Abstract
Objective
To test an active-learning, empowerment approach to teaching patients about the “diabetes ABCs” (hemoglobin A1C, systolic blood pressure, and low density lipoprotein cholesterol).
Methods
84 (97%) diabetic patients who participated in a randomized effectiveness trial of two clinic-based group educational methods and completed a post-intervention assessment. The empowerment arm participated in a group session that incorporated two educational innovations (a conceptual metaphor to foster understanding, and team-based learning methods to foster active learning). The traditional diabetes education arm received a didactic group session focused on self-management and educational materials about the diabetes ABCs. Participants in both arms received individual review of their current ABC values.
Results
A questionnaire evaluated knowledge, understanding, and recall of the diabetes ABCs was administered three months after enrollment in the study. At three months, participants in the empowerment group demonstrated greater understanding of the diabetes ABCs (P<.0001), greater knowledge of their own values (P<.0001), and greater knowledge of guideline-derived target goals for the ABCs compared with participants in the traditional arm (P<.0001).
Conclusion
An active-learning, empowerment-based approach applied to diabetes education can lead to greater understanding and knowledge retention.
Practice Implications
An empowerment approach to education can facilitate informed, activated patients and increase performance of self-management behaviors.
Keywords: Diabetes Education, Self-Management, Patient Empowerment, Team-Based Learning, Group Clinics
1. Introduction
Patient education is an integral component of high quality diabetes care [1]. The National Diabetes Education Program stresses the need for patients to have a practical understanding of approaches to self-management of diabetes and related conditions [2]. Knowledge and understanding may be important elements in moving an activated patient towards self-management [3], but are often not sufficient to maintain performance of self-management behaviors [4,5]. On the other hand, self-management education alone is unlikely to succeed if patients [6] are not empowered to adapt basic diabetes knowledge from a population level to the particularities of their own daily health behaviors, emotions, and role functions [7,8]. Self-management support interventions employ such empowerment strategies by encouraging patients to use personalized approaches to diabetes risk assessment, goal-setting, and problem-solving. These have been effective at increasing performance with self-management behaviors [9], functional status [10], and glucose control [11] among even vulnerable and co-morbid diabetes patients.
As a foundation for self-management, diabetes educators place particular emphasis on patients’ understanding the clinical importance and predictive value of three key metabolic markers: Hemoglobin A1C, systolic Blood pressure, and low density lipoprotein (LDL) Cholesterol values. Known collectively as the “diabetes ABCs”, these three values form the National Diabetes Education Program’s cornerstone for monitoring actions and mitigating the risk of long-term complications of diabetes [12]. Guidelines for diabetes education stress the importance of teaching patients to know the clinical significance of the diabetes ABCs and to be aware of their own personal ABC values [1].
Evidence suggests that greater awareness of the ABC concepts leads to better diabetes self-management and glycemic control [13]. In addition, enhancing knowledge and understanding of diabetes ABC goals is associated with subsequent improvements in glycemic control [14]. However, studies have shown that most diabetes patients do not know their personal ABC values, or even the clinical importance of these values [15, 16]. Further, evidence suggests that community-based diabetes education programs often are not effective at improving even basic retention of patients’ understanding of the diabetes ABCs, let alone knowledge of their own personal values [17].
Despite the general consensus that diabetes self-management support interventions are superior to more traditional, didactic approaches to patient education [7, 10], diabetes education specifically related to knowledge of the Diabetes ABCs has remained wedded to traditional, didactic approaches. Didactic approaches to patient education assume that once experts “teach” the relevant information and provide recommendations, patients should be capable of recalling recommendations at the conclusion of the education session and adhering to those recommendations thereafter [6]. In contrast, an empowerment approach to diabetes education relays information and recommendations in ways that increase patients’ ability to “think critically and act autonomously” even when experts are not readily available [18]. An empowerment process [6, 18] would place knowledge and understanding of the ABCs within the context of personalized goal-setting, skills-building and one’s daily roles; and thus enhance appreciation of the personal significance of ABC values rather than rote memorization and recall of numbers. To test this hypothesis, we performed a randomized, effectiveness trial of an empowerment approach to enhance participants’: a) knowledge and understanding of the diabetes ABCs, and b) recall of personal ABC values, as compared to a traditional clinic-based diabetes education program.
2. Methods
2.1 Study participants
We recruited patients receiving diabetes care from various primary care clinics in a single regional Veterans Affairs Medical Center (VAMC) drawing from the Southwestern Gulf Coast region of the United States. We used referrals from primary care providers, advertisements that targeted patients in outpatient clinics, and the VAMC clinic database to identify potential participants. Inclusion criteria included age 50–90 years old, primary care provider within the VA health care system, diagnosis of type 2 diabetes mellitus (ICD-9 codes 250), and mean A1C greater than 7.5% in past 6 months. Exclusion criteria were serum creatinine greater than or equal to 2.5 and a prior diagnosis of dementia. Eligible participants received a letter inviting them to participate in the study, followed by a telephone call to explain the study and obtain informed consent from interested patients. After enrollment, we randomized participants to either the empowerment intervention or the traditional health system-based diabetes education program. The study period was three months long, and both groups continued to see their primary care provider during this time. Among the 87 subjects who were originally randomized in the original study, 84 (97%) completed the Diabetes ABCs questionnaire at 3-months follow-up. These 84 subjects constitute the analytical sample for the current study.
2.2 Empowerment intervention arm
As part of the self-management support intervention for the empowerment group, we embedded an active learning session aimed at increasing participants’ awareness and use of the diabetes ABCs in their daily lives. This one-hour session was conducted as the first in a series of four group (8–10 patients per group) clinic sessions for patients in the intervention arm. Subsequent intervention sessions focused on goal setting, action planning, and active communication with one’s physician. One general internist with nurse support facilitated all intervention sessions. Participants also received 10 minutes of one-on-one time with a study clinician following each hour-long group session. During the one-on-one consultation with the study clinician, participants discussed their ABCs status, received feedback on their specific diabetes goal and action plan, and addressed medication related issues. While issues related to the diabetes ABCs surfaced during the subsequent sessions, only the first session focused specifically on the ABCs and their application to self-management.
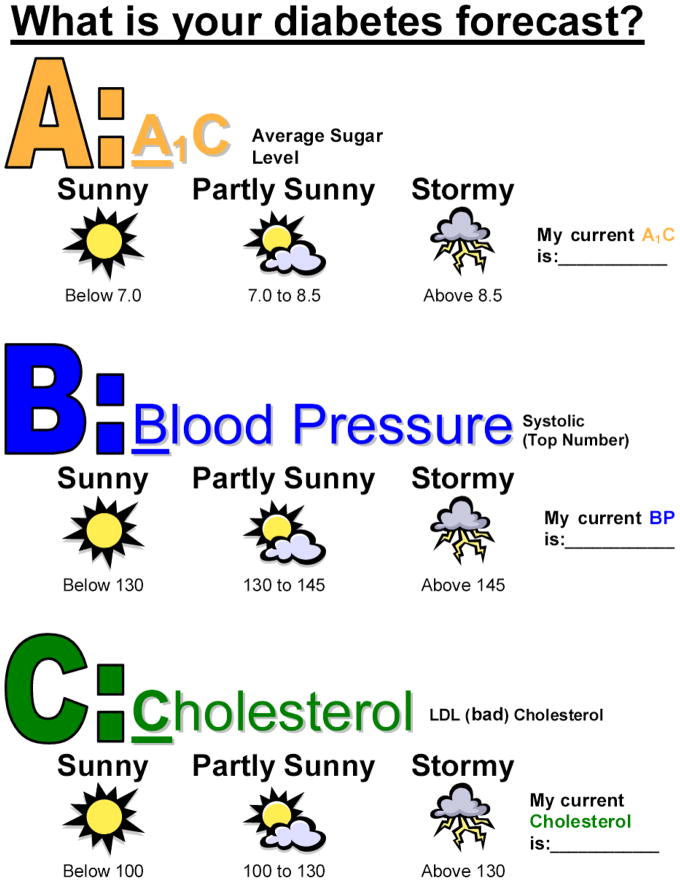
During the first session, we used two strategies to create meaning and increase the relevance of the ABC concepts for the study patients. First, we used a conceptual metaphor to create meaning about patients’ own A1C, blood pressure, and cholesterol levels. Cognitive linguistic theory suggests that humans use metaphors to foster understanding of complex concepts by “mapping” them to more concrete and understandable concepts [19]. In the intervention session, we introduced the concept of diabetes ABCs by mapping it to a weather prediction concept, presenting various levels of A1C, systolic blood pressure, and LDL cholesterol as being consistent with a “sunny”, “partly cloudy”, or “stormy” diabetes “forecast”. We used the weather metaphor along with universally understood weather icons as a method of translating the ABCs into predictors of future health consequences. We presented participants with their own ABC values on a sheet that used the icons to signify different levels of diabetes-related risks. Figure 1 presents an example of this sheet, with the icons and underlying conceptual metaphor.
Figure 1.
Empowerment Intervention Diabetes ABC’s Forecast Worksheet
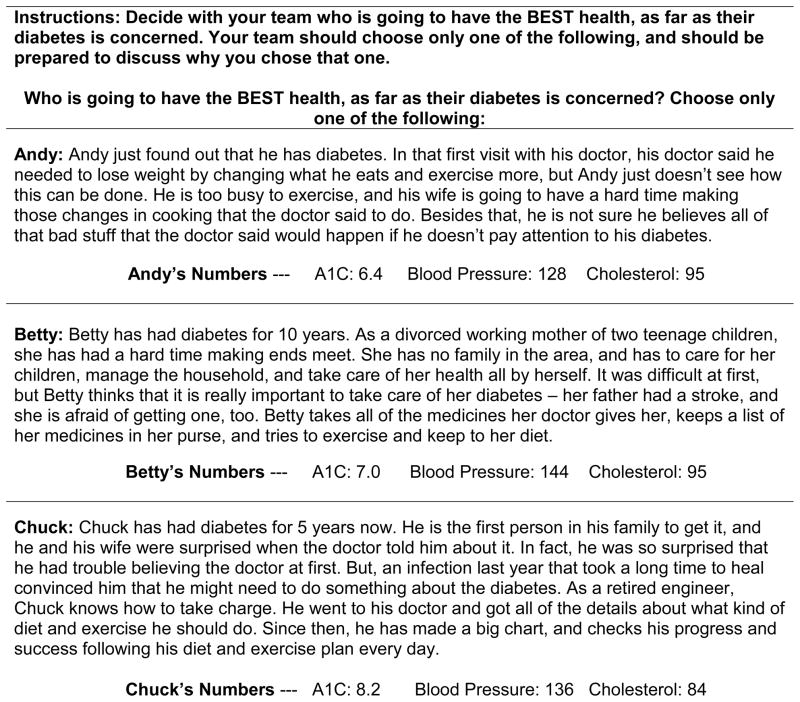
Our second strategy drew from team-based learning methods [20, 21], and aimed to give participants active hands-on practice in applying ABC values to cases that simulated real-world complexity. In this exercise, participants worked in small teams (3–4 participants each) to decide which of three case patients was at greatest risk for suffering long-term complications from diabetes based on their behaviors. After each team made their decision, they revealed their choice to the other teams, and the session educator facilitated a discussion where teams defended their answers to each other and discussed the meaning of ABC values in managing and preventing diabetes complications. The case descriptions appear in Figure 2. As the case descriptions demonstrate, there is no “correct” answer to the exercise; rather, participants had to discuss, wrestle with, and decide on the relative importance of ABC values, social support, motivation, and personal resources in making their prediction as to which of the three patients would enjoy the best health. The complexity of the exercise arises from the fact that for each case patient, different diabetes concepts varied in their severity and circumstances. For example, “Andy,” the first case patient, has the most favorable ABC values, but lower motivation and intermediate social support compared with the other case patients. The sequential structure of intra-team followed by inter-team discussion allowed participants to both discover and deepen their understanding of diabetes management concepts in two steps. First, during the intra-team discussion, team members had space to share insights and experience with each other. Second, during the inter-team discussion, the session moderator could assess the conceptual depth with which teams were making their arguments and deepen the conversation by posing questions, underscoring important statements, and providing information as needed. This discussion of the diabetes ABCs in a contextualized setting provided a critical foundation for goal-setting and action planning activities during the subsequent sessions.
Figure 2.
Empowerment Intervention Team-Based Leaning Activity
2.3 Traditional diabetes education arm
As part of their participation in the comparison group, patients in the traditional arm received a two-hour, didactic group session on diabetes self-management followed by a 5–10 minute individual review of each participant’s current diabetes ABC’s. Both the group and individual sessions were conducted by a nurse educator certified in diabetes education, and followed American Diabetes Association guidelines for patient education about diabetes [1]. Topics covered in this session included the diabetes ABCs, the role of diet and exercise in diabetes care and management, the importance of self-monitoring, and decision-making about the ABC values. Participants were provided with printed information that stressed the importance of knowing one’s ABC values and discussing these with one’s physician. In addition to the diabetes education group session, participants were also scheduled to receive a group session with a registered dietician to discuss issues specific to dietary management of diabetes. Following both the group diabetes education and nutrition sessions, participants were scheduled for an additional clinic visit with their primary care provider. Primary care providers were instructed to focus specifically on diabetes care during this additional outpatient clinic visit.
2.4 Measures and scoring
Study participants from both the empowerment and traditional group attended data collection sessions at baseline and 3-months after enrollment, following the active intervention period. During the 3-months data collection, participants completed a Diabetes ABC’s Questionnaire developed by our study team to evaluate knowledge, understanding and recall of the diabetes ABCs. Study personnel collected baseline socio-demographic and clinical data as well as two validated scales of the Diabetes Care Profile [22] to determine participants’ self-reported knowledge of diabetes and everyday burden of illness at baseline. The Knowledge and Understanding of Diabetes scale is from section 4 of the Diabetes Care Profile, and it consists of 13 items with higher scores indicating greater knowledge and understanding. The How Much Diabetes Interferes with Daily Life scale is from section 7 of the Diabetes Care Profile, and its consists of 14 items with higher scores indicating greater interference in daily life.
2.4.1 Diabetes ABCs questionnaire
Participants completed a Diabetes ABC’s questionnaire three months after enrollment. The Diabetes ABCs questionnaire included three questions: (1) In Diabetes ABCs, what does A, B, & C stand for?; (2) The last time your ABC’s were checked, what were the numbers?; and (3) What would you like your ABC numbers to be? Each question required three unique answers to be considered complete: one answer each for each biomarker - A1C, blood pressure, and cholesterol. Our purpose was to assess participants’ knowledge of the ABC acronym, the individual’s actual value, and the individual’s target value.
2.4.2 Development of scoring
Because the participants’ answers were open-ended, our team developed procedures for scoring the responses. The initial procedures were utilized by six scorers on a small subset of five participant responses to the questionnaire. Scorers agreed on the majority of scores, with few disagreements. Though scoring was highly consistent across scorers, disagreements were discussed and resolved, with minor clarifications made to the scoring procedures. The final scoring procedures, with definitions of partially or fully correct scores, are shown in Table 1 and described in further detail below. The remaining participants’ responses were scored using these procedures by all six scorers, with final scores for each response being those scores on which four of the six scorers agreed. Only four (4.8%) responses garnered scores on which less than four scorers agreed; these were discussed by the full team and resolved.
Table 1.
Scoring of ABCs Questionnaire
| Question | Score for each biomarker | Definition |
|---|---|---|
| Question #1: “In Diabetes ABCs, what does A, B, & C stand for?” | 0 | No answer, “don’t know,” incorrect answer |
| 1 | A partially correct response of general terms for each biomarker, such as “blood sugar” or “glucose” for A1c, “blood” for blood pressure | |
| 2 | A fully correct response of specific terms for each biomarker, such as “A1c” or “average sugar level” for A1c, “blood pressure” or “bad cholesterol” | |
| Total Possible Question #1 score | 6 | Add together the scored responses for A, B, and C |
| Question #2: “The last time your ABC’s were checked, what were the numbers?” | 0 | No answer, “don’t know,” incorrect answer, a response without numeric values specific to the possible range of the biomarker*, or a response without forecast icons+, including answers such as “fine” |
| 1 | A correct score, when the participant provided a number that correctly matched the possible values of the biomarker* or if a forecast icon+ was given | |
| Total Possible Question #2 Score | 3 | Add together the scored responses for A, B, and C |
| Question #3: “What would you like your ABC numbers to be?” | 0 | No answer, Incorrect values (i.e., not a possible value for the biomarker, outside biomarker range*) |
| 1 | A partially correct response that included an appropriate forecast icon‡ or value for the biomarker§, even if the value was greater that what was given in question 2. | |
| 2 | A fully correct response that included a value equal to or less than the value provided in question 2 for the biomarker or if a value that was in the desired range of the biomarker§. | |
| Total Possible Question#3 Score | 6 | Add together the scored responses for A, B, and C |
| Total Possible Questionnaire Score | ||
| 15 | Add together the totals for Questions #1, #2, and #3 | |
Reasonable biomarker ranges: A1c <7.0%; Blood pressure <130; Cholesterol <100
Forecast Icons: Sunny, Partly Sunny, Stormy
Desirable Forecast Icons: Partly Sunny, Sunny
A1c < 7%, systolic Blood pressure < 130, Cholesterol < 100
2.4.3. Scoring diabetes ABC questionnaire
Scoring for the Diabetes ABCs Questionnaire is shown in detail in Table 1. Generally, for each biomarker on question 1 (“in Diabetes ABCs, what does A, B, & C stand for?”), responses were scored with a 0, 1, or 2. This resulted in a total possible score of 6 for question 1. For each biomarker on question 2 (“The last time your ABC’s were checked, what were the numbers?”), responses were scored with a 0 or a 1. This resulted in a total possible score of 3 for question 2. For each biomarker on question 3 (“What would you like your ABC numbers to be?”), participant responses were scored using the same procedures for question 1, resulting in a total possible score of 6. The full Questionnaire has a possible total score of 15. Higher scores on the full Questionnaire and each of its questions indicated greater participant knowledge and understanding of the ABCs. For questions 2 and 3, higher numbers indicated greater participant knowledge and understanding of the ABCs.
2.5 Analysis
Since not all participants attended the ABC session in either the empowerment or traditional groups, we analyzed all participants’ data on an intention to treat basis. We hypothesized that the responses of participants in the intervention group would indicate greater participant knowledge and understanding of diabetes ABCs than the responses of the participants in the comparison group. T-tests were used to evaluate the differences in responses to the diabetes ABC questionnaire between participants in the two study groups.
3. Results
Table 2 describes the baseline characteristics of our study sample. The average participant had over 3 chronic conditions and was 63.9 ± 7 years of age. Participants had a mean hemoglobin A1C of 8.61% ± 1.2% at baseline. Half of the participants were non-white and more than half had some college education. Most (82%) participants attended the corresponding ABCs education class according to their study group. On the Diabetes Care Profile questions, both study groups reported to have a “Fair” knowledge and understanding of diabetes. Most participants reported that diabetes moderately interfered with daily life. There were no significant baseline differences among participants in the empowerment versus traditional education arms.
Table 2.
Baseline Characteristics of the Study Population (N=85)
| Characteristics | Empowerment Intervention Arm (n=44) | Traditional Education Arm (n=41) | P-Value |
|---|---|---|---|
| Age, mean (SD) | 64.6 (7.3) | 63.6 (7.7) | 0.57 |
| Race, number (%) | |||
| White | 22 (50%) | 17 (41%) | |
| African American | 13 (30%) | 14 (34%) | 0.54 |
| Hispanic or Latino | 6 (13%) | 9 (22%) | |
| Other | 3 (7%) | 1 (3%) | |
| Deyo Score, mean (SD) | 2.98 (2.3) | 3.66 (3.1) | 0.25 |
| Baseline Hemoglobin A1C, mean (SD) | 8.53 (1.20) | 8.65 (1.23) | 0.67 |
| Education Level, number (%) | |||
| ≤ High School | 12 (27.3%) | 10 (24.4%) | 0.76 |
| > Some College/Trade School | 32 (72.7%) | 31 (75.6%) | |
| Attended Session, number (%) | 34 (77%) | 35 (85%) | 0.34 |
| Knowledge and Understanding of Diabetes*, mean (SD) | 3.1 (.85) | 2.9 (1.0) | 0.54 |
| How Much Diabetes Interferes with Daily Life†, mean (SD) | 2.5 (.77) | 2.7 (.88) | 0.36 |
Diabetes Care Profile, section 4, (13-item subscale, scale range 1–5 [Higher score indicates greater knowledge])
Diabetes Care Profile, section 7 (14-items subscale, scale range 1–5 [Higher score indicates more interference])
Table 3 describes responses to the open-ended questionnaire about the Diabetes ABCs for participants in each study arm. Each open-ended response was scored according to our ABCs scoring rubric. The empowerment group had a significantly higher mean score overall compared to the traditional education group (13.16 ± 3.19 versus 1.30 ± 3.25, P< 0.0001) and for each component item of the ABC Questionnaire. When asked “In the Diabetes ABCs what does A B & C stand for?” the empowerment group scored 5.5 ± 1.02 (out of a possible total score of 6) compared to the traditional education group who scored 0.53 ± 1.41. Participants in the empowerment group were also more likely to be able to report their own number for each of the ABC biomarkers when compared to the traditional group. In response to the question “What would you like your ABCs numbers to be?”, empowerment participants’ mean scores were also higher than the traditional group (5.09 ± 1.65 and 0.53 ± 1.3).
Table 3.
Study Participants’ Diabetes ABC Questionnaire Scores (n=85)
| Question | Empowerment Intervention Arm (n=44) | Traditional Education Arm (n=41) | P-Value |
|---|---|---|---|
| In the Diabetes ABC’s, what does A B & C stand for?*, mean (SD) | 5.5 (1.02) | 0.53 (1.41) | <0.0001 |
| The last time your ABC’s were checked, what were the numbers? (give your best guess)†, mean (SD) | 2.5 (0.93) | 0.25 (0.63) | <0.0001 |
| What would you like your ABC numbers to be?*, mean (SD) | 5.09 (1.65) | 0.53 (1.30) | <0.0001 |
| Total Questionnaire Score‡, mean (SD) | 13.16 (3.19) | 1.30 (3.25) | <0.0001 |
Abbreviations: A= Hemoglobin A1C; B= Systolic Blood Pressure; C= Low Density Lipoprotein Cholesterol; PCP, Primary Care Provider
Scores for each item represent participants’ responses to the Diabetes ABC Questionnaire three months after study enrollment and immediately after the conclusion of the active study period.
Scale 0–6 (Higher rating indicates greater participant knowledge and understanding of ABCs)
Scale 0–3 (Higher rating indicates greater participant accuracy)
Scale 0–15 (Summary score from all three ABC questionnaire items)
4.1 Discussion
This study describes results from a randomized effectiveness trial comparing two approaches to diabetes education. The purpose of this study was to evaluate participants’ understanding of the clinical relevance of the diabetes ABCs and their recall of personal ABC values. Participants in the empowerment intervention arm were significantly more likely to accurately recall the clinical meaning of the diabetes ABCs compared with participants in the traditional education arm. Similarly, participants in the empowerment intervention arm were much more likely to accurately recall their personal ABC values and a clinically reasonable target level for their ABC values compared to those in the traditional education arm.
The empowerment approach seems to have a profound rather than a subtle effect on our measure of the understanding of the ABCs and recall of personal and goals values. In the traditional education arm, very few participants could report an accurate understanding of the clinical meaning of any of the ABCs or recall any of their personal or goal ABC values. In contrast, nearly all the participants in the empowerment intervention arm accurately reported an understanding of the ABCs, and most could recall their personal or goal ABC values. These differences account for a ten-fold difference in the overall scores of participants in the two groups on the ABCs questionnaire. The knowledge difference between traditional and patient empowerment approaches in this study mirrors the differences found between these two approaches in a broad array of tests of diabetes self-management training [6]. The empowerment approach to self-management training is considered “a cornerstone of chronic disease care” [10] and is widely considered to be the conceptual basis for self-management support within the chronic care model [3, 23].
The results of our study support the need for adaptations of the empowerment approach to other facets of patient education embedded within health services programs. In essence, this study found that an empowerment approach to teaching the diabetes ABCs leads to a patient who may be ready to apply these new concepts to her personal diabetes care and daily routine (i.e., an informed, activated patient). Patient education programs grounded in this approach are important drivers of effective chronic care, because an activated patient in partnership with a prepared provider team forms a foundation for optimal chronic illness management [3]. Two key principles found within our intervention are worth underscoring. First, we translated the basic knowledge element of our education intervention using a conceptual metaphor [19]. This metaphor, “predicting the weather”, is especially effective in this setting because it uses low-literacy pictorial icons that have similar meaning across many populations, and because weather prediction is a widely understood concept for risk prediction (with the added benefit of conveying an understood sense of error and uncertainty in weather prediction). Participants in the current study appeared to comprehend and work very quickly with the information presented in Figure 1 and moved towards linking the ABCs to their daily activities.
The second principle underlies the pedagogical process used in the intervention. We used a team-based, active learning approach that is consistent with the contemporary literature on adult learning theory [24, 25]. The team-based learning approach empowered patients by fostering discussion among all participants about the relevance of the information, drawing on their prior and present experiences. In the team-based discussions, participants could “practice” using their understanding of the ABC concepts through case examples and working with others to resolve conflict and make decisions that simulated the topics and environments that they would face in their daily experiences with diabetes. In contrast, traditional diabetes education, at least with respect to the ABCs, relies on passive modes of learning in which participants are simply recipients of facts, often with little personal context. Such lecture-based modes of learning do not foster recall of facts let alone understanding of how to adapt new knowledge to novel problems and daily experiences with chronic care [26].
Improving patients’ diabetes-related understanding and their ability to critically resolve many of the daily challenges of diabetes self-care are key process measures of the empowerment approach to diabetes [6]. In addition, Anderson and Funnell [18] have described increased self-efficacy as an important outcome measure of the empowerment approach. Improved self-efficacy, especially when measured as the confidence to perform specific diabetes self-management tasks, is instrumental to achieving clinically important diabetes outcomes, such as metabolic control [10]. We have recently demonstrated [27] that participants enrolled in our four-session, group clinic intervention had significantly greater improvements in glycosylated hemoglobin levels post-intervention (0.67% ± 1.3%, P=.03) compared with those who attended traditional diabetes education and nutrition groups. These differences in metabolic improvements persisted (0.59% ±1.4%, P=.05) at one-year follow-up. Longitudinal data analyses demonstrated that self-efficacy for diabetes self-management was a mediator of the observed metabolic changes [27]. An empowerment approach to diabetes education and self-management support, therefore, may improve metabolic outcomes of diabetes care through enhancements in diabetes self-efficacy. Additional studies are needed to adequately test this relationship.
The current study has some limitations. First, the primary results rely on a novel measurement tool developed for this study. Our standardized, blinded, consensus-building process used to score participants’ responses has not been used in prior work or validated in other populations. Second, the wording of the ABC questionnaire during the follow-up data collection was more suited to the empowerment intervention process and may reflect participants’ familiarity with the process and materials rather than improvements in recall. Consistent with the conceptual model of the intervention [3], an activated patient may not need to rely on rote memory to facilitate adaptation of diabetes knowledge into improvements in self-management and clinical outcomes. The study did utilize a randomized, comparative effectiveness design underscoring its internal validity and practical clinical impact [28]. However, study participants were largely male Veterans from a single regional health center; which may limit the external validity of these findings. Further research using broader patient populations, settings, and clinical circumstances are needed to validate this adaptation of patient empowerment to patient education in chronic care.
4.2 Conclusion
Chronic care interventions tend to disproportionately focus on health systems, health services models, and clinicians. The current study runs counter to this trend in that it focuses on patients, adapting elements of educational models used in medical education and health services research [26]. We found that an active-learning empowerment approach to teaching of basic diabetes concepts outperformed traditional approaches. These findings should encourage changes in the methods used by diabetes educators to facilitate comprehension and application of the diabetes ABCs, especially in those diabetes education programs that are linked to health systems and clinician teams.
4.3. Practice Implications
Future work is needed to further adapt the empowerment intervention into the context of longitudinal patient-clinician interactions [29]. Integration of our empowerment approach for patient education into follow-up visits with clinicians could enhance awareness, patient-clinician communication and treatment of the gap between current and goal ABC values [29, 30].
Acknowledgments
This work was supported by a grant from the Agency for Healthcare Research and Quality (#U18HS016093), Centers for Research and Education on Therapeutics (Houston CERT, Suarez-Almazor, PI). The authors acknowledge additional project support from a Clinical Scientist Development Award from the Doris Duke Charitable Foundation and resources in the preparation of this manuscript from the Houston Health Services Research and Development Center of Excellence (HFP90-020) at the Michael E. DeBakey VA Medical Center. Dr. Naik receives additional support from the National Institute on Aging (K23AG027144). These sources had no role in the preparation, review, or approval of the manuscript.
The authors thank Andrea Price, BA, and Donna Rochon, PhD, for their assistance with patient recruitment, retention and project support; and Teresa Zhang, PhD, and Annette Walder, MS with data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Funnell MM, Brown TL, Childs BP, et al. National standards for diabetes self management education. Diabetes Care. 2009;32 (Suppl 1):S87–S94. doi: 10.2337/dc08-S087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Funnell MM National Diabetes Education Program. NIH Publication No. 06-5492. 2006. 4 Steps to Control Your Diabetes for Life. [Google Scholar]
- 3.Wagner EH, Austin BT, Von KM. Organizing care for patients with chronic illness. Milbank Q. 1996;74:511–44. [PubMed] [Google Scholar]
- 4.Hibbard JH, Greene J, Tusler M. Improving the outcomes of disease management by tailoring care to the patient’s level of activation. Am J Manag Care. 2009;15:353–60. [PubMed] [Google Scholar]
- 5.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–71. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 6.Anderson RM, Funnell MM. Patient empowerment: reflections on the challenge of fostering the adoption of a new paradigm. Patient Educ Couns. 2005;57:153–7. doi: 10.1016/j.pec.2004.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Funnell MM, Tang TS, Anderson RM. From DSME to DSMS: Developing Empowerment-Based Diabetes Self-Management Support. Diabetes Spectrum. 2007;20:221–6. [Google Scholar]
- 8.Morrow AS, Haidet P, Skinner J, Naik AD. Integrating diabetes self-management with the health goals of older adults: a qualitative exploration. Patient Educ Couns. 2008;72:418–23. doi: 10.1016/j.pec.2008.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadur CN, Moline N, Costa M, Michalik D, Mendlowitz D, Roller S, Watson R, Swain BE, Selby JV, Javorski WC. Diabetes management in a health maintenance organization. Efficacy of care management using cluster visits. Diabetes Care. 1999;22:2011–7. doi: 10.2337/diacare.22.12.2011. [DOI] [PubMed] [Google Scholar]
- 10.Schillinger D, Handley M, Wang F, Hammer H. Effects of self-management support on structure, process, and outcomes among vulnerable patients with diabetes: a three-arm practical clinical trial. Diabetes Care. 2009;32:559–66. doi: 10.2337/dc08-0787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Piette JD, Weinberger M, McPhee SJ, Mah CA, Kraemer FB, Crapo LM. Do automated calls with nurse follow-up improve self-care and glycemic control among vulnerable patients with diabetes? Am J Med. 2000;108:20–7. doi: 10.1016/s0002-9343(99)00298-3. [DOI] [PubMed] [Google Scholar]
- 12.Funnell MM National Diabetes Education Program. NIH Publication No. 06-5492. 2006. 4 Steps to Control Your Diabetes for Life. [Google Scholar]
- 13.Heisler M, Piette JD, Spencer M, Kieffer E, Vijan S. The relationship between knowledge of recent HbA1c values and diabetes care understanding and self-management. Diabetes Care. 2005;28:816–22. doi: 10.2337/diacare.28.4.816. [DOI] [PubMed] [Google Scholar]
- 14.Berikai P, Meyer PM, Kazlauskaite R, Savoy B, Kozik K, Fogelfeld L. Gain in patients’ knowledge of diabetes management targets is associated with better glycemic control. Diabetes Care. 2007;30:1587–89. doi: 10.2337/dc06-2026. [DOI] [PubMed] [Google Scholar]
- 15.Guirguis LM, Kieser MA, Chewning BA, Kanous NL. Recall of A1C, blood pressure, and cholesterol levels among community pharmacy patients with diabetes. J Am Pharm Assoc. 2007;47:29–34. doi: 10.1331/1544-3191.47.1.29.guirguis. [DOI] [PubMed] [Google Scholar]
- 16.Harwell TS, Dettori N, McDowall JM, Quesenberry K, Priest L, Butcher MK, Flook BN, Helgerson SD, Gohdes D. Do persons with diabetes know their (A1C) number? Diabetes Educ. 2002;28:99–105. doi: 10.1177/014572170202800111. [DOI] [PubMed] [Google Scholar]
- 17.Brick JC, Derr RL, Saudek CD. A randomized comparison of the terms estimated average glucose versus hemoglobin A1C. Diabetes Educ. 2009;35:596–602. doi: 10.1177/0145721709336298. [DOI] [PubMed] [Google Scholar]
- 18.Anderson RM, Funnell MM. Patient Empowerment: Myths and misconceptions. Patient Education and Counseling. 2010;79:277–282. doi: 10.1016/j.pec.2009.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lakoff G, Johnson M. Metaphors we live by. Chicago: University of Chicago Press; 1980. [Google Scholar]
- 20.Haidet P, Fecile ML. Team-based learning: a promising strategy to foster active learning in cancer education. J Cancer Educ. 2006;21:125–8. doi: 10.1207/s15430154jce2103_6. [DOI] [PubMed] [Google Scholar]
- 21.Michaelson L, Parmelee D, McMahon KK, Levine RE. Team-Based Learning for Health Professions Education. Sterling, VA: Stylus; 2008. [Google Scholar]
- 22.Fitzgerald JT, Davis WK, Connell CM, Hess GE, Funnell MM, Hiss RG. Development and validation of the Diabetes Care Profile. Eval Health Prof. 1996;19:208–30. doi: 10.1177/016327879601900205. [DOI] [PubMed] [Google Scholar]
- 23.Fisher EB, Brownson CA, O’Toole ML, Shetty G, Anwuri VV, Glasgow RE. Ecological approaches to self-management: the case of diabetes. Am J Public Health. 2005;95:1523–35. doi: 10.2105/AJPH.2005.066084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Knowles M, Holton EF, Swanson RA. The Adult Learner. Burlington, MA: Elsevier; 2005. [Google Scholar]
- 25.National Research Council Committee on Developments in the Science of Learning. How People Learn: Brain, Mind, Experience, and School. Washington, DC: National Academies Press; 2000. [Google Scholar]
- 26.Haidet P, O’Malley KJ, Richards B. An initial experience with “team learning” in medical education. Acad Med. 2002;77:40–4. doi: 10.1097/00001888-200201000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Naik AD, Palmer N, Petersen NJ, Street RL, Jr, Rao R, Suarez-Almazor M, Haidet P. Comparative Effectiveness of Goal-Setting in Diabetes Group Clinics. Archives of Internal Medicine. 2010 doi: 10.1001/archinternmed.2011.70. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Naik AD, Petersen LA. The neglected purpose of comparative effectiveness research. N Engl J Med. 2009;360:1929–31. doi: 10.1056/NEJMp0902195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Naik AD, Kallen MA, Walder A, Street RL., Jr Improving hypertension control in diabetes mellitus: the effects of collaborative and proactive health communication. Circulation. 2008;117:1361–8. doi: 10.1161/CIRCULATIONAHA.107.724005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Naik AD, Issac TT, Street RL, Jr, Kunik ME. Understanding the quality chasm for hypertension control in diabetes: a structured review of “co-maneuvers” used in clinical trials. J Am Board Fam Med. 2007;20:469–78. doi: 10.3122/jabfm.2007.05.070026. [DOI] [PMC free article] [PubMed] [Google Scholar]