Abstract
WHO reports estimate poisoning as one of the most common causes of increased morbidity and mortality rate world-wide. Various agents such as pesticides, drugs have been used for intentional and accidental poisoning in different countries. In the Indian scenario, pesticides are the most commonly used poisoning agents. To assess the prevalence and mortality incidence rate due to various poisoning agents a retrospective and prospective study conducted over a period of nine months in a tertiary care teaching hospital. Retrospective data of poisoning cases was collected from the medical records section and the prospective data of poisoning cases was collected from the emergency and causality departments. A total of 1045 poisoning related admissions were identified during the period January 2005 to September 2008. Among them, 68.40% of cases were due to intentional poisoning and 31.60% were due to accidental poisoning. Of the poisoning related admissions, 84.4% of patients recovered, whereas in 7.6% of cases condition did not improve. Mortality rate was observed 4%. Intentional poisoning was observed more in male population (60.2%) in the age group of 18-29 years. Accidental poisoning was seen more in children in the age group of 1-3 years. Incidence of overall poisoning cases were high due to pesticides (39.5%) followed by medicines (26.1%), household products (22.1%), environmental poisoning (12.1%) and heavy metals (0.2%). It was observed that availability of centralised poison information centre and treatment protocols will improvise poison management practices in tertiary care hospitals by the clinicians.
Keywords: Drugs, incidence, house hold products, pesticide, poisoning agent, prevalence
Poison is a substance that causes damage or injury to the body and endangers one's life due to its exposure by means of ingestion, inhalation, or contact[1]. Worldwide various agents such as agrochemicals, drugs or environmental agents are used as poisoning agents[2]. Worldwide intentional poisoning is one of the important causes for mortality and morbidity[3]. Exposure to agrochemicals, medicines and environmental agents are the major causes of poisoning. Distress due to loss in the business, failure in romance or differences with the intimate partner, or examination, emotional disturbances and chronic diseases are the common reasons for intentional poisoning[4].
World Health Organization (WHO) estimated 0.3 million people die every year due to various poisoning agents[5]. Acute pesticide poisoning is one of the most common causes of intentional deaths worldwide[6]. High doses of analgesics, tranquillizers, and antidepressants are the commonly used agents for intentional poisoning in industrialized countries[7] and agriculture pesticides are used in Asian region for self poisoning particularly in rural areas with a fatality range of 10-20%[8]. Majority of pesticide exposure is seen more in middle and low income countries due to increased use of agrochemicals in agricultural sector[9].
Studies have revealed that pesticides are the commonly used poisoning agents for intentional poisoning in India[10]. As agriculture is major profession in the rural part of India farmers stock the pesticides to eradicate the weeds and pests. Due to easy availability of the pesticides, they are commonly used by the individuals to end their life in stressful situations[11].
Mysore is a South Indian district where agriculture is the major occupation in rural Mysore. JSS Medical college hospital is a 1000 bed tertiary care, multi speciality teaching hospital catering to the health requirements of urban and rural population. Many rural patients get admitted to emergency department of JSS Medical College hospital due to poisoning. Department of Clinical Pharmacy frequently receives queries from emergency department pertaining to the antidotes for treating various poisoning agents. The present study was initiated to analyse the incidence and mortality rate of the poisoning cases admitted to the hospital to develop treatment protocols.
MATERIALS AND METHODS
The present study was a retrospective and prospective study conducted over a period of nine months. Case records of poisoning cases from January 2005 till January 2008 were reviewed retrospectively and prospectively from January 2008 to September 2009. A specially designed data collection form was used to collect the details of patients’ demography, type of poisoning agents consumed, method of poisoning (oral, inhalation, dermal or eye exposure), name of the poison consumed, quantity consumed, route of exposure, first aid rendered, signs and symptoms, investigations done, treatment given, specific antidote given, complications developed, treatment outcomes and events of mortality and the reasons for the mortality. The study was approved by the institutional ethics committee.
RESULTS AND DISCUSSION
During the study period, 1045 poisoning cases were reviewed retrospectively and prospectively. Among them, intentional poisoning cases were 68.42% and 31.58% cases were due to accidental poisoning (fig. 1). Commonly used agents for poisoning were pesticides (39.5%) followed by medicines (26.1%) (fig. 2). Oral route was the most common route of exposure to poison followed by inhalation and dermal route.
Fig. 1.
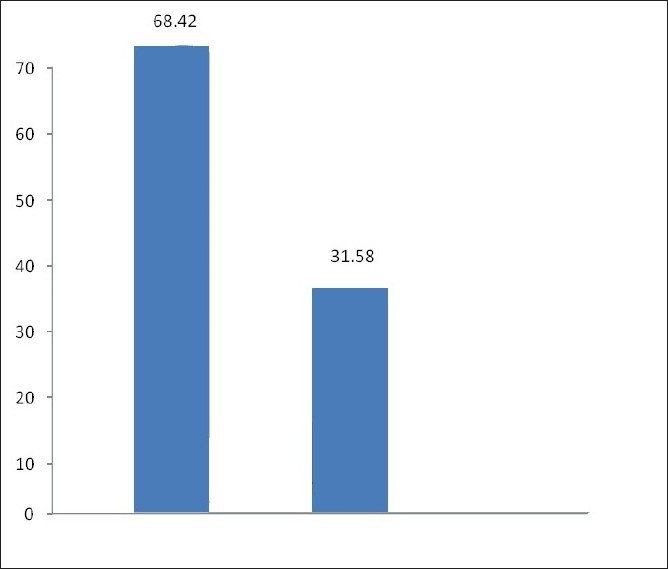
Incidences of intentional and accidental poisoning 68.42%: Intentional poisoning (715 cases); 31.58%: Accidental poisoning (330 cases)
Fig. 2.
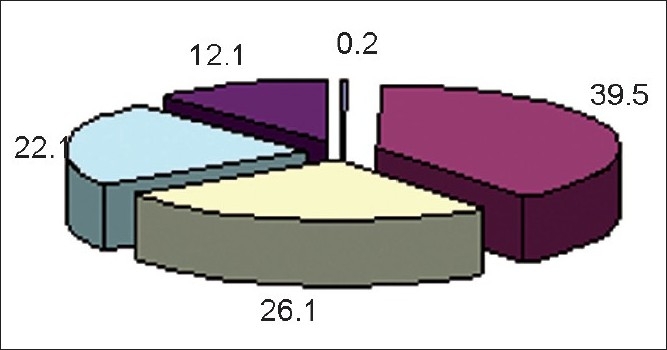
Agents commonly used for poisoning. Pesticides: 39.5%, Medicines: 26.1%, House hold products: 22.1%, Environmental: 12.1%, Heavy metals: 0.2%
Majority of the poisoning incidences were seen in age group between 18-29 years (fig. 3). Amongst the intentional poisoning cases, adult males (60.2%) predominated over adult females (39.8%) and in adolescence group majority were seen in females (71.4%) when compared to males (28.6%). It was also observed that the incidence of poisoning was decreased with the increasing age. Among the accidental poisoning, majority of the incidences were seen in adult males (42.3%) followed by male children (21.3%). In children, majority poisoning cases were seen in boys (64.9%) compared to the girls (35.1%). Accidental poisoning cases were seen more due to house hold products (64.6%), followed by pesticides (22.9%) and medicines (12.5%).
Fig. 3.
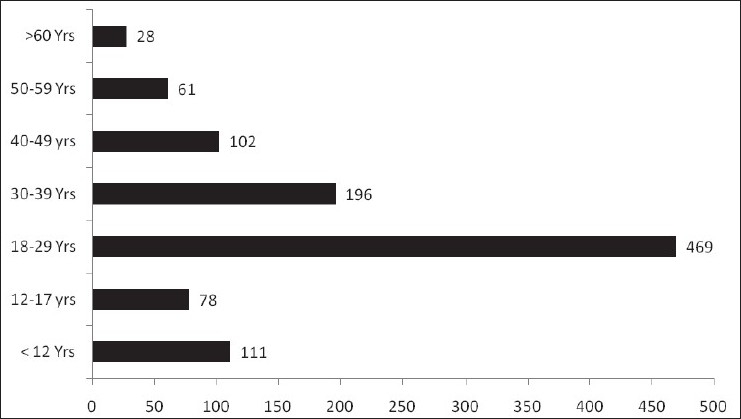
Age distribution of total poisoning cases Total number of cases: 1045, X axis= Age distribution, Y axis = Number of poisoning cases
From the results it was also observed that majority poisoning cases were seen during the summer season (28.1%) followed by the winter season (26%). The frequency of poisoning cases in different seasons is presented in fig. 4.
Fig. 4.
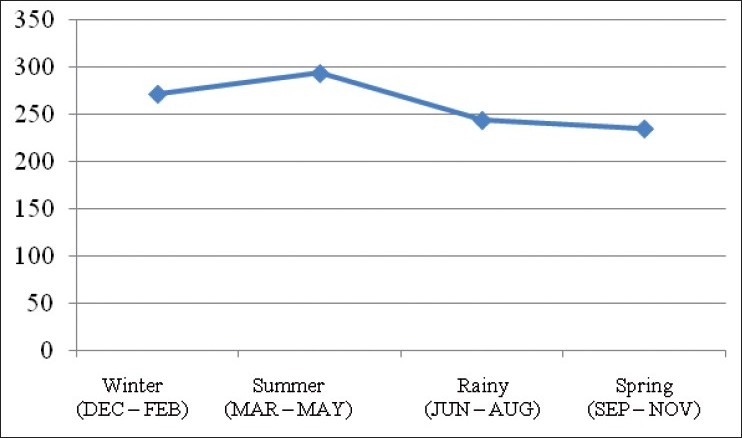
Season wise distribution of poisoning cases Total cases: 1045, Winter: 275 cases, Summer: 295 cases, Rainy: 240 cases, Spring: 235 cases
Among the pesticides, organophosphates (71%) followed by rat poisoning (zinc phosphide and aluminium phosphide, 13%), pyrethroids (7%), carbamates (6.5%), and organochlorine (2.5%) were the agents used for intentional poisoning. Benzodiazepines (33.33%), followed by analgesics (7.89%), antidepressants (6.14%), barbiturates (5.70%) were the commonly used medications for poisoning. Multiple drug poisoning was observed in 17.98% cases and unknown drug was observed in 12.28 % of cases. Medicines like anticonvulsants (2.19%), antihistamines (3.07%), antidiabetic (2.19%), alcohol (3.94%), iron (1.75%), and folic acid (0.87%) and zinc tablets (0.43%), antithyroid (1.37%), anti asthmatics (0.87%) were used rarely for intentional poisoning. There were 82% of single drug induced poisoning cases and 18% of multiple drug poisoning cases reported.
House hold products related poisoning was observed in children and most commonly used agents were hydrocarbons (68.35%) followed be phenyl (16.4%), naphthalene, (3.69) castor seed, caustic soda, acetone and hair dye, bleaching powder (1.03%), and 5.06 % cases were seen due to unknown liquid. There were two cases of heavy metals induced poisoning. One was due to arsenic and other one was due to copper. Environmental poisoning was seen more due to snake bite, followed by stings (bee, scorpion) and insect bite (fig. 5).
Fig. 5.
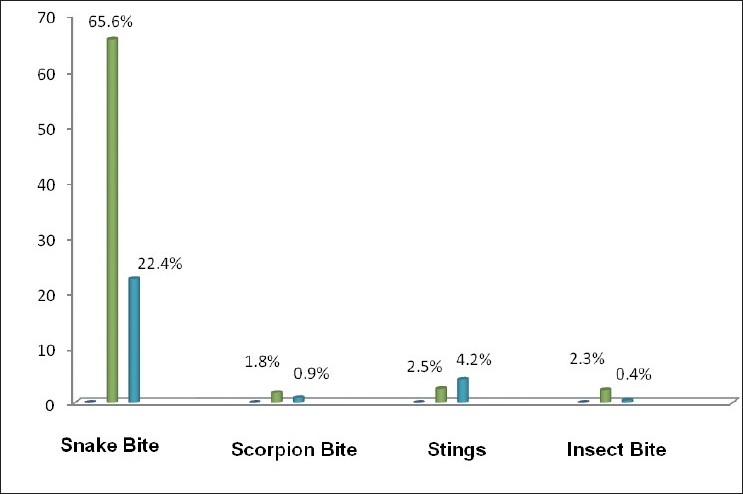
Percentage wise distribution of environmental poisoning cases Snake bite: 193 cases (Male= 144, Female= 49), Scorpian bite: 6 cases (Male= 4, Female= 02), Stings: 15 cases (Male= 6, Female= 9), Insect bite: 06 Cases (Male= 05, Female=01)
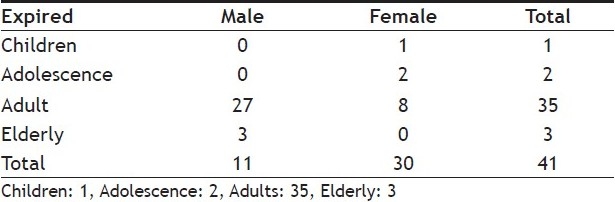
Among the poisoning related admissions 84.4% of patients recovered, whereas in 7.6% of cases condition was not improved, mortality rate was found in 4%. The details are shown in Table 1. Majority of deaths were seen in adults and only few deaths were reported in children. Results of the same are presented in Table 2.
TABLE 1.
TREATMENT OUTCOME OF THE POISONING CASES
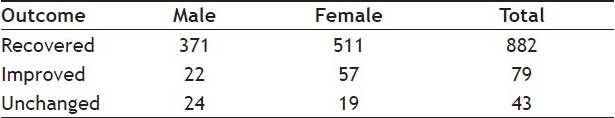
TABLE 2.
INCIDENCE OF MORTALITY
Various national and international studies have projected the raise of incidence of intentional poisoning cases[11–13]. During the study period a total of 1045 cases were collected with an average of 20-30 cases per month. The results of the study report that the incidence of poisoning was seen more in adults than children. Most commonly used route for poisoning exposure was oral followed by inhalation and dermal exposure. Intentional poisoning was seen more in adult male group because they are more often exposed to the stress and strain in their profession in work places and in day to day life. Most of the poisoning was seen in younger adult age group i.e. 18-29 years. The possible reasons for increased poisoning in this age group may be because of problems in family, studies, marriage, life settlement and employment which may themselves stressed and this may make them to attempt to suicide. In adolescence age, majority poisoning cases were seen in girls than boys due to stress factors like family arguments, love failures, failure in studies and mental conflicts[7].
Several studies have reported that pesticides were the most commonly used agents for poisoning in Asia Pacific Regions. Even our study findings also shows that pesticides contributed for the maximum poisoning cases and associated with high mortality rate followed by drugs 21.8% and household products 7.6%[10–12]. India is a county, where agriculture is the prime profession for majority of people in rural areas and pest control is one of the most common problems faced by the farmers in agriculture. In order to eradicate the weeds and pests farmers procure and keep pesticides at their houses. Because of easy availability of the pesticides people are tend to use them for intentional poisoning. Apart from pesticide poisoning, the other common types of poisons used were medicines like benzodiazepines, analgesics, anti depressants and barbiturates. Medicines are used as poisoning agents for intentional poisoning in developed countries[7] and urban areas of India. In certain places, street drugs and OTC medicines like paracetamol, antihistamines are also used for intentional poisoning[15,16].
House hold products induced poisoning was seen more in children of age less than 5 years. Most commonly used agents are hydrocarbons, phenyl, and other corrosive agents. Accidental poisoning in children is more seen in males, because children at this age become more curious in their newly acquired hand skills and mobility due to their exploratory, active and restless behaviours than the female children. Negligence or unawareness from the parents and caretakers is one of the main factors in making the environment of the child favourable for poisoning. Majority of poisoning takes place in small houses because of lack of space where chemical or disinfectants or other house hold products will be kept which would be in easy reach of children, which is considered as another reason for accidental poisoning in children.
Environmental poisoning was also found as a significant cause in poisoning admissions to the hospital. Reptile bite is one of the major environmental poisoning occurring in rural areas than the urban area. The present study reports environmental poisoning was seen more in adult males followed by females and this was due to snake bite, followed by bee Stings, insect and scorpion bite.
Poisoning incidence also varies according to the seasons. Incidence was seen more in summer season followed by the winter season. Incidences of poisoning during summer months, are more because as the summer days being longer and during which the person becomes easily fatigued and exhausted as a result of extreme heat conditions leading to mental imbalance. Other reason may be the preservation of grains during summer is more and in order protect them pesticides are procured and preserved[9]. Due to the easy accessibility to pesticides, people may try to consume the pesticides to end their life when they suffer from economic burdens or any emotional conflicts.
The reasons observed for the mortality in poisoned individuals were the delay in admission to hospital, improper management of the poisoned patient, lack of information regarding the poison agent and its antidote. To reduce the poison induced morbidity and mortality following steps such as having a centralised poison information centre, availability of standard treatment protocols for managing various poisons, and educational programs for rural people may be more appropriate.
Incidences of intentional poisoning are rising day by day due to social, emotional and professional stress. Most commonly used agents for intentional poisoning are pesticides or medicines by the people. The findings of the study conclude that intentional poisoning was more in male adults and in female adolescent group. The mortality and morbidity due to poisoning can be reduced by conducting educational programs in rural areas and providing counselling services and poison information services to the needy people.
Acknowledgments
Authors thank JSS University, Dr. H. G. Shivakumar, Principal, JSS College of Pharmacy, Dr. G. Parathasarathi, Head, Department of Pharmacy Practise, Dr. K. Veerabhadrappa, Medical Superindent, Dr. M. D. Ravi, Professor, Department of Paediatrics, Dr. M. G. Narahari, Associate Professor, JSS Medical College Hospital, Dr. H. Basvanna Gowdappa, Principal, JSS Medical College for their support during the research work.
Footnotes
Jesslin, et al.: Assessment of Prevalence and Mortality Incidences Due to Poisoning
REFERENCES
- 1.Thomas WF, John HD, Willium RH. Stedman's Medical Dictonery. 28th ed. New York: Lippincott William and Wilkins; 2007. p. 2004. [Google Scholar]
- 2.Hempestead K. Manner of death and circumstances in fatal poisoning: Evidence from New Jersey. Inj Prev. 2006;12:44. doi: 10.1136/ip.2006.012583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eddleston M, Phillips MR. Self poisoning with pesticides. BMJ. 2004;328:42–4. doi: 10.1136/bmj.328.7430.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chowdhary AN, Banerjee S, Brahma A, Biswas MK. Pesticide poisoning in nonfatal, deliberate self-harm: A public health issue. Indian J Psychiatry. 2007;49:117–20. doi: 10.4103/0019-5545.33259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thundiyil JG, Stober J, Besbelli N, Pronczuk J. Acute pesticide poisoning: a proposed classification tool. Bull World Health Organ. 2008;86:205–9. doi: 10.2471/BLT.08.041814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Konradsen F, Dawson AH, Eddleston M, Gunnell D. Pesticide self-poisoning: thinking outside the box. Lancet. 2007;369:169–70. doi: 10.1016/S0140-6736(07)60085-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McClure GM. Suicide in children and adolescents in England and Wales 1970-1998. Br J Psychiatry. 2001;178:469–74. doi: 10.1192/bjp.178.5.469. [DOI] [PubMed] [Google Scholar]
- 8.Marecek J. Culture, gender, and suicidal behavior in Sri Lanka. Suicide Life Threat Behav. 1998;28:69–81. [PubMed] [Google Scholar]
- 9.Dash SK, Raju AS, Mohanty MK. Sociodemographic Profile of Poisoning Cases. J Indian Acad Foreni Sci. 2005;27:133–8. [Google Scholar]
- 10.Srinivas Rao Ch, Venkateswarlu V, Surender T, Eddleston M, Buckley NA. Pesticide poisoning in south India: opportunities for prevention and improved medical management. Trop Med Int Health. 2005;10:581–8. doi: 10.1111/j.1365-3156.2005.01412.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aaron R, Joseph A, Abraham S, Muliyil J, George K, Prasad J, et al. Suicides in young people in rural southern India. Lancet. 2004;363:1117–8. doi: 10.1016/S0140-6736(04)15896-0. [DOI] [PubMed] [Google Scholar]
- 12.Roberts DM, Karunarathna A, Buckley NA, Manuweera G, Sheriff MH, Eddleston M. Influence of pesticide regulation on acute poisoning deaths in Sri Lanka. Bull World Health Organ. 2003;81:789–98. [PMC free article] [PubMed] [Google Scholar]
- 13.Gunnell J, Eddleston M. Suicide by intentional ingestion of pesticides: a continuing tragedy in developing countries. Int J Epidemiol. 2003;32:902–9. doi: 10.1093/ije/dyg307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh S, Singhi S, Sood NK, Kumar L, Walia BN. Changing pattern of childhood poisoning (1970-1989): experience of a large north Indian hospital. Indian Pediatr. 1995;32:331–5. [PubMed] [Google Scholar]
- 15.Goto K, Endoh Y, Kuroki Y, Yoshioka T. Poisoning in children in Japan. Indian J Pediatr. 1997;64:461–8. doi: 10.1007/BF02737750. [DOI] [PubMed] [Google Scholar]
- 16.Yang CC, Wu JF, Ong HC, Kuo YP, Deng JF, Ger J. Children Poisoning in Taiwan. Indian J Paediatr. 1997;64:469–83. doi: 10.1007/BF02737751. [DOI] [PubMed] [Google Scholar]


