Abstract
Overview
The horseshoe kidney is more prone to blunt abdominal trauma because of its low position and the presence of the isthmus across the midline. This is a rare case of complete transection of a horseshoe kidney at the isthmus due to blunt abdominal trauma with two sites of active extravasation on initial CT imaging. This extravasation was successfully treated by embolization with coils. Superselective embolization may be used for effective, minimally invasive control of active extravasation due to blunt renal trauma, even in kidneys with congenital malformations such as the horseshoe kidney.
Keywords: trauma, atelectasis, ARDS, acute lung injury, respiratory failure, spinal cord injury
Introduction
A 41-year-old morbidly obese woman, who was an unrestrained passenger in a rollover motor vehicle collision, was transferred to the Rocky Mountain Regional Level One Trauma Center after sustaining a C4-C5 fracture/subluxation. She arrived intubated, on vasopressor support, with a heart rate in the 40’s. She was a C-4 tetraplegic and was found to have bilateral vertebral artery injuries. The patient underwent prompt anterior and posterior internal fixation of her spine injury, and a tracheostomy was performed on post-injury day 5 for respiratory failure.
On hospital day 8 she developed a low-grade fever (38.4 C) and became increasingly hypoxemic with a Pa02 to FI02 (P:F) ratio of 57. Chest radiograph demonstrated collapse of the right lower lobe and FIO2 was increased to 100%. Flexible fiberoptic bronchoscopy was performed with slight improvement in ventilation due to suctioning out her tracheobronchial tree. She failed to show meaningful improvement four hours later, however, with a P:F ratio of 61 and persistent right lower lobe collapse (Figure 1).
Figure 1.
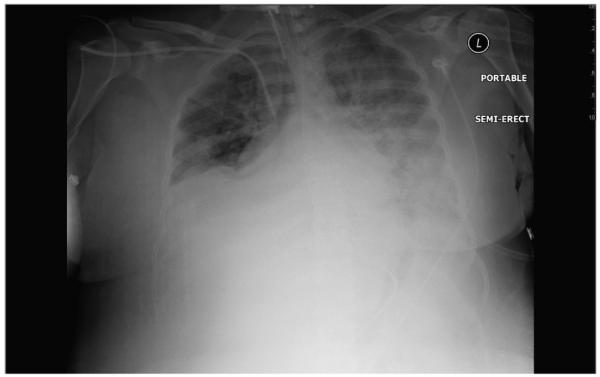
CXR indicating persistent right lower lobe collapse in our patient.
Attempts to increase PEEP to optimize oxygenation only worsened her condition, resulting in elevated peak airway pressures. Bronchoscopy was repeated with institution of selective intrabronchial air insuffl ation (SII) (Table 1) to resolve atelectasis in the right lower lobe. The associated lung expansion, which correlated with the patient’s immediate decrease in oxygen requirements, is demonstrated on this chest radiograph (Figure 2).
Table 1.
Selective intrabronchial air insufflation technique.
| Selective Intrabronchial Air Insufflation Technique |
|---|
| 1. Insert an (15 mm) airway adaptor from a Mallinckrodt 3.0 mm ID uncuffed tracheal tube on to the instillation port of the bronchoscope [Mallinckrodt Inc., St. Louis, MO] (Figures 3,4). |
| 2. Advance bronchoscope into the segment of collapse. |
| 3. Occlude the suction tubing. |
| 4. Attach manual resuscitator (i.e. bag valve mask). |
| 5. Apply 5-10 positive pressure breaths into every segment of collapsed lobe, while monitoring the patient’s hemodynamic status. |
Figure 2.
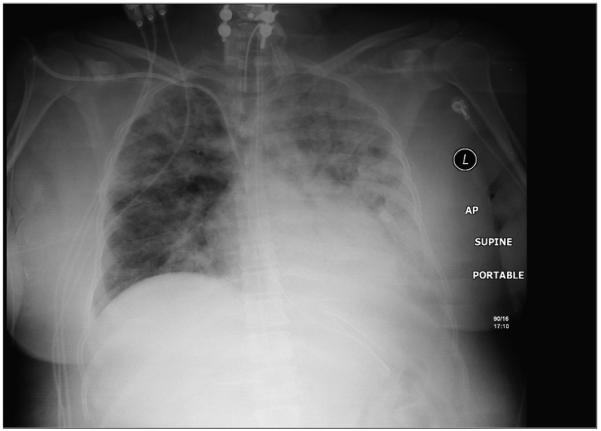
CXR in our patient demonstrative resolving atelectasis in our patient following SII.
Discussion
Lobar atelectasis is frequently encountered in the Surgical Intensive Care unit. The spectrum of collapse ranges from subsegmental atelectasis to collapse of an entire lung. Common etiologies include resorption atelectasis due to mucous plugging airway obstruction, passive atelectasis from hypoventilation, compressive atelectasis from abdominal distension, and adhesive atelectasis due to increased surface tension.1 Conventional management includes chest physiotherapy, bronchodilators, surfactant, DNase, positive end-expiratory pressure, and fiberoptic bronchoscopy. When these treatments fail, SII can become a useful tool for the intensivist.
Attempts to recruit lung volume via increased PEEP levels may lead to hemodynamic instability which is not tolerated in vasopressor-dependent conditions (tetraplegia, septic shock, CHF exacerbation, atrial fibrillation). Selective recruitment of lobar collapse utilizing SII, on the other hand, improves “targeted” lung volume and oxygenation with fewer hemodynamic effects.2 Additionally, SII is useful in non-intubated patients who are unable to participate in chest physiotherapy due to altered mental status (i.e. traumatic brain injury) chest wall pain (i.e. polytrauma with multiple rib fractures) and the morbidly obese (Table 2).
Table 2.
Patients, indications for therapy, their age, and average PaO2 to FiO2 ratios before and after selective intrabronchial air insufflation.
| Pt | Indication | Age | PaO2:FIO2 Before SII |
PaO2:FIO2 After SII |
|---|---|---|---|---|
| 1 | Non-compliant | 3 | 225 | 285 |
| 2 | Acute hypoxemia | 21 | 87 | 180 |
| 3 | Failed Conventional | 56 | 130 | 130 |
| 4 | Failed Conventional. | 19 | 340 | 425 |
| 5 | Acute hypoxemia | 28 | 90 | 240 |
| 6 | Failed Conventional | 62 | 165 | 180 |
| 7 | Failed Conventional | 26 | 123 | 123 |
| 8 | Failed Conventional | 44 | 192 | 188 |
| 9 | Failed Conventional | 69 | 124 | 130 |
| 10 | Acute hypoxemia | 86 | 61 | 188 |
| 11 | Acute hypoxemia | 44 | 77 | 97 |
| 12 | Acute hypoxemia | 21 | 60 | 338 |
| 13 | Failed Conventional | 12 | 160 | 195 |
| 14 | Acute hypoxemia | 18 | 74 | 218 |
| 15 | Failed Conventional | 60 | 146 | 172 |
| 16 | Acute hypoxemia | 23 | 100 | 200 |
| MEAN | 39 | 135 | 206 | |
The primary indication for SII is refractory lobar collapse in the absence of mucous plugging. In a series of 17 critically ill patients, bronchoscopy with SII was 82% effective in treating patients with acute lobar collapse, with optimal treatment in the first 72 hours3 (Figure 5). In a porcine model, lobar collapse showed a pressure-lung volume relationship similar to that found in acute respiratory distress syndrome.4 Once collapsed, substantial transpulmonary airway pressure must be generated in order to re-expand the distal airways. Aggressive non-selective recruitment maneuvers i.e. increased positive pressure with PEEP may lead to injurious transpulmonary pressures in the non-collapsed lung. In contrast, collapsed lobes re-expanded without overinflation when SII treatments were delivered, resulting in a safe and effective maneuver for refractory lobar collapse.
Figure 5.
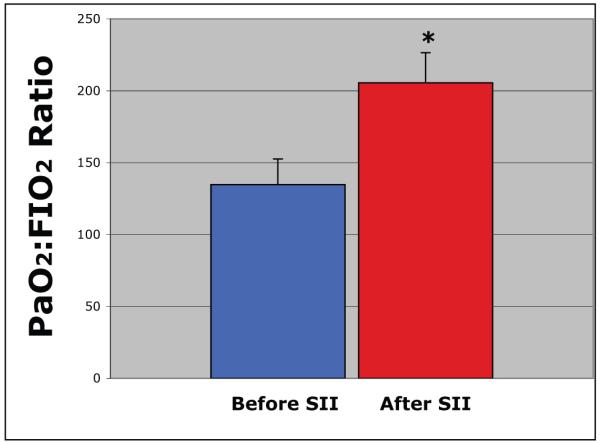
Selective intrabroncial insufflation improves oxygenation in 16 critically patients (P:F Before SII Treatment vs. p=0.001 After SII Treatment; p=0.001).
Figure 3.

Bronchoscope outfitted to permit us to complete a selective intralobar insufflation.
Figure 4.

Insufflation after selective intubation by fiberoptic bronchoscopy.
Footnotes
Disclosures The authors have no disclosures or conflicts of interest related to this manuscript.
References
- 1.Schindler M. Treatment of atelectasis: Where is the evidence? Critical Care. 2005 Aug;9:341–342. doi: 10.1186/cc3766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hansen LK, Sloth E, Nielsen J, Koefoed-Nielsen J, Lambert P, Lunde S, Larsson A. Selective recruitment maneuvers for lobar atelectasis: effects on lung function and central hemodynamics: an experimental study in pigs. Anesth Analg. 2006;102:1504–10. doi: 10.1213/01.ane.0000202477.29064.49. [DOI] [PubMed] [Google Scholar]
- 3.Haenel JB, Moore FA, Moore EE, Read RA. Efficacy of selective intrabronchial air insufflation in acute lobar collapse. Am J Surg. 1992 Nov;164(5):501–5. doi: 10.1016/s0002-9610(05)81189-4. [DOI] [PubMed] [Google Scholar]
- 4.Koefoed-Nielsen J, Hansen L Kjærsgaard, Larsson A. Does a solitary lobar collapse give pressure–lung volume relationship similar to that found in acute respiratory distress syndrome? A porcine experimental study. Clin. Physiol. Funct. Imaging. 2008;28:391–97. doi: 10.1111/j.1475-097X.2008.00819.x. [DOI] [PubMed] [Google Scholar]


