Abstract
Background
Older age is an independent predictor of all-cause mortality in patients with mild to moderate heart failure (HF). Whether older age is also an independent predictor of mortality in patients with more advanced HF is unknown.
Methods
Of the 2707 Beta-Blocker Evaluation of Survival Trial (BEST) participants with ambulatory chronic HF (New York Heart Association class III/IV and left ventricular ejection fraction <35%), 1091 were elderly (≥65 years). Propensity scores for older age, estimated for each of the 2707 patients, were used to assemble a cohort of 603 pairs of younger and older patients, balanced on 66 baseline characteristics.
Results
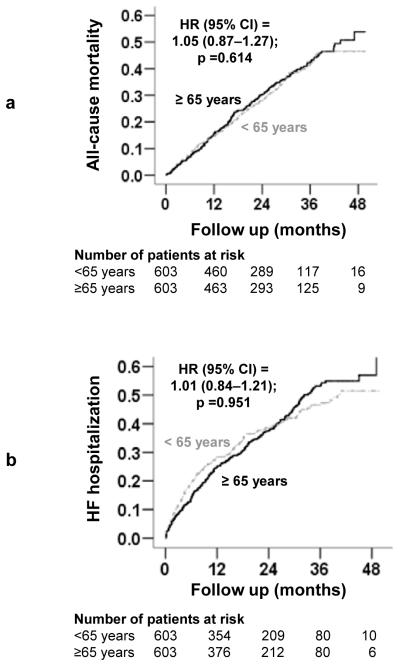
All-cause mortality occurred in 33% and 36% of younger and older matched patients respectively during 4 years of follow-up (hazard ratio {HR} associated with age ≥65 years, 1.05; 95% confidence interval {CI}, 0.87—1.27; P=0.614). HF hospitalization occurred in 38% and 40% of younger and older matched patients respectively (HR, 1.01; 95% CI, 0.84–1.21; P=0.951). Among 603 pairs of unmatched and unbalanced patients, all-cause mortality occurred in 28% and 36% of younger and older patients respectively (HR, 1.34; 95% CI, 1.10–1.64; P=0.004) and HF hospitalization occurred in 34% and 40% of younger and older unmatched patients respectively (HR, 1.24; 95% CI, 1.03–1.50; P=0.024).
Conclusion
Significant bivariate associations suggest that older age is a useful marker of poor outcomes in patients with advanced chronic systolic HF. However, lack of significant independent associations suggests that older age per se has no intrinsic effect on outcomes in these patients.
Keywords: Age, heart failure, mortality, hospitalization
1. Introduction
The majority of heart failure (HF) patients are ≥65 years, and most deaths and HF-related hospitalizations in HF patients occur in this patient group [1]. We have previously demonstrated that in a propensity-matched cohort of ambulatory patients with mild to moderate chronic HF, older age (≥65years) was associated with increased mortality but not hospitalization [2]. However, associations between older age and outcomes in patients with chronic advanced systolic HF remain less clear and furthermore have not been studied by propensity-matched design. The refore, the objective of the current study was to examine the independent effect of older age on outcomes in chronic advanced systolic HF patients using a propensity-matched design.
2. Methods
2.1 Data source and patients
This study was conducted using retrospective analysis of public-use copies of the Beta-Blocker Evaluation of Survival Trial (BEST) datasets obtained from the National Heart, Lung, and Blood Institute (NHLBI). The design and findings of the BEST have been described previously in detail [3]. Briefly, the BEST was a multicenter randomized controlled trial of the beta-blocker bucindolol in chronic systolic HF. Over a three-year period, 2708 patients with advanced systolic HF were enrolled from 90 different sites across the United States and Canada. All patients had New York Heart Association class III or IV symptoms and a left ventricular ejection fraction of <35%. Over 90% of patients enrolled were receiving angiotensin-converting enzyme (ACE) inhibitors, diuretics, and digitalis. Of the 2707 patients in the public-use copy of the BEST dataset (one patient did not consent to be included in the public-use copy), 1091 (40%) patients were ≥65 years. We categorized patients into two age groups: younger (<65 years) and older (≥65 years) with 1091 (40%) patients comprising the ≥65 year group
2.2 Study outcomes
Primary outcomes were all-cause mortality and HF hospitalization. Secondary outcomes included cardiovascular mortality, HF mortality and all-cause hospitalization. All outcomes were centrally adjudicated.
2.3 Assembly of a balanced study cohort
Due to significant imbalances in baseline characteristics between older and younger patients (Figure 1), we used propensity score matching to assemble a cohort of patients in which older and younger patients would be well-balanced on all measured baseline covariates (Table 1) [4-16]. We began by using a non-parsimonious multivariable logistic regression model to estimate propensity score for age ≥65 years for each of the 2707 participants. In the model, an age ≥65 years was used as the dependent variable and all clinically relevant baseline characteristics (Figure 1) were included as covariates [6-16]. Using a greedy matching protocol described elsewhere in detail [6-16], we were able to match 603 of the 1091 older patients with 603 patients <65 years old who had similar propensity scores.
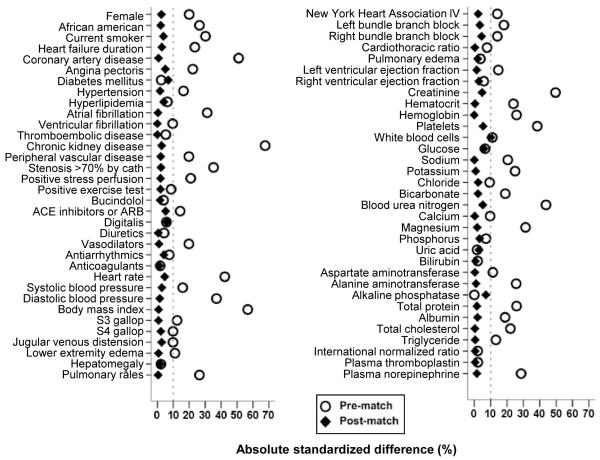
Figure 1.
Love plot displaying absolute standardized differences for baseline characteristics between young (<65 years) and older (≥65 years) patients with advanced systolic heart failure, before and after propensity score matching
(ACE=angiotensin-converting enzyme; ARB=angiotensin receptor blocker)
Table 1.
Baseline patient characteristics by age before and after propensity matching
| Before propensity matching** | After propensity matching* | |||||
|---|---|---|---|---|---|---|
| n (%) or mean (±SD) | Age <65 years (n=603) |
Age ≥65 years (n=603) |
P value |
Age <65 years (n=603) |
Age ≥65 years (n=603) |
P value |
| Female | 139 (23) | 119 (20) | 0.160 | 125 (21) | 119 (20) | 0.718 |
| African American | 154 (26) | 126 (21) | 0.056 | 121 (20) | 126 (21) | 0.768 |
| Current smoker | 127 (21) | 84 (14) | 0.001 | 92 (15) | 84 (14) | 0.549 |
| New York Heart Association IV | 42 (7) | 54 (9) | 0.202 | 50 (8) | 54 (9) | 0.757 |
| Past medical history | ||||||
| Heart failure duration, months | 46 (±48) | 53 (±52) | 0.009 | 52 (±50) | 53 (±52) | 0.634 |
| Coronary artery disease | 303 (50) | 398 (66) | <0.001 | 400 (66) | 398 (66) | 1.000 |
| Angina pectoris | 293 (49) | 327 (54) | 0.050 | 342 (57) | 327 (54) | 0.424 |
| Hypertension | 340 (56) | 363 (60) | 0.179 | 368 (61) | 363 (60) | 0.818 |
| Diabetes mellitus | 216 (36) | 237 (39) | 0.212 | 217 (36) | 237 (39) | 0.279 |
| Hyperlipidemia | 251 (42) | 272 (45) | 0.222 | 284 (47) | 272 (45) | 0.531 |
| Thromboembolic disease | 103 (17) | 117 (19) | 0.297 | 117 (19) | 117 (19) | 1.000 |
| Chronic kidney disease | 148 (25) | 263 (44) | <0.001 | 255 (42) | 263 (44) | 0.861 |
| Atrial fibrillation | 103 (17) | 154 (26) | <0.001 | 153 (25) | 154 (26) | 1.000 |
| Ventricular fibrillation | 56 (9) | 62 (10) | 0.561 | 62 (10) | 62 (10) | 1.000 |
| Peripheral vascular disease | 75 (12) | 114 (19) | 0.002 | 109 (18) | 114 (19) | 0.760 |
| Medications | ||||||
| Angiotensin-converting enzyme inhibitors or angiotensin receptor blocker |
590 (99) | 583 (97) | 0.217 | 577 (96) | 583 (97) | 0.441 |
| Bucindolol | 318 (53) | 299 (50) | 0.274 | 294 (49) | 299 (50) | 0.821 |
| Digitalis | 555 (92) | 543 (90) | 0.226 | 553 (92) | 543 (90) | 0.348 |
| Diuretics | 554 (92) | 559 (93) | 0.589 | 560 (93) | 559 (93) | 1.000 |
| Vasodilators | 241 (40) | 274 (45) | 0.055 | 277 (46) | 274 (45) | 0.911 |
| Anti-coagulants | 356 (59) | 350 (58) | 0.726 | 354 (59) | 350 (58) | 0.858 |
| Anti-arrhythmic drugs | 15 (3) | 14 (2) | 0.851 | 18 (3) | 14 (2) | 0.597 |
| Physical examination | ||||||
| Body mass index, kilogram/ m2 | 38.6 (±8.8) | 35.3 (±7.2) | <0.001 | 35.3 (±7.2) | 35.3 (±7.2) | 0.885 |
| Systolic blood pressure, mm Hg | 116 (±18) | 117 (±17) | 0.300 | 118 (±19) | 117 (±17) | 0.635 |
| Diastolic blood pressure, mm Hg |
73 (±12) | 70 (±10) | <0.001 | 70 (±11) | 70 (±10) | 0.790 |
| Heart rate per minute | 83.5 (±13.7) | 80.3 (±12.1) | <0.001 | 79.8 (±12.8) | 80.3 (±12.1) | 0.423 |
| Jugular venous distension | 0.41 (±0.49) | 0.47 (±0.50) | 0.032 | 0.46 (±0.50) | 0.47 (±0.50) | 0.650 |
| S3 gallop | 264 (44) | 255 (42) | 0.601 | 253 (42) | 255 (42) | 0.954 |
| S4 gallop | 117 (19) | 106 (18) | 0.415 | 101 (17) | 106 (18) | 0.762 |
| Pulmonary râles | 59 (10) | 88 (15) | 0.011 | 89 (15) | 88 (15) | 1.000 |
| Lower extremity edema | 143 (24) | 169 (28) | 0.087 | 167 (28) | 169 (28) | 0.949 |
| Laboratory data | ||||||
| Creatinine, mg/dl | 1.17 (±0.39) | 1.30 (±0.41) | <0.001 | 1.28 (±0.43) | 1.30 (±0.41) | 0.388 |
| Potassium, mEq/L | 4.27 (±0.47) | 4.34 (±0.47) | 0.009 | 4.34 (±0.50) | 4.34 (±0.47) | 0.873 |
| Sodium, mEq/L | 139 (±3) | 139 (±4) | 0.358 | 139 (±3) | 139 (±4) | 0.980 |
| Glucose, mg/dl | 139 (±79) | 138 (±80) | 0.967 | 134 (±72) | 138 (±80) | 0.319 |
| Cholesterol, mg/dl | 197 (±46) | 192 (±44) | 0.054 | 192 (±47) | 192 (±44) | 0.950 |
| Triglycerides, mg/dl | 229 (±189) | 207 (±179) | 0.041 | 206 (±174) | 207 (±179) | 0.912 |
| Plasma norepinephrine | 465 (±235) | 527 (±261) | <0.001 | 523 (±336) | 527 (±261) | 0.778 |
| Hemoglobin, g/dl | 14.2 (±1.7) | 13.9 (±1.6) | 0.003 | 13.9 (±1.6) | 13.9 (±1.6) | 0.999 |
| White blood cell, 103/μL | 7.6 (±2.0) | 7.5 (±2.5) | 0.663 | 7.3 (±2.0) | 7.5 (±2.5) | 0.083 |
| Platelet, 103/μL | 230 (±85) | 217 (±63) | 0.003 | 214 (±60) | 217 (±63) | 0.349 |
| X-ray | ||||||
| Pulmonary edema | 64 (11) | 71 (12) | 0.523 | 67 (11) | 71 (12) | 0.794 |
| Multiple gated acquisition scan | ||||||
| Left ventricular ejection fraction, % |
22.3 (±7.4) | 23.0 (±7.0) | 0.140 | 23.1 (±7.3) | 23.0 (±7.0) | 0.799 |
| Right ventricular ejection fraction, % |
34.2 (±12.2) | 35.2 (±11.2) | 0.147 | 34.8 (±12.0) | 35.2 (±11.2) | 0.626 |
The 603 pairs of post-match patients were assembled by a 1 to 1 propensity score matching algorithm that matched 603 of the 1091 patients ≥65 years with 603 patients <65 years who had similar propensity scores. This was completed to balance all measured baseline covariates between the two groups
The 603 pairs of pre-match patients were assembled by pairing the 603 matched patients ≥65 years with a random 603 patients <65 years from the 1616 pre-match patients <65 years. This was completed to assemble a pre-match cohort that would have the same sample size as the matched cohort
Because propensity score models are sample-specific adjusters and are not intended to be used for out-of-sample prediction or estimation of coefficients, measures of fitness and discrimination are not important to assess the models’ effectiveness. Instead, estimating pre- and post-match between-group absolute standardized differences for covariates is the best way to assess the efficacy of propensity score models [17]. Standardized differences directly quantify the bias in the means of covariates across the groups, expressed as a percentage of the pooled standard deviation. Therefore, we estimated pre- and post-match absolute standardized differences for each covariate for the 2707 and 1206 patients respectively and presented theresults as Love plots (Figure 1) [6-16]. An absolute standardized difference of 0% indicates no residual bias and an absolute standardized difference <10% is regarded as insignificant bias.
To ensure that comparison of the pre- and post-match associations would not be affected by differences in sample size and power between the pre- and post-match cohorts, we assembled a pre-match cohort of 1206 patients. We accomplished this by merging the 603 elderly matched patients with 603 younger patients who were randomly selected from the 1660 younger patients in the pre-match cohort. Thus, these 603 pairs of patients had the same sample size as the matched cohort but were not propensity matched and thus not balanced on baseline covariates (Table 1).
2.4 Statistical analysis
For descriptive analyses, we used Pearson Chi-square and Wilcoxon rank-sum tests for the pre-matched population, and McNemar’s test and paired sample t-tests for the matched population as appropriate. Kaplan-Meier survival analyses and Cox proportional hazard analyses were used to determine the association of age with various outcomes during the 23 months of mean follow-up. We repeated our analysis in the pre-match cohort of 1206 patients using three different statistical models: (1) unadjusted, (2) multivariable-adjusted, including all covariates used in the propensity score model, and (3) propensity score-adjusted.
To identify confounders associated with increased unadjusted mortality among older adults, we created separate multivariable models adjusting for sex, race, morbidities (coronary artery disease, hypertension, diabetes, atrial fibrillation and chronic kidney disease), medication use (bucindolol, ACE inhibitors or angiotensin receptor blockers, diuretics and digitalis), and clinical characteristics (body mass index, systolic and diastolic blood pressure, New York Heart Association class, and left and right ventricular ejection fractions). Subgroup analyses of matched patients were conducted to assess heterogeneity of the associations of aging with all-cause mortality. All statistical tests were two-tailed, and tests with P <0.05 were considered significant. All statistical tests were performed using SPSS for Windows Version 15 (SPSS Inc., Chicago, IL) [18].
3. Results
3.1 Baseline patient characteristics
Matched patients had a mean age of 56 (±7) and 71 (±4) years in younger and older groups respectively, 20% was female, and 20% was African American. Before matching, older patients were more likely to have coronary artery disease, atrial fibrillation and chronic kidney disease than younger patients. Baseline characteristics for both groups before and after matching are displayed in Table 1. After matching, absolute standardized differences between age groups were <10% for all measured covariates (with the exception of white blood cell count which was 10.2%) with most values <5% demonstrating substantial covariate balance across the groups (Fig 1).
3.2 Association of age and mortality
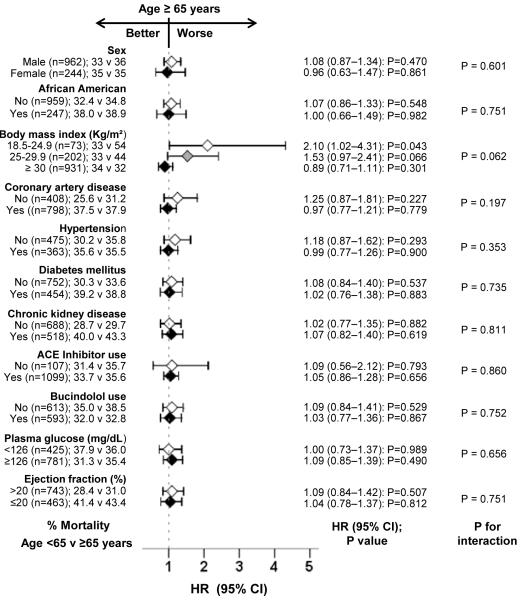
All-cause mortality occurred in 33% (202/603) and 36% (215/603) of matched younger and older patients respectively during 4 years of follow-up (hazard ratio {HR} when older patients are compared to younger patients, 1.05, 95% confidence interval {CI}, 0.87–1.27, P=0.614; Table 2 and Figure 2). Older age had no association with cardiovascular mortality but was significantly associated with increased risk of HF mortality (HR when older patients are compared to younger patients, 1.51, 95% CI, 1.07–2.14, P=0.020; Table 2). The association of age with mortality was homogeneous across subgroups of patients, except that among those with lower body mass index, older age was associated with increased mortality (Figure 3).
Table 2.
Age ≥65 years and outcomes in the matched cohort
| Outcomes | Events (%) | Absolute risk difference* (%) |
Hazard ratio (95% confidence interval) |
P value | |
|---|---|---|---|---|---|
| <65 years (n = 603) |
≥65 years (n = 603) |
||||
| All-cause mortality | 202 (33%) | 215 (36%) | +2% | 1.05 (0.87–1.27) | 0.614 |
| Cardiovascular mortality | 182 (30%) | 168 (28%) | − 2% | 0.91 (0.74–1.12) | 0.379 |
| Heart failure mortality | 52 (9%) | 80 (13%) | +5% | 1.51 (1.07–2.14) | 0.020 |
| All-cause hospitalization | 375 (62%) | 409 (68%) | +6% | 1.07 (0.93–1.23) | 0.372 |
| Heart failure hospitalization | 229 (38%) | 240 (40%) | +2% | 1.01 (0.84–1.21) | 0.951 |
Absolute risk differences were calculated by subtracting percent events in the <65 year group from the percent events in the ≥65 year group (before rounding)
Figure 2.
Kaplan-Meier plots for a) all-cause mortality and b) heart failure (HF) hospitalization by age group
(CI=confidence interval; HR=hazard ratio)
Figure 3.
Association between older age and all-cause mortality in subgroups of propensity score matched patients in BEST trial
(ACE=angiotensin-converting enzyme; CAD=coronary artery disease; CI=confidence interval; HR=hazard ratio)
Among the 603 pairs of pre-match patients, all-cause mortality occurred in 28% (170/603) and 36% (215/603) of younger and older patients respectively (unadjusted HR when older patients are compared to younger patients, 1.34; 95% CI, 1.10–1.64; p=0.004). This association was unaffected by sex and race (HR, 1.34; 95% CI, 1.10–1.65; p=0.004) or additional adjustment for cardiovascular morbidities (coronary artery disease, diabetes mellitus, atrial fibrillation, hypertension, and peripheral arterial disease) (HR, 1.25; 95% CI, 1.02–1.53; p=0.035). When chronic kidney disease (CKD) was added to the model, the association between older age and mortality became non-significant (HR, 1.14; 95% CI, 0.93–1.40; p=0.224). The association also became non-significant when adjusted for CKD alone (HR, 1.20; 95% CI, 0.98–1.47; p=0.084). Unadjusted, multivariable-adjusted and propensity-adjusted associations of older age with cause-specific mortalities among the 603-pairs of pre-match patients are displayed in Table 3.
Table 3.
Age ≥65 years and outcomes in the pre-match cohort
| Outcomes | Events (%) | Absolute risk difference* (%) |
Hazard ratio (95% confidence interval) |
P value | |
|---|---|---|---|---|---|
| <65 years (n = 603) |
≥65 years (n = 603) |
||||
| All-cause mortality | |||||
| Unadjusted | 170 (28%) | 215 (36%) | +8% | 1.34 (1.10–1.64) | 0.004 |
| Multivariable-adjusted | --- | --- | --- | 1.13 (0.90–1.42) | 0.287 |
| Propensity-adjusted | --- | --- | --- | 1.10 (0.88–1.37) | 0.394 |
| Cardiovascular mortality | |||||
| Unadjusted | 151 (25%) | 168 (28%) | +3% | 1.18 (0.95–1.47) | 0.145 |
| Multivariable-adjusted | --- | --- | --- | 0.97 (0.76–1.24) | 0.792 |
| Propensity-adjusted | --- | --- | --- | 0.94 (0.74–1.19) | 0.622 |
| Heart failure mortality | |||||
| Unadjusted | 48 (8%) | 80 (13%) | +5% | 1.77 (1.24–2.54) | 0.002 |
| Multivariable-adjusted | --- | --- | --- | 1.41 (0.93–2.15) | 0.105 |
| Propensity-adjusted | --- | --- | --- | 1.28 (0.88–1.88) | 0.202 |
| All-cause hospitalization | |||||
| Unadjusted | 345 (57%) | 409 (68%) | +11% | 1.30 (1.13–1.50) | <0.001 |
| Multivariable-adjusted | --- | --- | --- | 1.10 (0.94–1.30) | 0.250 |
| Propensity-adjusted | --- | --- | --- | 1.16 (0.99–1.34) | 0.067 |
| Heart failure hospitalization | |||||
| Unadjusted | 203 (34%) | 240 (40%) | +6% | 1.24 (1.03–1.50) | 0.024 |
| Multivariable-adjusted | --- | --- | --- | 1.05 (0.85–1.30) | 0.651 |
| Propensity-adjusted | --- | --- | --- | 1.14 (0.93–1.40) | 0.216 |
Absolute risk differences were calculated by subtracting percent events in the <65 year group from the percent events in the ≥65 year group (before rounding)
3.3 Association of age and hospitalization
HF hospitalization occurred in 38% (229/603) and 40% (240/603) of younger and older matched patients respectively (HR when older patients are compared to younger patients, 1.01, 95% CI, 0.84–1.21, P=0.951; Table 2 and Figure 2). Older age also had no association with all-cause mortality (Table 2). Among the 603 pairs of pre-match patients, HF hospitalization occurred in 34% and 40% of younger and older patients respectively (HR associated with older age, 1.24; 95% CI, 1.03–1.50; p=0.024; Table 3). Unadjusted, multivariable-adjusted and propensity-adjusted associations of older age with HF and all-cause hospitalizations among the pre-match cohort of 1206 patients are displayed in Table 3.
Discussion
Findings from the current study demonstrate that in patients with advanced systolic HF, older age was associated with increased mortality and hospitalization, but this association was not independent in nature. The significant bivariate associations suggest that older age remains an important predictor of poor outcomes in these patients. However, the lack of an intrinsic association of age with poor outcomes suggests that older age by itself may not add to the already poor prognosis of advanced systolic HF patients and that age alone should not be used as a basis for treatment decisions. These findings are important as most HF patients are ≥65 years and HF is the leading cause of hospitalization in that age group [1].
Bivariate associations of age with poor outcomes are not surprising as aging is associated with increased morbidities and functional decline [19, 20]. This is demonstrated by the longer duration of HF and a greater comorbidity burden among older adults before matching. However, these associations disappeared among the balanced matched patients demonstrating lack of an intrinsic association. This lack of significant association is unlikely to be a function of power as these associations were significant in a pre-match unbalanced cohort with the same sample size as the matched cohort. Further, most of these associations lost significance after multivariable and propensity score adjustment (Table 3). Although multivariable regression models can adjust for baseline covariates, it cannot guarantee between-group baseline covariate balance [21]. Propensity score methods, in contrast, can be used to assemble cohorts in which covariate balance can be achieved and displayed in a tabular form. Further, designing of observational studies using propensity score methods is blinded to study outcomes [5].
Bivariate associations between age and poor outcomes among advanced systolic HF patients observed in the current study are similar to those in our previous study of patients with mild to moderate systolic and diastolic HF [2]. However, in that study, older age also had a significant independent association with increased mortality. This is likely due to the more advanced nature of HF and higher baseline mortality rates in the current study. Younger patients in the current study had a higher mortality (33%) than older patients with mild to moderate HF (29%) in that study [2]. It is possible that the high mortality rate of younger patients in advanced systolic HF may have minimized the independent impact of older age. It is also possible that adjustment for many more baseline characteristics in the current study may have reduced bias by those variables that were unmeasured in the previous study [2]. Taken together, these findings suggest that poor outcomes observed in older patients with advanced systolic HF are driven primarily by higher comorbidity, in particular CKD. However, whether more aggressive management of comorbidities would reduce the risk of poor outcomes in older adults with advanced systolic HF remains unknown.
A key limitation in all observational studies is that of potential confounding by an unmeasured covariate, and ours is no exception. A sensitivity analysis would normally help quantify the degree of a hidden bias that would need to be present to invalidate conclusions based on significant associations in an observational study. However, sensitivity analyses cannot be performed if the observed association is non-significant. Because the current study is based on data derived from a randomized clinical trial, they may not be generalizable to other older adults with HF[22]. However, findings from major HF registries suggest that the mean age (71, ±4 years) of HF patients in the community is similar to that of older patients in the current study [23, 24].
In conclusion, in patients with advanced chronic systolic HF, older age is an important marker of increased mortality and hospitalization, but has no intrinsic effect on outcome. Therapeutic decisions in older adults with advanced HF should not be biased on the basis of age alone.
Acknowledgement
“The Beta-Blocker Evaluation of Survival Trial (BEST) study was conducted and supported by the NHLBI in collaboration with the BEST Investigators. This Manuscript was prepared using a limited access dataset obtained by the NHLBI and does not necessarily reflect the opinions or views of the BEST Study or the NHLBI.”
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology [25].
Funding/Support: Dr. Ahmed is supported by the National Institutes of Health through grants (R01-HL085561 and R01-HL097047) from the National Heart, Lung, and Blood Institute and a generous gift from Ms. Jean B. Morris of Birmingham, Alabama
Footnotes
Conflict of Interest Disclosures: None
References
- [1].Lloyd-Jones D, Adams R, Carnethon M, et al. Heart disease and stroke statistics--2009 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:480–6. doi: 10.1161/CIRCULATIONAHA.108.191259. [DOI] [PubMed] [Google Scholar]
- [2].Wahle C, Adamopoulos C, Ekundayo OJ, Mujib M, Aronow WS, Ahmed A. A propensity-matched study of outcomes of chronic heart failure (HF) in younger and older adults. Arch Gerontol Geriatr. 2009;49:165–71. doi: 10.1016/j.archger.2008.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].The BEST Investigators A trial of the beta-blocker bucindolol in patients with advanced chronic heart failure. N Engl J Med. 2001;344:1659–67. doi: 10.1056/NEJM200105313442202. [DOI] [PubMed] [Google Scholar]
- [4].Rosenbaum PR, Rubin DR. The central role of propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- [5].Rubin DR. Using propensity score to help design observational studies: Application to the tobacco litigation. Health Services and Outcomes Research Methodology. 2001;2:169–188. [Google Scholar]
- [6].Adamopoulos C, Pitt B, Sui X, Love TE, Zannad F, Ahmed A. Low serum magnesium and cardiovascular mortality in chronic heart failure: a propensity-matched study. Int J Cardiol. 2009;136:270–7. doi: 10.1016/j.ijcard.2008.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Ahmed A, Pitt B, Rahimtoola SH, et al. Effects of digoxin at low serum concentrations on mortality and hospitalization in heart failure: a propensity-matched study of the DIG trial. Int J Cardiol. 2008;123:138–46. doi: 10.1016/j.ijcard.2006.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ahmed A, Young JB, Love TE, Levesque R, Pitt B. A propensity-matched study of the effects of chronic diuretic therapy on mortality and hospitalization in older adults with heart failure. Int J Cardiol. 2008;125:246–53. doi: 10.1016/j.ijcard.2007.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Ahmed MI, Ekundayo OJ, Mujib M, et al. Mild hyperkalemia and outcomes in chronic heart failure: A propensity matched study. Int J Cardiol. 2010 October;144:389–393. doi: 10.1016/j.ijcard.2009.04.041. Epud May 15, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Alper AB, Campbell RC, Anker SD, et al. A propensity-matched study of low serum potassium and mortality in older adults with chronic heart failure. Int J Cardiol. 2009;137:1–8. doi: 10.1016/j.ijcard.2008.05.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ekundayo OJ, Adamopoulos C, Ahmed MI, et al. Oral potassium supplement use and outcomes in chronic heart failure: A propensity-matched study. Int J Cardiol. 2010;141:167–74. doi: 10.1016/j.ijcard.2008.11.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Ekundayo OJ, Dell’italia LJ, Sanders PW, et al. Association between hyperuricemia and incident heart failure among older adults: A propensity-matched study. Int J Cardiol. 2010;142:279–87. doi: 10.1016/j.ijcard.2009.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Giamouzis G, Agha SA, Ekundayo OJ, et al. Incident coronary revascularization and subsequent mortality in chronic heart failure: A propensity-matched study. Int J Cardiol. 2010;140:55–9. doi: 10.1016/j.ijcard.2008.10.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Pitt B, Zannad F, Gheorghiade M, et al. Transatlantic similarities and differences in major natural history endpoints of heart failure after acute myocardial infarction: A propensity-matched study of the EPHESUS trial. Int J Cardiol. 2010 September 3;43(3):309–16. doi: 10.1016/j.ijcard.2009.03.036. Epud April 14, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Ritchie C, Ekundayo OJ, Muchimba M, et al. Effects of diabetes mellitus in patients with heart failure and chronic kidney disease: A propensity-matched study of multimorbidity in chronic heart failure. Int J Cardiol. 2009;134:330–5. doi: 10.1016/j.ijcard.2008.12.089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Sui X, Gheorghiade M, Zannad F, Young JB, Ahmed A. A propensity matched study of the association of education and outcomes in chronic heart failure. Int J Cardiol. 2008;129:93–9. doi: 10.1016/j.ijcard.2007.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Normand ST, Landrum MB, Guadagnoli E, et al. Validating recommendations for coronary angiography following acute myocardial infarction in the elderly: a matched analysis using propensity scores. J Clin Epidemiol. 2001;54:387–98. doi: 10.1016/s0895-4356(00)00321-8. [DOI] [PubMed] [Google Scholar]
- [18].SPSS for Windows, Rel. 15 program. SPSS Inc.; Chicago, IL: 2008. [Google Scholar]
- [19].Wolinsky FD, Callahan CM, Fitzgerald JF, Johnson RJ. Changes in functional status and the risks of subsequent nursing home placement and death. J Gerontol. 1993;48:S94–101. [PubMed] [Google Scholar]
- [20].Yancik R, Ershler W, Satariano W, Hazzard W, Cohen HJ, Ferrucci L. Report of the national institute on aging task force on comorbidity. J Gerontol A Biol Sci Med Sci. 2007;62:275–80. doi: 10.1093/gerona/62.3.275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Fitzmaurice G. Confounding: regression adjustment. Nutrition. 2006;22:581–3. doi: 10.1016/j.nut.2006.02.004. [DOI] [PubMed] [Google Scholar]
- [22].Fang J, Mensah GA, Croft JB, Keenan NL. Heart failure-related hospitalization in the U.S., 1979 to 2004. J Am Coll Cardiol. 2008;52:428–34. doi: 10.1016/j.jacc.2008.03.061. [DOI] [PubMed] [Google Scholar]
- [23].Fonarow GC, Abraham WT, Albert NM, et al. Association between performance measures and clinical outcomes for patients hospitalized with heart failure. Jama. 2007;297:61–70. doi: 10.1001/jama.297.1.61. [DOI] [PubMed] [Google Scholar]
- [24].Fonarow GC, Adams KF, Jr., Abraham WT, Yancy CW, Boscardin WJ. Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. Jama. 2005;293:572–80. doi: 10.1001/jama.293.5.572. [DOI] [PubMed] [Google Scholar]
- [25].Coats AJ. Ethical authorship and publishing. Int J Cardiol. 2009;131:149–50. doi: 10.1016/j.ijcard.2008.11.048. [DOI] [PubMed] [Google Scholar]