Abstract
Objective
Fibromyalgia is a common, chronic pain condition for which patients frequently use complementary and alternative medicine, including Reiki. Our objective was to determine whether Reiki is beneficial as an adjunctive fibromyalgia treatment.
Design
This was a factorial designed, randomized, sham-controlled trial in which participants, data collection staff, and data analysts were blinded to treatment group.
Setting/location
The study setting was private medical offices in the Seattle, Washington metropolitan area.
Subjects
The subjects were comprised 100 adults with fibromyalgia.
Intervention
Four (4) groups received twice-weekly treatment for 8 weeks by either a Reiki master or actor randomized to use direct touch or no touch (distant therapy).
Outcome measures
The primary outcome was subjective pain as measured by visual analog scale at weeks 4, 8, and 20 (3 months following end of treatment). Secondary outcomes were physical and mental functioning, medication use, and health provider visits. Participant blinding and adverse effects were ascertained by selfreport. Improvement between groups was examined in an intention-to-treat analysis.
Results
Neither Reiki nor touch had any effect on pain or any of the secondary outcomes. All outcome measures were nearly identical among the 4 treatment groups during the course of the trial.
Conclusion
Neither Reiki nor touch improved the symptoms of fibromyalgia. Energy medicine modalities such as Reiki should be rigorously studied before being recommended to patients with chronic pain symptoms.
Introduction
Fibromyalgia is a condition of unknown cause characterized by chronic, diffuse pain and tenderness to palpation at specific musculoskeletal sites.1 It is the second most common rheumatologic condition after osteoarthritis, afflicting 2–4% of the general population.2 Perhaps because most randomized, controlled trials of allopathic interventions have failed to demonstrate sustained benefit,3 a majority of patients with fibromyalgia report having tried at least one complementary and alternative medicine treatment.4–6 In one study,6 55% of patients with fibromyalgia noted using energy medicine modalities such as Reiki, therapeutic touch, qigong, and magnet therapy. Although evidence is scant regarding its efficacy, safety, and mechanisms, energy medicine has been promulgated as a low-risk adjunctive treatment for chronic pain.7,8
Reiki is a form of energy medicine developed in Japan in the late 1800s in which the healer channels “universal life energy” to the patient through light touch and positive healing intention.7,8 Advanced Reiki providers, or masters, report being able to heal with intention alone, without physically contacting the patient or even being in close vicinity, a technique called distant Reiki.7,8 According to the largely anecdotal literature, Reiki improves pain control and psychologic well-being with few, if any, adverse effects.7–11
To our knowledge, no blinded, randomized controlled trials of Reiki for chronic pain have been published. We conducted a clinical trial with a factorial design to investigate whether Reiki is beneficial as an adjunctive treatment for fibromyalgia. Participants were randomized to true Reiki administered by Reiki masters or sham therapy administered by actors. In addition, participants received either direct-touch Reiki or distant Reiki from their assigned providers. We hypothesized a priori that true Reiki would result in the most clinical improvement, with direct touch outperforming distant therapy because the relative invasiveness of touch versus no-touch would be more likely to activate a therapeutic placebo response.
Materials and Methods
Participants
Participants were recruited from the Seattle, Washington metropolitan area between April 2003 and September 2004. Recruitment strategies included disseminating information on the study through media stories in newspapers, television, advertisements, signs posted on research bulletin boards at tertiary care, university-based hospitals, and letters to local fibromyalgia support groups and health care providers with large caseloads of patients with fibromyalgia. We also recruited individuals with fibromyalgia who had participated in a clinical trial in the Seattle area 2 years prior and patients with fibromyalgia seeking care at a specialty referral clinic. The Institutional Review Board at the University of Washington approved the study and participants provided written informed consent.
Participants were screened for eligibility by a research coordinator. Eligibility criteria required that potential participants (1) speak English, (2) were ≥18 years old, (3) have a physician diagnosis of fibromyalgia, (4) have a global pain score of ≥4 on a visual analog scale (VAS, 0 = no pain, 10 = worst pain ever), (5) be willing to be randomized, (6) keep pharmacological and nonpharmacological therapies for fibromyalgia constant throughout the study, and (7) use only acetaminophen and ibuprofen for breakthrough pain. Participants were excluded if they reported other pain-related medical conditions, were pregnant or breastfeeding, used narcotics, were involved in ongoing litigation related to their fibromyalgia or receiving disability payments (which might reduce their incentive for improvement), lived more than an hour away from the research center, were unable to attend 8 weeks of biweekly therapy, or had previously received any energy medicine modality (to maximize blinding).
Randomization
Potential participants were told they had an equal chance of being assigned to 1 of 4 treatments, representing combinations of direct Reiki or distant Reiki and treatment by a Reiki master or a sham Reiki provider. After enrollment but before randomization, a research coordinator trained in the tender-point examination conducted a baseline examination and confirmed the fibromyalgia diagnosis using the 1990 American College of Rheumatology criteria.1 Next, another research coordinator not involved with data collection randomized participants using a computer-generated blocked random allocation sequence with a block size of 4. This research coordinator, who was blinded to whether providers were Reiki masters or actors, informed sites of the treatment assignment.
Intervention
Providers
Three experienced female Reiki masters trained in the popular Usui style with 5–18 years of experience in the United States treated study participants in private medical offices. Four (4) actors who were matched to the Reiki masters in age group, gender, race, and general appearance provided control interventions. Additional selection criteria for the actors were no experience with or knowledge of energy medicine, no self-reported natural ability as a healer, and low healing touch potential according to the subjective assessments of the Reiki masters after meeting the actors and feeling their hands. The principal investigator trained all Reiki masters and actors in study procedures. Every effort was made to have participants treated by the same provider for the entire 8 weeks.
Treatments
Participants were randomized into 1 of 4 groups. The first was a generic 30-minute direct contact treatment delivered by a Reiki master in which the participant was lightly touched for ∼2 minutes at each of 12 standardized Reiki hand positions7,8 (eyes, back of head, crown, thymus/lungs, solar plexus/heart, abdomen, scapula, midback, lower back, sacrum, feet, energy brush from head to toes). The second was distant Reiki administered by a master who sat ∼2 feet away, maintained hand positions in the “sending” mode, and focused healing intention on the participants. The third was sham direct contact Reiki at the 12 standardized hand positions given by actors. In the fourth arm, actors sat ∼2 feet away from participants and mimicked the “sending” position of distant Reiki. Actors attempted to minimize unconscious healing intentions by occupying their minds with thoughts unrelated to the participant (e.g., doing mental arithmetic, practicing vocabulary from a foreign language, or rehearsing lines from a play). All participants were supine on a massage table in a white-walled treatment room without incense or music. Participants treated with direct touch were prone for the second half of the treatment.
The trial consisted of 2 treatments weekly for 8 weeks (16 treatments). We selected this schedule based on recommendations of both the National Center for Complementary and Alternative Medicine website on Reiki therapy9 and our experienced Reiki masters who predicted that this duration and frequency of treatment would result in differences in treatment outcomes. We considered participants who received at least 12 treatments (75%) as completing a full course. Outcome data were collected at regularly scheduled time points from participants who discontinued treatment.
Blinding
Reiki masters and actors could not be blinded to group assignments and participants could not be blinded to direct versus distant therapy. To optimize participant blinding to master or sham provider assignment, we staggered appointments to limit overlap time in the waiting area and conversation between participants. Providers used a standardized script that minimized talking with participants, used pre-formulated answers to common questions, wore uniforms, and used false names. Compliance with the protocol was monitored by random visits during treatments from the principal investigator and a research coordinator. All research personnel who collected, monitored, and analyzed data were unaware of treatment group.
Covariate and outcome measures
Demographic measures collected at the initial examination included age, sex, race, education, income, marital status, number and type of pain medicines, and number of visits to conventional and complementary and alternative providers. To ascertain whether participants' knowledge and expectations differed at baseline, we asked them how reasonable Reiki seemed as a treatment for fibromyalgia.
We collected outcome data at baseline (week 0), midway through the intervention (week 4), at the end of treatment (week 8), and 3 months after completion of treatment (week 20). The primary outcome was subjective pain during the previous month, as measured by a standard 10-cm visual analog scale (VAS) (0 = no pain at all, 10 = severe pain). Other VAS outcomes included fatigue intensity (0 = no fatigue, 10 = severe fatigue), sleep quality (0 = worst possible, 10 = could not be better), and general well-being (0 = worst possible, 10 = could not be better). Of principal interest was the longitudinal profile of VAS measurements over the treatment and follow-up period.
Secondary outcomes were physical and mental functioning as measured by the Medical Outcomes Study 36-item Short-Form Health Survey,12 which has high reliability and validity in diverse patient populations, including those with chronic pain and fatigue.13,14 The Short Form-36 physical and mental component scales are standardized in the American population to have a mean of 50 and a standard deviation of 10, with higher scores indicating better functioning.15
To verify that use of fibromyalgia therapies were stable during the study, we compared participants' pain medication use at baseline with those used during the previous 7 days at weeks 4, 8, and 20. We also calculated the number of new medications for each participant at each time point and the number of visits to conventional and complementary and alternative health care providers.
To evaluate the adequacy of blinding, participants rated the skill level of their provider, efficacy of Reiki for fibromyalgia, and how sure they were that they had received Reiki versus sham Reiki at weeks 4, 8, and 20 using an ordinal scale (0 = most negative, 5 = most positive). We defined endorsement as a response of 3 or more. At 4, 8, and 20 weeks, participants indicated whether they had experienced increased anxiety, a theoretical concern resulting from too much energy medicine or other symptoms they attributed to their treatment.
Statistical Analysis
Descriptive statistics
We described demographic, clinical, and outcome variables at baseline using means and standard deviations for continuous variables and percents for categorical variables, stratified by treatment group.
VAS outcomes
We used all study data according to participants' random assignment, thus adhering to an intention-to-treat analysis. We used generalized estimating equations to model the association between treatment group and the VAS and functional outcomes. Treatment group variables included provider assignment (Reiki master or actor) and treatment type (direct touch or distant therapy). All models included week since enrollment (week 0) as a set of 3 binary variables indicating observations were made at 4, 8, and 20 weeks. Such coding required no assumptions regarding the relationship between the outcome measures and time. The generalized estimating equations models used the identity link for continuous outcomes, assumed an unstructured working correlation matrix, and used the robust variance estimator16 to account for correlated measurements of each participant's data.
Preliminary analyses included an interaction term modeling the combined effect of receiving direct Reiki from a master. This term was only included in the final models if it was statistically significant in the preliminary analyses. Because we did not detect any interactions between provider assignment and type of therapy, the interaction term was removed from the final model for each outcome. No treatment-by-time interactions were suspected a priori, and so none were included in the analysis. Final results are presented as adjusted least-square means with 95% confidence intervals. We maintained an α level of 0.05 as the threshold for statistical significance.
Other outcomes
(1) Medications and Health Care Utilization: We used generalized estimating equations to evaluate the association between treatment group and number of pain medications, as well as number of health care provider visits reported at baseline and at 4, 8, and 20 weeks. Identical models were used for primary outcomes and adverse events, except that we used a log link to model Poisson distributions for the count data. (2) Blinding: For each blinding question, we used χ2 tests to compare the endorsement proportions at week 8 by provider assignment. (3) Adverse Effects: We used generalized estimating equations to evaluate the association of treatment group and adverse events. The models were identical to those described for the primary outcomes, above, except that we used the logit link to model the log-odds of experiencing adverse events.
Missing data
The estimates produced by generalized estimating equations modeling are valid only if model variables and the missingness of data are not systematically related. Thus, participants with missing outcome measurements were included in the analysis, assuming these data were missing at random. In addition, we used a separate generalized estimating equation to determine whether missingness of data was related to treatment assignment for the primary outcome variable. These models treated missingness as a binary outcome and were modeled using a logit link function assuming binomial variance for the missingness indicator, and an unstructured working correlation matrix to account for correlation between measurements provided by a single individual.
Power
This study had a two-factor design (provider assignment and therapy type). Therefore, to ascertain our power, we determined the magnitude of treatment effects due to a single factor detectible with 80% power, given that 50 individuals were randomly assigned to each level of the factor. We used standard deviation information from baseline measures from a recent clinical trial17 involving a similar sample of patients with fibromyalgia to calculate the magnitude of detectible differences in our outcomes measures. For an α error threshold of 0.05, we had 80% power to detect differences of 1.0 cm or more on the VAS for pain and fatigue, 1.2 cm for sleep quality and overall well-being, and differences of 4.7 and 5.8 on the Short Form-36 physical and mental component scores, respectively.
Role of funding source
The National Center for Complementary and Alternative Medicine funded the study, but had no role in study design, data collection, data analysis, data interpretation, writing of the manuscript, or decision to submit the paper for publication.
Results
Participant flow
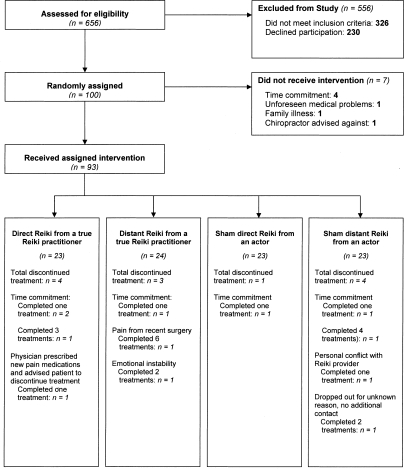
One hundred (100) participants provided baseline measurements and were randomized (Fig. 1). Of these, 7 dropped out of the study prior to receiving any therapy. An additional 12 participants dropped out after receiving 1–8 treatments. The most common reason given for dropping out was other time commitments (Fig. 1). Overall, 76% of participants completed a full course of treatment with no statistical differences (p > 0.05) between provider assignment or therapy type.
FIG. 1.
Patient flow diagram for Reiki study.
Baseline participant characteristics
Most participants were white women with a college degree (Table 1). The mean age of all participants was 49 years and 43% were married. The mean VAS was 6.4 cm for pain, 6.8 cm for fatigue, 4.1 cm for quality of sleep, and 4.5 cm for overall well-being. The mean physical and mental component summary scores were 32 and 42, respectively. Almost half of participants reported being sure that Reiki could relieve the symptoms of fibromyalgia. Baseline demographic characteristics, clinical features, and treatment expectations did not differ across the 4 treatment groups.
Table 1.
Demographic and Clinical Features by Treatment Assignment at Enrollment
| |
Reiki master |
Actor |
|
||
|---|---|---|---|---|---|
| |
Direct |
Distant |
Direct |
Distant |
Total |
| Characteristics | (n = 25) | (n = 25) | (n = 25) | (n = 25) | (n = 100) |
| Demographic features | |||||
| Age in years, mean (SD) | 49 (13) | 52 (15) | 45 (12) | 49 (13) | 49 (13) |
| Female, % | 92 | 92 | 96 | 88 | 92 |
| White ethnicity, % | 76 | 80 | 84 | 80 | 80 |
| College graduate, % | 52 | 56 | 46 | 56 | 53 |
| Marital status, % | |||||
| Never married | 21 | 33 | 32 | 24 | 27 |
| Married or living with partner | 50 | 46 | 40 | 40 | 43 |
| Separated, divorced, or widowed | 29 | 21 | 28 | 36 | 28 |
| Income,a % | |||||
| $0–14,999 | 36 | 28 | 16 | 32 | 28 |
| $15,000–24,999 | 16 | 8 | 12 | 12 | 12 |
| $25,000–34,999 | 4 | 24 | 28 | 12 | 17 |
| $35,000–49,999 | 24 | 16 | 16 | 16 | 18 |
| $50,000 and above | 16 | 24 | 28 | 28 | 24 |
| Clinical features | |||||
| Pain medications taken 2 weeks prior to enrollment, % | |||||
| None | 25 | 26 | 10 | 28 | 22 |
| 1 | 55 | 37 | 45 | 44 | 45 |
| 2 or more | 20 | 37 | 45 | 28 | 32 |
| CAMb visits within 30 days prior to enrollment, % | |||||
| 0 visits | 64 | 56 | 64 | 68 | 63 |
| 1 or 2 visits | 16 | 16 | 20 | 20 | 18 |
| 3 or 4 visits | 16 | 16 | 4 | 12 | 12 |
| 5 or more visits | 4 | 12 | 12 | 0 | 7 |
| Allopathic visits within 30 days prior to enrollment, % | |||||
| 0 visits | 44 | 28 | 20 | 24 | 29 |
| 1 or 2 visits | 36 | 36 | 28 | 36 | 34 |
| 3 or 4 visits | 4 | 16 | 24 | 20 | 16 |
| 5 or more visits | 16 | 20 | 28 | 20 | 21 |
| Outcome measures at enrollment | |||||
| Visual analog scale,c mean (SD) | |||||
| Pain intensity | 6.3 (2.2) | 6.4 (2.6) | 6.8 (2.1) | 6.1 (2.4) | 6.4 (2.3) |
| Fatigue intensity | 6.6 (2.4) | 7.1 (1.6) | 6.2 (2.7) | 7.3 (2.0) | 6.8 (2.2) |
| Sleep quality | 4.2 (2.7) | 4.4 (2.5) | 4.1 (2.5) | 3.8 (2.5) | 4.1 (2.5) |
| Overall well-being | 4.4 (2.7) | 4.0 (2.1) | 5.0 (2.4) | 4.5 (2.4) | 4.5 (2.4) |
| Short Form-36,d mean (SD) | |||||
| Physical component | 32 (9) | 31 (8) | 34 (10) | 33 (9) | 32 (9) |
| Mental component | 40 (13) | 42 (10) | 45 (11) | 40 (13) | 42 (12) |
Income data were not available for one participant who received direct Reiki from a Reiki master.
Complementay and alternative medicine (CAM) included acupuncture, massage therapy, chiropractic, naturopathy, homeopathy, and spiritual or psychic healing. Allopathic care included standard primary care from physicians, nurses, and physician assistants, rheumatology, orthopedic therapy, physical therapy, occupational therapy, biofeedback, psychiatry, mental health counseling, and nutritional counseling.
One subject did not provide any data at baseline nor at any follow-up visits.
Short-Form Health Survey.
SD, standard deviation.
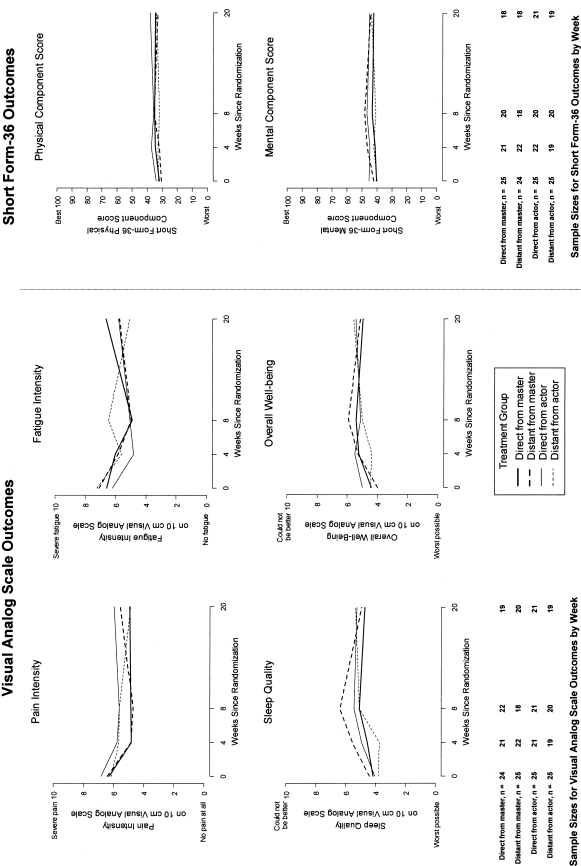
VAS outcomes
Figure 2 depicts the mean values for the VAS and functional outcomes for each treatment group at each time point. No VAS or functional outcome differed between the 4 treatment groups during or following the interventions. Table 2 shows estimates of the mean differences attributable to the two treatment factors for each outcome. No treatment factor main effects were significant for any outcome.
FIG. 2.
Mean values of visual analog scale (VAS) and Short Form-36 (SF-36) outcomes and sample sizes by week and treatment group. Measurements were made during active therapy (weeks 0, 4, and 8), and 12 weeks post-therapy (week 20).
Table 2.
Estimated Mean Differences in Primary Outcome Measures by Treatment Factor
| |
Reiki master |
Direct touch |
||||
|---|---|---|---|---|---|---|
| Outcome | Mean differencea | (95% CI) | p-value | Mean differenceb | (95% CI) | p-value |
| Visual analog scale | ||||||
| Pain | −0.4 | (−1.1, 0.3) | 0.31 | 0.2 | (−0.5, 1.0) | 0.52 |
| Fatigue | 0.4 | (−0.4, 1.1) | 0.31 | −0.3 | (−1.0, 0.4) | 0.45 |
| Sleep quality | 0.2 | (−0.5, 0.9) | 0.52 | −0.1 | (−0.8, 1.1) | 0.78 |
| Overall well-being | −0.2 | (−0.8, 0.5) | 0.61 | 0.2 | (−0.4, 1.2) | 0.51 |
| Short form-36 | ||||||
| Physical | −1.7 | (−5.0, 1.6) | 0.32 | 1.9 | (−1.4, 5.2) | 0.26 |
| Mental | −1.2 | (−4.8, 2.4) | 0.52 | 0.7 | (−3.0, 4.3) | 0.72 |
Comparing outcomes of those assigned to a Reiki master to those assigned to an actor.
Comparing outcomes of those assigned to direct touch to those assigned to distant therapy.
One individual assigned to receive direct Reiki from a master was missing baseline and follow-up VAS and all follow-up functional outcome measurements; 10 other participants were missing follow-up data for the VAS and functional measures (2 receiving direct Reiki, 2 distant Reiki, 2 sham direct Reiki, 4 sham distant Reiki). All participants with VAS baseline data (n = 99) and functional outcome data (n = 100) were included in the outcome analyses. Missingness was not associated with either provider assignment or treatment type on the VAS (p = 0.90 and p = 0.45) or functional (p = 0.29 and p = 0.64) outcomes. Our test for interaction between provider assignment and treatment type in predicting missingness of these outcome measures was also not significant.
Adverse events
Of the 93 individuals who received at least one study treatment, 38 (41%) reported excess energy or feelings of anxiety and 17 (18%) reported other adverse events such as worsening of sleep and depressed mood. Neither provider assignment nor treatment type was associated with adverse events.
Other outcomes
Medications
In a generalized estimating equation model, the mean number of pain medications was 29% lower among participants assigned to Reiki masters than those seen by actors (95% confidence interval: 3%, 48%, p = 0.03).
Health care utilization
Regression analysis indicated that provider assignment was unrelated to the average monthly visits to allopathic (p = 0.18) and complementary and alternative medicine (p = 0.47) providers. Likewise, direct touch and distant treatment groups had similar monthly use of allopathic (p = 0.76) and complementary and alternative (p = 0.23) medicine providers.
Blinding
At week 8, 79 participants rated their certainty about being treated by a Reiki master, 77 reported on their provider's skill level, and 77 on their confidence in Reiki to relieve symptoms. The proportion of participants who believed they had been treated by a Reiki master did not differ by assignment to a master or actor (77% versus 65%, p = 0.24). Likewise, participants treated by both Reiki masters and actors felt that their providers demonstrated high skill levels (89% versus 85%, p = 0.52) and could relieve fibromyalgia symptoms (74% versus 66%, p = 0.38).
Discussion
Anecdotal reports have shown promise and few negative side-effects for the use of Reiki and other energy medicine modalities for pain in clinical settings.7–11 To our knowledge, this is the first randomized, blinded, sham-controlled trial of Reiki for chronic pain. The factorial design, which compared treatment by a Reiki master and sham provider and direct and distant techniques, revealed no treatment improved the pain, fatigue, well-being, or physical and mental functioning of participants with fibromyalgia. Similarly, secondary outcomes such as health care utilization did not differ between treatment groups with the exception of pain medication use, which is likely to have occurred by chance given the lack of difference between groups for multiple other outcome indicators.
Only two other trials have examined Reiki for chronic pain.10,18 Neither of these trials met the criteria for a rigorously designed study of energy medicine.19 In an unblinded study of 24 patients with cancer pain,10 self-reported pain control and quality of life improved but opioid use was unchanged when direct Reiki was used as an adjunctive therapy. Another trial compared direct Reiki to progressive muscle relaxation, sham Reiki, and no treatment in 120 patients with pain due to diverse chronic medical conditions.18 Although pain, depression, and anxiety were reduced, no data were presented to verify that participants were adequately blinded to the treatment interventions; also, the sham Reiki providers were research assistants, healing intention was not controlled for, and it is unclear whether the individuals involved in collecting the data were blinded to the treatment assignment.
Our study has several strengths including using sham Reiki providers that controlled for both touch and healing intention and a study design that accounted for the potential placebo effects of light touch. We also were vigilant about blinding participants, data collectors, and data analysts and measuring treatment expectations. In addition, we had a relatively low rate of attrition for an unconventional therapy and our follow-up extended 12 weeks beyond the actual treatment. Lastly, we used standard, validated outcome measures for fibromyalgia.
Nonetheless, our study also has limitations. First, our sample size was modest and our study was not powered to detect subtle changes. Second, our study providers used standardized Reiki positions that did not cater to individualized participant needs. Third, although the duration and length of treatment for Reiki have not been clearly defined, our treatment intensity or duration may have been insufficient for a chronic pain disorder. Finally, our trial was so tightly controlled to avoid the many potential sources of information leakage, bias, and psychologic impact of the healer–patient relationship (even with sham healers), that it may not represent the optimal circumstances for healing to take place. Some distant healing researchers have advocated conducting studies in nonhuman populations to minimize the bias of multiple possible psychologic factors,20 and others21 have resorted to waiting lists and informing some of their patients of their randomization group.
Conclusion
Applying the paradigm of randomized, double-blinded placebo-controlled trials, the “gold standard” for biomedically based interventions, is challenging in energy medicine studies. The utilization of energy medicine such as Reiki has increased in the United States over the last 15 years22,23 with use of 10% by those 50 and older.24 Two (2) pilot Reiki studies show improvements in biological and psychologic measures of stress after Reiki treatments compared to sham and placebo treatments,11,25 although no robustly designed clinical trial has shown a therapeutic benefit of Reiki for pain. Our randomized controlled trial of Reiki for fibromyalgia suggests that adults with fibromyalgia are unlikely to benefit from Reiki. Future Reiki trials should require blinding of participants and staff who handle data as well as thoughtful construction of control and placebo interventions—no easy feat considering our nebulous understanding of energy medicine therapies.
Acknowledgments
The authors would like to thank the staff at the Center for Clinical and Epidemiologic Research involved in the Reiki study (Roxane Geller, Langley Partridge, and Jovine Umali), the Reiki masters, actors, and study participants. In addition, we appreciate the helpful feedback of Dr. Karen Sherman on study design and manuscript review. This study was supported by grant R21 AT01075-01 from the National Center for Complementary and Alternative Medicine, National Institutes of Health. Controlled Trial #: ISRCTN32552026 http://www.controlledtrials.com/isrctn/trial/|/0/32552026.html
Disclosure Statement
No authors have competing financial interests.
References
- 1.Wolfe F. Smythe HA. Yunus MB, et al. The American College of Rheumatology 1990 criteria for the classification of fibromyalgia: Report of the multicenter criteria committee. Arthritis Rheum. 1990;33:160–172. doi: 10.1002/art.1780330203. [DOI] [PubMed] [Google Scholar]
- 2.Wolfe F. Ross K. Anderson J, et al. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19–28. doi: 10.1002/art.1780380104. [DOI] [PubMed] [Google Scholar]
- 3.Goldenberg DL. Burckhardt C. Crofford L. Management of fibromyalgia syndrome. JAMA. 2004;292:2388–2395. doi: 10.1001/jama.292.19.2388. [DOI] [PubMed] [Google Scholar]
- 4.Crofford LJ. Appleton BE. Complementary and alternative therapies for fibromyalgia. Curr Rheumatol Rep. 2001;3:147–156. doi: 10.1007/s11926-001-0010-9. [DOI] [PubMed] [Google Scholar]
- 5.Pioro-Boisset M. Esdaile JM. Fitzcharles MA. Alternative medicine use in fibromyalgia syndrome. Arthritis Care Res. 1996;9:13–17. doi: 10.1002/art.1790090105. [DOI] [PubMed] [Google Scholar]
- 6.Herman CJ. Allen P. Prasad A, et al. Use of complementary therapies among primary care clinic patients with arthritis. Prev Chronic Dis. 2004;1:A12. [PMC free article] [PubMed] [Google Scholar]
- 7.Barnett L. Chambers M. Davidson S. Reiki Energy Medicine. Rochester, VT: Healing Arts Press; 1996. [Google Scholar]
- 8.Miles P. True G. Reiki: Review of a biofield therapy history, theory, practice, and research. Altern Ther Health Med. 2003;9:62–72. [PubMed] [Google Scholar]
- 9.NCCAM. An introduction to Reiki. www.nccam.nih.gov/health/Reiki/ [Jan 25;2007 ]. www.nccam.nih.gov/health/Reiki/
- 10.Olson K. Hanson J. Michaud M. A phase II trial of Reiki for the management of pain in advanced cancer patients. J Pain Symptom Manage. 2003;26:990–997. doi: 10.1016/s0885-3924(03)00334-8. [DOI] [PubMed] [Google Scholar]
- 11.Shore AG. Long term effects of energetic healing on symptoms of psychological depression and self-perceived stress. Altern Ther Health Med. 2004;10:42–48. [PubMed] [Google Scholar]
- 12.Ware JE. Snow K. Kosinski M, et al. Short Form-36 Health Survey Manual & Interpretation Guide. Lincoln, MA: QualityMetric, Inc.; 2000. [Google Scholar]
- 13.Buchwald D. Pearlman T. Umali J, et al. Functional status in patients with chronic fatigue syndrome, other fatiguing illnesses and healthy individuals. Am J Med. 1996;71:364–370. doi: 10.1016/S0002-9343(96)00234-3. [DOI] [PubMed] [Google Scholar]
- 14.Komaroff AL. Fagioli LR. Doolittle TH, et al. Health status in patients with chronic fatigue syndrome and in general population and disease comparison groups. Am J Med. 1996;101:281–290. doi: 10.1016/S0002-9343(96)00174-X. [DOI] [PubMed] [Google Scholar]
- 15.Ware JE. Kosinski M. Keller SD. Short Form-36 Physical and Mental Health Summary Scales: A User's Manual. Boston, MA: The Health Institute; 1994. [Google Scholar]
- 16.Diggle PJ. Heagerty PJ. Liang KY, et al. Analysis of Longitudinal Data. Second Edition. Oxford, UK: Oxford University Press; 2002. [Google Scholar]
- 17.Assefi NP. Sherman KJ. Jacobsen C, et al. A randomized clinical trial of acupuncture compared with sham acupuncture in fibromyalgia. Ann Intern Med. 2005;143:10–19. doi: 10.7326/0003-4819-143-1-200507050-00005. [DOI] [PubMed] [Google Scholar]
- 18.Dressen L. Singg S. Effects of Reiki on pain and selected affective and personality variables of chronically ill patients. Subtle Energies Energy Med. 1998;9:51–82. [Google Scholar]
- 19.Warber SL. Gordon A. Gillespie BW, et al. Standards for conducting clinical biofield energy healing research. Altern Ther Health Med. 2003;9:A54–A64. [PubMed] [Google Scholar]
- 20.Astin JA. Harkness E. Ernst E. The efficacy of “distant healing”: A systematic review of randomized trials. Ann Intern Med. 2000;132:903–910. doi: 10.7326/0003-4819-132-11-200006060-00009. [DOI] [PubMed] [Google Scholar]
- 21.Walach H. Bosch H. Lewith G, et al. Effectiveness of distant healing for patients with chronic fatigue syndrome: A randomized controlled partially blinded trial. Psychother Psychosom. 2008;77:158–166. doi: 10.1159/000116609. [DOI] [PubMed] [Google Scholar]
- 22.Eisenberg DM. Davis R. Ettner S, et al. Trends in alternative medicine use in the United States, 1990–1997. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 23.Tindle HA. Davis RB. Phillips RS, et al. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern Ther Health Med. 2005;11:42–49. [PubMed] [Google Scholar]
- 24.AARP and NCCAM. Complementary and alternative medicine: What people over 50 are using and discussing with their physicians. AARP and NCCAM report 2007. www.aarp.org/research/health/prevention/cam_2007.html. [Mar 5;2007 ]. www.aarp.org/research/health/prevention/cam_2007.html
- 25.Mackay N. Hansen S. McFarlane O. Autonomic nervous system changes during Reiki treatment: A preliminary study. J Altern Complement Med. 2004;10:1077–1081. doi: 10.1089/acm.2004.10.1077. [DOI] [PubMed] [Google Scholar]