Abstract
Background
Primary percutaneous coronary intervention (PCI) is preferred over fibrinolysis for the treatment of ST-segment elevation myocardial infarction (STEMI). In the United States, nearly 80% of people aged 18 years and older have access to a PCI facility within 60 minutes. We conducted this study to evaluate the areas in Canada and the proportion of the population aged 40 years and older with access to a PCI facility within 60, 90 and 120 minutes.
Methods
We used geographic information systems to estimate travel times by ground transport to PCI facilities across Canada. Time to dispatch, time to patient and time at the scene were considered in the overall access times. Using 2006 Canadian census data, we extracted the number of adults aged 40 years and older who lived in areas with access to a PCI facility within 60, 90 and 120 minutes. We also examined the effect on these estimates of the hypothetical addition of new PCI facilities in underserved areas.
Results
Only a small proportion of the country’s geographic area was within 60 minutes of a PCI facility. Despite this, 63.9% of Canadians aged 40 and older had such access. This proportion varied widely across provinces, from a low of 15.8% in New Brunswick to a high of 72.6% in Ontario. The hypothetical addition of a single facility to each of 4 selected provinces could increase the proportion by 3.2% to 4.3%, depending on the province. About 470 000 adults would gain access in such a scenario of new facilities.
Interpretation
We found that nearly two-thirds of Canada’s population aged 40 years and older had timely access to PCI facilities. The proportion varied widely across the country. Such information can inform the development of regionalized STEMI care models.
Primary percutaneous coronary intervention (PCI) is preferred over fibrinolysis for the treatment of ST-segment elevation myocardial infarction (STEMI) because of the reduced risk of death, stroke and recurrent myocardial infarction.1-4 However, the success of primary PCI depends on timely access.5-7 Current American, Canadian and European guidelines suggest that primary PCI be performed within 90 minutes after first medical contact (when the patient is first seen by pre-hospital care providers).8-10
Despite primary PCI being the preferred therapy for STEMI, it is not offered to all patients.11,12 Transportation time is one important barrier.13 This time constraint has led to a focus on the development of regional STEMI care models. Within these models, diagnosis is expedited and patients are transferred directly to PCI facilities. Regional care models are currently being implemented and tested across North America14-17 and internationally.5,18,19
To create regionalized care models, policy-makers must first evaluate the areas and populations where timely access to hospitals with PCI facilities is possible. The implications of driving times to PCI facilities in terms of pre-hospital triage has been studied in the United States.20,21 Nearly 80% of Americans aged 18 years and older are estimated to have access to a PCI facility within 60 minutes.21 We conducted this study to determine the current areas in Canada and the proportion of the population aged 40 and older with timely access to PCI facilities (within 60, 90 and 120 minutes). We also determined how the hypothetical addition of new facilities in underserved areas could change these estimates.
Methods
Data sources
We used road network analysis to evaluate geographic access to PCI facilities based on travel along a road network. This analysis requires data representing origins of travel, destinations and the linear features along which travel occurs. The road network we used was the CanMap® RouteLogistics file (DMTI Spatial, Markham, Ont.). This file can be used for shortest-route analyses of both time and distance. In addition to containing detailed street names and address locations along each segment of road, fields are included for the length and speed limit along each segment of road.
For origins of travel, we used individual dissemination areas from the 2006 Canadian census. (A dissemination area is the smallest geographic unit at which the census is publicly distributed.) We used the geographic centre of each dissemination area as the originating point of travel. There are 54 626 such areas in the country. Use of dissemination areas as the origin of travel allowed us to link population data to areas with access to primary PCI. Because we focused primarily on travel in and surrounding the immediate vicinity of urban areas, use of data at the level of the dissemination area was considered appropriate.22,23
For destinations, we used a comprehensive list of PCI facilities in Canada. The list was compiled through consultation with experts in both the Canadian Cardiovascular Outcomes Research Team (www.ccort.ca) and the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (www.approach.org). Each facility was geocoded based on its address location. The process of geocoding allowed for the creation of spatial files from text descriptions of addresses.24
We used geographic information systems to estimate travel time by ground transport based on the distance and speed limit stored in the road network file between each origin and destination. Geographic information systems are valuable tools for evaluating access to health services,25-28 specifically access to PCI facilities.21 We used ESRI ArcGIS 9.2 (Redlands, Calif.) for all geographic information systems analyses and map production.
Travel times
The methodology we used to analyze travel times was adapted from a 2006 study by Nallamothu and colleagues,21 who studied geographic access to PCI facilities in the United States. Because the recommended time to reperfusion after first medical contact is 90 minutes or less, we considered a baseline transporation time constraint of 60 minutes, which allowed an additional 30 minutes from hospital door to first balloon inflation. This 60-minute time constraint has been used in previous studies of access to PCI.21,29 In Canada, a recent quality-of-care indicator for acute myocardial infarction (AMI) is reperfusion within 120 minutes from first medical contact.30 Recognizing this longer window, we considered additional pre-hospital transportation times of 90 and 120 minutes.
Boundaries of the dissemination areas were used to calculate individual areas (in square kilometres) and their geographic centres. The population density for each dissemination area was calculated based on the total population and the geographic area within a dissemination area for each province (residents per square kilometre).The population densities were divided into tertiles, with the top third categorized as urban, the middle third as suburban and the bottom third as rural. This density designation was based on a prior study.21
We used the Network Analyst extension of ESRI ArcGIS 9.2 to evaluate travel time by ground. Travel cost matrices were used to determine the shortest route in minutes from each centre of a dissemination area to the nearest PCI facility within a province. To determine pre-hospital times more realistically, additional times were included in the baseline travel times. These additional times were based on data from studies in the United States and accounted for time to dispatch, time to patient and time spent at the scene. Dispatch times of 1.4 minutes were added to travel times in urban and suburban areas and 2.9 minutes in rural areas to account for the time from a call to emergency services to the dispatch of an ambulance.31 In the absence of information on ambulance locations at time of dispatch, empirically derived constants based on the literature were used to account for the time for an ambulance to reach a patient. Multipliers of 1.6 were used for travel times in urban areas, 1.5 in suburban areas and 1.4 in rural areas.32,33 For time at the scene, fixed additions of 8 minutes in urban and suburban areas and 9 minutes in rural areas were used.8,21
We conducted sensitivity analyses to evaluate the effect of changes in the overall travel time on the proportion of the population with access to a PCI facility. These sensitivity analyses could simulate situations in which travel time is increased or decreased owing to conditions such as changes in speed, time of day and weather conditions. Absolute changes were evaluated based on an increase or decrease of 10 minutes in the overall travel time. Relative changes were evaluated based on an increase or decrease of 25% in the overall travel time. One study in the United States showed that about 50% of patients with myocardial infarction transport themselves to hospital.34 Recognizing this, we conducted a final sensitivity analysis to model a scenario of patient self-transport to a PCI facility. In this analysis, the dispatch time, time to patient and time at the scene were removed from the models.
Populations with timely access
For each province in Canada, we determined the population of adults aged 40 years and older in each dissemination area who had access to a PCI facility within a specified travel time. We then summed the populations in these dissemination areas. This calculation was done separately for each time constraint under consideration (60, 90 and 120 minutes) as well as for each sensitivity analysis. Thepopulation with access was then divided by the total provincial population aged 40 and older to obtain the proportion of adults in that age group who had access within the specified time. We repeated these calculations for people aged 50, 60 and 70 years and older to evaluate how different age groups varied in terms of their access to a PCI facility within 60 minutes.
Hypothetical addition of new PCI facilities
To evaluate how the addition of new facilities would affect the population with access, a hypothetical situation was created whereby a PCI facility was added to each of the 4 most populated provinces (British Columbia, Alberta, Ontario and Quebec). The selection of a specific urban centre for the hypothetical facility in each of these provinces was guided by geograpic information systems analysis. The urban centre with the highest population density that fell outside of existing zones for timely access was selected for each province. Within these selected sites, we chose the current major hospital providing advanced health services as the hypothetical location for a new PCI facility. We evaluated the travel times for these hypothetical facilities using the methods described above for existing facilities.
A combination of variables was used to estimate the possible outcome benefits associated with the hypothetical addition of new PCI facilities. We first multiplied the increased population aged 20 years and older with access to a facility by the rates of hospital admission because of AMI among those 20 years and older (250.4 per 100 000)35 to estimate the potential number of hospital admissions because of AMI in this age group. Of these hospital admissions, estimates suggest that about 50% could be because of STEMI.36 Death within 4-6 weeks of an AMI has been shown to be reduced by 2%, and the combined outcome of mortality, reinfarction and stroke by 6%, with PCI relative to thrombolysis.3 The potential number of admissions because of STEMI were multiplied by these improvement percentages to estimate the number of deaths, nonfatal AMIs and strokes that could potentially be prevented with the addition of new PCI facilities.
Results
Geographic analysis of populations with timely access
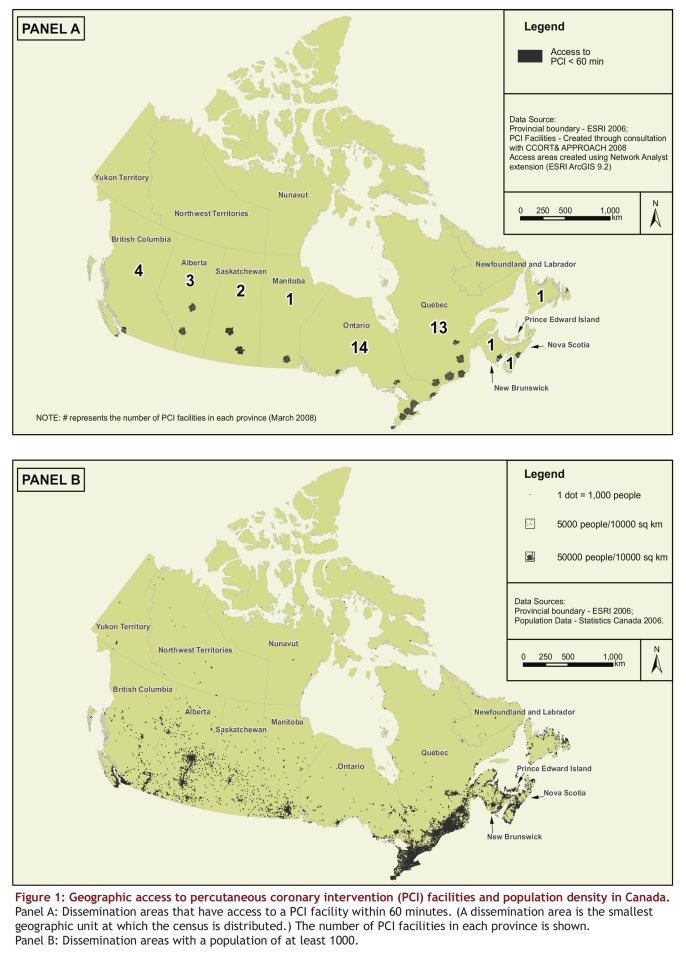
The total adult population aged 40 years and older in Canada was about 15.5 million based on 2006 Canadian census data. We identified 40 PCI facilities across Canada (Fig. 1A). The number of facilities varied by province. For example, Quebec and Ontario had 13 and 14 facilities respectively; all 3 territories and 1 province (Prince Edward Island) did not have any PCI facilities.
Figure 1.
Geographic access to percutaneous coronary intervention (PCI) facilities and population density in Canada.
Only a small proportion of the country’s geographic area was within 60 minutes of a PCI facility (Fig. 1A). Despite this, a reasonably large proportion of adults aged 40 years and older had access within this time. Figure 1B highlights the dissemination areas with a population of at least 1000. The population density was highest in the areas of Ontario and Quebec adjacent to the United States border. Other areas with high population density were on the west coast of British Columbia and in pockets of southern Alberta. These areas generally corresponded to the location of PCI facilities.
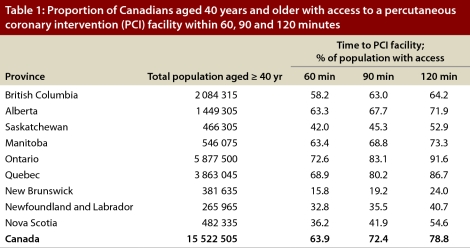
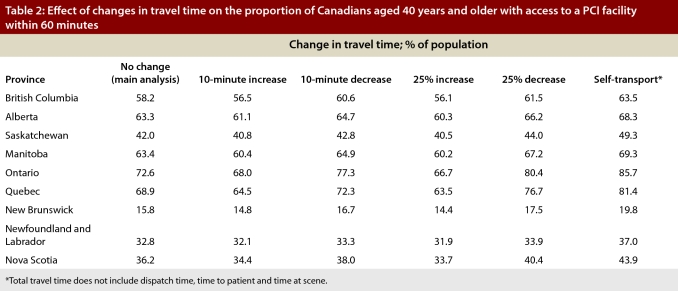
Overall, 63.9% of Canadians aged 40 years and older had access to a PCI facility within 60 minutes, 72.4% within 90 minutes and 78.8% within 120 minutes (Table 1). The proportion varied greatly by province. New Brunswick had the lowest level of access within 60 minutes (15.8%), and Ontario the highest (72.6%). There was an increase in the proportion across all provinces when 90- and 120-minute travel times were considered. When we confined the analysis to older groups, we found that 62.5% of those aged 50 years and older, 61.4% of those 60 and older, and 61.5% of those 70 and older had access to PCI within 60 minutes.
Table 1.
Proportion of Canadians aged 40 years and older with access to a percutaneous coronary intervention (PCI) facility within 60, 90 and 120 minutes
In the sensitivity analyses, changes in the travel time by either absolute or relative times altered the proportion of the population with 60-minute access by less than 5% on average in either direction (Table 2). In the model of patient self-transport, the population with 60-minute access increased by as much as 13% because of the removal of ambulance dispatch and patient loading times (see caveats in the Interpretation section).
Table 2.
Effect of changes in travel time on the proportion of Canadians aged 40 years and older with access to a PCI facility within 60 minutes
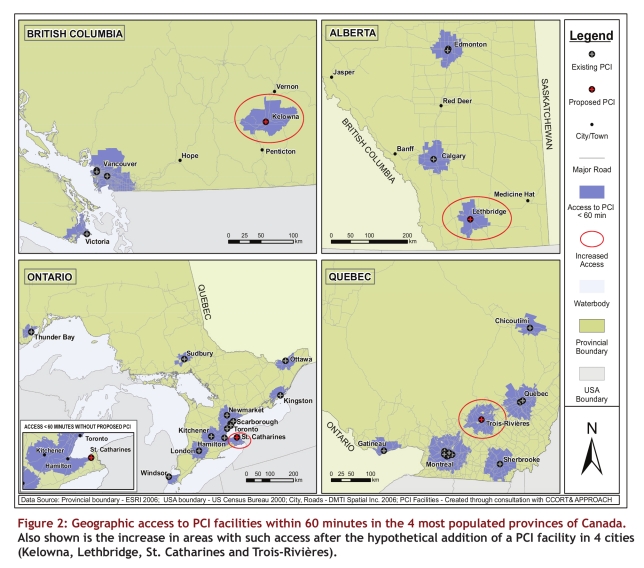
Hypothetical addition of new PCI facilities
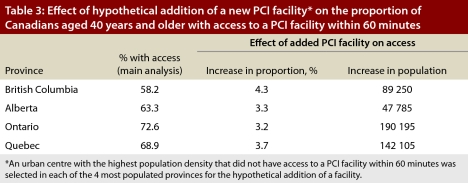
The following urban centres were selected for the hypothetical addition of a new PCI facility: Kelowna (British Columbia), Lethbridge (Alberta), St. Catharines (Ontario) and Trois-Rivières (Quebec). Our analyses showed that such additions would increase the proportion of the population with access to a PCI facility within 60 minutes by 3.2% to 4.3% depending on the province (Fig. 2 and Table 3). Overall, about 470 000 adults aged 40 and older would gain access to primary PCI in such a scenario. About 675 000 people 20 years of age and older would have access to these hypothetical facilities. Using these population numbers and the efficacy estimates of PCI relative to thrombolysis (as described in the Methods section), we estimated that about 17 deaths that would have occurred within 4-6 weeks of an AMI and 34 recurrent nonfatal myocardial infarctions or strokes could be avoided through the addition of these 4 hypothetical facilities.
Figure 2.
Geographic access to PCI facilities within 60 minutes in the 4 most populated provinces of Canada. Also shown is the increase in areas with such access after the hypothetical addition of a PCI facility in 4 cities (Kelowna, Lethbridge, St. Catharines and Trois-Rivières).
Table 3.
Effect of hypothetical addition of a new PCI facility on the proportion of Canadians aged 40 years and older with access to a PCI facility within 60 minutes
Interpretation
We found that 63.9% of Canadians aged 40 years and older had access to a PCI facility within 60 minutes. However, the level of access varied substantially by province. This proportion is lower than the nearly 80% of people aged 18 years and older in the United States with such access.21 Possible reasons for this difference include the much lower number of PCI facilities in Canada than in the United States (40 v. 1176) and differences in population density in the 2 countries. In Canada, there is about 1 PCI facility for every 595 000 adults (40 PCI facilities for 23.8 million adults 20 years of age and older); in the United States, there is about 1 PCI facility for every 176 000 adults (1176 facilities for 207.5 million adults aged 18 and older).21
The hypothetical addition of a new PCI facility in each of the 4 most populated provinces would increase the proportion of the population with timely access. In Ontario, for example, a province with relatively high population access because of a recent expansion of PCI facilities, the hypothetical addition of a new facility could provide additional access to about 190 000 adults aged 40 and older. The impact could be even greater if a new facility were added to a province with a low level of access. For example, in New Brunswick, increasing access to as few as 75 000 more adults aged 40 and oldercould increase the provincial proportion with access by nearly 15%. Other studies have also shown that adding facilities to currently underserved areas improves access to PCI.29
What is the potential impact of such new facilities on patient outcomes? Of deaths within 4-6 weeks of an AMI, we estimated that about 17 could be avoided through the hypothetical addition of these 4 facilities, along with 34 recurrent nonfatal myocardial infarctions or strokes. Such numbers, although not entirely negligible, might be viewed by some as indicating only a modest outcome benefit. Similarly, the increases in population coverage associated with the new facilities (3.2% to 4.3%, depending on the province) may also be viewed as modest. In fact, they could be perceived as arguments against the allocation of resources to create new facilities. However, in addition to the potential reduction in morbidity and mortality associated with acute STEMI care, there may be benefits to patients who present with other cardiovascular diseases in areas served by new facilities. Furthermore, a recent Canadian study showed that early PCI after fibrinolysis (transfer and PCI performed a few hours after fibrinolysis) was associated with significantly fewer ischemic complications than was standard treatment (STEMI patients remaining at their presenting hospital for at least 24 hours after fibrinolysis unless indications for rescue PCI were present).37 Such an approach to regional STEMI care with post-thrombolysis transfer could benefit from the existence of additional PCI facilities.
The above estimates and discussion should not lead to blind enthusiasm for the creation of new PCI facilities, however. There will always be a trade-off between equity and efficiency. Indeed, the logistics of adding new facilities are complex. Barriers such as lack of funding, lack of experienced PCI operators and lack of technical staff are some of the reasons why 24-hour PCI facilities do not exist in all hospitals with PCI facilities.11 Another consideration when locating a PCI facility is its distance to the nearest cardiac surgery facility. In our analysis of the hypothetical addition of PCI facilities, the travel time by ground to the nearest existing cardiac surgery facility varied across the 4 provinces, from about 45 minutes between St. Catharines and Hamilton in Ontario, to about 4 hours between Kelowna and Vancouver in British Columbia. Furthermore, regardless of how many PCI facilities are added, there will always be some inequity in access to primary PCI. Some Canadians with STEMI will not be able to access PCI simply because of the great geographic expanse and remoteness of certain areas of Canada. This is certainly true in the United States, where there are substantial numbers of Americans who do not have access to PCI within 60 minutes despite there being a far greater number of PCI facilities.
Our analysis of the hypothetical addition of new PCI facilities in 4 selected provinces is not intended to be comprehensive. It only demonstrates the possibility of increased geographic access with the addition of a new facility to areas with high population density that currently do not have access. We did not consider other locations within the 4 provinces or locations outside of these selected provinces that might also warrant consideration for new PCI facilities. Other important considerations when proposing the addition of new PCI facilities include the association between worse PCI outcomes and lower volume, the lack of on-site cardiac surgery, and the cost of creating, running and maintaining a PCI facility in relation to the number of patients with STEMI treated each year. Future analyses could focus on using the distance to the nearest cardiac surgery facility in combination with the possible volume of STEMI patients treated in order to locate hypothetical new PCI facilities. The redistribution of PCI services could also be analyzed to determine how population access is affected by hypothetically moving a service from an area where multiple facilities exist within short distances (e.g., within 10 km of each other) to areas where there are currently no facilities.
Although we focused on geographic access to PCI facilities, equity of access by socioeconomic status can also be considered. Across each of the zones with 60-minute access, there is a full spectrum of income levels represented. However, rural areas have lower levels of access than urban areas do because of the placement of PCI facilities in larger cities. Studies have shown that regional per capita employment incomes in Canada decrease when going from urban to rural areas38 and that there is a relation between socioeconomic levels and outcomes among patients with cardiac disease, with more favourable outcomes among those with higher income levels.39 Thus, there is clearly a complex interplay between socioeconomic status and geography.
Our findings can contribute to the development of STEMI care models. However, they do not in and of themselves constitute a care model. Building on the information presented here, individual centres, health regions and provinces need to decide whether the implementation of a regional STEMI care model is feasible. Considerations include operational hours for PCI facilities, local protocols for inter-hospital transfer and transfer for rescue PCI, balanced consideration of alternatives to fibrinolysis and the overall structure of regional emergency medical services.40 Examples of successful regional STEMI care models in Canada have been demonstrated and can provide guidance for the implementation of other models.14,16 Our findings will also contribute to the rational planning of fibrinolysis delivery. Indeed, there are many areas without timely access to PCI where fibrinolytic drugs are the only practical option for reperfusion.
Our study has limitations. First, we looked at geographic access to PCI facilities in terms of a best-case scenario, where all of the facilities provided primary PCI 24 hours a day, 7 days a week. However, there are PCI facilities in Canada that currently do not provide primary PCI, that do not operate on a 24/7 schedule or that do not accept STEMI patients from surrounding regional hospitals.12 New cardiac catheterization facilities in community settings usually do not offer immediate primary PCI; instead, they often start with diagnostic angiography before moving to elective low-risk PCI and then primary PCI. Also, there is an important relation between primary PCI volume and outcomes; new centres need to have sufficient primary PCI volumes to ensure quality.41,42
Second, we used pre-hospital travel times based on assumptions founded on emergency transport studies conducted in the United States. Travel times in the United States and Canada may differ; however, our sensitivity analyses in which we adjusted travel times by absolute and relative times did not change the proportion of the population with timely access greatly. Also, a previous study using different methods showed that the proportion of the population with access to a PCI facility within 90 minutes in Alberta was similar to the proportion in our study (69.6% and 68.7% respectively).43
Third, we focused on pre-hospital times. We did not consider in-hospital delays that can be important barriers to timely primary PCI. Also, although self-transport of STEMI patients may increase the proportion of patients with timely access to primary PCI, as was shown in our final sensitivity analysis, patients who drive themselves to a hospital may have longer in-hospital delays because of prolonged triage time.34 Because of that consideration, and other benefits of pre-hospital care, we certainly do not advocate self-transport to save pre-hospital time, despite our findings.
In summary, we found that over 60% of Canadians aged 40 years and older have access to a PCI facility within 60 minutes. Our study shows the potential utility of geographic information systems analysis to inform strategic decisions about the infrastructure of our health care system. Our findings provide a foundation of knowledge for care providers and decision-makers to explore approaches to developing regional STEMI care models to improve access to primary PCI.
Acknowledgments
The authors thank research members of the Canadian Cardiovascular Outcomes Research Team (CCORT) and the Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) for their comments on this study.
Biographies
Alka B Patel is a PhD student in the Department of Community Health Sciences at the University of Calgary, Calgary, Alberta, Canada.
Jack V Tu is a senior scientist and head of the Cardiovascular and Diagnostic Imaging Research Program at the Institute for Clinical Evaluative Sciences (ICES) and is attending physician in the Divisions of Cardiology (Schulich Heart Program) and General Internal Medicine at the Sunnybrook Health Sciences Centre, Toronto, Ontario.
Nigel M Waters is director of the Geographic Information Science Center of Excellence and professor of geography at George Mason University, Fairfax, Virginia, United States.
Dennis T Ko is a scientist at ICES, an interventional cardiologist at the Schulich Heart Centre, Sunnybrook Health Sciences Centre, and assistant professor of medicine at the University of Toronto, Toronto.
Mark J Eisenberg is an academic interventional cardiologist, a clinical epidemiologist and an associate professor of medicine at McGill University, Montréal, Quebec.
Thao Huynh is a clinical cardiologist and associate professor of medicine at the Montréal General Hospital and McGill University, Montréal.
Stéphane Rinfret is professor of medicine under grant at Laval University, a clinical and outcomes researcher at the Centre de recherche de l’Institut universitaire de cardiologie et de pneumologie de Québec (IUCPQ) and a clinical and interventional cardiologist in the Department of Cardiology at the IUCPQ (Quebec Heart and Lung Institute), Quebec City, Quebec.
Merril L Knudtson is professor of medicine at the University of Calgary and an interventional cardiologist at the Foothills Medical Centre, Calgary.
William A Ghali is a professor in the Centre for Health and Policy Studies, Department of Community Health Sciences, University of Calgary, and a general internist in the Department of Medicine, Foothills Medical Centre, Calgary.
Footnotes
Competing interests: The authors have no competing interests to declare. William Ghali is an associate editor of Open Medicine. He was not involved in reviewing the article or deciding on its acceptance for publication.
Contributors: All of the authors contributed to the conceptionand design of the study and to the interpretation of the data. Alka Patel acquired the data, performed the analysis and draftedthe manuscript. William Ghali and Nigel Waters provided supervision and oversight of all aspects of the project. All of the authors revised the article for importantintellectual content and approved the final version submittedfor publication.
Funding source: No specific funds were obtained for this study. Alka Patel is supported by a Canadian Institutes of Health Research (CIHR) Doctoral Research Award, a Canadian Cardiovascular Outcomes Research Team (CCORT) Travel Award funded through a CIHR Team Grant in Cardiovascular Outcomes Research and an Alberta Heritage Foundation for Medical Research Incentive Award. William Ghali and Jack Tu are supported by Government of Canada Research Chairs in Health Services Research. William Ghali is also supported by a Senior Health Scholar Award from the Alberta Heritage Foundation for Medical Research. Jack Tu is also supported by a Career Investigator Award from the Heart and Stroke Foundation of Ontario. Dennis Ko is supported by a Clinician-Scientist Award from the Heart and Stroke Foundation of Ontario.
References
- 1.Andersen Henning R, Nielsen Torsten T, Rasmussen Klaus, Thuesen Leif, Kelbaek Henning, Thayssen Per, Abildgaard Ulrik, Pedersen Flemming, Madsen Jan K, Grande Peer, Villadsen Anton B, Krusell Lars R, Haghfelt Torben, Lomholt Preben, Husted Steen E, Vigholt Else, Kjaergard Henrik K, Mortensen Leif Spange DANAMI-2 Investigators. A comparison of coronary angioplasty with fibrinolytic therapy in acute myocardial infarction. N Engl J Med. 2003;349(8):733–742. doi: 10.1056/NEJMoa025142. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=12930925&promo=ONFLNS19. [DOI] [PubMed] [Google Scholar]
- 2.Henriques J P S, Zijlstra F, van't Hof A W J, de Boer M-J, Dambrink J-H E, Gosselink A T M, Hoorntje J C A, Ottervanger J P, Suryapranata H. Primary percutaneous coronary intervention versus thrombolytic treatment: long term follow up according to infarct location. Heart. 2005 Apr 14;92(1):75–79. doi: 10.1136/hrt.2005.060152. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=15831596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Keeley Ellen C, Boura Judith A, Grines Cindy L. Primary angioplasty versus intravenous thrombolytic therapy for acute myocardial infarction: a quantitative review of 23 randomised trials. Lancet. 2003;361(9351):13–20. doi: 10.1016/S0140-6736(03)12113-7. [DOI] [PubMed] [Google Scholar]
- 4.Widimský P, Budesínský T, Vorác D, Groch L, Zelízko M, Aschermann M, Branny M, St'ásek J, Formánek P 'PRAGUE' Study Group Investigators. Long distance transport for primary angioplasty vs immediate thrombolysis in acute myocardial infarction. Final results of the randomized national multicentre trial – PRAGUE-2. Eur Heart J. 2003;24(1):94–104. doi: 10.1016/s0195-668x(02)00468-2. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=12559941. [DOI] [PubMed] [Google Scholar]
- 5.Carstensen Steen, Nelson Greg C I, Hansen Peter S, Macken Lewis, Irons Stephen, Flynn Michael, Kovoor Pramesh, Soo Hoo Soon Y, Ward Michael R, Rasmussen Helge H. Field triage to primary angioplasty combined with emergency department bypass reduces treatment delays and is associated with improved outcome. Eur Heart J. 2007 Aug 01;28(19):2313–2319. doi: 10.1093/eurheartj/ehm306. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=17670756. [DOI] [PubMed] [Google Scholar]
- 6.Nallamothu B, Fox K A A, Kennelly B M, Van de Werf F, Gore J M, Steg P G, Granger C B, Dabbous O H, Kline-Rogers E, Eagle K A GRACE Investigators. Relationship of treatment delays and mortality in patients undergoing fibrinolysis and primary percutaneous coronary intervention. The Global Registry of Acute Coronary Events. Heart. 2007 Jun 25;93(12):1552–1555. doi: 10.1136/hrt.2006.112847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Steg P G, Juliard J-M. Primary percutaneous coronary intervention in acute myocardial infarction: time, time, and time! Heart. 2005;91(8):993–994. doi: 10.1136/hrt.2004.050625. http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=16020578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Antman Elliott M, Hand Mary, Armstrong Paul W, Bates Eric R, Green Lee A, Halasyamani Lakshmi K, Hochman Judith S, Krumholz Harlan M, Lamas Gervasio A, Mullany Charles J, Pearle David L, Sloan Michael A, Smith Sidney C, Anbe Daniel T, Kushner Frederick G, Ornato Joseph P, Jacobs Alice K, Adams Cynthia D, Anderson Jeffrey L, Buller Christopher E, Creager Mark A, Ettinger Steven M, Halperin Jonathan L, Hunt Sharon A, Lytle Bruce W, Nishimura Rick, Page Richard L, Riegel Barbara, Tarkington Lynn G, Yancy Clyde W 2004 Writing Committee Members. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients With ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2007 Dec 10;117(2):296–329. doi: 10.1161/CIRCULATIONAHA.107.188209. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=18071078. [DOI] [PubMed] [Google Scholar]
- 9.Silber Sigmund, Albertsson Per, Avilés Francisco F, Camici Paolo G, Colombo Antonio, Hamm Christian, Jørgensen Erik, Marco Jean, Nordrehaug Jan-Erik, Ruzyllo Witold, Urban Philip, Stone Gregg W, Wijns William, Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart J. 2005 Mar 15;26(8):804–847. doi: 10.1093/eurheartj/ehi138. http://eurheartj.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=15769784. [DOI] [PubMed] [Google Scholar]
- 10.Welsh Robert C, Travers Andrew, Huynh Thao, Cantor Warren J, Canadian Cardiovascular Society Working Group. Canadian Cardiovascular Society Working Group: Providing a perspective on the 2007 focused update of the American College of Cardiology and American Heart Association 2004 guidelines for the management of ST elevation myocardial infarction. Can J Cardiol. 2009;25(1):25–32. doi: 10.1016/s0828-282x(09)70019-4. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=19148339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kristensen S D, Andersen H R, Thuesen L, Krusell L R, Bøtker H E, Lassen J F, Nielsen T T. Should patients with acute ST elevation MI be transferred for primary PCI? Heart. 2004;90(11):1358–1363. doi: 10.1136/hrt.2003.021881. http://heart.bmj.com/cgi/pmidlookup?view=long&pmid=15486148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ko Dennis T, Donovan Linda R, Huynh Thao, Rinfret Stéphane, So Derek Y, Love Michael P, Galbraith Diane, Tu Jack V, Canadian Cardiovascular Outcomes Research Team (CCORT. A survey of primary percutaneous coronary intervention for patients with ST segment elevation myocardial infarction in Canadian hospitals. Can J Cardiol. 2008;24(11):839–843. doi: 10.1016/s0828-282x(08)70192-2. http://www.pubmedcentral.nih.gov/articlerender.fcgi?tool=pubmed&pubmedid=18987757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacobs Alice K, Antman Elliott M, Ellrodt Gray, Faxon David P, Gregory Tammy, Mensah George A, Moyer Peter, Ornato Joseph, Peterson Eric D, Sadwin Larry, Smith Sidney C American Heart Association's Acute Myocardial Infarction Advisory Working Group. Recommendation to develop strategies to increase the number of ST-segment-elevation myocardial infarction patients with timely access to primary percutaneous coronary intervention. Circulation. 2006 Mar 28;113(17):2152–2163. doi: 10.1161/CIRCULATIONAHA.106.174477. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=16569790. [DOI] [PubMed] [Google Scholar]
- 14.Le May Michel R, So Derek Y, Dionne Richard, Glover Chris A, Froeschl Michael P V, Wells George A, Davies Richard F, Sherrard Heather L, Maloney Justin, Marquis Jean-François, O'Brien Edward R, Trickett John, Poirier Pierre, Ryan Sheila C, Ha Andrew, Joseph Phil G, Labinaz Marino. A citywide protocol for primary PCI in ST-segment elevation myocardial infarction. N Engl J Med. 2008;358(3):231–240. doi: 10.1056/NEJMoa073102. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=18199862&promo=ONFLNS19. [DOI] [PubMed] [Google Scholar]
- 15.Henry Timothy D, Sharkey Scott W, Burke M Nicholas, Chavez Ivan J, Graham Kevin J, Henry Christopher R, Lips Daniel L, Madison James D, Menssen Katie M, Mooney Michael R, Newell Marc C, Pedersen Wes R, Poulose Anil K, Traverse Jay H, Unger Barbara T, Wang Yale L, Larson David M. A regional system to provide timely access to percutaneous coronary intervention for ST-elevation myocardial infarction. Circulation. 2007 Aug 01;116(7):721–728. doi: 10.1161/CIRCULATIONAHA.107.694141. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=17673457. [DOI] [PubMed] [Google Scholar]
- 16.de Villiers Jacobus S, Anderson Todd, McMeekin James D, Leung Raymond C M, Traboulsi Mouhieddin Foothills Interventional Cardiology Service; Calgary STEMI QIHI group. Expedited transfer for primary percutaneous coronary intervention: a program evaluation. CMAJ. 2007;176(13):1833–1838. doi: 10.1503/cmaj.060902. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=17576980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ting Henry H, Rihal Charanjit S, Gersh Bernard J, Haro Luis H, Bjerke Christine M, Lennon Ryan J, Lim Choon-Chern, Bresnahan John F, Jaffe Allan S, Holmes David R, Bell Malcolm R. Regional systems of care to optimize timeliness of reperfusion therapy for ST-elevation myocardial infarction: the Mayo Clinic STEMI Protocol. Circulation. 2007 Aug 01;116(7):729–736. doi: 10.1161/CIRCULATIONAHA.107.699934. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=17673456. [DOI] [PubMed] [Google Scholar]
- 18.De Luca Assunta, Gabriele Stefania, Lauria Laura, Francia Carlo, Caminiti Alessandro, Tubaro Marco, Pillon Sergio, Pristipino Christian, Ammirati Fabrizio, Guasticchi Gabriella Gruppo di Lavoro del Progetto Cuore Sicuro. Implementation of an emergency clinical pathway for ST-elevation myocardial infarction in the Lazio Region: results of a pilot study. G Ital Cardiol. 2006;9(2):118–125. [PubMed] [Google Scholar]
- 19.National Infarct Angioplasty Project (NIAP) interim report. London (UK): Department of Health; 2008. http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_083061. [Google Scholar]
- 20.Chakrabarti Anjan, Krumholz Harlan M, Wang Yongfei, Rumsfeld John S, Nallamothu Brahmajee K National Cardiovascular Data Registry. Time-to-reperfusion in patients undergoing interhospital transfer for primary percutaneous coronary intervention in the U.S: an analysis of 2005 and 2006 data from the National Cardiovascular Data Registry. J Am Coll Cardiol. 2008;51(25):2442–2443. doi: 10.1016/j.jacc.2008.02.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nallamothu Brahmajee K, Bates Eric R, Wang Yongfei, Bradley Elizabeth H, Krumholz Harlan M. Driving times and distances to hospitals with percutaneous coronary intervention in the United States: implications for prehospital triage of patients with ST-elevation myocardial infarction. Circulation. 2006;113(9):1189–1195. doi: 10.1161/CIRCULATIONAHA.105.596346. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=16520425. [DOI] [PubMed] [Google Scholar]
- 22.Apparicio Philippe, Abdelmajid Mohamed, Riva Mylène, Shearmur Richard. Comparing alternative approaches to measuring the geographical accessibility of urban health services: Distance types and aggregation-error issues. Int J Health Geogr. 2008 Feb 18;7:7. doi: 10.1186/1476-072X-7-7. http://www.ij-healthgeographics.com/content/7//7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geographic units: dissemination area (DA) Ottawa: Statistics Canada; http://www12.statcan.ca/english/census01/Products/Reference/dict/geo021.htm. [Google Scholar]
- 24.Geocoding in ArcGIS. Redlands (CA): ESRI; 2004. [Google Scholar]
- 25.Hare TS, Barcus HR. Geographical accessibility and Kentucky's heart-related hospital services. Appl Geography. 2007;27:181–205. [Google Scholar]
- 26.Wang Lu. Immigration, ethnicity, and accessibility to culturally diverse family physicians. Health Place. 2006 Dec 15;13(3):656–671. doi: 10.1016/j.healthplace.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 27.Baumgardner Dennis J, Halsmer Sarah E, Steber Dale L, Shah Dharmen S, Mundt Marlon P. Does proximity to clinic affect immunization rates and blood pressure? Int J Psychiatry Med. 2006;36(2):199–209. doi: 10.2190/9N36-W446-194L-9KHW. [DOI] [PubMed] [Google Scholar]
- 28.Cinnamon Jonathan, Schuurman Nadine, Crooks Valorie A. A method to determine spatial access to specialized palliative care services using GIS. BMC Health Serv Res. 2008;8:140. doi: 10.1186/1472-6963-8-140. http://www.biomedcentral.com/1472-6963/8/140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pereira Augustine, Niggebrugge Aphrodite, Powles John, Kanka David, Lyratzopoulos Georgios. Potential generation of geographical inequities by the introduction of primary percutaneous coronary intervention for the management of ST segment elevation myocardial infarction. Int J Health Geogr. 2007 Sep 23;6:43–46. doi: 10.1186/1476-072X-6-43. http://www.ij-healthgeographics.com/content/6//43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tu Jack V, Khalid Laila, Donovan Linda R, Ko Dennis T Canadian Cardiovascular Outcomes Research Team / Canadian Cardiovascular Society Acute Myocardial Infarction Quality Indicator Panel. Indicators of quality of care for patients with acute myocardial infarction. CMAJ. 2008;179(9):909–915. doi: 10.1503/cmaj.080749. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=18936456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carr Brendan G, Caplan Joel M, Pryor John P, Branas Charles C. A meta-analysis of prehospital care times for trauma. Prehosp Emerg Care. 2006;10(2):198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 32.Branas Charles C. No time to spare: improving access to trauma care. LDI Issue Brief. 2005;11(1):1–4. [PubMed] [Google Scholar]
- 33.Branas Charles C, MacKenzie Ellen J, Williams Justin C, Schwab C William, Teter Harry M, Flanigan Marie C, Blatt Alan J, ReVelle Charles S. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633. doi: 10.1001/jama.293.21.2626. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=15928284. [DOI] [PubMed] [Google Scholar]
- 34.Canto John G, Zalenski Robert J, Ornato Joseph P, Rogers William J, Kiefe Catarina I, Magid David, Shlipak Michael G, Frederick Paul D, Lambrew Costas G, Littrell Katherine A, Barron Hal V National Registry of Myocardial Infarction 2 Investigators. Use of emergency medical services in acute myocardial infarction and subsequent quality of care: observations from the National Registry of Myocardial Infarction 2. Circulation. 2002;106(24):3018–3023. doi: 10.1161/01.cir.0000041246.20352.03. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=12473545. [DOI] [PubMed] [Google Scholar]
- 35.Hall RE, Tu JV. Hospitalization rates and length of stay for cardiovascular conditions in Canada, 1994 to 1999. Can J Cardiol. 2003;19:1123–1131. [PubMed] [Google Scholar]
- 36.Bradshaw Pamela J, Ko Dennis T, Newman Alice M, Donovan Linda R, Tu Jack V. Validation of the Thrombolysis In Myocardial Infarction (TIMI) risk index for predicting early mortality in a population-based cohort of STEMI and non-STEMI patients. Can J Cardiol. 2007;23(1):51–56. doi: 10.1016/s0828-282x(07)70213-1. http://www.pulsus.com/journals/abstract.jsp?sCurrPg=journal&jnlKy=1&atlKy=7003&isuKy=151&isArt=t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cantor Warren J, Fitchett David, Borgundvaag Bjug, Ducas John, Heffernan Michael, Cohen Eric A, Morrison Laurie J, Langer Anatoly, Dzavik Vladimir, Mehta Shamir R, Lazzam Charles, Schwartz Brian, Casanova Amparo, Goodman Shaun G TRANSFER-AMI Trial Investigators. Routine early angioplasty after fibrinolysis for acute myocardial infarction. N Engl J Med. 2009;360(26):2705–2718. doi: 10.1056/NEJMoa0808276. http://content.nejm.org/cgi/pmidlookup?view=short&pmid=19553646&promo=ONFLNS19. [DOI] [PubMed] [Google Scholar]
- 38.Beckstead D, Brown WM. Provincial income disparities through an urban–rural lens: evidence from the 2001 census. Ottawa: Statistics Canada; 2005. [Google Scholar]
- 39.Southern Danielle A, McLaren Lindsay, Hawe Penelope, Knudtson Merril L, Ghali William A APPROACH Investigators. Individual-level and neighborhood-level income measures: agreement and association with outcomes in a cardiac disease cohort. Med Care. 2005;43(11):1116–1122. doi: 10.1097/01.mlr.0000182517.57235.6d. [DOI] [PubMed] [Google Scholar]
- 40.Travers Andrew. Achieving optimal care for ST-segment elevation myocardial infarction in Canada. CMAJ. 2007;176(13):1843–1844. doi: 10.1503/cmaj.061567. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=17576982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McGrath P D, Wennberg D E, Dickens J D, Siewers A E, Lucas F L, Malenka D J, Kellett M A, Ryan T J. Relation between operator and hospital volume and outcomes following percutaneous coronary interventions in the era of the coronary stent. JAMA. 2000;284(24):3139–3144. doi: 10.1001/jama.284.24.3139. http://jama.ama-assn.org/cgi/pmidlookup?view=long&pmid=11135777. [DOI] [PubMed] [Google Scholar]
- 42.McNamara RL, Herrin J, Bradley EH. Hospital improvement in time to reperfusion in patients with acute myocardial infarction, 1999 to 2002. J Am Coll Cardiol. 2006;47:45–51. doi: 10.1016/j.jacc.2005.04.071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Patel Alka B, Waters Nigel M, Ghali William A. Determining geographic areas and populations with timely access to cardiac catheterization facilities for acute myocardial infarction care in Alberta, Canada. Int J Health Geogr. 2007 Oct 16;6:47. doi: 10.1186/1476-072X-6-47. http://www.ij-healthgeographics.com/content/6//47. [DOI] [PMC free article] [PubMed] [Google Scholar]