Abstract
Traditional exercise programs for older adults may not be suitable for frail, deconditioned nursing home residents with AD. Adaptations for this population include self-paced walking, use of assistive devices, rest as indicated, redirection when distracted, and engagement in conversation to increase willingness to participate. Appropriate footwear, monitoring response to the exercise, removal of fall hazards and use of a gait belt are suggested. Two studies of the effect of a program of regularly scheduled assisted walking on mobility and function of nursing home residents with AD are reported. Results of the first study suggest that participation in a walking exercise program can contribute to maintenance of mobility and that willingness to participate is significantly enhanced by development of a relationship with the intervenor. Preliminary results from the second study suggest that ability to perform the basic activities of daily living may also be supported by this type of exercise.
Keywords: Exercise, Walking, Mobility, Function, Alzheimer's Disease
Although older adults' capacity to benefit from exercise is well documented, traditional approaches to exercise have met with limited acceptability and/or effectiveness in individuals with Alzheimer's disease (AD). This is particularly true of those who are in nursing homes where chronic inactivity can exacerbate the effects of the disease on mobility and functional independence1. When the effects of advanced age, disease progression and disuse are combined, they can hasten the cascade of events that will eventually leave the individual immobile and dependent on others2. Participation in an exercise program, on the other hand, may substantially delay immobility and functional dependence.
Walking is a natural, overlearned behavior which increases the potential for acceptability of the exercise program in a cognitively impaired population. With adequate monitoring, most frail, deconditioned nursing home residents with AD who are still mobile can safely engage in a walking program.
In this article, we describe the results of a walking exercise program for nursing home residents with AD. Adaptations that increase participants' willingness to walk and safety precautions are also described. A study in which assisted walking was compared to conversation and a combination of walking and conversation has been completed (Study I). A second study in which walking is compared to a combination of exercises and a social conversation control group is presently underway (Study II).
Study I
Method
A sample of 65 nursing home residents with clinically diagnosed AD based on the NINCDS-ADRDA criteria were randomly assigned to one of three treatment groups: assisted walking, assisted walking with conversation and conversation alone. Reflecting the community nursing home population in the U.S., the majority of the sample were women (84%). Their average age was 87 (range 70 to 105) and their average Mini-Mental score was 10.83 with a range of 0 to 23.
Participants in the walking group walked with an intervenor at their own pace for as much of the 30 minute treatment sessions as they could. Rest was allowed as requested or as indicated. Those in the walking without conversation group were not actively engaged in conversation during the session but intervenors did respond to any attempts to converse. Participants in the conversation group were engaged in discussion of their present day experiences and concerns by the intervenors. Those in the walking with conversation group were walked for as much of the 30 minutes as tolerated and simultaneously engaged in conversation simultaneously3.
Results
Those participants who were engaged in conversation during the walking session completed 75% of the sessions while those who walked without conversation completed only 57% of the sessions. Furthermore, the walking with conversation group virtually maintained their pretest level of mobility (as measured by the distance walked in 6 minutes4) while those who were not engaged in conversation during their walk declined 21%, similar to the conversation control group's 19% decline (Figure 1). These differences were significant at the p = .01 or better level of significance3.
Figure 1.
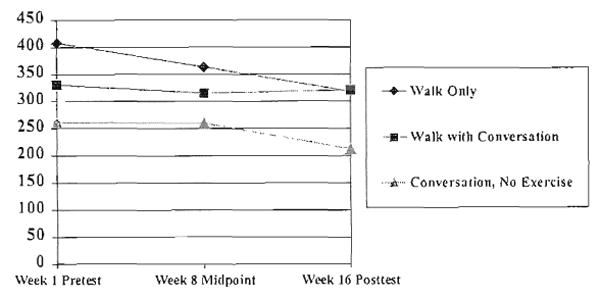
Comparison Of Walking, Walking With Conversation And Conversation Alone Over 16 Week Treatment Period (Distance in Feet)
From these results we can draw several conclusions: 1) those who were not walked experienced a decline in mobility 2) those who walked were more likely to retain their level of mobility than those who did not engage in this exercise 3) higher levels of adherence to the walking program led to better maintenance of mobility and 4) development of a relationship with the intervenor is a critical factor in achieving adherence to the walking program.
Study II
Method
In this current study, nursing home residents with clinically diagnosed AD based on the NINCDS-ADRDA criteria are randomly assigned to one of three different treatment groups: walking, a combination of walking and other exercises and social conversation. All exercisers are engaged in conversation in this study because conversation had contributed substantially to adherence in the earlier study. Ninety-one percent of the sample are female. Their average age is 86.5 (range 73 to 102) and their average Mini-Mental score is 7.78 (range 0 to 25).
Results
A comparison of the walking group (n = 9) with the conversation group (n = 10) indicates a significant difference in both distance walked in 6 minutes (F 9.39, p = .0074) and in ability to perform the basic activities of daily living as measured by the Physical Self-Maintenance Scale (F 4.93, p = .01)5. Data on the effect of the combination of walking and other exercise are too limited to report at this time. Although still preliminary, these results suggest that walking exercise may contribute to maintenance of function as well as mobility.
Adaptations For This Population
Safety Precautions
During the treatment sessions, participants used whatever assistive device had been recommended for them prior to entering the study. In addition, a gait belt was used with all walkers. It was sometimes necessary to clear the pathway of hazards-objects on the floor or in the pathway of the person walking-or to guide the person around them. Appropriate footwear and clothing can also reduce the risk of fall or injury. Vital signs were taken before and after the treatment session and intervenors (all registered nurses) were expected to monitor participants for signs of excessive fatigue or other distress. If these occurred, they were reported to the nursing home staff
Increasing Adherence to the Program
The intervenors noted that participants were easily distracted and often had to be redirected to continue walking. Residents were encouraged to express a preference for the route taken during the walk. The opportunity to go outdoors or to peer out a large picture window added to the pleasure derived from the experience. Those who were afraid of falling were reassured by the use of a guiding hand or arm for support in addition to the gait belt. Several wanted their wheelchair nearby for security, “just in case I need it.” Those who became ill or injured were remobilized as soon as possible after the acute episode to counter the effects of disuse that can accumulate rapidly in a deconditioned population.
Discussion
The results of these studies suggest that mobility of nursing home residents with AD can be maintained over 16 weeks by consistent participation in a walking exercise program. There is also some preliminary evidence that ability to perform the basic activities of daily living may be supported by participation in a regular walking exercise program. Mindfulness of safety precautions and environmental hazards is the responsibility of the intervenor, as is constant monitoring of the resident's response to the activity and level of fatigue. Residents who have experienced falls are often fearful; hands-on guidance in addition to the gait belt affords a sense of security as the patient begins his or her walk about the unit or outdoors.
Residents set their own pace, rest when fatigued, and are encouraged to keep going when distracted. They are given choices and actively participate in choosing the route of the walk. By respecting the resident's choice, the intervenor demonstrates respect for the individual and consideration of his or her need for dignity and respect. The intervenors also engaged each resident in adult level conversation to the extent possible, encouraging the resident to talk about his or her recent experiences, interests and concerns and responding in a respectful, noncondescending manner. This frames the intervention with an interpersonal connection between patient and intervenor that is based on trust, patience and caring.
The relationship that develops between resident and intervenor appears to be a key factor in the success of a walking exercise program. Coming to know the resident as a person, understanding the nuances of his or her behavior and responding to the needs of the person with genuine caring appears to have increased their willingness to participate in the exercise program and thereby contributed to maintenance of their mobility and, possibly, function.
A well supervised, carefully monitored person-centered walking exercise program may make a substantial contribution to the physical mobility, function and, ultimately, the quality of life of nursing home residents with Alzheimer's disease.
Acknowledgments
Funding Sources: National Institute of Health, National Institute of Nursing Research, Grant #R01 NR04176 Exercise Effect on Function of Residents with AD, Principal Investigator: Ruth M. Tappen, EdD, RN, FAAN.
National Institutes of Health, National Institute of Nursing Research, Grant #R01 NR03322 Activity Vs Discourse to Improve Communication in AD, Principal Investigator: Ruth M. Tappen, EdD, RN, FAAN.
Contributor Information
Ruth M. Tappen, Christine E. Lynn Eminent Scholar and Professor, Florida Atlantic University College of Nursing, 777 Glades Road, Boca Raton, FL 33431-0991, Telephone: 561-297-3188, Fax: 561-297-2170, email: rtappen@fau.edu.
Patricia P. Kronk, Florida Atlantic University College of Nursing.
References
- 1.Perrin T. Occupational need in severe dementia: A descriptive study. Journal of Advanced Nursing. 1997;25(5):934–941. doi: 10.1046/j.1365-2648.1997.1997025934.x. [DOI] [PubMed] [Google Scholar]
- 2.Spirduso WW. Physical Dimensions of Aging. Champaign, ILL: Human Kinetics; 1995. [Google Scholar]
- 3.Tappen RM, Roach KE, Applegate EB, Stowell P. Effect of a combined walking and conversation intervention on functional mobility of nursing home residents with Alzheimer Disease. Alzheimer Disease and Associated Disorders. 2000 Fall;14(4) doi: 10.1097/00002093-200010000-00002. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tappen R, Roach K, Buchner D, Barry C, Edelstein J. Reliability of Physical Performance Measures in nursing home residents with Alzheimer's Disease. The Journals of Gerontology Medical. 1997;52A(1):M52–55. doi: 10.1093/gerona/52a.1.m52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawton MP, Brody EM. Assessment of older people: Self-Maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]


