Abstract
Background
Malnutrition is prevalent among patients within certain cancer types. There is lack of universal standard of care for nutrition screening, lack of agreement on an operational definition and on validity of malnutrition indicators.
Objective
In a secondary data analysis, we investigated prevalence of malnutrition diagnosis by three classification methods using data from medical records of a National Cancer Institute (NCI)-designated comprehensive cancer center.
Interventions/Methods
Records of 227 patients hospitalized during 1998 with head and neck, gastrointestinal or lung cancer were reviewed for malnutrition based on three methods: 1) physician diagnosed malnutrition related ICD-9 codes; 2) in-hospital nutritional assessment summary conducted by Registered Dietitians; and 3) body mass index (BMI). For patients with multiple admissions, only data from the first hospitalization was included.
Results
Prevalence of malnutrition diagnosis ranged from 8.8% based on BMI to approximately 26% of all cases based on dietitian assessment. Kappa coefficients between any methods indicated a weak (kappa=0.23, BMI and Dietitians and kappa=0.28, Dietitians and Physicians) to fair strength of agreement (kappa=0.38, BMI and Physicians).
Conclusions
Available methods to identify patients with malnutrition in an NCI designated comprehensive cancer center resulted in varied prevalence of malnutrition diagnosis. Universal standard of care for nutrition screening that utilizes validated tools is needed.
Implications for Practice
The Joint Commission on the Accreditation of Healthcare Organizations requires nutritional screening of patients within 24 hours of admission. For this purpose, implementation of a validated tool that can be used by various healthcare practitioners, including nurses, needs to be considered.
INTRODUCTION
Malnutrition has been shown to be a common problem in hospitalized patients for more than 30 years 1–5 and is highly prevalent among head and neck, lung and gastrointestinal cancer patients6–9. There is no consistent standard of care for nutrition screening in inpatient or outpatient oncology settings to date. Compounding this issue is the lack of universal agreement on the operational definition of malnutrition and on the validity of the assessment indicators 10. Approximately 20% to 80% of cancer patients become malnourished during their clinical course 6, 11–14. Currently, most of the nutrition screening in oncology settings is completed by nursing professionals, but not all of the methods used for this purpose have been validated 15.
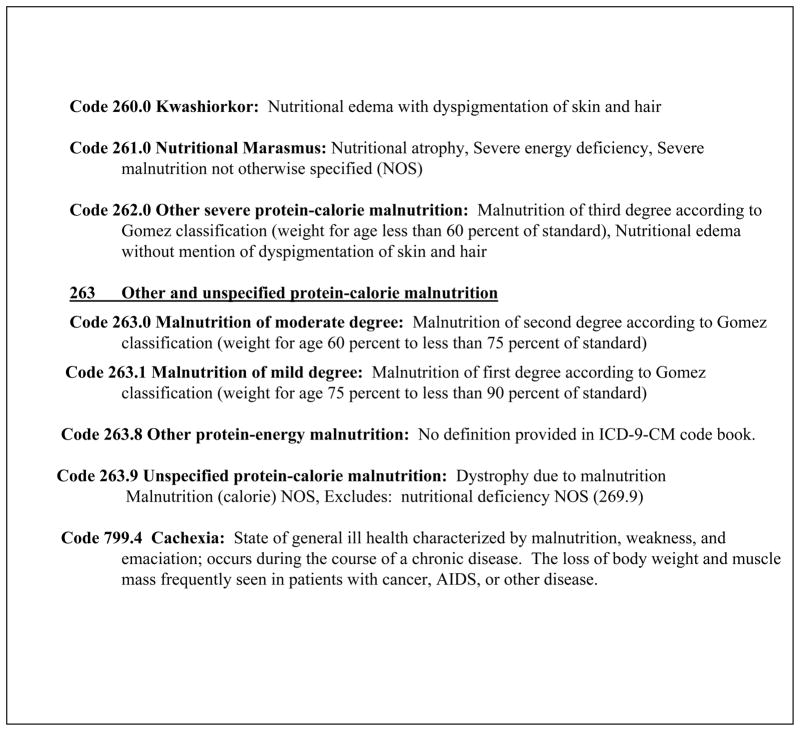
Examinations of malnutrition in patient populations have used weight loss as the primary indicator of malnutrition - specifically, involuntary weight loss of greater than 10% 16. Other indicators used in the assessment of malnutrition include serum albumin and body mass index (BMI) 10, 17, 18. Physicians utilize the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) which includes major diagnoses of malnutrition 19. The malnutrition-related diagnoses, including cachexia, coded by the ICD-9-CM are displayed in Figure 1. As Swails et al. stated in 1996, these descriptions were based on primary malnutrition in the pediatric populations of less-developed countries, and therefore should not be used as a standard reference for hospitalized adults in industrialized populations 20. A new coding system, the ICD-10 has been in place in countries other than the United States since 1994, but accurate, universally-accepted and clinically relevant classifications of malnutrition are still lacking 21.
FIGURE 1.
Malnutrition Related ICD-9-CM Codes21
To date the condition of malnutrition remains under diagnosed in hospitalized patients 5–9. This is due to several factors including a lack of a universal standard of care for malnutrition screening, lack of agreement on the operational definition of malnutrition, and lack of the use of validated screening methods. Nursing professionals are usually responsible for nutrition screening in the oncology setting. They cannot work effectively with nutrition professionals to manage malnutrition if it is not identified. Additionally, due to the inconsistency of methods used for nutrition screening in oncology settings, the incidence of malnutrition cannot be determined accurately within cancer centers. The impact of this dilemma therefore remains understated and healthcare resources are not made available to manage this issue.
The primary framework guiding this research is consistent with the framework that guided the parent study and is the quality health outcomes model developed by the American Academy of Nursing Expert Panel on Quality of Health 22. This model proposes that interventions affect and are affected by characteristics of the system and the client to produce outcomes. The components of the quality health outcomes model are reciprocal, that is there are feedback relationships between components. Specifically for this study, the outcome is the prevalence of malnutrition diagnosis in certain cancer populations. Using data from medical records of a National Cancer Institute (NCI)-designated comprehensive cancer center, the prevalence of malnutrition diagnosis was investigated using three available classification methods. Hospitalization records of 227 patients hospitalized during a one year period in 1998 with either head and neck, gastrointestinal or lung cancer were examined. The aims of this secondary data analysis were to (1) compare prevalence of malnutrition diagnosis as identified by three methods and (2) determine agreement of clinical judgment between physicians, dietitians and BMI criteria for the identification of malnutrition in these patients.
METHODS
Study Design
Retrospective data were obtained from hospital medical records of an NCI-designated comprehensive cancer center by trained data extractors for this secondary analysis. In the parent study, three large data sets of cancer patients were analyzed for the impact of malnutrition on health care costs. All medical records of adult persons hospitalized during 1998 that had a diagnosis of lung, gastrointestinal or head and neck cancer were selected. Patient data including diagnosis and stage of cancer and treatment type were collected. The original population contained 393 patients. After the selection criteria were applied, 227 patients were eligible for this study. In the case that a patient had multiple hospitalizations (n=45), the first hospitalization meeting the inclusion criteria was used for analysis. The inclusion criteria for this study required that the medical record for each hospitalization contain, at a minimum, a completed nutrition assessment with documented height, weight before or at the day of the nutrition assessment and serum albumin values. The 166 patient records eliminated had one or more of these indicators missing. The most frequent missing indicator was serum albumin. Exclusion criteria included patients under the age of 18 and patients without a diagnosis of lung, gastrointestinal or head and neck cancer.
Measures of Malnutrition
Three available methods to identify malnutrition among patients in this comprehensive cancer center were selected for comparison: ICD-9 malnutrition codes determined by physicians, in-hospital nutritional assessment summaries by staff Registered Dietitians, and body mass index (BMI) of patients.
ICD-9 Codes
For each discharge, the responsible physician documented all of the primary and secondary discharge diagnoses in the medical record and these were assigned ICD-9 codes by staff coders. If ICD-9 codes ranging from 260.0 to 263.9 or code 799.4 were found, the case was designated as malnourished (see Figure 1). Coding for cachexia (799.4) was included in this study, as cachexia and malnutrition share clinical components such as abnormal BMI values.
For quite a long period of time there has been a lack of consensus regarding the exact meaning of malnutrition. In 2008, an operational definition was published stating that malnutrition is “a subacute or chronic state of nutrition in which a combination of varying degrees of over-or undernutrition and inflammatory activity has led to a change in body composition and diminished function” 23. Prolonged malnutrition may result in cachexia 10. Cachexia involves an increase in tissue catabolism, impaired anabolism along with the release of tumor derived catabolic factors, neuroendocrine dysfunction and the presence of inflammatory cytokines 24, 25. Cachexia is not overturned by nutrition support alone and requires the use of anti-cachexia agents to affect the proteolysis, lipolysis, anorexia, inappropriate increased resting energy expenditure and the acute phase response 26. Since some of the criteria used to determine malnutrition might also be used for cachexia, this endpoint was included in the investigation.
In-Hospital Nutritional Assessment Summaries
It was a policy of the NCI-designated comprehensive cancer care center that a nutrition assessment be completed by a Registered Dietitian and included in the medical record of every inpatient. Staff dietitians classified the nutritional status of patients as “adequate”, “at risk” or “compromised” based on institutional criteria. Criteria for establishing nutritional status of patients included the consideration of clinical ranges for indicators such as percentage of ideal body weight, body mass index (BMI), serum albumin values and clinical symptoms such as mucositis and dysphagia. Dietitians used clinical judgment in reviewing these indicators and determined nutritional status. Cases identified as “compromised” were designated as malnourished for this investigation.
Body Mass Index
Weight and height for each patient was extracted from the medical record. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Values below 18.5 were interpreted as malnourished as described by Heymsfield et al. 16.
Procedures
Three nursing students and one clinical dietetic intern were trained to extract data from the medical records. After several practice sessions, interrater reliability was tested and 90% agreement was achieved. Interrater agreement was also tested midway through data collection with 90% agreement. The medical records staff of the comprehensive cancer center identified all adult patients with cancer diagnoses of head and neck, gastrointestinal and lung. Data were entered into the database and entries were verified by other trained staff. The study was approved by the University at Buffalo Health Science IRB after receiving administrative approval from the designated comprehensive center, an affiliate of the University at Buffalo
Statistical Analyses
The Statistical Package for Social Scientists (SPSS, version 11) was used for all statistical analyses. Descriptive analyses examining prevalence, means and standard deviations for the height, weight, BMI and serum albumin measurements of the population were used to summarize the data. The percent agreement for the prevalence of malnutrition using the different diagnostic methods was compared for all cases combined using the kappa statistic. The kappa statistic describes the amount of agreement that exceeds the agreement that would be expected by chance. The kappa statistic ranges from 0 (no additional agreement) to 1 (perfect agreement).
RESULTS
Patient Characteristics and Description of Nutritional Status
Of the 227 patients that met the selection criteria, 56% were males and 44% were females. The primary cancer diagnoses were as follows: 46% gastrointestinal, 39% lung and 15% head and neck. Approximately 20% had in situ or local stage of disease, 36% had regional stage of disease (in or near primary organ site), 40% had metastatic disease and stage was unknown for 4%. A summary of indicators of nutritional status can be found in Table 1. The average BMI and albumin was 25.1 kg/m2 (± 5.7) and 3.2 g/dl (± 0.6) respectively.
Table 1.
Descriptive Statistics of Nutritional Status Indicators
| Indicator | N | Mean | Standard Deviation | Minimum | Maximum |
|---|---|---|---|---|---|
| Height (cm) | 227 | 168.2 | 10.3 | 140.0 | 188.0 |
| Weight (kg) | 227 | 71.1 | 17.5 | 37.0 | 132.6 |
| Body Mass Index (kg/m2) | 227 | 25.1 | 5.7 | 13.8 | 54.6 |
| Albumin (g/dl) | 227 | 3.2 | 0.6 | 1.5 | 4.8 |
Comparison of Prevalence of Malnutrition Diagnosis by Classification Methods
Using the different classification methods, the prevalence of malnutrition diagnosis for all cases combined ranged from 9.3% for ICD-codes to approximately 26% based on dietitian assessments. Among patients identified with malnutrition by physicians using ICD-9 codes, 6 were coded with 263.9 (unspecified protein-calorie malnutrition), 2 each were coded with 261.0 (nutritional marasmus) and 263.1 (malnutrition of mild degree) and one each was coded with 262.0 (other severe protein-calorie malnutrition) and 263.0 (malnutrition of moderate degree). Another 11 patients were coded with 799.4 (cachexia). One of these 11 patients was additionally coded with 261.0 and another was additionally coded with 263.9. Among specific cancer types, the prevalence of malnutrition diagnosis also varied by classification method. Dietitian assessments identified most of the malnutrition cases for each type of cancer (Table 2).
Table 2.
Prevalence of Malnutrition Diagnosis based on Three Classification Methods by Cancer Diagnosis
| Cancer Type | ||||
|---|---|---|---|---|
| Diagnosis Method | Any n=227 n (%) | Gastrointestinal n=104 n (%) | Lung n=89 n (%) | Head and Neck n=34 n (%) |
| ICD-code | 21 (9.3) | 7 (6.7) | 11 (12.4) | 3 (8.8) |
| Dietitian | 59 (26.0) | 27 (26.0) | 22 (24.7) | 10 (29.4) |
| BMI | 20 (8.8) | 8 (7.7) | 11 (12.4) | 1 (2.9) |
When comparing the different methods with each other for all cases, the agreement in malnourished diagnoses was calculated using a kappa statistic (Table 3). The kappa coefficients between any methods indicated a weak (kappa=0.23 for agreement between BMI and Dietitians and kappa=0.28 for agreement between Dietitians and Physicians) to fair strength of agreement (kappa=0.38 for agreement between BMI and Physicians) at best.
Table 3.
Frequency of Agreement in Identification of Malnutrition (Kappa Statistic)
| Physician | Dietitian | BMI | |
|---|---|---|---|
| Physician | 21 (1.00) | ||
| Dietitian | 15 (0.28) | 59 (1.00) | |
| BMI | 9 (0.38) | 13 (0.23) | 20 (1.00) |
DISCUSSION
There is no universal or commonly shared method for identifying those who are malnourished among cancer patients, yet malnutrition is associated with decreased survival in these patients 8, 9, 27. We investigated the differences in the prevalence of malnutrition diagnosis by available classification methods in a comprehensive cancer setting.
The differences between the identification of malnutrition by the three methods in this study are notable. There was a three -fold difference in prevalence of malnutrition diagnosis, depending on the particular measure used. BMI based identification of malnutrition resulted in the lowest prevalence, which is closely followed by physician based identification (ICD-9 codes) of malnutrition. The advantage of using BMI as a classification tool is that one only needs values for height and weight, which are routinely measured and examined in acute care settings 28, 29. Unfortunately, BMI is not sensitive enough to detect differences in body composition, relevant biochemical markers, and changes in energy expenditure or functions of body systems and it has been recommended that more than two nutritional indicators be used to determine malnutrition in patients 16, 17, 30. Additionally, the cut-off point of less than18.5 kg/m2 for malnutrition may be too low to capture all of those who are truly malnourished and some researchers have recommended a malnutrition cut off point of less than 20.0 kg/m2 31. Furthermore, given that the prevalence of abnormal BMI measures in the population is high due to overweight status and obesity, the use of BMI to truly detect malnutrition may be difficult especially with a one-time measure. The average BMI for this group of patients was 25.1. Involuntary weight loss of greater than 10% is a much more sensitive measure of malnutrition and the onetime measure of BMI is not sensitive to the history of unplanned weight loss 16. Unfortunately, we only had information concerning weight loss for approximately 21% of the population.
Dietitians identified more than three times as many cases of malnutrition as physicians based on institutional criteria and subjective judgment, neither of which is a validated method. In the nutrition assessment process, dietitians used serum albumin as one of the criteria for determining nutritional status, however serum albumin is sensitive to dilution effects and can be affected by the primary disease, by the treatment and by related conditions rather than by malnutrition 16. Additionally, one of the criteria for dietitians to consider in assessing nutritional status is BMI and this may have confounded results; however we are not sure to what extent BMI was considered as a factor in assessing nutritional status by the dietitian as each determination was based on subjective clinical judgment. In institutional settings, RDs typically assess nutritional status using several indicators including serum albumin and BMI 29, 32, 33
Dietitians indicated that approximately 26% of the patients in our study were malnourished, but higher numbers might have been expected since the cancer types chosen have a high prevalence of malnutrition. Ranges of 20% to 80% of cancer patients who develop malnutrition during their clinical course have been reported in the literature 6, 11–14, 34. Methods used in these studies to determine prevalence of malnutrition include the subjective global assessment (SGA), the patient generated subjective global assessment (PG-SGA), the mini nutrition assessment (MNA) and percentage of weight loss or history of weight loss. It is possible that physicians code patients as having cachexia and not malnutrition and therefore we included this ICD-9 code. Additionally, it must be noted that 56% of our population had in situ or regional stage disease which may have accounted for the lower percentage of identified malnutrition. Estimated prevalence rates for cancer associated malnutrition vary with tumor site and stage of disease and there is evidence that tumor stage is associated with inadequate nutritional status 35, 36.
Based on this study’s results, the frequency of agreement in malnutrition identification was poor between physicians and dietitians and BMI and dietitians and at best fair between physicians and BMI. The purpose of the study was to compare the prevalence of malnutrition diagnosis as identified by three classification methods and to determine the agreement of the clinical judgment of physicians and dietitians on the identification of malnutrition for these patients.
Applications and Limitations
Applications
There are several implications of these findings for research, clinical practice and administration. In research, the lack of agreement in defining and assessing malnutrition hinders comparison of incidence and treatment outcomes across studies.
In relation to clinical practice, comprehensive nutrition screening and assessment tools have been developed and evaluated in cancer populations. Tools such as the Short Nutritional Assessment Questionnaire, the Malnutrition Screening Tool, the Malnutrition Universal Screening Tool and the Nutritional Risk Screening provide comprehensive measures of nutritional status 10, 18, 37, 38. Dietitians who are responsible for the nutrition assessment of patients, are usually understaffed in cancer centers 39 and may simply not be available to screen for malnutrition. Nurses are ideally suited to routinely screen for malnutrition and should consider using them. The Joint Commission on the Accreditation of Healthcare Organizations required nutrition screening within a 24 hour time frame of admission to an acute care facility in the mid-1990s which was then expanded to outpatient centers 29, 40. This requirement may have increased the reliance on nursing staff to perform nutrition screens 41. In 2007, Kubrak and Jensen critically evaluated screening tools for nursing professionals to use in the oncology setting and strongly encouraged the use of the PG-SGA. 15. Ultimately, these patients need to be routinely screened with validated tools and preferably tools that can be used by various types of healthcare practitioners such as the PG-SGA. As a result, dietitians can effectively use their time to comprehensively assess those identified by screen and provide the necessary medical nutrition therapy.
In 2009, Soeters and Schols published a theoretical approach to grading the degree of malnutrition in initial patient assessments and suggested that the lack of agreement on the pathophysiology of malnutrition is most likely the basis for the lack of agreement concerning the measurement of malnutrition 10. In this study, ICD-9 codes were a very conservative measure of malnutrition or cachexia and had poor agreement with other measures. Recently, Fox et al, estimated cachexia among cancer patients based on four definitions and showed, as this study did with malnutrition, that the proportion of cachexia among patients varied based on the definition used 42. These authors proposed the development of a standard operational definition for cachexia in clinical practice 42. An operational definition is also needed for malnutrition.
From a health care system perspective, it is difficult for administrators to appropriately charge for and allocate resources to address the problem if the prevalence of malnutrition diagnoses has such marked variance based on the method used to identify it. Although this study could not determine which of the diagnostic methods examined was the most accurate, we suggest that the use of ICD-codes may underestimate the true prevalence of malnutrition and that a onetime measure of BMI may also underestimate the true prevalence. Weight loss is a strong and independent predictor of malnutrition and mortality in cancer patients 43, 44 and approximately 45% of patients suffer a weight loss of 10% or greater prior to diagnosis 3, 45–47. Unintentional weight loss prior to diagnosis is one of several factors that needs to be included in malnutrition screening and is a component of several of the available tools noted previously.
Limitations
Limitations of this study relate to the retrospective data sampling from hospital records. Moreover, there was limited control over the quality and the amount of the data available for the study because of the intrinsic variability of hospital chart data and record keeping. A prospective review of patients as they are hospitalized would yield higher quality data to provide further insight.
In conclusion, this study compared the prevalence of malnutrition diagnosis by three available classification methods in a cancer patient population with the likelihood of a high prevalence of malnutrition and was able to show that these approaches varied widely in the detection of malnutrition. At the root of this concern are several factors. Primarily, there is no universal standard for the screening of malnutrition in this setting and therefore the problem may be underestimated. Additionally, there is the lack of an operational definition of malnutrition and a lack of agreement of nutritional indicators that accurately identify malnutrition in cancer patients. Nurses as front line clinicians could effectively interact with nutrition professionals and begin to use validated tools to identify these patients. As a result, this multidisciplinary clinician approach might provide better intervention with appropriate nutrition support to improve nutritional outcomes, quality of life and response to treatment. In the process, the need for resources to provide nutritional support will be demonstrated thereby improving nutritional support overall.
Footnotes
Funding Disclosure:
This work was funded by the Oncology Nursing Society Foundation and Genentech Inc.Outcomes Research Grant: “Nutritional Status and Health Care Costs in Cancer Patients” and by the National Institutes of Health grant number R25CA114101
REFERNCES
- 1.Bistrian B, Blackburn G, Hallowell E, Heddle R. Protein Status of General Surgical Patients. JAMA. 1974;230(6):858–860. [PubMed] [Google Scholar]
- 2.Bistrian B, Blackburn G, Vitale J, Cochran D, Naylor J. Prevalence of Malnutrition in General Medical Patients. JAMA. 1976;235(15):15671570. [PubMed] [Google Scholar]
- 3.Dewys WD, Begg C, Lavin PT, et al. Prognostic effect of weight loss prior to chemotherapy in cancer patients. Eastern Cooperative Oncology Group. Am J Med. 1980 Oct;69(4):491–497. doi: 10.1016/s0149-2918(05)80001-3. [DOI] [PubMed] [Google Scholar]
- 4.Gallagher-Allred C, Voss A, Finn S, McCamish M. Malnutrition And Clinical Outcomes: The Case For Medical Nutrition Therapy. Journal of the American Dietetic Association. 1996;96(4):361–366. 369. doi: 10.1016/s0002-8223(96)00099-5. [DOI] [PubMed] [Google Scholar]
- 5.Corish C, Kennedy N. Protein-energy undernutrition in hospital in-patients. British Journal of Nutrition. 2000;83:575–591. doi: 10.1017/s000711450000074x. [DOI] [PubMed] [Google Scholar]
- 6.Segura A, Pardo J, Jara C, et al. An epidemiological evaluation of the prevalence of malnutrition in Spanish patients with locally advanced or metastatic cancer. Clin Nutr. 2005 Oct;24(5):801–814. doi: 10.1016/j.clnu.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Guo C-B, Ma D-Q, Zhang K-H, Hu X-H. Relation between nutritional state and postoperative complications in patients with oral and maxillofacial malignancy. British Journal of Oral and Maxillofacial Surgery. 2006;45:467–470. doi: 10.1016/j.bjoms.2006.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Garcia-Peris P, Paron L, Velasco C, et al. Long-term prevalence of oropharyngeal dysphagia in head and neck cancer patients: Impact on quality of life. Clin Nutr. 2007 Dec;26(6):710–717. doi: 10.1016/j.clnu.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Lecleire S, Di Fiore F, Antonietti M, et al. Undernutrition is predictive of early mortality after palliative self-expanding metal stent insertion in patients with inoperable or recurrent esophageal cancer. Gastrointest Endosc. 2006 Oct;64(4):479–484. doi: 10.1016/j.gie.2006.03.930. [DOI] [PubMed] [Google Scholar]
- 10.Soeters PB, Schols AM. Advances in understanding and assessing malnutrition. Curr Opin Clin Nutr Metab Care. 2009 Sep;12(5):487–494. doi: 10.1097/MCO.0b013e32832da243. [DOI] [PubMed] [Google Scholar]
- 11.Capra S, Ferguson M, Ried K. Cancer: impact of nutrition intervention outcome-- nutrition issues for patients. Nutrition. 2001 Sep;17(9):769–772. doi: 10.1016/s0899-9007(01)00632-3. [DOI] [PubMed] [Google Scholar]
- 12.Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Nutritional deterioration in cancer: the role of disease and diet. Clin Oncol (R Coll Radiol) 2003 Dec;15(8):443–450. doi: 10.1016/s0936-6555(03)00155-9. [DOI] [PubMed] [Google Scholar]
- 13.Ravasco P, Monteiro-Grillo I, Vidal PM, Camilo ME. Cancer: disease and nutrition are key determinants of patients' quality of life. Support Care Cancer. 2004 Apr;12(4):246–252. doi: 10.1007/s00520-003-0568-z. [DOI] [PubMed] [Google Scholar]
- 14.Slaviero KA, Read JA, Clarke SJ, Rivory LP. Baseline nutritional assessment in advanced cancer patients receiving palliative chemotherapy. Nutr Cancer. 2003;46(2):148–157. doi: 10.1207/S15327914NC4602_07. [DOI] [PubMed] [Google Scholar]
- 15.Kubrak C, Jensen L. Critical evaluation of nutrition screening tools recommended for oncology patients. Cancer Nurs. 2007 Sep–Oct;30(5):E1–6. doi: 10.1097/01.NCC.0000290818.45066.00. [DOI] [PubMed] [Google Scholar]
- 16.Shils M, Shike M, Ross A, Caballero B, Cousins R, editors. Modern Nutrition In Health and Disease. 10. New York: Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 17.Elia M, Lunn PG. Biological markers of protein-energy malnutrition. Clinical Nutrition. 1997;16(Suppl 1):11–17. doi: 10.1016/s0261-5614(97)80044-1. [DOI] [PubMed] [Google Scholar]
- 18.Pereira Borges N, D'Alegria Silva B, Cohen C, Portari Filho PE, Medeiros FJ. Comparison of the nutritional diagnosis, obtained through different methods and indicators, in patients with cancer. Nutr Hosp Jan–Feb. 2009;24(1):51–55. [PubMed] [Google Scholar]
- 19.National Center for Health Statistics, International Classification of Diseases. Clinical Modification (ICD-9-CM) 1978:169–170. [Google Scholar]
- 20.Swails W, Samour P, Babineau T, Bistrian B. A proposed revision of current ICD-9-CM malnutrition code definitions. Journal of the American Dietetic Association. 1996;96:370–373. doi: 10.1016/S0002-8223(96)00101-0. [DOI] [PubMed] [Google Scholar]
- 21.Brouch K. Where in the World is ICD-10? Journal of the American Health Information Management Association. 2000;71(8):52–57. [Google Scholar]
- 22.Mitchell PH, Ferketich S, Jennings BM. Quality health outcomes model. American Academy of Nursing Expert Panel on Quality Health Care. Image J Nurs Sch. 1998;30(1):43–46. doi: 10.1111/j.1547-5069.1998.tb01234.x. [DOI] [PubMed] [Google Scholar]
- 23.Soeters PB, Reijven PL, van Bokhorst-de van der Schueren MA, et al. A rational approach to nutritional assessment. Clin Nutr. 2008 Oct;27(5):706–716. doi: 10.1016/j.clnu.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 24.George J, Cannon T, Lai V, et al. Cancer cachexia syndrome in head and neck cancer patients: Part II. Pathophysiology. Head Neck. 2007 May;29(5):497–507. doi: 10.1002/hed.20630. [DOI] [PubMed] [Google Scholar]
- 25.Tisdale MJ. Cancer cachexia. Langenbecks. Arch Surg. 2004 Aug;389(4):299–305. doi: 10.1007/s00423-004-0486-7. [DOI] [PubMed] [Google Scholar]
- 26.Couch M, Lai V, Cannon T, et al. Cancer cachexia syndrome in head and neck cancer patients: part I. Diagnosis, impact on quality of life and survival, and treatment. Head Neck. 2007 Apr;29(4):401–411. doi: 10.1002/hed.20447. [DOI] [PubMed] [Google Scholar]
- 27.Ollenschlager G, Viell B, Thomas W, Konkol K, Burger B. Tumor anorexia: causes, assessment, treatment. Recent Results. Cancer Res. 1991;121:249–259. doi: 10.1007/978-3-642-84138-5_28. [DOI] [PubMed] [Google Scholar]
- 28.Bailey KV, Ferro-Luzzi A. Use of body mass index of adults in assessing individual and community nutritional status. Bull World Health Organ. 1995;73(5):673–680. [PMC free article] [PubMed] [Google Scholar]
- 29.Higgins PA, Daly BJ, Lipson AR, Guo SE. Assessing nutritional status in chronically critically ill adult patients. Am J Crit Care. 2006 Mar;15(2):166–176. quiz 177. [PMC free article] [PubMed] [Google Scholar]
- 30.Klein S, Kinney J, Jeejeebhoy K, et al. Nutrition support in clinical practice: review of published data and recommendations for future research directions. Summary of a conference sponsored by the National Institutes of Health, American Society for Parenteral and Enteral Nutrition, and American Society for Clinical Nutrition. Am J Clin Nutr. 1997 Sep;66(3):683–706. doi: 10.1093/ajcn/66.3.683. [DOI] [PubMed] [Google Scholar]
- 31.Campillo B, Paillaud E, Uzan I, et al. Value of body mass index in the detection of severe malnutrition: influence of the pathology and changes in anthropometric parameters. Clin Nutr. 2004 Aug;23(4):551–559. doi: 10.1016/j.clnu.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 32.de Luis DA, Izaola O, Cuellar L, et al. Nutritional assessment: predictive variables at hospital admission related with length of stay. Ann Nutr Metab. 2006;50(4):394–398. doi: 10.1159/000094362. [DOI] [PubMed] [Google Scholar]
- 33.Charney P. Nutrition screening vs nutrition assessment: how do they differ? Nutr Clin Pract. 2008 Aug–Sep;23(4):366–372. doi: 10.1177/0884533608321131. [DOI] [PubMed] [Google Scholar]
- 34.Ravasco P, Monteiro-Grillo I, Marques Vidal P, Camilo ME. Impact of nutrition on outcome: a prospective randomized controlled trial in patients with head and neck cancer undergoing radiotherapy. Head Neck. 2005 Aug;27(8):659–668. doi: 10.1002/hed.20221. [DOI] [PubMed] [Google Scholar]
- 35.Stratton RJ, Green CJ, Elia M. Disease-related Malnutrition: an Evidence-based Approach to Treatment. Wallingford: CABI Publishing; 2003. [Google Scholar]
- 36.Meyenfeldt M. Cancer-associated malnutrition: An introduction. European Journal of Oncology Nursing. 2005;9:S35–S38. doi: 10.1016/j.ejon.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 37.Isenring E, Cross G, Daniels L, Kellett E, Koczwara B. Validity of the malnutrition screening tool as an effective predictor of nutritional risk in oncology outpatients receiving chemotherapy. Support Care Cancer. 2006 Nov;14(11):1152–1156. doi: 10.1007/s00520-006-0070-5. [DOI] [PubMed] [Google Scholar]
- 38.Neelemaat F, Kruizenga HM, de Vet HC, Seidell JC, Butterman M, van Bokhorst-de van der Schueren MA. Screening malnutrition in hospital outpatients. Can the SNAQ malnutrition screening tool also be applied to this population? Clin Nutr. 2008 Jun;27(3):439–446. doi: 10.1016/j.clnu.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 39.Huhmann MB, Cunningham RS. Importance of nutritional screening in treatment of cancer-related weight loss. Lancet Oncol. 2005 May;6(5):334–343. doi: 10.1016/S1470-2045(05)70170-4. [DOI] [PubMed] [Google Scholar]
- 40.Joint Commission on Accreditation of Healthcare Organizations. Chicago 2007 Comprehensive Accrediation Manual for Hospitals. [PubMed] [Google Scholar]
- 41.Heller L. Nutritional screening and the pediatric patient in the hospital setting. Building Block for Life. 2003;26:1–4. [Google Scholar]
- 42.Fox KM, Brooks JM, Gandra SR, Markus R, Chiou CF. Estimation of Cachexia among Cancer Patients Based on Four Definitions. J Oncol. 2009;2009:693458. doi: 10.1155/2009/693458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vigano A, Donaldson N, Higginson IJ, Bruera E, Mahmud S, Suarez-Almazor M. Quality of life and survival prediction in terminal cancer patients: a multicenter study. Cancer. 2004 Sep 1;101(5):1090–1098. doi: 10.1002/cncr.20472. [DOI] [PubMed] [Google Scholar]
- 44.Vigano A, Dorgan M, Buckingham J, Bruera E, Suarez-Almazor ME. Survival prediction in terminal cancer patients: a systematic review of the medical literature. Palliat Med. 2000 Sep;14(5):363–374. doi: 10.1191/026921600701536192. [DOI] [PubMed] [Google Scholar]
- 45.Bosaeus I, Daneryd P, Svanberg E, Lundholm K. Dietary intake and resting energy expenditure in relation to weight loss in unselected cancer patients. Int J Cancer. 2001 Aug 1;93(3):380–383. doi: 10.1002/ijc.1332. [DOI] [PubMed] [Google Scholar]
- 46.Van Cutsem E, Arends J. The causes and consequences of cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9( Suppl 2):S51–63. doi: 10.1016/j.ejon.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 47.Argiles JM. Cancer-associated malnutrition. Eur J Oncol Nurs. 2005;9( Suppl 2):S39–50. doi: 10.1016/j.ejon.2005.09.006. [DOI] [PubMed] [Google Scholar]