Abstract
Objective
Studies of the doctor–patient relationship have focused on the elaboration of power and/or authority using a range of techniques to study the encounter between doctor and patient. The widespread adoption of computers by doctors brings a third party into the consultation. While there has been some research into the way doctors view and manage this new relationship, the behavior of patients in response to the computer is rarely studied. In this paper, the authors use Goffman's dramaturgy to explore patients' approaches to the doctor's computer in the consultation, and its influence on the patient–doctor relationship.
Design
Observational study of Australian general practice. 141 consultations from 20 general practitioners were videotaped and analyzed using a hermeneutic framework.
Results
Patients negotiated the relationship between themselves, the doctor, and the computer demonstrating two themes: dyadic (dealing primarily with the doctor) or triadic (dealing with both computer and doctor). Patients used three signaling behaviors in relation to the computer on the doctor's desk (screen watching, screen ignoring, and screen excluding) to influence the behavior of the doctor. Patients were able to draw the doctor to the computer, and used the computer to challenge doctor's statements.
Conclusion
This study demonstrates that in consultations where doctors use computers, the computer can legitimately be regarded as part of a triadic relationship. Routine use of computers in the consultation changes the doctor–patient relationship, and is altering the distribution of power and authority between doctor and patient.
Keywords: Physician patient relationship, medical informatics, qualitative research, office visits, computers, patient-centered medicine
Introduction
The consultation is at the heart of any patient's interaction with the medical profession, and the success of the consultation depends on the quality of the communication between doctors and patients1 2 In this paper, we focus on a new element in contemporary consultations—the computer—which influences the balance in what have traditionally been dyadic communicative interactions.3
The literature on patient–doctor relationships is replete with calls for a shift in the balance of power between patient and doctor to favor the patient.4 Patient centeredness as a theoretical concept was first elaborated by Balint, who described doctors' use of the relationship as a therapeutic agent in and of itself.5 Balint understood that the relationship itself can affect the outcome of the consultation, independent of any therapeutic interventions.6 Patient centeredness is encapsulated in the Patient Centred Clinical Method,7 through which the consultation is directed toward assisting doctors to understand the patient's perspective. The Patient Centred Clinical Method is not a specific procedure, but rather a method of making doctors aware of the power imbalance, and compensating for it.
Drawing initially on the work of Szasz,8 the quality of shared decision-making in the doctor–patient relationship can be categorized into a series of ideal types, synthesizing common elements of a social interaction.9 Four models of doctor–patient relationships have been described: paternalistic, informative, interpretive, and deliberative,10 although increasingly the last two are being conflated into a single, shared model.11 Despite work aimed at shifting the balance of power, the dominant model has been the paternalistic, in which the doctor adopts the role of the guardian of the passive patient.12 By contrast, the other models each feature some form of shared power, and emphasize the importance of information as a resource for encouraging patients and doctors to work together to develop a treatment or investigation plan.11 A further refinement on ‘shared decision-making’ is the concept of relationship-centered care,13 which harks back to the work of Balint. Relationship-centered care positions the relationship itself as important to the outcomes of the consultation.14
The research about the patient–doctor relationship is explicit about the role that power (and its proxy, authority—the legitimate application of power) plays in the consultation,15 particularly with regard to the rebalancing of this power away from the doctor toward the patient. While the ideal situation is held to be a balanced distribution of the power in the consultation,16 more often this is not the case.4 17 18 Doctors are understood to hold significant power in the consultation, due to their standing as a professional, their control of knowledge, their social standing, and their status as healer.19 Some of that power comes from the patient's perceptions of doctors as a source of authority and the relationship they have, and some is ‘granted’ by bodies that gave doctors control over processes such as certification.15 20 That power has been shown to manifest itself in both the verbal language used4 and the body language.21 22 This power is now established to extend beyond humans—information technology is in itself adopting a position of power and authority in our society.23
In Australia, New Zealand, The Netherlands, and the UK, primary care is almost completely computerized, whereas in the USA, the hospital sector leads in computerization.24 At issue is how this computerization alters the balances inherent in the doctor–patient relationship.25 26 Such studies have shown that the computer does affect the consultation27 28; reduces ‘patient centeredness’,29 and increases the cognitive load on the doctor.30 Most of these studies have concentrated on doctor behaviors, with classifications revolving around the doctor's relationship with the computer.31 32 Importantly, what is now emerging is the concept of a ‘triadic’ relationship, denoting the interaction between doctor, patient, and computer.3 In doing so, we need to rethink the clinical methods we have used in the past, to allow for the significant influence the computer now exerts.26
This paper describes the elements and practices of this triadic relationship with particular emphasis on the patient.
Method
To examine the relationship, we chose an observational method, rather than eliciting accounts of the experiences of the actors. Despite the importance of theory informing ethnographic research, theoretical work on the medical consultation is sparse.33 We have chosen Erving Goffman's dramaturgical theories of human interaction to help us explore the phenomenon.34 Goffman views social interactions as one would a theatrical play; humans interact with each other according to perceived roles and accepted rules of behavior, much as one performs a scripted play. Importantly, when we say the patient's perspective, we do not mean that we have sought to understand the patient's perceptions or understandings of the interaction, simply that we have focused on the patient contribution to the triad—as distinct from other studies which have emphasized the doctor's contribution. A detailed discussion of the theoretical approach in this study is available online (www.jamia.org).
All participants were given an explanation of the study and plain-language statements. GPs gave signed consent, and patients were asked to give signed consent before the consultation, and reaffirm that consent at the end of the consultation. No patient withdrew after the consultation. Twenty GPs agreed to allow a single consulting session to be videotaped (2.5–3 h). We purposively recruited GPs who were significant computer users—defined as using clinical software for progress notes, as well as prescribing and test ordering. These GPs only generated paper when required by an external organization. The computerization of Australian general practice developed organically; there are no formal training programs in this area, and most practices have had to integrate the hardware into established rooms, with setups as varied as the doctors themselves.35 Each GP videotaped between five and 12 consultations. We were able to code 141 consultations with a further 34 consultations lost due to technical difficulties (failure of camera technique or battery life), and 17 due to patient refusal. This refusal rate (8.9%) is lower than that previously reported.36 Non-consenting patients tended to be female, and anticipating a consultation with an intimate examination.
The detail of the interpretive process has been described elsewhere.37 Each session of the consultation was digitized into video-management software which allowed the researchers to tag specific micro actions in the videos (eg, gaze direction) as well as observing the flow of the consultation.37 This tagging allowed sequential viewing of individual consultations, as well as comparisons across consultations. The hermeneutic methodology used (for details, see online supplement at www.jamia.org) requires sequential viewing of data with differing emphases on overarching themes and detailed elements. For this, a general practitioner and a sociologist viewed each consultation. They reviewed parts of the consultation and the whole visit as necessary.
Both the actors in the interaction (the human participants) and the actant (computer) were classified according to their ‘key’ or style: a term derived from Goffman that describes the attributes of each actor and actant that influence the flow of the interaction. Goffman describes this as being akin to a musical key signature.34 An example might be playing children, where one plays in an aggressive way (the key) and another passively. These keys shape the behaviors seen in different play settings, just as the behaviors can be seen as part of the overall way that children play. A further classification was made on the basis of the ‘behaviors’ or observable actions that have identifiable meanings within the context of the interaction. Behaviors differ from keys in that they are discreet actions, rather than an overarching style.
On the first pass, a framework of the overarching keys was developed. A second researcher reviewing the videos then tested the application of these keys. The hermeneutic framework required multiple viewings, starting from an overall assessment of patients into the two keys, followed by increasingly detailed descriptions of the behaviors seen, and the contexts in which they occurred. The framework was then tested several times on three reference groups: the extended research team, a wider group of academics, and several times with practicing clinicians. Adjustments were then made to the framework. A similar process was undertaken with the behaviors. This process continued until no further changes were suggested. Once this process was complete, there was little discordance between observers as to describing behaviors.
Results
A wide range of reasons for presentations occurred across the 141 consultations, encompassing acute to chronic presentations, and ranging from requests for certificates to the delivery of cancer diagnosis. The ratio of female to male patients (86:57) was similar to the ratio of all patients in Australian general practice.38 Analysis of the orientation of the patient's body and their conversation suggests that patient orientations in the relationship could be classified through two keys: dyadic, where the interaction with the physician was their predominant focus with the computer functioning as an adjunctive element, or triadic, where the patient approaches the computer as an integral element in the consultation. Two-thirds of the patients were dyadic in orientation, and one-third were triadic (table 1).
Table 1.
Sample
| GP characteristics | Consultations | |||
| Gender | Sample | Useable | Lost-technical | Lost-consent |
| Male | 13 | 103 | 4 | |
| Female | 7 | 38 | 13 | |
| Location | ||||
| Urban | 10 | 60 | 16 | |
| Rural | 10 | 81 | 16 | |
| Practice size | ||||
| Solo | 3 | 20 | 5 | |
| 1–5 | 12 | 75 | 26 | |
| >5 | 5 | 46 | 1 | |
| Total consults | 141 | 34 | 17 | 192 |
| Mean length | 12.66 min | Range 2 to 41 min | ||
| Patient characteristics | Female | 86 | Dyadic | 94 |
| Male | 57 | Triadic | 49 | |
There were more patients than consults, as several consults were for two people. Nine consults had a child as the main focus—classification is on the basis of parent. Children did not demonstrate a particular style.
Regardless of whether the patient's primary orientation was toward the physician (dyadic) or inclusive of the computer (triadic), patients exhibited three distinct behaviors. In the first behavior, screen watching, the patient focuses their attention on the screen. This is evident through both gaze and small shifts in posture. The second behavior, screen controlling, takes that focus further by bringing the computer (usually through its surrogate, the screen) into play in the consultation. Patients would, for example, point to the screen. In the third behavior, screen ignoring, the patient will deliberately disregard the screen, even to the extent of turning the body away, or subtly by placing a bent arm like a barrier between the screen and the patient. These behaviors can be employed variously within a consultation, whereas a key was maintained throughout the consultation regardless of individual behaviors.
Using our framework, we reviewed the videos to observe how these behaviors influenced the flow of the consultation. Patients exhibited actions that brought the computer into play as a source of information, as a source of authority and as a source of power. At its simplest, in the beginning of these consultations there were two phrases commonly uttered by patients who brought the computer into play. Any variation of ‘I'm here for a prescription’ or ‘I'm here for my test results’ would cause both humans to stare at the screen, regardless of whether of not the computer was to be used at that time. Clearly, retrieval of test results and generation of prescriptions are both tasks in which the involvement of the computer is seen to be crucial. This gaze matching has been called conjugate gaze,39 and contrasts with dysconjugate gaze when the humans are looking at different objects. For triadic patients, this period of conjugate gaze was followed by a period of dysconjugate gaze. The doctor would transfer their attention to the patient, while the patient would continue to focus their gaze on the screen (screen-watching behavior).
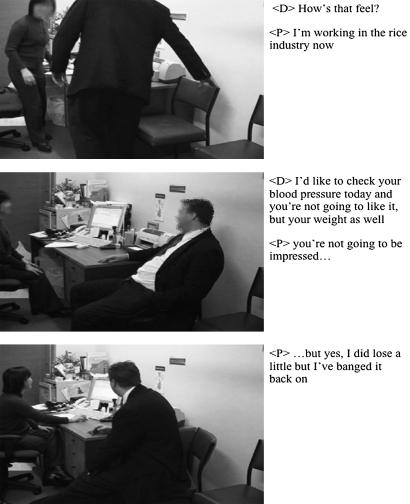
Figure 1 shows a sequence of three frames from a consultation that exhibits these features. This triadic patient has attended for a routine review of blood pressure. The computer contains significant information relating to past BP and weight measurements. In the first frame, the patient moves the chair to better create a triangle, signaling wordlessly that he is a triadic patient. In the second frame, he is engaging the GP as they negotiate the outcomes of the consultation. The patient places his elbow on the desk to exclude the computer screen, and the patient and doctor use conjugate gaze as they engage each other. In the third frame, the consultation has shifted—as a discussion moves to the patient's weight, the patient undertakes screen-engaging behavior, sitting forward and twisting direct gaze to the screen (past recordings of weight and blood pressure), drawing the doctor's gaze there as well.
Figure 1.
Shaping the consultation.
The fact that patients can change the course of the consultation is not new, but their involvement of the computer in doing so is. In the course of the consultation, the patient actively sat forward, stared at the computer, indicated it with his finger, and was comfortable with the doctor spending long periods of time at the computer. In a similar context, a dyadic patient will use different behaviors to repeatedly engage the doctor's gaze and attention, away from the computer.
Dyadic and triadic patients
In keeping with the hermeneutic methodology, the observed actions were analyzed both for what was observed and for the context of the consultation when it was observed. Each key exhibited unique behaviors, similar behaviors seen more or less frequently, and behaviors used in different contexts. Other influences such as doctor style and room setup also had to be taken into account. Triadic patients were much more active in involving the computer in the consultation. While both keys would use words—‘it's [the information] in there somewhere, isn't it?’—triadic patients tended to use their bodies more—indicating with hands, pointing, and actively leaning over the desk to see on the screen. They were observed to be directing the doctor toward the computer. Such active involvement contrasted with dyadic patients, who frequently used the same words, but in a passive fashion, sitting back and waiting for the doctor to reach their own conclusions. The same words, but with different physical moves, signal for triadic patients the assertion of power and authority in the consultation and, for dyadic patients, the ceding of both. Dyadic patients used screen-ignoring behaviors more often as a means of drawing the doctor away from the computer. Elbow pointing was common among dyadic patients and rare in triadic patients.
The context of the consultation played a role. In keeping with other research,40 consultations with a significant psychological component produced much greater engagement between the humans and less with the computer for both dyadic and triadic patients. In general, the components of the consultation where the computer provided most information into the consultation—test results, prescribing, and reminders for health activities—produced the greatest differences between dyadic and triadic patients. Other consultation components where the computer was more likely to become an active participant in the consultation involved it functioning as a repository for past history and consultations, and provider of disease information. During these elements of the consultation, triadic patients were more likely to actively encourage the doctor to engage with the computer.
Power
The computer has the ability to change the balance of power and authority in the consultation, and patients appeared to make differing uses of that potential. All the models of patient–doctor relationships have in common a sense that the doctor is the trustee of information that must be passed onto the patient. There is also recognition that patients too are custodians of information—usually of their condition, but also an understanding of their wider social milieu, and features such as their understanding of disease. The computer, however, is the custodian of information par excellence, and patients are able to use this for their benefit. Patients were often observed to break impasses in information by invoking the computer, by inviting the doctor to refer instead to the ‘better’ information repository. This activity was accompanied by screen-watching or screen-controlling behaviors, usually characterized by body shifts and hand gestures toward the computer. Extensive use of such behaviors was a defining feature of triadic patients, but was also seen in dyadic patients. Whereas triadic patients would exclude the screen with hand gestures, dyadic patients would do so with larger movements of their central body. Further examples with demonstrating figures are available online (www.jamia.org).
Limitations
There are many limitations to a study such as this, many trade-offs that are inherent in any research. By choosing an observational method, we have excluded the internal perspective that would have come from interviews with the participants. Observational work allows things to be seen that the actors in the consultation cannot perceive, yet it also ignores their perspectives. In examining a triadic relationship where one party cannot speak (the computer), it avoids the intentional fallacy, whereby the stated intentions of the actors are taken as sufficient explanation for observed phenomena. Choosing an observational method allowed us to examine a large number of consultations, but further work needs to be done to take into account those missing emic perspectives. In addition, there is always the risk that the act of being observed will alter the interaction. The use of video cameras (especially small modern ones) is less intrusive than a human observer; nevertheless, the results must be interpreted in that light.
The nature of the sampling frame meant that we concentrated on individual doctors rather than individual patients. While we observed doctors over a number of consultations, we saw patients only for a single consultation. We do not know therefore if patients change their consultation style for different consultations, or indeed with different doctors or problems. We are also aware that we were observing a system in flux. While computers have been commonplace for many years, they have only recently begun to be extensively used for clinical purposes. We do not know what influence this has had on the findings and whether or not patient behaviors will change over time. We do not know if patients are slowly transitioning from dyadic to triadic, or whether the determinants of dyadic and triadic keys arise from other factors. What is not in doubt is that computers will take a greater role, as shared electronic records and decision support become more pervasive.
We have focused only on a particular section of the total interactions between the three players, which for us constitutes the time when the triadic interaction is most prominent. Computers are altering the interaction in other ways, as patients gather information outside the consultation that comes into play.41 42 What we have described is therefore only part of a bigger picture. In particular, the interaction is shaped by many other things: room setups,43 the content of the consultation41 and other factors as yet unstudied.
Discussion
We have described here the development of a structure to examine patient activity in the consultation. While the description of dyadic/triadic may seem simplistic, our results show that patients have a specific key throughout the consultation and differing behaviors within it. The key/behavior interplay in the specific context of that particular consultation allows a deeper understanding of the three-way interaction. Consciously or unconsciously, patients are using the changed nature of the consultation and the presence of a third party to exert influence in the consultation, and therefore accrue power. Patients do so by involving or excluding the other two participants according to need. No longer are doctors seen as the ultimate authority in the consultation. In fact, the computer was often brought into play by patients to directly challenge the doctor's authority. Patients often direct the doctor toward the computer, or away from it, in response to queries or statements. They were able to draw gaze away from the computer, or toward it.
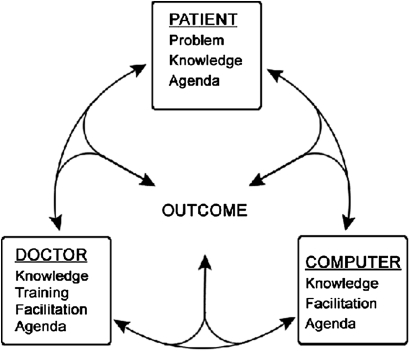
In the past, the consultation was characterized as a merging of doctor and patient agendas to meet a common, negotiated outcome.44 Previous models of the consultation, often constructed around notions of fixed power relationships, need to be redrawn to take into account the fluid nature of information flow. Triadic patients in particular were adept at altering the focus of the consultation between the three players, and may be harbingers of a future in which patients are much more actively involved in challenging the doctor's role. Our results suggest that computers allow power in the consultation to be shared in ways it has not been before. We argue that a more fluid model now exists, as characterized in figure 2.
Figure 2.
Consultation circle.
In this figure, the patient comes with a problem (the reason for encounter), an agenda, and their own knowledge of themselves and their diseases. Doctors come with their training, knowledge, and own agenda for the consultation. In the past, the doctor's training and knowledge would often trump that of the patient. In the contemporary consultation using computers, the computer has standing and authority with regard to the information it provides, and provides information to facilitate the consultation. Computers in effect come with their own agendas, in the form of reminders, suggestions for preventive health activities, decision support, and many other things as the role of the computer increases.
Conclusion
In the future, computers will have greater agency, not less, and patients will involve themselves in the three-way consultation in more creative ways—for example, through online communication, or through the plugging into computers of their own electronic records, creating a situation where they co-own the information in the computer. There is a need for further research into the possible effects such changes will make to patient outcomes. In the mean time, doctor awareness of the significance of different patient behaviors will enable them to understand the consultation dynamics better. This should involve training on methods of effectively involving the computer in the consultation, and recognition of the signals patients give toward that involvement.
The information in the consultation, and the power and authority that flow from it, are now more malleable, with each actor exhibiting power at different stages of the consultation. Information flows in a circle between the three actors until an outcome has been reached. The consultations we have described come from a system in change, one that is common across the world as we move to a connected ‘E-Health’ environment. In Australian general practice, paper is still prominent—prescription and test requests have to be printed. In the near future, all this is likely to happen electronically, and much more information will be shared in various electronic systems. The struggle in medical training has been to bring primacy to the patients' concerns, and to create in effect a patient-centered system. Whereas some authors have expressed concerns that the advent of the computer will swing the balance further away from the patient, our study shows that this is not necessarily the case. By democratizing and commoditizing information flows and authority in the consultation, we may in fact create truly patient-centered medicine, with the patient directing the action.
Supplementary Material
Footnotes
Competing interests: None.
Ethics approval: This study was conducted with the approval of the University of Melbourne Human Research Ethics Committee.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gask L, Usherwood T. ABC of psychological medicine. The consultation. BMJ 2002;324:1567–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simpson M, Buckman R, Stewart M, et al. Doctor–patient communication—the Toronto Consensus Statement. BMJ 1991;303:1385–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scott D, Purves I. Triadic relationship between doctor, computer and patient. Interact Comput 1996;8:347–63 [Google Scholar]
- 4.Ainsworth-Vaughn N. Claiming Power in Doctor–Patient Talk. New York: Oxford University Press, 1998 [Google Scholar]
- 5.Balint M. The Doctor, his Patient and the Illness. 2nd edn Edinburgh: Churchill Livingstone, 1964 [Google Scholar]
- 6.Balint E. The possibilities of patient-centered medicine. J R Coll Gen Pract 1969;17:269–76 [PMC free article] [PubMed] [Google Scholar]
- 7.Stewart M, Brown J, Weston W, et al. Patient-Centred Medicine: Transforming the Clinical Method. 2nd edn Oxford: Radcliffe Medical Press, 2003 [Google Scholar]
- 8.Szasz TH, Hollender M. A contribution to the philosophy of medicine: the basic models of the doctor–patient relationship. Arch Intern Med 1956;97:585–92 [DOI] [PubMed] [Google Scholar]
- 9.Weber M. Economy and Society; an Outline of Interpretive Sociology. New York: Bedminster Press, 1968 [Google Scholar]
- 10.Emanuel EJ, Emanuel LL. Four models of the physician–patient relationship. JAMA 1992;267:2221–6 [PubMed] [Google Scholar]
- 11.Charles C, Gafni A, Whelan T. Decision-making in the physician–patient encounter: revisiting the shared treatment decision-making model. Soc Sci Med 1999;49:651–61 [DOI] [PubMed] [Google Scholar]
- 12.Charles C, Whelan T, Gafni A, et al. Shared treatment decision making: what does it mean to physicians? J Clin Oncol 2003;21:932–6 [DOI] [PubMed] [Google Scholar]
- 13.Frankel R, Quill T. Integrating biopsychosocial and relationship centered care into mainstream medical practice: a challenge that continues to produce positive results. Families Systems and Health 2005;23:413–21 [Google Scholar]
- 14.Bowman MA. Good physician–patient relationship=improved patient outcome. J Fam Pract 1991;32:135–6 [PubMed] [Google Scholar]
- 15.Waitzkin H. The Politics of Medical Encounters: How Patients and Doctors Deal with Social Problems. New Haven, CT: Yale University Press, 1991 [Google Scholar]
- 16.Goodyear-Smith F, Buetow S. Power issues in the doctor–patient relationship. Health Care Anal 2001;9:449–62 [DOI] [PubMed] [Google Scholar]
- 17.Arborelius E, Timpka T. Comparison of patients' and doctors' comments on video-recorded consultations. Scand J Prim Health Care 1991;9:71–7 [DOI] [PubMed] [Google Scholar]
- 18.Foucault M, Gordon C. Power/Knowledge: Selected Interviews and other Writings, 1972–1977. Brighton, UK: Harvester Press, 1980 [Google Scholar]
- 19.Brody H. The Healer's Power. New Haven, CT: Yale University Press, 1992 [Google Scholar]
- 20.Starr P. The Social Transformation of American Medicine. New York: Basic Books, 1982 [Google Scholar]
- 21.Bensing JM, Kerssens JJ, Vanderpasch M. Patient-directed gaze as a tool for discovering and handling psychosocial problems in general-practice. J Nonverbal Behavior 1995;19:223–42 [Google Scholar]
- 22.Blanck PD, Buck R, Rosenthal R. Nonverbal Communication in the Clinical Context. University Park: Pennsylvania State University Press, 1986 [Google Scholar]
- 23.Gallivan M, Srite M. Information technology and culture: identifying fragmentary and holistic perspectives of culture. Inform Organ 2005;15:295–338 [Google Scholar]
- 24.Jha AK, Doolan D, Grandt D, et al. The use of health information technology in seven nations. Int J Med Inform 2008;77:848–54 [DOI] [PubMed] [Google Scholar]
- 25.Pearce CM, Trumble S. Computers can't listen—algorithmic logic meets patient centredness. Aust Fam Physician 2006;35:439–42 [PubMed] [Google Scholar]
- 26.Purves IN. Facing future challenges in general practice: a clinical method with computer support. Fam Pract 1996;13:536–43 [DOI] [PubMed] [Google Scholar]
- 27.Frankel R, Altschuler A, George S, et al. Effects of exam-room computing on clinician–patient communication: a longitudinal qualitative study. J Gen Intern Med 2005;20:677–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsu J, Huang J, Fung V, et al. Health information technology and physician–patient interactions: impact of computers on communication during outpatient primary care visits. J Am Med Inform Assoc 2005;12:474–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shachak A, Reis S. The impact of electronic medical records on patient–doctor communication during consultation: a narrative literature review. J Eval Clin Pract 2009;15:641–9 [DOI] [PubMed] [Google Scholar]
- 30.Shachak A, Hadas-Dayagi M, Ziv A, et al. Primary care physicians' use of an electronic medical record system: a cognitive task analysis. J Gen Intern Med 2009;24:341–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Booth N, Robinson P, Kohannejad J. Identification of high-quality consultation practice in primary care: the effects of computer use on doctor–patient rapport. Inform Prim Care 2004;12:75–83 [DOI] [PubMed] [Google Scholar]
- 32.Ventres W, Kooienga S, Marlin R, et al. Clinician style and examination room computers: A video ethnography. Fam Med 2005;37:276–81 [PubMed] [Google Scholar]
- 33.Scambler G, Britten N. System, lifeworld and doctor–patient interaction. In: Scambler G, ed. Habermas, Critical Theory and Health. London: Routledge, 2001:viii, 212. [Google Scholar]
- 34.Goffman E. Frame Analysis: An Essay on the Organization of Experience. York, PA: Northeastern University Press, 1974 [Google Scholar]
- 35.Pearce C, Walker H, O'Shea C. A visual study of computers on doctors' desks. Inform Prim Care 2008;16:111–17 [DOI] [PubMed] [Google Scholar]
- 36.Coleman T. Using video-recorded consultations for research in primary care: advantages and limitations. Fam Pract 2000;17:422–7 [DOI] [PubMed] [Google Scholar]
- 37.Pearce C, Dwan K, Phillips C, et al. Analysing the doctor–patient–computer relationship: the use of video data. Inform Prim Care 2006;14:221–6 [PubMed] [Google Scholar]
- 38.Australian Institute of Health and Welfare General Practice Activity in Australia 2006–7, 2008. http://www.aihw.gov.au/publications/index.cfm/title/10574
- 39.Argyle M, Dean J. Eye-contact, distance and affiliation. Sociometry 1965;28:289–304 [PubMed] [Google Scholar]
- 40.Chan WS, Stevenson M, McGlade K. Do general practitioners change how they use the computer during consultations with a significant psychological component? Int J Med Inform 2008;77:534–8 [DOI] [PubMed] [Google Scholar]
- 41.Anderson JG, Rainey MR, Eysenbach G. The impact of CyberHealthcare on the physician–patient relationship. J Med Syst 2003;27:67–84 [DOI] [PubMed] [Google Scholar]
- 42.Andreassen HK, Trondsen M, Kummervold PE, et al. Patients who use e-mediated communication with their doctor: new constructions of trust in the patient–doctor relationship. Qual Health Res 2006;16:238–48 [DOI] [PubMed] [Google Scholar]
- 43.Pearce C, Kumarpeli P, de Lusignan S. Getting seamless care right from the beginning—integrating computers into the human interaction. Stud Health Technol Inform 2010;155:196–202 [PubMed] [Google Scholar]
- 44.Middleton JF. The exceptional potential of the consultation revisited. J R Coll Gen Pract 1989;39:383–6 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.