This is important in the context of the high reporting of diarrhoeal disease among the inhabitants of the low-cost communities in the present study. Thus the effort and money spent on improving the sanitation systems in these communities should improve the diarrhoeal morbidity experienced by these communities. Unfortunately, estimations of the possible impact of improvements seldom include the expected easing of disease burdens as well as the reduction in the patient loads of the primary health services.
This survey only recorded conditions that were diagnosed formally at the clinic and for which the medication could be verified. A major factor influencing the accessibility of primary health care was the inability of some persons needing medical attention to procure transport to the clinic. The cost of using a communal taxi, especially for those with chronic conditions who had to visit the clinic repeatedly, made significant inroads into their household budget.
Many of the inhabitants of low-cost housing communities preferred to treat their ailments using home remedies or traditional medicines. South Africa has many tradition healers who dispense herbal medicines of various origins. Unfortunately the efficacy and safety of some of these medicines are unknown. At worst, such treatment may delay the diagnosis or treatment of serious transmissible conditions such as HIV and TB. This necessitates a need for traditional healers to work in synergy with Western medical treatment to improve the safety and health of inhabitants from low-income areas in South Africa. Although there have been sporadic programs to incorporate traditional healers into the formal health services, no systematic policy for incorporating them into the formal health services exists.
Barriers to access to health information and support services include cost, geographic location, illiteracy, disability and capacity to utilize information effectively.27,28 All of these restraints are present in the communities in the present survey and effective ways of bridging these gaps are not in place at present. Deliberate delays in obtaining medications were reported to be one of the most common strategies among urban poor in Australia.28 There are indications that this strategy was also prevalent among the participants in the present study since most attempted home remedies first. Many of those who should have been on treatment (TB and HIV positive persons) were not. Although the local clinic is within reachable distance for many, cost of transport remains a significant factor for these communities. The barriers resulting in low utilization have not been addressed in these communities, warranting further research into such barriers in order to prioritize their removal.
The low opinion of the perceived quality of care available at the clinics also contributed to the poor utilization of the primary health care available to these communities. Haddad et al (1998) studied the expectations and criteria that two rural communities in Guinea used to determine quality of service.29 He found that the criteria depended inter alia on gender and the ability to access the services and that the communities placed considerable emphasis on outcomes of treatment, but little emphasis on preventative services.29 With such poor utilization as reported in the present study and so many barriers to effective primary health care, the local clinics cannot play any meaningful role in addressing the serious health needs of the urban poor in these four communities. Preventative actions by the local clinics that are so sorely needed in these communities with their high HIV and TB burdens as well as the added complications of poverty, substance abuse and hunger will be largely fruitless under the present circumstances and needs to be addressed urgently.
Conclusion
The overall conclusion is that the envisaged improvements in health supposed to be associated by rehousing impoverished urban shack dwellers in improved housing did not materialise due to unforeseen housing design aspects as well as social and behavioural aspects. The reasons are not straight-forward. The lack of improvement in health resulted from complex interactions of poor design (especially sanitation infrastructure of both the dwellings and the municipal structures), low levels of education, poor sanitation behaviour, poverty and overcrowding. The shacks in the backyard contributed significantly to overcrowding, sanitation failures and environmental pollution, but were not in all instances the main drivers of these risk factors. They however added to the burdens already present in the communities. The shacks did contribute a moderate amount of income to the owners of the main houses, but whether this contribution is offset by the extra burden of disease (for instance) cannot be answered by the present study, nor was it designed to do so.
Given the design of these houses and the added pressure on the existing infrastructure by the inhabitants of unplanned housing in the backyard, these results send a powerful message that the existence of unplanned informal housing for the purposes of augmenting income intruding into upgraded government-sponsored housing can have a severe detrimental effect on the inhabitants of new low-cost housing schemes. A further negative aspect is the added pressures on the environment and the various services such as primary health care clinics and municipal water and sewerage systems. This informal densification needs to be better managed. Sensible policies to cope with this reality would allow the improved housing schemes to deliver the improved health that was promised at its inception.
The unfortunate separation of the fields of public health and urban planning has contributed to uncoordinated efforts to address the health of urban populations and a general failure to recognize the links between the built environment and health disparities facing low-income populations.30 A reconnection of these two responsibilities is a prerequisite for successful improvement of the present unsafe and unhealthy conditions prevailing in low-cost housing areas in South Africa.31 The irony is that these resettlement programs were instituted to improve the living conditions of the urban poor and it is imperative that this improvement be realized.
Figure 1.
Adjoining shacks in the Greenfields settlement obscuring municipal reticulation systems.
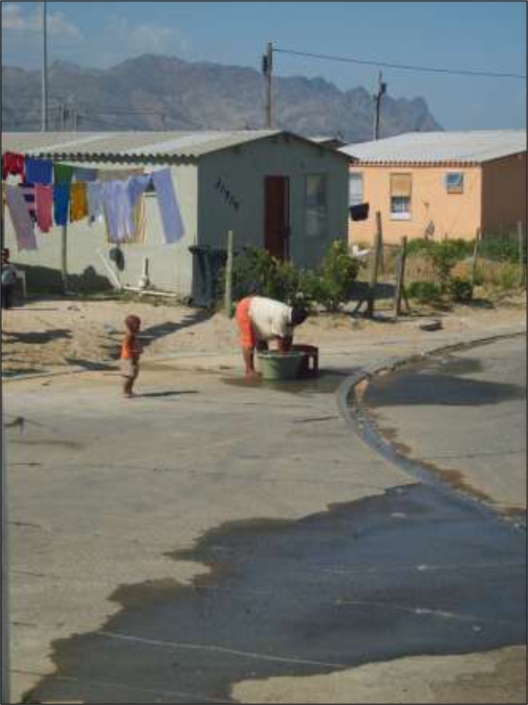
Figure 2.
An example of a low-cost house in Tafelsig.
Figure 3.
Dampness penetrating bedroom wall with infant sleeping on bed in a low-cost house in Greenfields.
Figure 4.
An example of structural damage: a seriously cracked wall of main house in Tafelsig.
Figure 5.
Tap against the wall on right is either lost or removed. Note the broken pipe and cistern, as well as the broken window which has been repaired with cardboard in Masipumelela.
Figure 6.
Flushing mechanism on this toilet is broken in a house in Masipumelela. Users flush toilet by manually manipulating the mechanism inside the system. Note that the toilet is dirty.
Figure 7.
An example of a kitchen area in Greenfields. Note the rudimentary facilities and dirty wall. This is the only working tap in the main house.
Figure 8.
Solid waste blocking the storm water inlet on street causing subsequent flooding during rain storms in Greenfields.
Figure 9.
Waste water running down the street in Greenfields. The woman doing her washing on the side walk is adding to the polluted water stream.
Acknowledgments
We thank the Harry Crossley Foundation, the German Academic Exchange Service (DAAD), the National Research Foundation and Stellenbosch University for the funding of this project. We are grateful to Sister N. Lethuka for assisting in the administering of the survey and Professor M. Kidd from the Centre for Statistical Consultation at Stellenbosch University for statistical support.
Appendicies
Appendix A: Health evaluation questionnaire
Good day Sir/Madam
My name is Sister Lethuka. You are invited to take part in a research project carried out by the Medical Faculty of the University of Stellenbosch. We are going to be studying your health and home. Note that your participation in the study is voluntary and you may opt to leave the interview at any time. All answers and comments will be kept highly confidential. We will not record your name and we promise that no information you give us will be attached to you or anyone living in your home. Please do not hesitate to ask any questions that you may have with this study.
Section 1: Biographical details
1.1 Please provide us with the following information, so that we can learn more about your family.
| Code of person | Role in household | Age | Is this person disabled? | How long has the person lived in this house (years) | Sex | Status of individual | Educational status: | ||
|---|---|---|---|---|---|---|---|---|---|
| Male | Female |
U—Unemployed F—Full time employed P—Part time employed IRR—Irregular employment S—Scholar C—Child at home A—Adult at home |
A—No schooling B—Pre-primary to grade 4 C—Grade 5 to grade 7 D—Grade 8 to grade 10 E—Grade 9 to grade 12 F—Tertiary level U—Unsure |
||||||
| Yes | No | ||||||||
| A1 | |||||||||
| A2 | |||||||||
| A3 | |||||||||
| A4 | |||||||||
| A5 | |||||||||
| A6 | |||||||||
1.2 Are members of the household
Mark the person’s choice (✓)
| South African Citizens | Yes | |
| No | ||
| If no, what is your country of citizenship | ||
| And for how long have you lived in South Africa | ||
Have there been any deaths among the persons living in the house in the past 6 months and if possible please specify the cause?
Mark the person’s choice (✓)
| Yes | Specify: | |
| No |
Section 2: Disease and health services
2.1 During the past two weeks, are there symptoms that affected you or persons living in your house?
| Symptom | Code of person/persons with symptom | Home treatment (✓) | Visited clinic/Doctor (✓) | Is the person still suffering from the symptom (Y/N) |
|---|---|---|---|---|
| Diarrhoea | ||||
| Fever | ||||
| Nausea | ||||
| Vomiting | ||||
| Cramps/abdominal pain | ||||
| Blood in stools or vomit | ||||
| Worms in faeces | ||||
| Body/hand sores | ||||
| Eye infection | ||||
| Coughing | ||||
| Shortness of breath | ||||
| Tiredness and weakness of body | ||||
| Coughing blood | ||||
| Loss of appetite and weight | ||||
| Night sweats | ||||
| Headaches | ||||
| Nits/lice | ||||
| Yellow looking skin | ||||
| White of eyes are yellow | ||||
| Itchy skin | ||||
| Coughing for more than 1 week | ||||
| Other: |
2.2 Have any members of your household visited the clinic and/or doctor in the past two months and been diagnosed with an illness/disease?
| Code of the person | Illness/disease | Was medicine given for the illness? (Y/N) | Is the illness cured? (Y/N) | Have you or any member in your household suffered from the illness before? (Y/N) |
|---|---|---|---|---|
2.3 Are any members of the household on chronic medication?
Mark the person’s choice (✓)
| Yes | |
| No | |
| If yes, specify for what illness |
Note to interviewer: If the answer is yes, ask to see the medication.
2.4 Do you think that people in your household suffer from the following diseases at the moment? (Optional)
Mark the person’s choice (✓)
| Yes | No | Unsure | |
|---|---|---|---|
| TB | |||
| HIV/AIDS |
2.5 What are some of the other health problems facing your household?
| 1. | 2. | 3. |
| 4. | 5. | 6. |
2.6 Do members of your household take part in using the following substances?
Mark the person’s choice (✓)
| Cigarettes | Alcohol | Drugs | |
|---|---|---|---|
| Yes | |||
| No | |||
| Unsure |
2.7 What is the name of the clinic that members of your household visit when ill? ––––––––––––––––––––––––
2.8 How do you get to the clinic?
Mark the person’s choice (✓)
| Walk | |
| Taxi | |
| Bus | |
| Private transport | |
| Other, specify: |
2.9 What does a return trip to the clinic cost (if you need to pay)? R _____, ___
2.10 Has there ever been a time when you or a family member needed to visit the clinic, but did not have the money to pay for transport?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
2.11 Are you satisfied with the services provided by the clinic?
| Mark the person’s choice (✓) | |
| Yes | |
| No | |
| Unsure | |
2.12 Do you think that private health facilities provide better services than your clinic?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
2.13 Have you or members of your household ever called for an ambulance?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
2.14 Usually, how many meals does your family eat per day?
| Ring the person’s choice | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
Section 3: Hygiene and the environment
3.1 Do you think that you can get sick from the following?
Mark the person’s choice (✓)
| Using a dirty toilet | Yes | No | Unsure |
| An unclean home | Yes | No | Unsure |
| Dirt and rubbish in your yard or the street | Yes | No | Unsure |
| Drinking dirty water | Yes | No | Unsure |
| Drinking water from rivers and streams | Yes | No | Unsure |
3.2 Is it difficult to keep your home clean?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
3.3 Do you find it expensive to purchase cleaning material for your home?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
3.4 Have you or any member of your household been a victim of crime in the past six months?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
3.5 Can you mention some of the crime committed in your community?
| 1. | 2. | 3. |
| 4. | 5. | 6. |
3.6 Are there safe places to play for the children in your household?
Mark the person’s choice (✓)
| Yes | |
| No | |
| Unsure |
Notes:________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________________
Thank you for taking the time to answer our questions. Again, any information provided by yourself during the interview will be kept confidential. Your participation in the study is highly appreciated.
| Date of interview: | |||||
| Time of interview: | |||||
| Street Name and House number (This information will be kept strictly confidential) | |||||
| Classify: | Main | House | or | Shack | |
| Suburb: | 1 | 2 | 3 | 4 | |
Appendix B: Housing Evaluation Questionnaire
My name is Thashlin Govender. You are invited to take part in a research project carried out by the Medical Faculty of the University of Stellenbosch. We are studying your health and home. Please note that your participation in the study is voluntary. All answers and comments will be kept highly confidential. We would appreciate it if you could allow us to ask you some questions about your home and have a look at the structure of your house. We will not need your name and we promise that no information you give us will be attached to you or anyone living in your home. Please do not hesitate to ask any questions that you may have regarding this study.
Section 1: Household information
1.1 What is the total income of the household living in the dwelling per month?
| Mark the correct one (✓) | |
| Less than R600 per month | |
| R600 to R1 200 per month | |
| R1200 to R2500 per month | |
| More than R2500 per month | |
| Unsure | |
1.2 What is the dwelling used for?
| Mark the correct one (✓) | |
| Main household accommodation | |
| Additional household accommodation | |
| Rented out accommodation | |
| Business premises | |
| Storage room | |
| Garage | |
| Other: | |
| Other: | |
1.3 Who owns this home?
_________________________
1.4 Does he/she stay here?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
1.5 If you rent the home, how much do you pay per month?
R _____, ___
1.6 Where did you stay prior to moving to this settlement?
1.7 Backyard dwellers only: Have you applied to join the housing list? If yes, how long have you been waiting for a house?
| Mark the correct one (✓) | On waiting list for: | |
| Yes | ––––––– years | |
| No | ––––––– months | |
| Unsure |
1.8 RDP house only: Did you get this home by joining the housing list? If yes, how long ago did you receive this home?
| Mark the correct one (✓) | When did you receive the home? | |
| Yes | ––––––– years | |
| No | ––––––– months | |
| Unsure |
1.9 Who pays for the repairs of this home?
____________________________
1.10 Can you afford the repairs of the home?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
1.11 Do you pay for water to drink and clean your home and if yes, who do you pay?
| Mark the correct one (✓) | Yes | No | Unsure | Recipient of payment: |
| Drink | ||||
| Clean your home |
1.12 Do you pay for electricity and if yes, who do you pay?
| Mark the correct one (✓) | ||
| Yes | Recipient of payment: | |
| No | ||
| Unsure | ||
1.13 Do you (or somebody in your home) receive a social grant?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
Section 2: Toilet facilities
2.1 Where is the toilet for the persons living in this house?
| Mark the correct one (✓) | Primary | Secondary | |
| Toilet inside the house | |||
| Toilet outside the house, but on the same property | |||
| Communal toilet away from the dwelling | |||
| No toilet available within easy walking distance | |||
| If no toilet is available, what do the inhabitants use? | |||
2.2 What sort of toilet is it?
| Mark the correct one (✓) | |
| Flush toilet | |
| Longdrop (pit latrine) | |
| Bucket system | |
| Other, specify: | |
1.3 Does your toilet break or is it blocked often?
Mark the correct one (✓)
| Yes | |
| No | |
| Unsure | |
| Not applicable |
2.4 Where do the members of the household dispose of soiled products, eg, sewage, soiled nappies?
| Please mark ✓ = Yes, ✗ = No | |||
| In the street | Outside bin | ||
| Into the storm water drain | If other, specify: | ||
| Rubbish skip |
2.5 If the toilet is away from the dwelling, how far do the inhabitants have to walk to get to the toilet
Distance:
 paces
paces
2.6 Do you know who to contact if there is a drain blocked or overflowing? If yes, specify
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
2.7 Who would you tell if there is a drain blocked and overflowing?
| 1. | 2. |
2.8 What will happen if rubbish is thrown into the toilet?
| Mark the correct one (✓) | |
| Nothing | |
| It will block the toilet and the pipes | |
| Don’t know | |
2.9 Can you get sick from not washing your hands after you used the toilet?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
2.10 How often is your toilet cleaned?
| Mark the correct one (✓) | |
| Once a day | |
| Twice a week | |
| Once a week | |
| Sometimes | |
| Unsure | |
2.11 What are the cleaning materials used to clean the toilet?
| Please mark ✓ = Yes, ✗ = No | |
| Disinfectant | |
| Soap | |
| Detergent | |
| Toilet brush | |
| Cloth | |
2.12 Do you pay to use the toilet?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
Section 3: Washing and other water use
3.1 Is there a working tap available?
| Mark the correct one (✓) | |
| Inside the house | |
| On the property | |
| Nearby (not on property) | |
3.2 Are there facilities nearby to wash your hands after using the toilet?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
3.3 Where are your clothes washed?
__________________________
3.4 What happens to the water used to wash your clothes?
3.5 When water is used to wash and prepare food, what happens to that water?
3.6 Where do the persons living in the house wash themselves?
3.7 What happens to the wash water?
Section 4: Solid waste
4.1 Where does the household dispose of its rubbish?
| Please mark ✓ = Yes, ✗ = No | |||
| In a rubbish bin inside the house | |||
| At the skip outside on the street | |||
| Throw it on the street | |||
| Other | |||
| If “Other”, please specify: ............................................................................. ...................................................................................................................... ...................................................................................................................... | |||
Section 5: Vector identification
5.1 Have you found any rats, mice or cockroaches in your home?
| Mark the correct one (✓) | |
| Yes | |
| No | |
| Unsure | |
| If yes, specify the type of animal | a) |
| b) | |
| c) | |
Thank you for taking the time to answer our questions. Again, any information provided by yourself during the interview will be kept confidential. Your participation in the study is highly appreciated.
| Date of interview: | |||||
| Time of interview: | |||||
| Street Name and House number (This information will be kept strictly confidential) | |||||
| Classify: | Main | House | or | Shack | |
| Suburb: | 1 | 2 | 3 | 4 | |
| Survey Number: | |||||
Appendix C: Dwelling Checklist
| Survey Number: | ||||||
| Ring the appropriate answer | Comments | |||||
| 1 | Type of dwelling | Main dwelling | Shack in backyard | Other | ||
| 2 | Is the house neatly maintained? | Poor | Fair | Good | ||
| 3 | Are the outside walls of the home painted? | Yes | No | |||
| 4 | Are the inside walls of the home painted? | |||||
| 5 | Are there cracks on the wall? | Yes | No | |||
| 6 | Does the house have electricity? | Yes | No | |||
| 7 | Is the roof of the house leaking? | |||||
| 8 | Is the door well fitted? | Yes | No | |||
| 9 | Does the house have any broken windows? | Yes | No | |||
| 10 | Is the bathroom clean? | Poor | Fair | Good | ||
| 11 | Is the toilet in working order? | Yes | No | |||
| 12 | Is the toilet leaking? | Yes | No | |||
| 13 | Is the tap leaking? | Yes | No | |||
| 14 | Is there toilet paper in the bathroom? | Yes | No | |||
| 15 | Is there soap available in the bathroom to wash hands? | Yes | No | |||
| 16 | Is there a clean towel or paper towels available in the bathroom? | Yes | No | |||
| 17 | Is the drain clean? | Poor | Fair | Good | ||
| 18 | Is the roof leaking? | Yes | No | |||
| 19 | Are there any structural damages to the home? | Yes | No | |||
| 20 | Are there any structural alterations or extensions to the home? | Yes | No | |||
| 21 | What is the state of the yard outside the home? | Poor | Fair | Good | ||
| 22 | Is there a bin inside the home? | Yes | No | |||
| 23 | Is there a bin outside the home? | Yes | No | |||
| 24 | Is there a garden outside the home? | Yes | No | |||
| 25 | Is rubbish evident outside the home? | Yes | No | |||
| 26 | Are there pools of water outside the home? | Yes | No | |||
| 27 | Is there broken glass evident outside the home? | Yes | No | |||
| 28 | Does the family own pets/animals? | Yes | No | |||
| 29 | Does the home have electricity? And if yes, is it legal or illegal? | Yes | No | Legal | Illegal | |
| 30 | Is there evidence of other forms of heating/lighting? | Yes | No | |||
| 31 | Does the home have an operational refrigerator? | Yes | No | |||
| 32 | Does the home have an operational stove? | Yes | No | |||
Appendix D: Participant Information Leaflet and Consent Form
TITLE OF THE RESEARCH PROJECT:
An epidemiological study on the health and sanitation status of specific low cost housing communities as contrasted with those occupying ‘backyard dwellings’ in the City of Cape Town, South Africa.
REFERENCE NUMBER: N09-08-214/215/216.
PRINCIPAL INVESTIGATOR: Thashlin Govender, PhD Candidate, Division of Community Health, Department of Interdisciplinary Health Sciences, Faculty of Health Science, Tygerberg Campus, Stellenbosch University.
ADDRESS: 55 Carnie Road, Rylands Estate, Cape Town, 7764.
CONTACT NUMBER: 083 730 2846.
You are being invited to take part in a research project. Please take some time to read the information presented here, which will explain the details of this project. Please ask the study staff or doctor any questions about any part of this project that you do not fully understand. It is very important that you are fully satisfied that you clearly understand what this research entails and how you could be involved. Also, your participation is entirely voluntary and you are free to decline to participate. If you say no, this will not affect you negatively in any way whatsoever. You are also free to withdraw from the study at any point, even if you do agree to take part.
This study has been approved by the Committee for Human Research at Stellenbosch University and will be conducted according to the ethical guidelines and principles of the international Declaration of Helsinki, South African Guidelines for Good Clinical Practice and the Medical Research Council (MRC) Ethical Guidelines for Research.
What is this research study all about?
A total of 50 homes with a plot number will be randomly selected to take part in the study. The reason for us doing the study is to investigate the health of the people in your community and the water use and sanitation in your home. There are two parts to the study that we need your assistance with. Firstly, we will ask you questions about your home and your water use and sanitation. For this part of the survey we will also take a look around your home. You may accompany us during this part of the survey. Secondly, a nurse will ask you some questions about the health of your family. These surveys will be done for your home alone. We will be taking down your address, but we will not be taking down any names of you and your family in the interview. This is done so that no one will be able to identify from whom the information was obtained and who is sick or who became ill in your home. This consent form will not be attached to your answer sheet, so that again no one will be able to find out that this information was provided by you. Once you have completed this consent form, this form will be placed in a sealed box together with all the other forms from your community, for safety purposes. A report of the findings from the study will be sent to your ward councilor, and we will try to make the information available in a community newspaper. We will also send a report to the City of Cape Town offices, so that they know about the living conditions in your community and the problems that you and your community are faced with. You can contact Dr J.M Barnes at 021-9389480 if you have any questions or problems or would like to know the results of this study. You may also contact the Committee for Human Research at Stellenbosch University at 021-938 9207 if you have any concerns or complaints. You will receive a copy of this information and consent form for your own records.
Why have you been invited to participate?
You have been selected by chance so that the information we gather is a fair representation of your community. We want to investigate the health status of you and your family and the living conditions in and around your environment.
What will your responsibilities be?
To please answer the questions as best as you can.
Will you benefit from taking part in this research?
The results from this study will be summarised and provided to the local, provincial and national government in order to improve planning for housing and health. The results will help us understand the needs of your community and environment.
Are there any risks involved in your taking part in this research?
There are no risks involved in taking part in the study. And we assure you of your anonymity.
If you do not agree to take part, what alternatives do you have?
YOU HAVE A RIGHT TO NOT TAKE PART OR STOP THE INTERVIEW; AND THERE WILL BE NO IMPLICATIONS IF THIS IS YOUR DECISION.
DECLARATION BY PARTICIPANT
By signing below, I ................................................... agree to take part in a research study entitled, An epidemiological study on the health and sanitation status of specific low cost housing communities as contrasted with those occupying ‘backyard dwellings’ in the City of Cape Town, South Africa.
I declare that:
I have read or had read to me this information and consent form and it is written in a language with which I am fluent and comfortable.
I have had a chance to ask questions and all my questions have been adequately answered.
I understand that taking part in this study is voluntary and I have not been pressurised to take part.
I may choose to leave the study at any time and will not be penalised or prejudiced in any way.
I may be asked to leave the study before it has finished, if the study doctor or researcher feels it is in my best interests, or if I do not follow the study plan, as agreed to.
I have given permission to take and use pictures of my home and family members for publication purposes.
Signed at (place) ................... on (date) ....................... 2009.
...................................................... ................................................................
Signature of participant Signature of witness
DECLARATION BY INVESTIGATOR
I (name)............................................ declare that:
I explained the information in this document to ..................
I encouraged him/her to ask questions and took adequate time to answer them.
I am satisfied that he/she adequately understands all aspects of the research, as discussed above.
I did/did not use a interpreter. (If an interpreter is used then the interpreter must sign the declaration below).
Signed at (place) .................. on (date) ..................... 2009.
............................................... .......................................................................
Signature of investigator Signature of witness
Declaration by interpreter
I (name) ............................................ declare that:
I assisted the investigator (name) ............................... to explain the information in this document to (name of participant) ................................. using the language medium of Afrikaans/Xhosa.
We encouraged him/her to ask questions and took adequate time to answer them.
I conveyed a factually correct version of what was related to me.
I am satisfied that the participant fully understands the content of this informed consent document and has had all his/her question satisfactorily answered.
Signed at (place) .................................................. on (date) ...........................
............................................................ ...........................................................
Signature of interpreter Signature of witness
Footnotes
Disclosure
This manuscript has been read and approved by all authors. This paper is unique and is not under consideration by any other publication and has not been published elsewhere. The authors and peer reviewers of this paper report no conflicts of interest. The authors confirm that they have permission to reproduce any copyrighted material.
References
- 1.Shaw M. Housing and Public Health. Annual Review of Public Health. 2004;25:397–418. doi: 10.1146/annurev.publhealth.25.101802.123036. [DOI] [PubMed] [Google Scholar]
- 2.Thomson H, Petticrew M, Morrison D. Health effects of housing improvement: systematic review of intervention studies. British Medical Journal. 2001;323:187–90. doi: 10.1136/bmj.323.7306.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.City of Cape Town, Department of Housing Breaking New Ground, Comprehensive plan for housing delivery. Downloaded on 6 March 2010. Available from: http://web.wits.ac.za/NR/rdonlyres/CF05F3D4-DFDC-49DD-9776-D924A89AB9D7/0/BreakingNewGroundHousingPlanCabinetapprovedversion.pdf.
- 4.Rauh VA, Landrigan PJ, Claudio L. Housing and Health, Intersection of Poverty and Environmental Exposures. Annals of the New York Academy of Science. 2008;1136:276–88. doi: 10.1196/annals.1425.032. [DOI] [PubMed] [Google Scholar]
- 5.World Health Organization Health Principles of Housing. 1989. Downloaded on 10 January 2010. Available from: http://whqlibdoc.who.int/publications/1989/9241561270_eng.pdf.
- 6.Brown VJ. Give me Shelter: the global housing crisis. Environmental Health Perspectives. 2003;111:A92–9. doi: 10.1289/ehp.111-a92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Burden of disease in DALYs by cause, sex and mortality stratum in WHO regions. 2002. Downloaded on 8 December 2009. Available from: http://www.who.int/whr/2003/en/Annex3-en.pdf.
- 8.Graham JP, Corella-Barus V, Avitia-Diaz R, Gurian P. The in-home environment and household health: A cross-sectional study of informal urban settlements in Northern Mexico. International Journal of Environmental Research and Public health. 2005;2:394–402. doi: 10.3390/ijerph2005030003. [DOI] [PubMed] [Google Scholar]
- 9.Lemanski C. Augmented informality: South Africa’s backyard dwellings as a by-product of formal housing policies. Habitat International. 2009;33:472–84. [Google Scholar]
- 10.Morange M. Backyard shacks: The relative success of this housing option in Port Elizabeth. Urban Forum. 2002;13:3–25. [Google Scholar]
- 11.Crankshaw O, Gilbert AG, Morris A. Backyard Soweto. International Journal of Urban and Regional Research. 2000;24:841–57. [Google Scholar]
- 12.Bank L. The rhythms of the yards: urbanism, backyards and housing policy in South Africa. Journal of Contemporary African studies. 2007;25:205–28. [Google Scholar]
- 13.World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. 2000. Downloaded on 26 July 2009. Available from: http://www4.ensp.fiocruz.br/etica/docs/artigos/Helsinq.pdf. [PubMed]
- 14.Republic of South Africa, Department of Health Guidelines for Good Clinical Practice in the Conduct of Clinical Trials in Human Participants in South Africa. 2000. Downloaded on 24 August 2009. Available from: http://www.doh.gov.za/docs/policy/trials/trials_01.html.
- 15.South African Press Association Role-players to brainstorm housing crisis—Sexwale. Cape Times. Apr 23, 2010. p. 9.
- 16.Godwin Y, Hudson DA, Bloch CE. Shack fires: a consequence of urban migration. Burns. 1997;23:151–3. doi: 10.1016/s0305-4179(96)00118-0. [DOI] [PubMed] [Google Scholar]
- 17.Godfrey L. Facilitating the improved management of waste in South Africa through a national waste information system. Waste Management. 2008;28:1660–71. doi: 10.1016/j.wasman.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 18.Govender T, Barnes JM, Pieper CH. Housing conditions, sanitation status and associated health risks in selected subsidized low-cost housing settlements in Cape Town, South Africa. Habitat International. 2010;35:335–42. [Google Scholar]
- 19.Armitage NP, Winter K, Spiegel A, Kruger E. Community-focused greywater management in two informal settlements in South Africa. Water Science Technology. 2009;59:2341–50. doi: 10.2166/wst.2009.294. [DOI] [PubMed] [Google Scholar]
- 20.Carden K, Armitage N, Winter K, Sichone O, Rivett U. The management of greywater in the non-sewered areas of South Africa. Urban Water Journal. 2008;5:329–43. [Google Scholar]
- 21.Parkinson J. Drainage and storm water management strategies for low-income urban communities. Environment and Urbanization. 2003;15:115–26. [Google Scholar]
- 22.Keraita B, Drechsel P, Philip A. Influence of urban waste water on stream water quality and agriculture in and around Kumasi, Ghana. Environment and Urbanization. 2003;15:171–8. [Google Scholar]
- 23.Palamuleni LG. Effect of sanitation facilities, domestic solid waste disposal and hygiene practices on water quality in Malawi’s urban poor areas: a case study of South Lunzu Township in the city of Blantyre. Physics and Chemistry of the Earth. 2002;27:845–50. [Google Scholar]
- 24.Republic of South Africa, Department of Health The National HIV and Syphilis Prevalence survey South Africa 2007. Downloaded on 2 March 2010. Available from: http://www.doh.gov.za/docs/reports/2007/hiv/part1.pdf.
- 25.Singh JA, Upshur R, Padayatchi N. XDR-TB in South Africa: Not time for denial or complacency. PLoS Medicine. 2007;4:19–25. doi: 10.1371/journal.pmed.0040050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Moraes LRS, Cancio JA, Caincross S, Huttly S. Impact of drainage and sewerage on diarrhoea in poor urban areas in Salvador, Brazil. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2003;97:153–8. doi: 10.1016/s0035-9203(03)90104-0. [DOI] [PubMed] [Google Scholar]
- 27.Eng TR, Maxfield A, Patrick K, Deering MJ, Ratzan SC, Gustadson DH. Access to health information and Support: A public highway or a private road? Journal of American Medical Association. 1998;280:1371–5. doi: 10.1001/jama.280.15.1371. [DOI] [PubMed] [Google Scholar]
- 28.Barnett R. Coping with the costs of primary care? Household and locational variations in the survival strategies of the urban poor. Health and Place. 2001;7:141–57. doi: 10.1016/s1353-8292(01)00013-2. [DOI] [PubMed] [Google Scholar]
- 29.Haddad S, Fournier P, Machouf N, Yatara F. What does quality mean to lay people? Community perceptions of primary health care services in Guinea. Social Sciences and Medicine. 1998;47:381–94. doi: 10.1016/s0277-9536(98)00075-6. [DOI] [PubMed] [Google Scholar]
- 30.Corburn J. Confronting the challenges in reconnecting urban planning and public health. American Journal of Public Health. 2004;94:541–6. doi: 10.2105/ajph.94.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Govender T, Barnes JM, Pieper CH. Living in low-cost housing settlements in Cape Town, South Africa—the epidemiological characteristics associated with increased health vulnerability. Journal of Urban Health. 2010;87:899–911. doi: 10.1007/s11524-010-9502-0. [DOI] [PMC free article] [PubMed] [Google Scholar]