Abstract
There is controversy over the impact of electronic health record (EHR) systems on cost of care and safety. The authors studied the effects of an inpatient EHR system with computerized provider order entry on selected measures of cost of care and safety. Laboratory tests per week per hospitalization decreased from 13.9 to 11.4 (18%; p<0.001). Radiology examinations per hospitalization decreased from 2.06 to 1.93 (6.3%; p<0.009). Monthly transcription costs declined from $74 596 to $18 938 (74.6%; p<0.001). Reams of copy paper ordered per month decreased from 1668 to 1224 (26.6%; p<0.001). Medication errors per 1000 hospital days decreased from 17.9 to 15.4 (14.0%; p<0.030), while near misses per 1000 hospital days increased from 9.0 to 12.5 (38.9%; p<0.037), and the percentage of medication events that were medication errors decreased from 66.5% to 55.2% (p<0.007). In this manuscript, we demonstrate that the implementation of an inpatient EHR with computerized provider order entry can result in rapid improvement in measures of cost of care and safety.
Introduction
Electronic health records (EHRs) have recently received renewed national attention as a critical tool to streamline patient care, reduce costs, and improve safety. The 2009 American Recovery and Reinvestment Act (ARRA) included the $19 billion Health Information Technology for Economic and Clinic Health (HITECH) provision to encourage use of EHRs. Significant drivers for implementation include the proposed financial incentives and penalties for hospitals and providers who do or do not demonstrate meaningful use.1
Organizations such as the Institute of Medicine and Leapfrog have been calling for implementation of EHRs, and computerized provider order entry (CPOE) in particular, for a number of years in order to improve patient safety and quality of care.2 3 The Center for Information Technology Leadership (CITL) estimates that 13.7% of laboratory tests are ordered because the ordering clinician does not have access to prior test results. The projected annual national benefit from reduced laboratory redundancy, laboratory administrative savings, and provider administrative savings is $31.8 billion.4 The RAND Corporation also cites a potential savings of tens of billions of dollars if EHRs are used effectively along with appropriate changes in healthcare.5 Yet it has been estimated that only 8% of hospitals have fully implemented CPOE systems, and those tend to be larger, not-for-profit, and teaching hospitals. It was reported that these hospitals showed a positive correlation between certain quality measures and CPOE implementation.6
Cost of care varies widely across the country, suggesting that cost savings due to EHR implementation might be substantially higher in some areas than others. The Dartmouth Atlas has reported an inflation-adjusted total Medicare spending per enrollee in 2006 ranging from a low of $5311 in the Honolulu, Hawaii hospital referral region to a high of $16 351 in the Miami, Florida region.7
With HITECH, the demand for evidence of system effectiveness is growing. Although there are studies showing a reduction in medication errors,8–11 there are also reports of increased mortality12 and the introduction of new types of medication errors.13 Additionally, there are questions regarding real return on investment from the upfront purchase and implementation costs. The Congressional Budget Office has suggested that the assumptions used by CITL and RAND to project cost savings may be overly optimistic.14 Himmelstein et al15 found that hospital computing might improve quality, but overall it does not reduce cost; indeed, the ‘most wired’ hospitals did no better on quality or cost. They conclude that ‘no reliable data support claims of cost savings or dramatic quality improvement’ from hospital computerization.15
We sought to shed light on these controversies by comparing data of selected cost of care and safety metrics pre- and postimplementation of a commercially available inpatient EHR with CPOE.
Methods
Gundersen Lutheran Medical Center is a community-based tertiary referral center and teaching hospital located in La Crosse, Wisconsin. The hospital has 325 licensed beds and is a Level II trauma center. An inpatient EHR (Epic, Verona, Wisconsin; version Spring 2008 IU3) was implemented at our institution on November 1, 2008. On February 4, 2009, the CPOE function was added.
Following Institutional Review Board approval of our application for a Health Insurance Portability and Accountability Act waiver for this retrospective, longitudinal study, data were collected for the period 1 year before EHR (pre-EHR) and 1 year after EHR (post-EHR) implementation. Measures of cost of care, safety, and quality for which data were readily available pre-EHR and post-EHR were selected and captured for all hospitalized patients. The emergency department was excluded. No other institution-wide initiatives that could reasonably be expected to have affected the data were initiated during the study periods.
Length of stay, readmission within 30 days, case mix index, and risk-adjusted mortality were used as surrogate markers of quality. Laboratory tests and radiology examinations completed, transcription costs, and paper consumption were selected as measures of cost of care. Medication events were studied as a measure of safety.
Descriptive statistics—including means, standard deviations, and frequencies—were calculated per month unless noted as weekly as in the case of laboratory tests per week per patient. Statistical analysis consisted of t tests for continuous variables and χ2 tests for nominal data. All analyses were completed using SAS statistical software, version 9.2. All comparisons were two-tailed and used α level of 0.05 to be considered significant. For further detail regarding the Methods, including a description of aspects contributing to implementation success, see online appendix 1.
Observations
General characteristics and quality surrogates
No significant difference was found between the pre- and post-EHR periods regarding number of hospitalizations, patient days per month, length of stay, readmission within 30 days, or case mix index (table 1). Likewise, risk-adjusted mortality was similar between study periods.
Table 1.
General characteristics and surrogate markers of quality in the year before electronic health record (EHR) implementation versus the year after EHR implementation*
| Characteristics | Pre-EHR | Post-EHR | Percentage change | p Value |
| No of hospitalizations per month | 1325 (73) | 1299 (78) | −2.0 | 0.40 |
| No of patient days per month | 4985 (309) | 4883 (329) | −2.0 | 0.44 |
| Length of stay, days | 3.8 (0.2) | 3.8 (0.2) | 0.0 | 0.76 |
| Case mix index | 1.48 (0.06) | 1.44 (0.04) | −2.7 | 0.12 |
| Percentage readmission within 30 days | 7.71 (1149/14 904) | 8.15 (1190/14 607) | 0.44† | 0.98 |
Data are presented as mean (SD) unless otherwise indicated.
Absolute difference.
Laboratory tests and radiology examinations
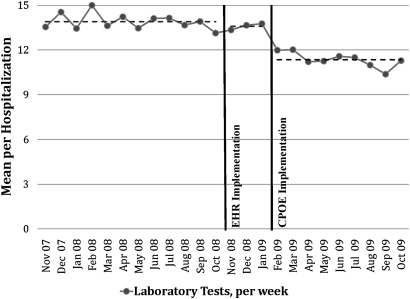
The number of laboratory tests per week per hospitalization declined from 13.9 pre-EHR to 11.4 in the 9 months after CPOE implementation, a decrease of 18.0% (p<0.001). There was no significant difference in the number of laboratory tests per week per hospitalization between the pre-EHR period and the first 3 months post-EHR period, that is, before CPOE was in use (figure 1).
Figure 1.
Mean number of laboratory tests per week per hospitalization in the year before electronic health record (EHR) implementation, the first 3 months after EHR implementation without computerized provider order entry (CPOE), and the 9 months after CPOE implementation.
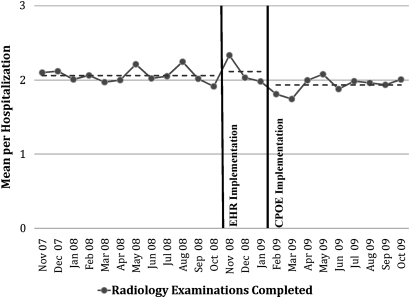
The number of radiology examinations completed per hospitalization was similar between the pre-EHR period and the first 3 months post-EHR, before CPOE was in use (figure 2); however, the number decreased from 2.06 in the pre-EHR period to 1.93 in the 9 months after CPOE implementation (6.3%; p=0.009). There was no significant difference in the number of radiology examinations canceled per hospitalization in the pre-EHR period and the first 3 months post-EHR, when CPOE was not in use, but the number increased 28.6%—from 0.28 to 0.36—after CPOE implementation (p<0.001). Reasons for cancellation were quantified, and the number canceled due to duplicate orders—that is, when a radiology staff member manually canceled an order because it was clearly a duplicate—increased significantly (p=0.008).
Figure 2.
Mean number of radiology examinations completed per hospitalization in the year before health record (EHR) implementation, the first 3 months after EHR implementation without computerized provider order entry (CPOE), and the 9 months after CPOE implementation.
Transcription costs
Using a strategy including partial dictation, monthly transcription costs decreased from $74 596 to $18 938, a decline of 74.6% (p<0.001). Savings in the year post-EHR totaled $667 896. The transcription system did not differentiate between transcription minutes used for full dictation versus transcription minutes used for partial dictation.
Paper consumption
Reams of copy paper ordered each month decreased 26.6%, from 1668 to 1224 (p<0.001), an annual savings of $11 815. One hundred eighteen paper forms were eliminated after EHR implementation, a savings of $18 716 per year. The total paper savings (copy paper plus forms) in the year after EHR implementation was 5.2 million sheets, for a total paper cost savings of $30 531.
Medication errors and near misses
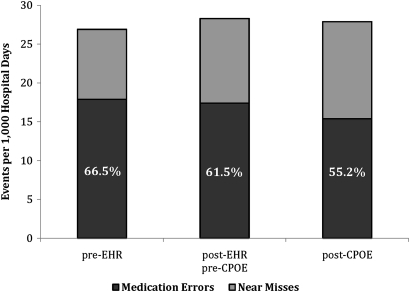
Medication errors per 1000 hospital days decreased 14.0%—from 17.9 in the pre-EHR period to 15.4 in the 9 months after CPOE implementation (p<0.030). Again, there was no significant difference in the rate of medication errors between the pre-EHR period and the post-EHR, but pre-CPOE, period. Near misses per 1000 hospital days increased from 9.0 in the pre-EHR period to 12.5 in the post-CPOE period (38.9%; p<0.037), and the percentage of medication errors to medication events defined as medication errors plus near misses decreased from 66.5% in the pre-EHR period to 55.2% in the post-CPOE period (p<0.007) (figure 3). Medication events per 1000 hospital days did not change significantly in these same periods (p=0.632).
Figure 3.
Medication events per 1000 hospital days and percentage of medication errors compared with near misses in the year before electronic health record (EHR) implementation, the first 3 months after EHR implementation without computerized provider order entry (CPOE), and the 9 months after CPOE implementation.
Discussion
Implementation of a commercially available inpatient EHR with CPOE appears to have quickly reduced cost of care and improved safety in our hospital. Although less commonly reported, others have found immediate benefit after implementation of CPOE. One site reported a quicker turnaround time in pharmacy, laboratory, and radiology orders.16 We have demonstrated a substantial decrease in laboratory and radiology utilization. According to the Dartmouth Atlas, our La Crosse, Wisconsin, referral region was fourth lowest in the nation in inflation-adjusted total Medicare spending per enrollee, with reported spending in 2006 of $5812, suggesting that our region's systems were very efficient, even before implementation of EHR.7 If cost of care can be reduced even in a highly efficient integrated healthcare delivery system such as ours, other less efficient systems may experience even greater reductions.
Our study demonstrated an 18% reduction in laboratory testing. Another study, one of a system without full CPOE, found that while an electronic alert of apparently redundant selected laboratory tests resulted in significantly fewer tests being ordered, the cost savings were far less than anticipated.17 In another study, Tierney et al18 found that computer entry of inpatient orders was associated with reduced bed charges, diagnostic test charges, and drug charges. This system was set up to display the patient's charge for each item, the most cost-effective tests for common problems, and only reasonable testing intervals. Others have found that the computerized display of charges for laboratory and radiology tests at the time of ordering did not significantly change the number of tests ordered.19
We are the first to report an association of inpatient electronic documentation with an option for partial dictation with a decrease in transcription costs. Others have reported a decrease in transcription of 61.5% to 88.2%, depending on note type, following a voluntary change to direct entry of documentation into the EHR by ob-gyn providers,20 but partial dictation was not used in that study. Our study found a reduction in transcription costs across our entire inpatient environment, not only in a single specialty.
Likewise, our inpatient EHR implementation was associated with a decrease in paper consumption. Because we used paper orders as a surrogate marker of paper consumption, it is possible that these variables did not correspond precisely. Although the dollar amount saved was small, the environmental impact, especially if projected over many organizations and over time, is substantial. To our knowledge, this metric has not been previously reported.
We found an increase in the percentage of near misses and concomitant reduction in the percentage of medication errors after inpatient EHR implementation. Our increase in near misses may demonstrate that EHR implementation introduced additional safety checks to identify potential errors that would not have been recognized without use of the EHR. Therefore, we agree with others that the number of near misses can increase, as ours did, to the benefit of the patient, and that the increase may represent refinement of error-prevention systems.8 Interestingly, Bates et al8 found a non-significant decrease in the number of ‘intercepted potential adverse drug events’ (ie, near misses) after CPOE was introduced, along with an overall decrease in medication errors. They showed no change in percentage of non-intercepted serious medication errors to intercepted potential adverse drug events. Two other studies observed an increase in this percentage, although the statistical significance was not reported.9 11
Among the strengths of this study is our inclusion of the entire hospital for metrics rather than certain units (eg, Intensive Care)11 or certain specialties (eg, ob-gyn),20 or with selected laboratory tests.17 We also report measures and findings not previously reported in the literature. In addition, we demonstrated that benefits of EHR and CPOE are attainable soon after implementation, as opposed to after system stabilization and refinement.
The single-center nature of the observations and the fact that our implementation experience may not be able to be generalized to other organizations are weaknesses of our study. Organizations of different sizes, specialty mixes, or number of residents may experience different results. In addition, the retrospective design creates bias, as other unknown variables may account for the results. Finally, in an integrated project, overall costs are difficult to determine, and this limits the impact of our study. For further detail regarding this Discussion, please see online appendix 2.
Implementation of an inpatient EHR with CPOE can result in rapid improvement in measures of cost of care and safety, even in an already highly efficient healthcare delivery system. Properly implemented systems have the potential to decrease the cost of care and to improve the safety of our nation's healthcare system.
Supplementary Material
Acknowledgments
The authors gratefully acknowledge the support of Gundersen Lutheran Medical Foundation, which provided the services of a biostatistician (MAM) for data analysis and a medical editor (CM Fischer) for manuscript editing.
Footnotes
Funding: Gundersen Lutheran Medical Foundation, La Crosse, Wisconsin.
Competing interests: None.
Ethics approval: Ethics approval was provided by the Gundersen Clinic Human Subjects Committee IRB.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Centers for Medicare and Medicaid Services Medicare and Medicaid Programs; Electronic Health Record Incentive Program; Proposed Rule. http://www.cms.gov/Recovery/Downloads/CMS-2009-0117-0002.pdf (accessed 28 Apr 2010).
- 2.Kohn LT, Corrigan JM, Donaldson MS. To Err is Human: Building a safer Health System. Washington, D.C: Institute of Medicine, National Academy Press, 1999 [PubMed] [Google Scholar]
- 3.Milstein A, Galvin RS, Delbanco SF, et al. Improving the safety of health care: the leapfrog initiative. Eff Clin Pract 2000;3:313–16 [PubMed] [Google Scholar]
- 4.Walker J, Pan E, Johnston D, et al. The Value of Health Care Information Exchange and Interoperability. Health Aff, Millwood, 2005. http://content.healthaffairs.org/cgi/content/full/hlthaff.w5.10/DC1 (accessed 29 Jun 2010). [DOI] [PubMed] [Google Scholar]
- 5.Girosi F, Meili R, Scoville RP. Extrapolating Evidence of Health Information Technology Savings and Costs. Santa Monica, CA: RAND Health, 2005:94 http://www.rand.org/pubs/monographs/2005/RAND_MG410.pdf (accessed 29 Jun 2010). [Google Scholar]
- 6.Yu FB, Menachemi N, Berner ES, et al. Full implementation of computerized physician order entry and medication-related quality outcomes: A study of 3364 hospitals. Am J Med Qual 2009;24:278–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fisher ES, Bynum J, Skinner J. The Policy Implications of Variations in Medicare Spending Growth. http://www.dartmouthatlas.org/downloads/reports/Policy_Implications_Brief_022709.pdf (accessed 27 Apr 2010). [PubMed]
- 8.Bates DW, Leape LL, Cullen DJ, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors. JAMA 1998;280:1311–16 [DOI] [PubMed] [Google Scholar]
- 9.Bates DW, Teich JM, Lee J, et al. The impact of computerized physician order entry on medication error prevention. J Am Med Inform Assoc 1999;6:313–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Doormaal JE, van den Bemt PM, Zaal RJ, et al. The influence that electronic prescribing has on medication errors and preventable adverse drug events: An interrupted time-series study. J Am Med Inform Assoc 2009;16:816–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shulman R, Singer M, Goldstone J, et al. Medication errors: A prospective cohort study of hand-written and computerised physician order entry in the intensive care unit. Crit Care 2005;9:R516–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Han YY, Carcillo JA, Venkataraman ST, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 2005;116:1506–12 [DOI] [PubMed] [Google Scholar]
- 13.Koppel R, Metlay JP, Cohen A, et al. Role of computerized physician order entry systems in facilitating medication errors. JAMA 2005;293:1197–203 [DOI] [PubMed] [Google Scholar]
- 14.Congressional Budget Office Evidence on the Costs and Benefits of Health Information Technology, 2008. Pub No 2976. http://www.cbo.gov/ftpdocs/91xx/doc9168/05-20-HealthIT.pdf (accessed 29 Jun 2010).
- 15.Himmelstein DU, Wright A, Woolhandler S. Hospital computing and the costs and quality of care: A national study. Am J Med 2010;123:40–6 [DOI] [PubMed] [Google Scholar]
- 16.Mekhjian HS, Kumar RR, Kuehn L, et al. Immediate benefits realized following implementation of physician order entry at an academic medical center. J Am Med Inform Assoc 2002;9:529–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bates DW, Kuperman GJ, Rittenberg E, et al. A randomized trial of a computer-based intervention to reduce utilization of redundant laboratory tests. Am J Med 1999;106:144–50 [DOI] [PubMed] [Google Scholar]
- 18.Tierney WM, Miller ME, Overhage JM, et al. Physician inpatient order writing on microcomputer workstations. Effects on resource utilization. JAMA 1993;269:379–83 [PubMed] [Google Scholar]
- 19.Bates DW, Kuperman GJ, Jha A, et al. Does the computerized display of charges affect inpatient ancillary test utilization? Arch Intern Med 1997;157:2501–8 [PubMed] [Google Scholar]
- 20.Lagrew DC, Jr, Stutman HR, Sicaeros L. Voluntary physician adoption of an inpatient electronic medical record by obstetrician-gynecologists. Am J Obstet Gynecol 2008;198:690.e1–5; discussion 690.e5–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.