Abstract
Background and Objectives
To avoid the risk of developing contrast-induced nephropathy (CIN), it has been suggested that patients be subjected to a minimal necessary dose of contrast medium (CM-dose). However, often it is not easy to determine such a dose. This study assessed the usefulness of the ratio of CM-dose to estimated glomerular filtration rate (eGFR) in predicting the risks of CIN and sought to determine the safe level of CM-dose/eGFR in patients undergoing non-emergent percutaneous coronary intervention (PCI).
Subjects and Methods
We enrolled a total of 226 patients and calculated the ratio of CM-dose using grams of iodine (g-I) to eGFR, thus expressing it as g-I/eGFR. Among the CIN patients, those with ne-phropathy requiring dialysis (NRD) were also evaluated.
Results
Overall, there were 16 cases (7.1%) of CIN. On univariate and multivariate regression analysis, g-I/eGFR alone was found to be an independent predictor for CIN (hazard ratio=10.73, p<0.001). In an receiver operating characteristic analysis, fair discrimination for CIN was found at a g-I/eGFR level of 1.42 (C statics=0.867), and at this value, the sensitivity and specificity were 81.3% and 80%, respectively. Of patients (n=51) with g-I/eGFR ≥1.42, 23.6% (13/51) and 7.8% (4/51) developed, while those with g-I/eGFR <1.42 (n=171) had a lower incidences of CIN (1.8%, 2/171, p<0.001) and NRD (0%, 0/171, p<0.001).
Conclusion
It can be concluded that a g-I/eGFR <1.42 is a simple, useful indicator for determining the safe CM-dose based on the pre-PCI eGFR values. Furthermore, g-I/eGFR might have a close relationship with the development of NRD as well as CIN.
Keywords: Contrast media, Angiography, Acute kidney injury, Effect of drugs
Introduction
Contrast-induced nephropathy (CIN) has been commonly defined as a sudden, rapid deterioration in renal status after the administration of iodinated contrast medium (CM) in the absence of any other causes.1),2) It had been reported that CIN is associated not only with an increased in-hospital morbidity and mortality but also a 1-year mortality; at least in connection with percutaneous coronary intervention (PCI).3-6) Accordingly, risks of developing CIN pose a major challenge for interventional cardiologists. Moreover, a considerable number of patients with cardiovascular disease have multiple risk factors for developing CIN, which include impaired renal function presented as glomerular filtration rate (GFR) <60 mL/min/1.73 m2, advanced age, diabetes mellitus, hemodynamic instability, anemia, volume depletion, nephrotoxic medications and an exposure to a large volume of CM.1),3),4),7),8) Unfortunately, a majority of these risk factors have been reported to be both preexisting and non-modifiable. Therefore, many patients who are candidates for PCI are prone to these inevitable multiple risk factors.
Despite several positive studies, no preventive method other than hydration, has been convincingly shown to prevent CIN in high-risk patients.9),10) Because the amount of CM is one of the major modifiable risk factors, it has been desirable that more acceptable methods be developed to assess the dose of CM (CM-dose) depending on risks to each patients. It has been generally accepted that the risk of CIN increases with higher CM-dose and lower GFR.11-16) It has also been speculated that the risks of developing CIN are closely associated with the ratio of CM-dose to GFR. Accordingly, by combining the amount of CM with an estimated glomerular filtration rate (eGFR) into a single continuous risk factor, new methods have been developed.12) Thus, the ratio of CM-dose to eGFR has been proposed to predict risks of developing CIN.
Because commercially available CM has a varying concentration of iodine ranging from 140 to 400 mg-I/mL, unpredictable errors have occurred while expressing the CM-dose with volume and thereby establishing a safe CM-dose. To correct this, the ratio of grams of iodine (g-I) to eGFR ratio (g-I/eGFR) has been proposed as a breakthrough method in contrast to the conventional ratio of CM-dose to eGFR. To date, studies have been performed using g-I/eGFR in patients with acute myocardial infarction who had undergone primary PCI.15) It remains questionable as to whether the ratio of g-I/eGFR would be effective in predicting CIN in patients who had undergone elective PCI. Furthermore, even small volumes of CM in high-risk patients have been shown to cause CIN and threshold levels of CM are still being debated.17) Additionally, few studies have been conducted to examine the correlations between safe amounts of CM and the status of renal function in patients who have undergone elective PCI, using g-I/eGFR. Given the background, we conducted this prospective study to assess the usefulness of the ratio of g-I/eGFR in predicting the risk of developing CIN and to determine safe levels of g-I/eGFR in patients undergoing non-emergency PCI.
Subjects and Methods
Patients
This study was conducted in a single-institution setting at a university hospital (Keimyung University Dongsan Hospital, Daegu, Korea) from April of 2008 to January of 2009. Eligibility criteria were 19 years of age or older and a referral for coronary angiography (CAG) and PCI. Exclusion criteria were as follows: cardiogenic shock, pulmonary edema, emergent CAG, end-stage renal disease requiring dialysis, and previous administration of CM within 72 hours of PCI.
Study protocol
One day before the CAG, blood and urine samples were collected and the following biochemical markers were assessed: blood urea nitrogen (BUN), serum creatinine (Cr), hemoglobin (Hb), hematocrit (Hct), high-sensitivity C-reactive protein (hs-CRP), total cholesterol, low density lipoprotein (LDL)-cholesterol, and routine urinalysis. Follow-up laboratory tests were also performed for Hb, Hct, and BUN/Cr on days 1 and 2 following the PCI. In patients who showed serum Cr elevation following the PCI, a follow-up laboratory test was performed. An estimated GFR was calculated as creatinine clearance by the Modified Diet in Renal Disease (MDRD) study equation.18),19) A two dimensional echocardiography was obtained several days before the PCI and left ventricular ejection fraction (LVEF) was calculated using the biplane modified Simpson method. All patients were given the same hydration regimen with intravenous isotonic saline at a rate of 1 mL/kg/hr for 12 hours before and after PCI. However, the prophylactic use of medications (e.g., N-acetylcysteine) was not allowed in these patients.
After informed consent was obtained, all procedures were done at the operator's discretion. Both CAG and PCI were performed as per the standard techniques, via either femoral or radial approach. All the patients received aspirin and clopidogrel and they were also given glycoprotein IIb/IIIa receptor blockers and heparin at the discretion of the operator. In the current study, we used either iso-osmolar, non-ionic CM, iodixanol (Visipaque™ 320 mg-I/mL; GE Healthcare Korea, Seoul, Korea), or low-osmolar, non-ionic CM, iohexol (Bonorex™ 350 mg I/mL; Dai Han Pharm, Seoul, Korea). The amounts of delivered CM were measured using an automated contrast delivery injection system (ACIST™; ACIST Medical Systems, Inc, Minnesota, USA) with CM amount calculated as g-I.
CIN was defined as a 25% elevation or an absolute increase of >0.5 mg/dL (>44 umol/L) in the Cr level compared to baseline within 48 to 72 hours after PCI according to the definition of the CIN consensus working panel.4) Any cases of CIN in which in-hospital renal replacement therapy was required due to severe nephropathy were labeled as nephropathy requiring dialysis (NRD). The decision to initiate dialysis was at the discretion of the consulting nephrologist.
Statistical analysis
All statistical analyses were performed with Statistical Package for the Social Sciences (SPSS, release 15.0; SPSS Inc., Chicago, IL, USA). To identify the correlations between CIN and the clinical and laboratory parameters, a univariate analysis was done using the Mann-Whitney U-test. In addition, analysis of variance and Chi-square tests were performed for continuous and categorical variables, respectively. We regarded a p<0.05 as statistically significant. A multivariate logistic regression analysis was used to assess the correlation among those parameters whose statistical significance was demonstrated through a univariate analysis at a level of p<0.05 and previously well-known risk factors, which did not show a significant difference in this study. Models were developed with stepwise techniques, for which results were expressed as odds ratios (OR) with 95% confidence intervals (CI). Finally, the g-I/eGFR ratio was added to the model as a separate predictor to test for an interaction between the CM-dose and eGFR. Interactions between variables were investigated and g-I/eGFR showed significant correlations with serum Cr, eGFR, and CM dose. Therefore, we choose g-I/eGFR as a single variable on behalf of variables according to kidney function and CM dose. A receiver operating characteristic (ROC) curve was plotted and the area under the curve was calculated. This was used as an overall measure of CIN classification ability in the final regression model.
Results
Clinical and laboratory characteristics of the patients
A total of 466 consecutive patients were referred for CAG and PCI, and were subsequently screened between May 2008 and January 2009. Of these, 226 patients were eligible for this study. One hundred thirty-six patients with primary PCI or emergency PCI, 18 patients with renal replacement therapy, and 53 patients with a history of CM exposure within 72 hours due to multi-detector coronary computerized tomography were excluded based on exclusion criteria.
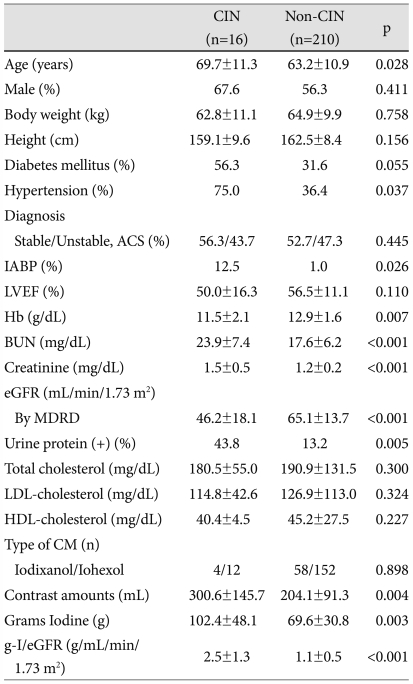
The study group was composed of 151 men and 75 women (63.7±11.0 years). Of the final 226 patients, CIN occurred in 16 patients (7.1%). Patients were divided into two groups based on the development of CIN: the CIN group (n=16) and the non-CIN group (n=210). Table 1 represents baseline characteristics of both groups of patients.
Table 1.
Baseline demographic data for the CIN and non-CIN patients
Values are mean±SD. CIN: contrast-induced nephropathy, IABP: intra-aortic balloon pump, LVEF: left ventricular ejection fraction, eGFR: estimated glomerular filtration rate, MDRD: equation of modified diet on renal disease study group, LDL: low density lipoprotein, HDL: high density lipoprotein, CM: contrast media, g-I/eGFR: ratio of delivered contrast media by grams of iodine and estimated glomerular filtration rate, ACS: acute coronary syndrome, BUN: blood urea nitrogen
The age and the incidence of hypertension were significantly higher in the CIN group. Further, of the baseline laboratory findings, the CIN group had a significantly lower degree of Hb and eGFR levels, a significantly higher degree of BUN and creatinine levels, and a significantly higher prevalence of positive urine protein dipstick results compared with the non-CIN group. The CIN group were also subjected to a higher dose of CM (g-I) and had a higher ratio of g-I/eGFR as compared with the non-CIN group. In the current study, there was no significant correlation between the types of delivered CM and the development of CIN.
Predictors of contrast-induced nephropathy
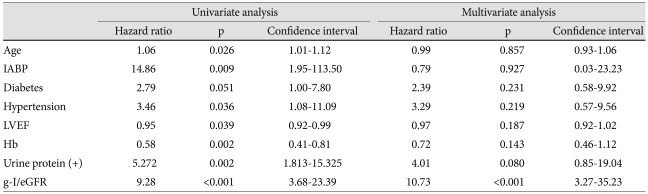
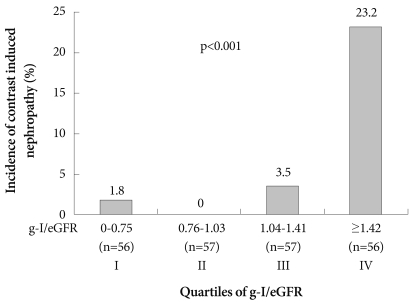
As shown in Table 2, upon univariate logistic regression analysis, age, usage of intraaortic balloon pump, hypertension, LVEF, Hb level, and g-I/eGFR were significantly correlated with the development of CIN. Although a history of diabetes was not within the range of statistical significance, it had a close correlation with the development of CIN (p=0.051). On multivariate analysis, only the ratio of g-I/eGFR remained as a significant independent risk factors for the development of CIN (g-I/eGFR, OR 9.786, 95% CI 3.40-28.15, p<0.001) (Table 2). In the analysis using g-I/eGFR ratio, quartiles showed a gradual increase in the incidence of CIN in quartiles III and IV. On the other hand, in quartiles I and II, the incidence of CIN were significantly lower than those of quartiles III and IV (Fig. 1).
Table 2.
Risk factors for CIN based on univariate and multivariate analyses
CIN: contrast-induced nephropathy, IABP: intra-aortic balloon pump, LVEF: left ventricular ejection fraction, Hb: hemoglobin, g-I/eGFR: ratio of delivered contrast media by grams of iodine and estimated glomerular filtration rate
Fig. 1.
Incidence of CIN according to quartiles of g-I/eGFR. Incidence of CIN is markedly higher in quartiles III and IV compared with quartiles I and II. CIN: contrast-induced nephropathy, g-I/eGFR: ratio of delivered contrast media by grams of iodine and estimated glomerular filtration rate.
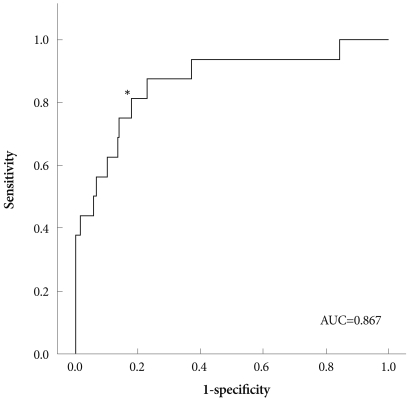
We analyzed g-I/eGFR to assess the predictive value of CIN using an ROC curve (Fig. 2). Results indicated that g-I/eGFR had a strong predictive value on the ROC curve (area under the curve=0.867). Further, the ROC curve analysis showed fair discrimination between the two groups at a g-I/eGFR level of 1.42. At this value, the sensitivity and specificity for development of CIN were 81.3% and 80%, respectively.
Fig. 2.
Receiver operating characteristic curves for the prediction of CIN using a g-I/eGFR ratio. The area under the curve for predicting CIN of g-I/eGFR was 0.867. The best cut-off value for g-I/eGFR was determined to be 1.42 (*). At this value, the sensitivity and specificity for the development of CIN were 81.3% and 80%, respectively. AUC: area under the curve, CIN: contrast-induced nephropathy, g-I/eGFR: ratio of delivered contrast media by grams of iodine and estimated glomerular filtration rate.
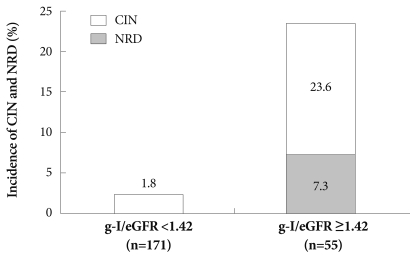
Of the patients (n=55) with g-I/eGFR ≥1.42, 23.6% (13/55) developed CIN while those with a g-I/eGFR <1.42 had a lower incidence of CIN (1.8%, 3/171; p<0.001) (Fig. 3).
Fig. 3.
Depiction of the incidence for CIN and NRD according to g-I/eGFR. Of patients with g-I/eGFR ≥1.42, there were significantly higher incidences of CIN and NRD compared with patients with g-I/eGFR <1.42 (p<0.001). CIN: contrast-induced nephropathy, NRD: nephropathy requiring dialysis, g-I/eGFR: ratio of delivered contrast media by grams of iodine and estimated glomerular filtration rate.
Impact of contrast-induced nephropathy on clinical course and outcome
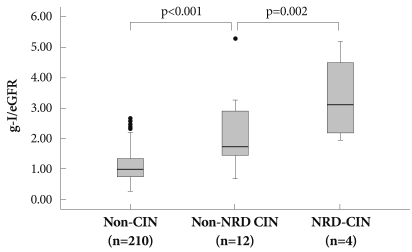
Of the 16 patients with CIN, 75% (12/16) had a transient impairment of renal function and then subsequently achieved spontaneous recovery; however, 25% (4/16) of them exhibited a critical clinical course and progressed to NRD, all of whom were started on renal replacement therapy. In our series, overall hospital mortality was 1.3% (3/226) and the in hospital mortality rate in the CIN group was 18.8% (3/16). Moreover, all cases of in-hospital mortality were associated with NRD. In other CIN cases, clinical outcomes were favorable and the renal function improved within a week to several months. Patients with CIN are commonly divided into two subgroups according to whether they were in need of dialysis: the non-NRD CIN group and the NRD group. In the current study, patients enrolled were divided into three groups: the non-CIN group (n=210), the non-NRD CIN group (n=12) and NRD-CIN group (n=4).
There was a significant difference in the g-I/eGFR level among the three groups. The mean g-I/eGFR level was 1.10±0.48 in the non-CIN group, 2.19±1.24 in the non-NRD CIN group and 3.35±1.46 in the NRD-CIN group. These results indicate that there was a gradual increased in the mean g-I/eGFR level in all three groups depending on the clinical features of CIN (non-CIN group vs. non-NRD CIN group, p<0.001; non-CIN group vs. NRD-CIN group, p<0.001; non-NRD CIN group vs. NRD-CIN group, p=0.002) (Fig. 4). Furthermore, all cases of NRD were consistently found to develop at a level of g-I/eGFR ≥1.42 based on the above-mentioned analysis of the ROC (Fig. 2).
Fig. 4.
Relationship between the g-I/eGFR ratio and clinical course after exposure to contrast Medium. g-I/eGFR levels (mean±SD) were significantly correlated with clinical courses of renal complication after PCI. g-I/eGFR: ratio of delivered contrast media by grams of iodine and estimated glomerular filtration rate, CIN: contrast-induced nephropathy, PCI: percutaneous coronary intervention.
Discussion
According to the results of the current prospective, observational study, it can be inferred that the ratio of g-I/eGFR may be the most significant predictor of CIN as compared with other previous well-known predictors. Besides, a close relationship was established between the ratio of g-I/eGFR, the incidence of CIN, and the clinical course of renal complication after PCI. In our series, there was a significant correlation between the ration of g-I/eGFR and the incidence of CIN irrespective of other combined risk factors. It can therefore be concluded that the ratio of g-I/eGFR is a simple, useful indicator for determining the safe dose of CM based on the pre-procedural eGFR values for elective PCI.
Estimation of a safe dose of contrast medium for elective percutaneous coronary intervention
Patients with multiple non-modifiable risk factors of developing CIN have been subjected to the minimal necessary dose of CM; however, the definition of an acceptable CM-dose for individual patients has been unclear. Of numerous risk factors for developing CIN, the CM-dose is a potentially modifiable one that can be controlled at the discretion of operators. Determination of a safe dose of CM based on the ratio of g-I/eGFR level would therefore be mandatory for establishing the acceptable CM-dose prior to PCI in individual patients.
The term CM/eGFR has been coined based on a pharmacotoxic mechanism: the CM-dose displays a positive correlation with the systemic exposure to CM and a negative correlation with the systemic clearance.20) The increased amount of CM and the decreased level of eGFR are closely associated with the development of CIN. Accordingly, a formula based on the ratio of the estimated CM-dose to eGFR might have a prognostic value in predicting risks for developing CIN.
To date, many efforts have been made to estimate a safe CM-dose using the above pharmacotoxic models. In 1989, Cigarroa et al.11) proposed a formula, according to which the maximal safe CM-dose was determined using {the volume of CM/body weight (kg)} solely based on the concentration of Cr. Recently, more accurate estimations of renal function have become possible using Cockcroft-Gault and MDRD equations.18),19),21) Since the CM-dose/eGFR was first introduced,12) clinical studies have been conducted in 3,179 unselected patients undergoing PCI, and these studies reported that CM volume/eGFR of <3.7 might be a useful indicator in determining the volume of CM that would not trigger the occurrence of CIN.14)
With respect to CM-dose, grams iodine is the preferred expression because various concentrations of iodine contained in a CM are used for CAG ranging from 140 to 400 mg-I/mL. Therefore, g-I/eGFR has been proposed as an alternative to the conventional CM-dose/eGFR ratio. Thus, the experience of CIN from one type of CM to another could be expanded based on the idea of expressing the dose of g-I.15)
In our series, the safe g-I/eGFR ratio was 1.42 which was somewhat higher than the value 1.0 previously reported from patients who had undergone primary PCI due to acute myocardial infarction.22) Our clinical series of cases consisted of controlled patients who were scheduled for elective PCI with appropriate hydration without other nephrotoxic agents. Little data is available from selective studies of CIN in cases of elective PCI using g-I/eGFR. Contrary to primary PCI cases, in scheduled PCI physicians can obtain sufficient information for safe CM-dose estimation prior to the procedure. Therefore, results of the current study have more potent clinical implications than previous studies.
Clinical implications of grams of iodine/estimated glomerular filtration rate associated with the development of contrast-induced nephropathy and nephropathy requiring dialysis
Of clinical importance, a g-I/eGFR ratio of 1.42 was also significantly correlated with a risk of developing NRD. CIN has a variable degree of clinical courses and outcomes. In other words, most cases of CIN have shown a mild transient impairment of renal function and benign clinical course, although a smaller number of patients had critical renal function deteriorated and were therefore, in need of renal replacement therapy (NRD). Moreover, it has also been reported that this critical form of CIN is associated with a higher degree of in-hospital mortality.3) In this study, there was a significant correlation of the g-I/eGFR level and the clinical courses of renal complication after PCI. In patients with a g-I/eGFR level ≥1.42, the incidence of CIN was 23.6% and that of NRD was 7.3%, with an in-hospital mortality rate of 5.9%. However, in patients with a g-I/eGFR <1.42, CIN occurred at an incidence 2.8% and none presented an NRD or an in-hospital mortality.
Clinical implications of the current study are that g-I/eGFR may represent a useful predictor for the occurrence of CIN and its clinical course after CIN. Therefore, a more careful consideration of a safe CM-dose should be mandatory in patients who are at increased risk for developing CIN based on a decreased eGFR prior to the PCI. Often, it has been the case that PCI treatment for complex lesions is associated with a large amount of CM administration. In these high-risk patients, we should consider the g-I/eGFR ratios and then maintain the CM-dose consistently lest it should exceed the CM-dose. In some cases, staged procedures should also be considered to minimize the chance for CIN.
A pre-interventional determination of an adequate CM-dose, based on the ratio of the g-I/eGFR, might be helpful in preventing CIN and NRD.
Limitations
Limitations of the current study are as follows.
Two different types of CM were used: non-ionic low-osmolar contrast media, iohexol and iso-osmolar contrast media, iodixanol and the selection CM was not randomized. Accordingly, there is an inevitable operator bias in the choice of CM. However, the current study was not meant to examine the relationship between the type of CM and risks of CIN and further, there was no significant difference of incidence of CIN according to type of CM. As compared with ionic high-osmolar contrast media, non-ionic low-osmolar contrast media (LOCM) has shown a less frequent development of CIN.23) Further, there is still a controversy as to whether iso-osmolar contrast media (IOCM) provides benefit over LOCM, although patients with both chronic renal insufficiency and diabetes mellitus may benefit from IOCM.24-27) Furthermore, the concept of expressing the CM-dose as g-I was devised to compensate for the concentration of iodine in different types of CM. To date, there has been no definite conclusion about the difference in the risk of CIN between IOCM and LOCM. Further studies with various types of contrast agents are warranted to confirm the efficacy of the equation in the context of various iodine concentrations.
Conclusions
In cases of elective PCI, the ratio of the amount of systemic exposure of CM to eGFR, expressed as g-I/eGFR, has a prognostic value in predicting the occurrence of CIN. Furthermore, the ratio of g-I/eGFR might have a close relationship with the development of NRD as well as CIN.
Based on our results, it can be concluded that a ratio of g-I/eGFR of <1.42 is a simple, useful indicator for determining a safe amount of CM based on the pre-procedural eGFR values for elective PCI.
A pre-interventional determination of adequate CM-dose, based on g-I/eGFR, might be helpful to avoid CIN and NRD.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Murphy SW, Barrett BJ, Parfrey PS. Contrast nephropathy. J Am Soc Nephrol. 2000;11:177–182. doi: 10.1681/ASN.V111177. [DOI] [PubMed] [Google Scholar]
- 2.Porter GA. Contrast-associated nephropathy: presentation, pathophysiology and management. Miner Electrolyte Metab. 1994;20:232–243. [PubMed] [Google Scholar]
- 3.McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368–375. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 4.McCullough PA, Adam A, Becker CR, et al. Epidemiology and prognostic implications of contrast-induced nephropathy. Am J Cardiol. 2006;98:5K–13K. doi: 10.1016/j.amjcard.2006.01.019. [DOI] [PubMed] [Google Scholar]
- 5.Rihal CS, Textor SC, Grill DE, et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002;105:2259–2264. doi: 10.1161/01.cir.0000016043.87291.33. [DOI] [PubMed] [Google Scholar]
- 6.Dangas G, Iakovou I, Nikolsky E, et al. Contrast-induced nephropathy after percutaneous coronary interventions in relation to chronic kidney disease and hemodynamic variables. Am J Cardiol. 2005;95:13–19. doi: 10.1016/j.amjcard.2004.08.056. [DOI] [PubMed] [Google Scholar]
- 7.Morcos SK. Contrast media-induced nephrotoxicity: questions and answers. Br J Radiol. 1998;71:357–365. doi: 10.1259/bjr.71.844.9659127. [DOI] [PubMed] [Google Scholar]
- 8.Lee KH, Lee SR, Kang KP, et al. Periprocedural hemoglobin drop and contrast-induced nephropathy in percutaneous coronary intervention patients. Korean Circ J. 2010;40:68–73. doi: 10.4070/kcj.2010.40.2.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Namgung J, Doh JH, Lee SY, Hur WS, Park SW, Lee WR. Effect of N-acetylcysteine in prevention of contrast-induced nephropathy after coronary angiography. Korean Circ J. 2005;35:696–701. [Google Scholar]
- 10.Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med. 2008;148:284–294. doi: 10.7326/0003-4819-148-4-200802190-00007. [DOI] [PubMed] [Google Scholar]
- 11.Cigarroa RG, Lange RA, Williams RH, Hillis LD. Dosing of contrast material to prevent contrast nephropathy in patients with renal disease. Am J Med. 1989;86:649–652. doi: 10.1016/0002-9343(89)90437-3. [DOI] [PubMed] [Google Scholar]
- 12.Altmann D, Zwas D, Spatz A, et al. Use of the contrast volume estimated creatinine clearance ratio to predict renal failure after angiography. J Interv Cardiol. 1997;10:113–119. [Google Scholar]
- 13.Bartholomew BA, Harjai KJ, Dukkipati S, et al. Impact of nephropathy after percutaneous coronary intervention and a method for risk stratification. Am J Cardiol. 2004;93:1515–1519. doi: 10.1016/j.amjcard.2004.03.008. [DOI] [PubMed] [Google Scholar]
- 14.Laskey WK, Jenkins C, Selzer F, et al. Volume-to-creatinine clearance ratio: a pharmacokinetically based risk factor for prediction of early creatinine increase after percutaneous coronary intervention. J Am Coll Cardiol. 2007;50:584–590. doi: 10.1016/j.jacc.2007.03.058. [DOI] [PubMed] [Google Scholar]
- 15.Nyman U, Almen T, Aspelin P, Hellstrom M, Kristiansson M, Sterner G. Contrast-medium-Induced nephropathy correlated to the ratio between dose in gram iodine and estimated GFR in ml/min. Acta Radiol. 2005;46:830–842. doi: 10.1080/02841850500335051. [DOI] [PubMed] [Google Scholar]
- 16.Kim U, Kim YJ, Lee WJ, et al. The estimated glomerular filtration rate with using the Mayo clinic quardratic equation as a new predictor for developing contrast induced nephropathy in patients with angina pectoris. Korean Circ J. 2008;38:301–304. [Google Scholar]
- 17.McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol. 2008;51:1419–1428. doi: 10.1016/j.jacc.2007.12.035. [DOI] [PubMed] [Google Scholar]
- 18.Levey AS, Greene T, Schluchter MD, et al. Glomerular filtration rate measurements in clinical trials. Modification of Diet in Renal Disease Study Group and the Diabetes Control and Complications Trial Research Group. J Am Soc Nephrol. 1993;4:1159–1171. doi: 10.1681/asn.v451159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999;130:461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 20.Frennby B, Sterner G. Contrast media as markers of GFR. Eur Radiol. 2002;12:475–484. doi: 10.1007/s003300100864. [DOI] [PubMed] [Google Scholar]
- 21.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 22.Nyman U, Bjork J, Aspelin P, Marenzi G. Contrast medium dose-to-GFR ratio: a measure of systemic exposure to predict contrast-induced nephropathy after percutaneous coronary intervention. Acta Radiol. 2008;49:658–667. doi: 10.1080/02841850802050762. [DOI] [PubMed] [Google Scholar]
- 23.Barrett BJ, Carlisle EJ. Metaanalysis of the relative nephrotoxicity of high- and low-osmolality iodinated contrast media. Radiology. 1993;188:171–178. doi: 10.1148/radiology.188.1.8511292. [DOI] [PubMed] [Google Scholar]
- 24.Liss P, Persson PB, Hansell P, Lagerqvist B. Renal failure in 57,925 patients undergoing coronary procedures using iso-osmolar or low-osmolar contrast media. Kidney Int. 2006;70:1811–1817. doi: 10.1038/sj.ki.5001887. [DOI] [PubMed] [Google Scholar]
- 25.Aspelin P, Aubry P, Fransson SG, Strasser R, Willenbrock R, Berg KJ. Nephrotoxic effects in high-risk patients undergoing angiography. N Engl J Med. 2003;348:491–499. doi: 10.1056/NEJMoa021833. [DOI] [PubMed] [Google Scholar]
- 26.Davidson CJ, Laskey WK, Hermiller JB, et al. Randomized trial of contrast media utilization in high-risk PTCA: the COURT trial. Circulation. 2000;101:2172–2177. doi: 10.1161/01.cir.101.18.2172. [DOI] [PubMed] [Google Scholar]
- 27.Carraro M, Malalan F, Antonione R, et al. Effects of a dimeric vs a monomeric nonionic contrast medium on renal function in patients with mild to moderate renal insufficiency: a double-blind, randomized clinical trial. Eur Radiol. 1998;8:144–147. doi: 10.1007/s003300050356. [DOI] [PubMed] [Google Scholar]