Abstract
Medical education is at a crossroads. Although unique features exist at the undergraduate, graduate, and continuing education levels, shared aspects of all three levels are especially revealing, and form the basis for informed decision-making about the future of medical education.
This paper describes some of the internal and external challenges confronting undergraduate medical education. Key internal challenges include the focus on disease to the relative exclusion of behavior, inpatient versus outpatient education, and implications of a faculty whose research is highly focused at the molecular or submolecular level. External factors include the exponential growth in knowledge, associated technologic (“disruptive”) innovations, and societal changes. Addressing these challenges requires decisive institutional leadership with an eye to 2020 and beyond—the period in which current matriculants will begin their careers. This paper presents a spiral-model format for a curriculum of medical education, based on disease mechanisms, that addresses many of these challenges and incorporates sound educational principles.
In this centennial anniversary year of the Flexner report on medical education in North America, medical schools find themselves under escalating pressures for fundamental change. How should they view and revise their educational mission? A number of authoritative recommendations have emerged from organizations such as the Association of American Medical Colleges, the Howard Hughes Medical Institute, the Carnegie Foundation, and, most recently, the Lancet Commissions (1–4). Although considerable overlap exists among these reports, so do differences, depending on the mission and perspective of each agency. The goal of this paper is not to return to these well-furrowed fields but rather to present a personal view on some of the challenges ahead. Medical schools are now in the midst of curricula redesign that will affect students who will graduate, complete residency training, and become practicing professionals in 2020 and beyond. This paper will provide a brief overview of some of the educational challenges for medical schools and the pros and cons of various curricular models, and will propose a new scheme for curricular organization.
Although increasingly forceful calls have emerged for the reform of medical education, Ludmerer was the first to systematically call attention to the growing threat to the entire mission of medical education (5). In his 2002 address to the ACCA, entitled “The Internal Challenges to Medical Education,” he identified growing disconnections in the delivery of medical education (6). Eight years later these disconnections remain largely unaddressed and are more acute than ever, as illustrated here:
In his 2007 Shattuck Lecture, Schroeder pointed out that ∼80% of medical education is focused on biology, yet 60% of premature deaths are due to “non-biologic” factors (7). Although these non-biologic factors ultimately act through biologic mechanisms, their genesis lies elsewhere—largely in behavioral choices.
Approximately 80% of clinical education occurs in inpatient settings, yet 80–90% of medicine is practiced in the outpatient arena. The least experienced learners begin their in-depth clinical exposure in the most complicated, fastest paced, environments of health-care delivery. In these arenas, novice students are increasingly displaced by more advanced learners whose performance must be increasingly supervised and documented in a setting increasingly geared for rapid patient discharge.
The sub-cellular/molecular focus of much of scientific inquiry presents a growing challenge to academic faculties in basic science as the highly focused areas of their research become further removed from direct application to clinical medicine.
In addition to these internal disconnections are a growing number of external challenges, including those listed in Table 1. Both types of problem must be addressed. Yet as complex as the internal disconnections may be, many if not all can be readily addressed by:
Decisive collegiate leadership committed to improved alignment of the educational mission with the resources intended to support it.
Greater central oversight for the curriculum.
Creation of an appropriate reward structure for education.
TABLE 1.
External Challenges Facing Medical Education
| Growth of Knowledge | Exponential increase |
| Need to define core concepts | |
| Societal issues | Health disparities |
| Disease prevention | |
| Aging population | |
| Maintaining functionality | |
| Chronic disease: How do we best teach and practice the management of multiple diseases in a single individual | |
| Expectations of other health-care stake holders | |
| Individual Issues | Continued specialization within medicine |
| Increased importance of lifestyle issues | |
| Implications for practice preferences and work force | |
| Technology | Human genome and personalized medicine |
| High-resolution functional imaging | |
| Implications for physical diagnosis | |
| Simulation science and quality improvement | |
| Information science | |
| Just-in-time learning | |
| Availability to patients, faculty, and students | |
| ;Leveling of the playing field of knowledge | |
| ;Potentially greater adeptness of students/patients than of faculty | |
| ;Need faculty development | |
| Health-care reform | Impact yet to be fully defined |
| Inter-professional education |
The external factors represent a more difficult challenge, precisely because they are external (i.e., beyond the control of individual institutions). They are less well defined and require the development of strategies that are sufficiently flexible to adapt to change. The rest of this paper will focus on the exponential increase in medical knowledge and existing curricular models, and present a different educational model with sufficient flexibility to address many of the challenges named above and in Table 1, both internal and external.
It is estimated that the doubling time of medical knowledge in 1950 was 50 years; in 1980, 7 years; and in 2010, 3.5 years. In 2020 it is projected to be 0.2 years—just 73 days. Students who began medical school in the autumn of 2010 will experience approximately three doublings in knowledge by the time they complete the minimum length of training (7 years) needed to practice medicine. Students who graduate in 2020 will experience four doublings in knowledge. What was learned in the first 3 years of medical school will be just 6% of what is known at the end of the decade from 2010 to 2020. Knowledge is expanding faster than our ability to assimilate and apply it effectively; and this is as true in education and patient care as it is in research. Clearly, simply adding more material and or time to the curriculum will not be an effective coping strategy—fundamental change has become an imperative.
Paradoxically, the expansion of knowledge will force medical schools to define those concepts that form the essential core of what students must learn. Because the practice of medicine inherently requires an intimate understanding of homeostasis, whether molecular or organismal, and because students' ability to apply knowledge to the solving of complicated clinical issues is promoted to a relatively greater extent by the integrated mastery of homeostatic mechanisms than by knowledge of these mechanisms' individual components (8, 9), identification of concepts underlying homeostasis should receive concentrated attention. Definition of these concepts should acknowledge that structure and function are the foundation of homeostasis—that all else relates either to homeostatic disruption or to interventions aimed at restoring homeostatic mechanisms.
The conceptual structure of the content to be learned has a major effect on learning. The size of this effect (ES) is large (ES = 0.57), especially as compared to that of clinical interventions considered to be effective (e.g., the use of daily aspirin to reduce the risk of myocardial infarction; ES = 0.04). Moreover, conceptual structure has its greatest value for students experiencing difficulty in relating concepts to one another (10, 11).
Beyond this, clinical expertise is linked to having well-organized knowledge. As students acquire knowledge, they organize it into schemes. In the typical “2+2” medical curriculum (2 years of basic science followed by 2 years of clinical rotations), students acquire information in each of a number of disciplines over the first 2 years. In contrast, as students travel from one clinical clerkship to the next, they encounter patients with specialty-specific complaints. The first of these realities imposes a discipline-based organizing scheme, whereas the second imparts a complaint-based scheme. In such curricula, it is largely left to the student to form the connections that integrate discipline-based knowledge with patient complaint/disease-focused information.
Three general schemes are currently used in US medical schools to organize curricula: (1) discipline-based; (2) organ-based; and (3) complaint-based. These schemes are compared and contrasted in Table 2. At Iowa, I have proposed a curriculum-organizing scheme based on mechanisms of disease (Table 3). This model is based on the premise that the body can respond to insult in only a finite number of ways. Advantages of such an approach are that: (1) it is organized into homeostatic units that group core organs or elements according to the primary role they play in the genesis of disease (some may be incorporated into more than one unit); (2) integrates basic and clinical knowledge in a contextual manner; and (3) utilizes a spiral format. A spiral curriculum is one that is deliberately designed to re-visit core material at periodic intervals. Each return-visit reviews and builds on previously introduced material and extends it in depth, breadth and application (12). The conscious definition of discrete homeostatic units, and the focus on mechanisms that disrupt and restore homeostasis, distinguish this curricular model from those that are organ system-based. Developing this approach within a spiral curricular format assures that the deliberate integration of identified core concepts, skills, and attitudes is reinforced at regular intervals and can be updated throughout a medical student's curricular experience. Such a curriculum clearly requires central oversight and has the additional benefit of encouraging collaborative development and teaching by basic science and clinical faculty. Small groups of selected and dedicated faculty (e.g., basic scientists, pathologists, generalists with a deep understanding of physiology) would be responsible for the longitudinal design, definition of concepts and general content, and sequencing of material within each homeostatic unit throughout the curriculum. Responsibility for conveying content (i.e., teaching) would largely remain with the faculty-at-large working in collaboration with the leadership team in each homeostatic unit.
TABLE 2.
Types of Medical Curricula in the United States
| Parameter | Organizing Schema |
||
|---|---|---|---|
| Discipline | Organ System | Complaint | |
| Management | Department with variable central oversight. | Some central management required. | Significant central management essential. |
| Administrative effort | Efficient, broad faculty engagement not required. Faculty members teach within their departmental offerings. | Efficient, but some degree of broader faculty engagement is necessary. Recruitment of teaching faculty can be a challenge. | Broad faculty engagement required for aspects of quality assurance related to large number of patient complaints. Designated teaching faculty track is common. |
| Contextual presentation of material | Information typically not presented in format in which it will be accessed. | Information is presented in a more contextual form. | Information presented contextually. |
| Reinforcement of presented material | Typically does not reinforce or update students' knowledge base in a deliberate or consistent manner. | Typically does not reinforce or update students' knowledge base in a deliberate or consistent manner. | May or may not deliberately reinforce integration of basic and clinical material. |
TABLE 3.
Proposed Model For Curricular Organization by Mechanisms of Disease
| Homeostatic Unit | Primary elements |
|---|---|
| Ischemia | Lung, cardiovascular system, erythrocytes, electron transfer, and ATP generation |
| Metabolism | Gastrointestinal tract, liver, kidney, endocrine organs, energy storage |
| Neoplasia | Genome and its variants, cell cycle |
| Inflammation | Immune system, infectious diseases, microbiology |
| Neuropsychiatric | Central and peripheral nervous system and special senses |
| Genetic | Genome, cell cycle, conception, gender differences. The “4Ps”: personalized, predictive, preventive, participatory |
| Trauma | Musculoskeletal system, skin |
| Socio-behavioral | Health-care disparities, socio-economic effects, health care systems, environment, behavior |
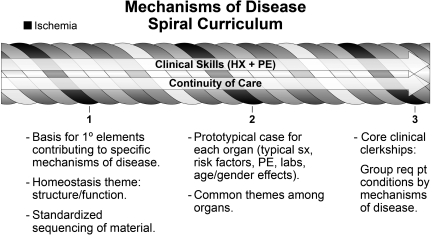
Figure 1 illustrates these concepts visually. Each of the homeostatic units is represented by one of the cables in the horizontal spiral shown in the figure. A standardized sequence would be defined for the presentation of material across all homeostatic units (e.g., molecular, cellular, organ, homeostasis, age/gender, clinical presentation, epidemiologic aspects). The optimal periodicity of the spiral would have to be determined empirically, the objective being to assure an optimal balance between the amount of material presented and the review and extension of previously introduced material in depth, breadth, and application. Recently, the importance of continuity in educational endeavors across the continuum of medical education, for learning and for assessment, has been re-emphasized (13). Continuity can be provided by educational threads that run longitudinally through the curriculum. Clinical skills and continuity-of-care clinics are examples of educational threads that run longitudinally throughout the proposed curricular model shown in Figure 1. For example, ischemia might be presented to students through a patient with angina pectoris of new onset. The elements contributing to this homeostatic unit would be introduced along with the basis for their inclusion as primary elements in the mechanisms of ischemia. Structure, function, sensing, and regulation would receive special emphasis in a progressive manner with each turn of the spiral. Each turn would be introduced by a patient with a disorder in one of the primary elements within the homeostatic unit, to illustrate how that element contributes to the relevant mechanism of disease (i.e., in this case ischemia). Concurrently, students would be introduced to relevant clinical skills and interact in a continuity-of-care clinic with a patient having the relevant disorder. Re-visiting material in this manner capitalizes on what is known about optimal learning, enhanced retention of knowledge, and application of knowledge. Later, after primary concepts have been introduced and mastered, students would be introduced to prototypical cases of ischemia in the remaining organ systems. The goal of this segment of the spiral would be to identify common themes: in the case of ischemia, these might include - supply versus demand, the importance of watershed areas, or markers of cell injury. Clinical skills would be expanded, and students would encounter representative but different patients in the continuity-of-care clinic.
Fig. 1.
Mechanisms of Disease Spiral Curriculum
Currently, the Liaison Committee on Medical Education (LCME) expects that the types of disorders students must encounter during each required clinical clerkship be specified. The continuation of a curricular model based on mechanisms of disease through the years of clinical training would build into this requirement the expectation that clerkships specify the mechanism(s) of disease exemplified by a given disorder. The organization of patient-based educational material would be expected to follow that introduced earlier in the curriculum (i.e., structure/function, homeostasis, age, gender, epidemiology, etc). As students progress from required to elective clerkships, responsibility for identifying the underlying mechanism(s) of disease would shift from the faculty to the student, and constitute a component of the student's performance evaluation.
The explicit linking of contextual material to a scheme for organizing knowledge based on a mechanisms-of-disease approach throughout the curriculum, and especially during clinical rotations, should not only enhance student learning and the mastery and application of knowledge, but can also be expected to provide the solid foundation of knowledge on which physicians rely when confronted with the most challenging and complicated cases of disease (11, 12).
In summary, advancing the mission of medical education requires decisive institutional leadership to address both internal and external challenges, not just today or tomorrow, but with a clear vision for the third decade of this century, in which our current students will begin their practice of medicine. Addressing external factors may represent a greater challenge precisely because they are external, are less well-defined, and require the development of strategies that are sufficiently flexible to adapt to changes in these factors that are beyond the direct control of any one institution. Herein, I have proposed a model of an educational curriculum based on mechanisms of disease. This model capitalizes on basic principles of learning, including the definition of core concepts, contextual presentation of material, and deliberate reinforcement and expansion of content over the 4-year medical-school curriculum. I submit that it simultaneously provides an appropriate balance between central responsibility for curricular oversight and distributed delivery of curricular content. This curriculum will require faculty development in a number of areas within and impinging on medical education, but also offers the potential for improved fulfillment of our educational mission and the opportunity to address internal challenges to that mission.
ACKNOWLEDGMENTS
The author is grateful to his colleagues on the Curriculum Renewal Steering Committee, and especially to Kristi Ferguson, Bill Radl, and Catherine Solow, for many productive discussions and editorial assistance.
Footnotes
Potential Conflicts of Interest: None disclosed.
DISCUSSION
Baum, New York: I just finished meeting with 183 students going from their third to their fourth year, and with writing 183 dean's letters, and there is a direct, invariable correlation between grades, being inducted into AOA, and being a dermatologist. If students don't want to be dermatologists, they want to be radiologists, orthopedists, ophthalmologists, or anesthesiologists. And so, while I agree with everything you said, I think that it's incredibly important internally for medical schools, and for a society of internists such as this is of equal if not of even greater importance to influence this trend, which I think will end by creating, or already has begun to create a society of physicians that really isn't going to meet the needs of people.
Densen, Iowa City: Thank you for the comment.
Collier, Newark: I would agree and would respectfully suggest that reimbursement mechanisms are driving people to dermatology and orthopedics, and that until we reform the way our physicians are reimbursed, we are going to continue to see this trend. In addition to the proliferation of medical knowledge, we see a real need for our students and residents to learn the principles that are surrounding patient care, of safety and quality, a team-based approach to care, communication during the transitions of care, and the principles of value-based care; and I think that as we look at the proliferation of medical knowledge, we really cannot lose sight of this.
Densen, Iowa City: Yes. I think those points are well-made. I wanted to share with you the concept of the mechanisms of disease in the spiral as the basis for curricular organization, but this does not preclude a needed emphasis on those elements upon which you touched.
Thibault, New York: I want to build on the last two questions. First of all, I want to congratulate you on this exceptional approach on how to organize information better and also use some new educational technologies. The challenges you stated at the beginning are obviously far bigger than organizational challenge, which is an important part of it; and building on the last two questioners, I'd like to ask you to share with us what your faculty and the people you are working with are thinking about in addressing some of these other challenges that have to do with: ‘Where is that education going to occur?’, particularly the clinical part of that. How is continuity going to be taught? How are the other health professions going to be involved? How are new content areas and new skills, as the previous questioner asked, going to be included, and how are we going to inculcate a truly lifetime learning, because there is no way that the challenge of that explosion of knowledge is going to be dealt with if we think of it in the boxes of our medical schooling and residency years, as opposed to thinking of it as a lifelong process? So please expand for us your vision, and how some of these other challenges are going to be dealt with beyond this very, I think, worthwhile organizational approach to information.
Densen, Iowa City: As the previous speaker indicated, there is only so much one can share in a 12-minute presentation. The elements of continuity of care that you alluded to, the question of whether outpatient exposure should come first?' and whether late third or fourth year medical students should be introduced into the clinical environment or a paced environment later are still under discussion at Iowa. But as you of all people know, there are some schools that have first moved into the outpatient arena, and I think that is something that many schools, including ours, need to think more seriously about. Some other elements were touched on by Ken Ludmerer in his 2002 presentation, particularly the element of “How can schools move knowledge from a basic scientist, whose research may focus on the phosphorylation of serines versus threonines, into the broader clinical environment?” I believe this challenge is going to drive faculty development and the need for medical schools to finance education differently than they do now, and I'm not unique in thinking that. The determination and commitment that a dean must have to successfully manage the flow of discretionary funds that may be helping to keep departmental budgets neutral, and to couple them to the delivery of medical education, is admittedly considerable. Nonetheless, this argument must be made. With regard to the question of: “How do you incorporate other healthcare professions?”, at Iowa, we have been educating medical students and physician-assistant students together for years, and have incorporated most of our health-science students into both the inpatient, and particularly the outpatient, settings. I know these are very general answers, and I'd be happy to discuss them in more detail with you later. I agree they are significant challenges.
Page, Madison: I really appreciate your thoughts and wanted to ask a question. As you may know, what had been the medical school at the University of Wisconsin is now a school of medicine and public health, and we are working to achieve greater integration of the curricula throughout the 4-year program. How are you seeing the public health perspective, which I believe has been underemphasized in traditional medical education? How are you incorporating that, given the overabundance of information we are trying to provide for our students in the first place?
Densen, Iowa City: Our current curriculum is relatively limited in this regard. But a point I was trying to make during the presentation is that in the proposed curriculum on mechanisms of disease, public health would be a specific mechanism of disease, category eight in the example. I have further proposed that the institution copy an initiative in place at Florida International University, in which anyone who goes into one of the health sciences, whether it be dentistry, pharmacy, or some other, must participate in a course covering, for example, the basic elements of health-care systems, public health, and health-care disparities. Such a course would be good not just because of the content, but also as a cornerstone for inter-professional education.
Alexander, Atlanta: Thank you for a terrific talk. We have a great deal of affinity for the notion of common mechanisms of multiple diseases or multiple phenotypes of the clinical expression of disease. You could even get those categories, I think as you suggested, even lower than eight. How many different mechanisms are there? A colleague of mine has 25. I have 3, but I think the general principle is very appealing. Given the challenging times in which we are living and our need to husband resources in the best possible manner, are departmental structures still relevant? I'm sure you've probably thought about this, and if you're like most people, haven't done much about it. But what are your thoughts?
Densen, Iowa City: I have thought about this issue quite a bit. When I was a medical student, you could tell the difference between a physiologist and a biochemist, because one walked around with a strain gauge while the other had a column chromatograph. But now you can't tell the difference between the two, because they use the same laboratory techniques, and their investigations are focused at the molecular level. So from my perspective, it is not important that basic science information be delivered in a discipline-centered manner, and this is evident in the mechanisms-of-disease model that I proposed. There does need to be a way to get basic scientists involved in the educational mission, but whether it's through the department of biochemistry or the department of physiology, in my view, is irrelevant. Some people would propose that's true also for the clinical disciplines. I am not as sanguine about that; I see some advantages and some disadvantages in it. But I do think that for schools like ours, in which students basically must rotate through every clinical discipline, it's going to be increasingly important to focus on the core clinical disciplines at an early stage, so that students can individualize their curricula for the last 12 to 18 months of their schooling. I can talk to you more about that later if you wish, but with regard to a non-departmentally-based clinical curriculum, unless the delivery of health care moves to integrated-care clinics, I think it would not be a good educational strategy to separate content from discipline. Moreover, the structure of graduate medical education and clinical practice will continue to support the discipline-based model.
Wolf, Boston: What are your thoughts about how to recruit teachers to do the teaching in the model you propose, and also about how to educate the teachers? Do you have a spiral approach to keeping the faculty up to date?
Densen, Iowa City: You have touched on a key element for all medical schools aspiring to implement a deeply integrated, non-discipline-based curriculum. My personal approach would to better align education dollars with the educational mission. I believe we can get more bang for that buck, and that education could be delivered by far fewer faculty across the disciplines than we currently utilize. One would still need to have a percentage, say 25%, of faculty with deeply specialized knowledge or expertise who have unique insights and can communicate them. But this doesn't mean that those faculty should devote significant amounts of time to the overall educational mission. Just as specialization is occurring in all fields of medicine, I think this should be, and will be, true in education. For this to happen, there will need to be a set of specific expectations and rewards for education faculty, which in turn will require the re-alignment of educational funds to support this mission, as I mentioned earlier. That's the challenge. Thank you very much.
REFERENCES
- 1.Cohen JJ, Hager M, Russell S. Revisiting the Medical School Mission at a Time of Expansion. New York: Josiah Macy, Jr. Foundation; 2009. [Google Scholar]
- 2.Scientific Foundations for Future Physicians. Report of the AAMC/HHMI Committee. Washington, DC: Association of American Medical Colleges; 2009. [Google Scholar]
- 3.Cooke M, Irby DM, O'Brien BC. Educating Physicians: A Call for Reform of Medical School and Residency. San Francisco, California: Jossey-Bass; 2010. [Google Scholar]
- 4.Frenk J, Chen L, Bhutta ZA, et al. Health Professionals for a New Century: transforming education to strengthen health systems in an interdependent world. Lancet. 2010;376:1923–1958. doi: 10.1016/S0140-6736(10)61854-5. [DOI] [PubMed] [Google Scholar]
- 5.Ludmerer KM. New York: Oxford University Press; 1999. Time to Heal: American Education from the Turn of the Century to the Era of Managed Care. [Google Scholar]
- 6.Ludmerer KM. The Internal Challenges to Medical Education. Trans Am Clin Climatol Assoc. 2003;114:241–253. [PMC free article] [PubMed] [Google Scholar]
- 7.Schroeder SA. We can do better—Improving the health of the American people. N Engl J Med. 2007;357:1221–1228. doi: 10.1056/NEJMsa073350. [DOI] [PubMed] [Google Scholar]
- 8.Woods NN, Brooks LR, Norman GR. It all makes sense: biomedical knowledge, causal connections and memory in the novice diagnostician. Adv Health Sci Educ. 2007;12:405–417. doi: 10.1007/s10459-006-9055-x. [DOI] [PubMed] [Google Scholar]
- 9.Woods NN, Brooks LR, Norman GR. The role of biomedical knowledge in diagnosis of difficult clinical cases. Adv Health Sci Educ. 2007;12:417–426. doi: 10.1007/s10459-006-9054-y. [DOI] [PubMed] [Google Scholar]
- 10.Hattie J. London: Routledge; 2009. Visible Learning: A Synthesis of Over 800 Meta-analyses Relating to Achievement; p. 168. [Google Scholar]
- 11.Norman GR. The effectiveness and effects of effect sizes. Adv Health Sci Educ. 2003;8:183–187. doi: 10.1023/a:1026090406201. [DOI] [PubMed] [Google Scholar]
- 12.Harden RM, Stamper N. What is a spiral curriculum? Med Teacher. 1999;21:142–143. doi: 10.1080/01421599979752. [DOI] [PubMed] [Google Scholar]
- 13.Hirsh DA, Ogur B, Thibault GE, et al. “Continuity” as an organizing principle for clinical education reform. N Engl J Med. 2007;356:858–866. doi: 10.1056/NEJMsb061660. [DOI] [PubMed] [Google Scholar]