Abstract
Objective
Cardiovascular disease (CVD) is the leading cause of death in patients with serious mental illness (SMI) and in patients with Type 2 diabetes. Inadequate pharmacologic care for CVD may partially explain poor health outcomes in individuals with both conditions. We sought to identify patients in this group at greatest risk for suboptimal pharmacologic management.
Methods
Among individuals with Type 2 diabetes and SMI identified from Maryland Medicaid data, we evaluated patient and service utilization factors associated with the prescription of HMG-CoA reductase inhibitors (“statins”) for hyperlipidemia and angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) for chronic kidney disease, congestive heart failure, and hypertension.
Results
From 2001 to 2003, the annual prevalence of use of statins and ACE-inhibitors/ARBs ranged from 44–59%, with rates increasing each year. Being female, having certain cardiovascular conditions, and having a greater number of outpatient visits for diabetes increased the odds of receiving statins and ACE-inhibitors/ARBs. More frequent contact with the mental health system was associated with a lower likelihood of receipt of both medication classes; having a substance use disorder was associated with reduced use of statins. African-Americans were less likely than Caucasians to receive statins, but more likely to receive prescriptions for ACE-inhibitors/ARBs.
Conclusions
Although use of cardioprotective medications in individuals with Type 2 diabetes and SMI increased over the study period, a considerable proportion of patients remained inadequately managed despite their considerable cardiac risk. Further study should focus on observed racial variations and strategies to increase the capacity of mental health contacts to improve prescribing of these agents.
Keywords: Diabetes, serious mental illness, Medicaid database analysis
1. Introduction
Individuals with schizophrenia and other serious mental illnesses (SMI) have a mortality rate at least two times as high as those without SMI, with the excess mortality largely attributed to higher rates of death from cardiovascular disease (CVD) (Brown et al., 2000; Colton and Manderscheid, 2006; Osby et al., 2000). Consistent with this observation are findings of significantly elevated ten-year coronary heart disease risk in individuals with SMI (Goff et al., 2005), which is likely a consequence of this population’s high rates of Type 2 diabetes (Dixon et al., 2000), metabolic syndrome (Kreyenbuhl et al., 2006; McEvoy et al., 2005), and other cardiovascular risk factors, such as obesity (Daumit et al., 2003), physical inactivity (Daumit et al., 2005), poor nutrition (McCreadie, 2003), and cigarette smoking (de Leon et al., 1995).
The increased prevalence of Type 2 diabetes in individuals with SMI has gained attention due to reports of newer antipsychotic medications that promote weight gain, hyperglycemia, and hyperlipidemia (Newcomer, 2005), and which may exacerbate the symptoms of diabetes and hasten its long-term cardiovascular complications. Type 2 diabetes is associated with a 2–4 fold increased risk for major cardiovascular events and is considered a coronary heart disease ‘risk equivalent’ that confers a level of risk equal to that in patients with pre-existing cardiovascular disease (CVD) (NCEP, 2001). However, a large body of evidence suggests that control of cholesterol levels and blood pressure leads to fewer cardiovascular events and reduced mortality in patients with Type 2 diabetes (ADA, 2007). To achieve these outcomes, the American Diabetes Association (ADA) recommends the use of cholesterol-lowering HMG-CoA reductase inhibitors (statins) as first-line treatments for hyperlipidemia in patients with Type 2 diabetes (ADA, 2007). The ADA also recommends that diabetes patients with hypertension or evidence of renal disease receive angiotensin converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), which improve cardiovascular outcomes and reduce the progression to diabetic nephropathy (ADA, 2007).
Emerging evidence suggests that recognition and management of cardiac risk in individuals with SMI in general (Nasrallah et al., 2006), and in those with diabetes specifically, (Kreyenbuhl et al., 2006; Weiss et al., 2006), is problematic. This under-appreciation of risk may contribute to the high rates of cardiovascular morbidity and mortality and contrasts with some recent progress in achieving relatively adequate glycemic control in these patients (Dixon et al., 2004; Krein et al., 2006; Weiss et al., 2006). Previous reports have demonstrated that few persons with SMI and diabetes are achieving ADA recommended goals for cholesterol (Frayne et al., 2005; Kreyenbuhl et al., 2006; Weiss et al., 2006) or blood pressure (Kreyenbuhl et al., 2006; Weiss et al., 2006), which corresponds with reports of low rates of screening for cardiovascular risk factors, particularly for hyperlipidemia (Frayne et al., 2005; Goldberg et al., 2007; Krein et al., 2006). Further, previous cross-sectional studies suggest that statins and ACE-inhibitors/ARBs are used infrequently in patients with SMI and diabetes (Kreyenbuhl et al., 2006; Weiss et al., 2006) who may reap particular benefits from these treatments. This is the first study to extend this earlier work by using a population-based design to examine the prescribing of statins and ACE-inhibitors/ARBs over 3 years in a large sample of Medicaid recipients with psychotic disorders and Type 2 diabetes, with the goal of identifying those patients not receiving care consistent with expert consensus panel guidelines for diabetes, which may place them at high risk for adverse cardiovascular outcomes.
2. Methods
2.1 Data source
This study used enrollment files and administrative encounter data consisting of records of adjudicated claims for health services and treatments provided to Maryland Medicaid enrollees who received at least one prescription for any antipsychotic medication or selected anti-manic medications (carbamazepine, divalproex sodium/valproic acid, lamotrigine, lithium) between 2001 and 2003. Enrollment histories, demographic characteristics, diagnoses, use of inpatient and outpatient health services, and outpatient prescriptions dispensed to individuals enrolled in both the fee-for-service and managed care portions of the program were available. The study was reviewed by the Institutional Review Boards of the University of Maryland School of Medicine and the Maryland Department of Health and Mental Hygiene and qualified as exempt research.
2.2 Study sample
Among 82 980 individuals who received at least one prescription for an antipsychotic or anti-manic medication between 2001 and 2003 and who had valid enrollment information, we identified 40 992 (49%) who were continuously enrolled in Maryland Medicaid throughout the study period (2001–2003). We used ICD-9-CM diagnostic codes to identify all patients with psychotic disorders (schizophrenia/schizoaffective disorder (295.0–4, 295.6–9); affective psychosis (296.0–1, 296.4–8); other psychotic disorders (297.0–3, 297.8–9, 298.0–4, 298.8–9)). Diagnosis was assigned by identifying the most prevalent ICD-9CM code for each patient. Exclusion of 3498 persons less than 18 years of age and 295 with missing information on race left 20 363 individuals in the study.
The final study cohort included individuals with concurrent diagnoses of Type 2 diabetes, identified as those who had at least 2 inpatient or outpatient records with diagnostic codes of 250.x0 or 295.x2, 357.2, 362.0, or 366.41 (Miller et al., 2004) during the study period. In order to increase the precision of case identification for Type 2 diabetes, we excluded 1129 persons who either only had records with diagnostic codes of 250.x1 or 250.x3 (who may have had Type 1 diabetes) or who only had one or more prescriptions for hypoglycemic medications. Due to small sample sizes, we also excluded 103 persons of Asian, Hispanic, and Native American descent, which resulted in a final sample of 3,265 individuals (16%) with a diagnosis of Type 2 diabetes.
2.3 Analytic Plan
We reviewed pharmacy data to identify prescriptions for cholesterol-lowering 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase inhibitors (statins), angiotensin converting enzyme (ACE) inhibitors, or angiotensin receptor blocking (ARB) agents during the 3-year study period. We examined the prescribing of ACE-inhibitors/ARBs in the subgroup of patients with one or more ADA-recommended indications (chronic kidney disease or hypertension), as well as in patients with congestive heart failure, for whom treatment is indicated in product labeling. Similarly, we examined the prescribing of statins in the subgroup of patients with hyperlipidemia, for whom these agents are recommended as first-line treatment by the ADA. For comparison purposes, we also described the use of non-statin cholesterol lowering agents (bile acid sequestrants, ezetimibe, fibric acid derivatives, and niacin) in this subgroup.
We used descriptive statistics to characterize the study sample, whether patients in the subgroups described above received one or more prescriptions for statins or ACE-inhibitors/ARBs during each of the 3 years of the study period, and the total duration of treatment with statins and ACE-inhibitors/ARBs between 2001 and 2003. We constructed dichotomous measures indicating whether each individual did or did not receive one or more prescriptions for statins and ACE-inhibitors/ARBs at any point during the study period, and conducted separate multiple logistic regression analyses to assess the relationship between receipt of the medications and patient demographic characteristics (age, gender, and race (African-American vs. Caucasian). We also evaluated the effect of several cardiovascular conditions that may have influenced prescribing decisions. We used ICD-9-CM diagnostic codes to identify cerebrovascular disease (ICD-9-CM 433–438), chronic kidney disease (250.4, 403, 404.x2, 404.x3, 580–583, 585, 586–588, 791.0), congestive heart failure (402.x1, 404.x1, 404.x3, 425, 428), coronary artery disease (410–414), hyperlipidemia (272.0–272.4), and hypertension (401–405) during the study period. (Hyperlipidemia was not evaluated in the analysis of statins since everyone in the subgroup studied had this diagnosis.) We also assessed the effect of use of insulin, whether the patient had a diabetes-related hospitalization, and the number of diabetes-related outpatient visits during the study period on receipt of statins and ACE-inhibitors/ARBs. In addition, we included in all analyses the type of psychotic disorder, the presence of a substance use disorder (ICD-9-CM 291–292, 303–305), the number of outpatient mental health/substance abuse visits, and whether the patient had a psychiatric/substance use disorder hospitalization during the study period. Due to the skewed nature of the number of outpatient diabetes-related and mental health/substance abuse visits, we categorized these data according to quartiles. All study analyses were completed using SAS, version 9.1.3.
3. Results
3.1 Characteristics of the Sample
The mean age of the study sample with a psychotic disorder and Type 2 diabetes (n=3265) was 52 (± 15) years, 67% were female, and 55% were African-American. Diagnoses of concurrent cardiovascular conditions were common, with hypertension (80%) and hyperlipidemia (55%) occurring most frequently. Ten percent of patients had a diabetes-related hospitalization and 30% were prescribed insulin. The 75% of patients with at least one outpatient visit for diabetes had a mean (± S.D.) of 8 (±7) visits during the study period.
Over half (55%) of patients had schizophrenia or schizoaffective disorder, 27% had an affective psychosis, and 18% had another psychotic disorder. Ten percent had concurrent substance use disorders and 30% had been hospitalized at least once for their psychiatric or substance use disorder between 2001 and 2003. The 83% of patients with at least one outpatient visit for their psychiatric or substance use condition had a mean (± S.D.) of 45 (± 57) outpatient visits over the study period.
3.2 Prevalence and Correlates of Statin Use
In the subgroup of 1792 individuals (55%) with a diagnosis of hyperlipidemia, 44%, 52% and 59% of these patients received one or more prescriptions for a statin in 2001, 2002, and 2003, respectively, (Figure 1). Sixty-seven percent of patients received at least one prescription for a statin at any point in the 3-year study period and 37% received statins in all 3 years. The median total duration of statin use in patients with hyperlipidemia in the study period was 235 days (mean ± S.D.: 356 ± 368 days). Seventeen percent (n=307) of patients with hyperlipidemia received one or more prescriptions for non-statin cholesterol lowering medications in 2001–2003, with rates of prescribing ranging from 9–12% in each individual study year.
Figure 1.
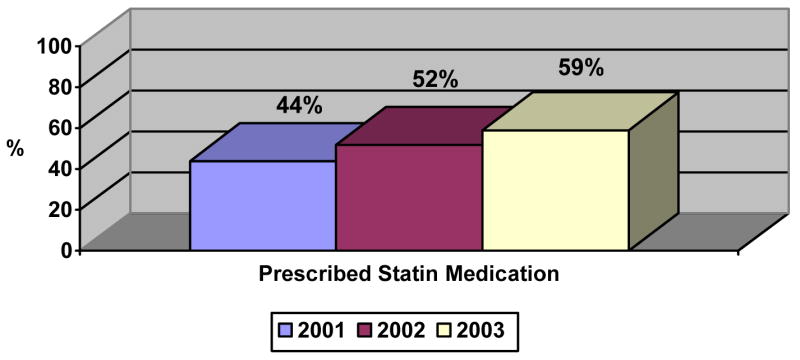
Prescription of statin medications for hyperlipidemia in individuals with psychotic disorders and Type 2 diabetes, 2001–2003 (n=1792).
Table 1 shows the results of the multivariable logistic regression analysis of statin prescribing. Whereas older patients and females had an increased likelihood of receiving statins, African-Americans were 30% less likely than Caucasians to be prescribed these agents. Patients with diagnoses of coronary artery disease or hypertension were more likely to be prescribed statins, and the odds of receiving these agents increased with increasing numbers of diabetes-related outpatient visits. Individuals with substance use disorders were almost one-third less likely than those without these conditions to receive statins.
Table 1.
Association of patient demographic and clinical characteristics to use of statin medications for hyperlipidemia in individuals with psychotic disorders and Type 2 diabetes (n=1792).
| Prescribed statin | Multivariable Statistic | |||||
|---|---|---|---|---|---|---|
| Characteristic | N | n | % | AORa | 95% CI | p value |
| Demographic characteristics | ||||||
| Age | ||||||
| ≤ 55 years | 1229 | 780 | 64% | Reference | ||
| >55 years | 563 | 424 | 75% | 1.43 | 1.10–1.86 | < 0.01 |
| Gender | ||||||
| Male | 599 | 374 | 62% | Reference | ||
| Female | 1193 | 830 | 70% | 1.28 | 1.03–1.60 | 0.03 |
| Race | ||||||
| Caucasian | 921 | 643 | 70% | Reference | ||
| African-American | 871 | 561 | 64% | 0.70 | 0.57–0.87 | < 0.01 |
| Diabetes-related characteristics and treatments | ||||||
| Co-occurring medical condition diagnoses | ||||||
| Cerebrovascular disease | ||||||
| No | 1360 | 894 | 66% | Reference | ||
| Yes | 432 | 310 | 72% | 0.98 | 0.74–1.29 | 0.86 |
| Chronic kidney disease | ||||||
| No | 1488 | 992 | 67% | Reference | ||
| Yes | 304 | 212 | 70% | 0.97 | 0.73–1.30 | 0.86 |
| Congestive heart failure | ||||||
| No | 1366 | 901 | 66% | Reference | ||
| Yes | 426 | 303 | 71% | 0.82 | 0.62–1.10 | 0.18 |
| Coronary artery disease | ||||||
| No | 1128 | 705 | 63% | Reference | ||
| Yes | 664 | 499 | 75% | 1.75 | 1.37–2.25 | < 0.01 |
| Hypertension | ||||||
| No | 275 | 152 | 55% | Reference | ||
| Yes | 1517 | 1052 | 69% | 1.53 | 1.15–2.03 | < 0.01 |
| Prescribed insulin | ||||||
| No | 1334 | 874 | 66% | Reference | ||
| Yes | 458 | 330 | 72% | 1.23 | 0.94–1.60 | 0.13 |
| Number of outpatient diabetes visits in study periodb | ||||||
| 0–2 | 563 | 339 | 60% | Reference | ||
| 3–6 | 447 | 320 | 72% | 1.79 | 1.35–2.36 | < 0.01 |
| 7–10 | 354 | 236 | 67% | 1.40 | 1.05–1.87 | 0.02 |
| ≥ 11 | 428 | 309 | 72% | 1.71 | 1.28–2.29 | < 0.01 |
| Any diabetes-related hospitalization in study period | ||||||
| No | 1642 | 1105 | 67% | Reference | ||
| Yes | 150 | 99 | 66% | 0.80 | 0.54–1.17 | 0.24 |
| Mental health characteristics and treatments | ||||||
| Psychotic disorder diagnosis | ||||||
| Schizophrenia/schizoaffective disorder | 1007 | 678 | 67% | Reference | ||
| Affective psychosis | 519 | 340 | 66% | 0.79 | 0.62–1.01 | 0.06 |
| Other psychotic disorder | 266 | 186 | 70% | 0.86 | 0.62–1.20 | 0.37 |
| Substance abuse diagnosis | ||||||
| No | 1653 | 1127 | 68% | Reference | ||
| Yes | 139 | 77 | 55% | 0.66 | 0.46–0.97 | 0.03 |
| Number of outpatient mental health visits in study periodb | ||||||
| 0–7 | 452 | 313 | 69% | Reference | ||
| 8–26 | 452 | 314 | 69% | 0.95 | 0.70–1.29 | 0.76 |
| 27–57 | 448 | 303 | 68% | 0.92 | 0.67–1.26 | 0.60 |
| ≥ 58 | 440 | 274 | 62% | 0.77 | 0.56–1.06 | 0.10 |
| Any psychiatric/substance abuse hospitalization in study period | ||||||
| No | 1257 | 855 | 68% | Reference | ||
| Yes | 535 | 349 | 65% | 1.02 | 0.81–1.28 | 0.89 |
Adjusted odds ratio, controlling for each variable listed in the first column of the table.
Categorized by quartiles.
3.3 Prevalence and Correlates of ACE-inhibitor/ARB Use
We evaluated the prescribing of ACE-inhibitors/ARBs in the subgroup of 2694 patients (83%) with diagnoses of chronic kidney disease, congestive heart failure, or hypertension. In each of the 3 study years, 46%, 54%, and 59% of patients received one or more prescriptions for an ACE-inhibitor or an ARB (Figure 2). A total of 69% of patients received these agents at least once during the study period and 37% received them in each study year. The median total duration of ACE-inhibitor/ARB use in the study period was 239 days (mean ± S.D.: 360 ± 366 days).
Figure 2.
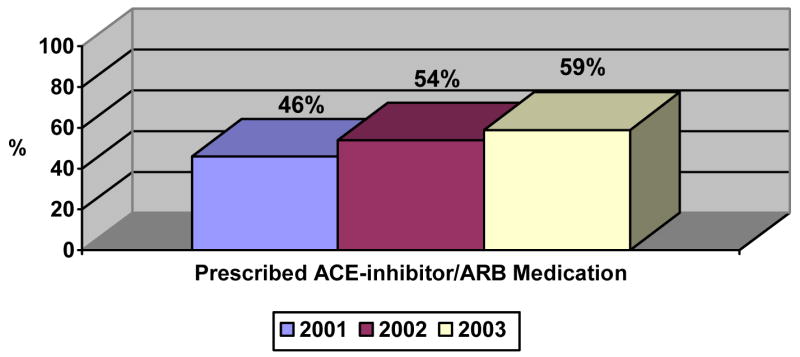
Prescription of ACE-inhibitors/ARBs for hypertension, congestive heart failure, or chronic kidney disease in individuals with psychotic disorders and Type 2 diabetes, 2001–2003 (n=2694).
Table 2 presents the multivariable analyses of the prescription of ACE-inhibitors or ARBs. Being female or African-American was associated with an increased likelihood of receiving an ACE-inhibitor or ARB. The presence of chronic kidney disease, congestive heart failure, hyperlipidemia, or hypertension was also associated with increased odds of receiving these agents. The likelihood of receiving the medications was higher in patients prescribed insulin and the odds also increased with greater numbers of diabetes-related outpatient visits. Patients with the greatest numbers of outpatient mental health or substance use visits had a lower likelihood of receipt of ACE-inhibitors/ARBs.
Table 2.
Association of patient demographic and clinical characteristics to use of ACE-inhibitors/ARBs for hypertension, congestive heart failure, or chronic kidney disease in individuals with psychotic disorders and Type 2 diabetes (n=2,694).
| Prescribed ACE-I/ARB | Multivariable Statistic | |||||
|---|---|---|---|---|---|---|
| Characteristic | N | n | % | AORa | 95% CI | p value |
| Demographic characteristics | ||||||
| Age | ||||||
| ≤ 55 years | 1614 | 1103 | 68% | Reference | ||
| >55 years | 1080 | 746 | 69% | 0.88 | 0.71–1.09 | 0.23 |
| Gender | ||||||
| Male | 870 | 563 | 65% | Reference | ||
| Female | 1824 | 1,286 | 71% | 1.26 | 1.05–1.52 | 0.01 |
| Race | ||||||
| Caucasian | 1159 | 761 | 66% | Reference | ||
| African-American | 1535 | 1088 | 71% | 1.28 | 1.07–1.53 | < 0.01 |
| Diabetes-related characteristics and treatments | ||||||
| Co-occurring medical condition diagnoses | ||||||
| Cerebrovascular disease | ||||||
| No | 1902 | 1273 | 67% | Reference | ||
| Yes | 792 | 576 | 73% | 1.10 | 0.88–1.37 | 0.40 |
| Chronic kidney disease | ||||||
| No | 2123 | 1411 | 67% | Reference | ||
| Yes | 571 | 438 | 77% | 1.64 | 1.30–2.08 | < 0.01 |
| Congestive heart failure | ||||||
| No | 1855 | 1212 | 65% | Reference | ||
| Yes | 839 | 637 | 76% | 1.72 | 1.38–2.15 | < 0.01 |
| Coronary artery disease | ||||||
| No | 1646 | 1079 | 66% | Reference | ||
| Yes | 1048 | 770 | 73% | 1.13 | 0.93–1.38 | 0.23 |
| Hyperlipidemia | ||||||
| No | 1157 | 746 | 64% | Reference | ||
| Yes | 1537 | 1103 | 72% | 1.28 | 1.06–1.54 | 0.01 |
| Hypertension | ||||||
| No | 84 | 30 | 36% | Reference | ||
| Yes | 2610 | 1819 | 70% | 4.80 | 2.96–7.77 | < 0.01 |
| Prescribed insulin | ||||||
| No | 1842 | 1218 | 66% | Reference | ||
| Yes | 852 | 631 | 74% | 1.25 | 1.01–1.53 | 0.04 |
| Number of outpatient diabetes visits in study periodb | ||||||
| 0–1 | 897 | 561 | 63% | Reference | ||
| 2–4 | 515 | 341 | 66% | 1.21 | 0.95–1.55 | 0.13 |
| 5–9 | 646 | 468 | 72% | 1.61 | 1.27–2.05 | < 0.01 |
| ≥ 10 | 636 | 479 | 75% | 1.79 | 1.39–2.31 | < 0.01 |
| Any diabetes-related hospitalization in study period | ||||||
| No | 2410 | 1642 | 68% | Reference | ||
| Yes | 284 | 207 | 73% | 0.99 | 0.73–1.34 | 0.96 |
| Mental health characteristics and treatments | ||||||
| Psychotic disorder diagnosis | ||||||
| Schizophrenia/schizoaffective disorder | 1454 | 989 | 68% | Reference | ||
| Affective psychosis | 736 | 518 | 70% | 1.07 | 0.87–1.32 | 0.51 |
| Other psychotic disorder | 504 | 342 | 68% | 0.79 | 0.62–1.02 | 0.08 |
| Substance abuse diagnosis | ||||||
| No | 258 | 167 | 65% | Reference | ||
| Yes | 2436 | 1682 | 69% | 0.86 | 0.64–1.16 | 0.33 |
| Number of outpatient mental health visits in study periodb | ||||||
| 0–2 | 701 | 474 | 68% | Reference | ||
| 3–17 | 648 | 464 | 72% | 1.07 | 0.83–1.39 | 0.59 |
| 18–44 | 674 | 487 | 72% | 1.09 | 0.83–1.42 | 0.55 |
| ≥ 45 | 671 | 424 | 63% | 0.75 | 0.56–0.99 | 0.04 |
| Any psychiatric/substance abuse hospitalization in study period | ||||||
| No | 1892 | 1306 | 69% | Reference | ||
| Yes | 802 | 543 | 68% | 0.91 | 0.75–1.11 | 0.34 |
Adjusted odds ratio, controlling for each variable listed in the first column of the table.
Categorized by quartiles.
4. Discussion
This study represents one of the few investigations of the prescription of two classes of medications shown to be beneficial in reducing diabetes-related cardiovascular morbidity and mortality, statins and ACE-inhibitors/ARBs, among persons with both Type 2 diabetes and SMI. Among patients with clear indications for treatment - for whom the benefits are greatest and for whom such therapy is universally recommended – nearly a third were not prescribed these agents over 3 years of opportunities for prescribing, with approximately 40–50% untreated in any single year. Even among those who received the medications, the average duration of therapy did not reach half of the study period, despite patients’ continuous enrollment in Medicaid during the 3 years studied.
Our 3-year observation period and population-based sampling design extend the few limited investigations of the prescribing of cardioprotective medications in individuals with SMI and diabetes. A cross-sectional study by Weiss and colleagues (2006) conducted in 5 internal medicine clinics found that approximately half of individuals with SMI and diabetes who were also diagnosed with hyperlipidemia received statins, which is consistent with our findings. Weiss et al., (2006) also found that approximately half of all SMI patients with diabetes in their sample received ACE-inhibitors/ARBs. The somewhat higher rates of use of ACE-inhibitors/ARBs in our sample (46–59% in any single study year; 69% across 3 years) likely reflects our evaluation of prescribing only among patients with clear indications for treatment (chronic kidney disease, congestive heart failure, hypertension) as specified in ADA recommendations at the time of the study (2001–2003).
Since more recent studies have demonstrated cardiovascular benefits of these agents regardless of baseline lipid levels (for statins) and their blood-pressure lowering effects (for ACE-inhibitors/ARBs), current ADA guidelines and other experts support broader empiric use of these agents in patients with adverse cardiac risk profiles (Hayward et al., 2006; Rosen, 2006), which would likely include many patients with SMI and diabetes. Our finding of year-over-year improvements in prescribing of both classes of medications is promising. More recent data to determine whether guideline concordant care continued to increase in these vulnerable patients should be examined.
Although our data suggest that treatment with statins and ACE-inhibitors/ARBs in persons with diabetes and psychotic disorders was incomplete, we cannot assert relative underuse without a non-mentally ill comparison sample. However, our current findings are generally consistent with those reported in several large studies of the general population with Type 2 diabetes conducted during the same time period (~40–75%) (Cooke and Fatodu, 2006; Grant et al., 2005; Nau and Mallya, 2005; Nau et al., 2004; Rosen et al., 2004; Rosen, 2006; Safford et al., 2003; Winkelmayer et al., 2005), including a recent study of beneficiaries of a Maryland Medicaid managed care organization (Cooke and Fatodu, 2006) reporting that 54% of diabetes patients were prescribed ACE-inhibitors/ARBs between 2001–2002.
A major focus and strength of our investigation was the identification of subgroups of individuals with SMI and diabetes at highest risk for adverse cardiovascular outcomes to whom quality improvement efforts should be targeted. Consistent with findings in studies of the general population with Type 2 diabetes (Safford et al., 2003; Sequist et al., 2006), we found that African-Americans in our sample were less likely than Caucasians to receive cholesterol-lowering statin medications. This is particularly concerning as African-Americans experience higher rates of Type 2 diabetes and its complications (Egede and Dagogo-Jack, 2005).
In contrast, we observed that African-Americans in our sample were more likely than Caucasians to be prescribed an ACE-inhibitor/ARB. Our finding differs from a study in the general population that found no disparities in the prescribing of these agents by race (Rosen et al., 2004). The increased prescription of ACE-inhibitor/ARBs in African Americans is reassuring since these patients are at higher risk for diabetes-related end-stage renal disease, which can be significantly delayed by treatment with ACE-inhibitors/ARBs. Despite earlier studies that suggested that African-Americans did not achieve the same degree of blood pressure lowering with ACE-inhibitor monotherapy as did Caucasian patients (Douglas et al., 2003), guidelines available at the time of this study for the treatment of hypertension in African-Americans (Douglas et al., 2003) considered ACE-inhibitors/ARBs first-line treatments. It is reassuring that our findings suggest that prescribers were aware of these guidelines.
While few would suggest that psychiatrists should treat co-occurring medical conditions in patients with SMI, virtually all would agree that psychiatrists have a responsibility for monitoring and facilitating care received by their patients, particularly when psychiatric treatments may cause or worsen medical conditions (Dixon et al., 2007). In this study, we found that greater numbers of contacts with the mental health system were associated with a lower likelihood of prescription of preventive cardiovascular treatments in individuals with SMI. These findings should not be construed to indicate that contact with mental health providers is a hindrance to receipt of cardioprotective therapies; a more plausible explanation is that frequent contact with the mental health system is a sign of patients’ psychiatric instability, with stabilization of psychiatric symptoms taking priority over management of ancillary medical concerns. If psychiatric instability is driving the increased mental health visits, such instability could also influence the treatment decisions of diabetes care providers who may be uncomfortable with substance abuse or psychosis or hesitant to further complicate an existing regimen of multiple psychotropic and somatic medications. In these instances, efforts to establish relationships between mental health and somatic providers may be integral to the provision of the highest quality diabetes care. In addition, we observed that prescribing of both medication classes was associated with more frequent contact with diabetes providers. As such, another avenue for optimizing cardiac health in SMI patients could involve mental health clinicians encouraging their patients’ regular attendance at outpatient visits with their diabetes providers.
Major strengths of this study included the administrative data source which enabled us to examine prescribing of cardioprotective medications over a three-year period in a large sample of individuals with SMI and diabetes. These strengths must be tempered by several limitations. Because our study design relied on case identification based on treatment records, potentially high rates of undiagnosed cases of metabolic disturbances were not captured in our analyses. Future studies that combine population-based screening studies with drug and service utilization data are needed to produce a more complete picture of the management of cardiac risk in diabetes patients with SMI. Such studies could also provide information on important risk factors for CHD, including clinical indicators (e.g., cholesterol levels), obesity, and smoking status, which were not available in our health services encounter data. We also were not able to ascertain whether antipsychotic-induced elevated liver enzymes (Garcia-Unzueta et al., 2003) or other liver disorders such as hepatitis that affect many people with SMI (Essock et al., 2003) influenced the prescribing of statins in our study. Finally, although our findings suggest that a lack of guideline concordant care regarding use of cardioprotective medications may contribute, in part, to the increased cardiovascular morbidity and mortality observed in SMI patients, more work is required to elucidate the direct mechanisms leading to poor health outcomes in this population.
More research is also needed to better understand how prescription decisions are made by primary care and diabetes specialty care providers treating patients with serious co-occurring medical and psychiatric disorders. While the limits of responsibility of the mental health system for management of diabetes and prevention of CVD are somewhat uncertain, our findings suggest opportunities for optimizing care, perhaps by building or strengthening relationships between mental health and somatic medical care providers.
Acknowledgments
The authors thank the Maryland Department of Health and Mental Hygiene for granting access to the administrative data used in this study. The authors also acknowledge C. Daniel Mullins, Ph.D. and the staff of Pharmaceutical Research Computing of the University of Maryland School of Pharmacy for their assistance with data acquisition and analysis. We also thank LiJuan Fang, M.S. for her assistance with data analyses and are grateful to Anthony F. Lehman, M.D., M.S.P.H. and Deanna L. Kelly, Pharm.D., BCCP for their helpful comments on the paper.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Diabetes Association. Standards of medical care in diabetes. Diabetes Care. 2007;30(Suppl 1):S4–S41. doi: 10.2337/dc07-S004. [DOI] [PubMed] [Google Scholar]
- Brown S, Inskip H, Barraclough B. Causes of the excess mortality of schizophrenia. Br J Psychiatry. 2000;177(3):212–217. doi: 10.1192/bjp.177.3.212. [DOI] [PubMed] [Google Scholar]
- Colton CW, Manderscheid RW. Congruencies in increased mortality rates, years of potential life lost, and causes of death among public mental health clients in eight states. [Accessed: October 30, 2007];Prev Chronic Dis. 2006 [serial online] Available from: URL: http://www.cdc.gov/pcd/issues/2006/apr/05_0180.htm. [PMC free article] [PubMed]
- Cooke CE, Fatodu H. Physician conformity and patient adherence to ACE inhibitors and ARBs in patients with diabetes, with and without renal disease and hypertension, in a medicaid managed care organization. J Manag Care Pharm. 2006;12(8):649–655. doi: 10.18553/jmcp.2006.12.8.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daumit GL, Clark JM, Steinwachs DM, Graham CM, Lehman A, Ford DE. Prevalence and correlates of obesity in a community sample of individuals with severe and persistent mental illness. J Nerv Ment Dis. 2003;191(12):799–805. doi: 10.1097/01.nmd.0000100923.20188.2d. [DOI] [PubMed] [Google Scholar]
- Daumit GL, Goldberg RW, Anthony C, Dickerson F, Brown CH, Kreyenbuhl J, Wohlheiter K, Dixon LB. Physical activity patterns in adults with severe mental illness. J Nerv Ment Dis. 2005;193(10):641–646. doi: 10.1097/01.nmd.0000180737.85895.60. [DOI] [PubMed] [Google Scholar]
- de Leon J, Dadvand M, Canuso C, White AO, Stanilla JK, Simpson GM. Schizophrenia and smoking: An epidemiological survey in a state hospital. Am J Psychiatry. 1995;152(3):453–455. doi: 10.1176/ajp.152.3.453. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Adler DA, Berlant JL, Dulit RA, Goldman B, Hackman AL, Oslin DW, Siris SG, Sonis WA, Valenstein M. Psychiatrists and primary caring: what are our boundaries of responsibility? Psychiatr Serv. 2007;58(5):600–602. doi: 10.1176/ps.2007.58.5.600. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Kreyenbuhl JA, Dickerson FB, Donner TW, Brown CH, Wohlheiter K, Postrado L, Goldberg RW, Fang L, Marano C, Messias E. A comparison of Type 2 diabetes outcomes among persons with and without severe mental illness. Psychiatr Serv. 2004;55(8):892–900. doi: 10.1176/appi.ps.55.8.892. [DOI] [PubMed] [Google Scholar]
- Dixon LB, Weiden P, Delahanty J, Goldberg R, Postrado L, Lucksted A, Lehman A. Prevalence and correlates of diabetes in national schizophrenia samples. Schizophr Bull. 2000;26(4):903–912. doi: 10.1093/oxfordjournals.schbul.a033504. [DOI] [PubMed] [Google Scholar]
- Douglas JG, Bakris GL, Epstein M, Ferdinand KC, Ferrario C, Flack JM, Jamerson KA, Jones WE, Haywood J, Maxey R, Ofili EO, Saunders E, Schiffrin EL, Sica DA, Sowers JR, Vidt DG. Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks: Management of high blood pressure in African Americans: consensus statement of the Hypertension in African Americans Working Group of the International Society on Hypertension in Blacks. Arch Intern Med. 2003;163(5):525–541. doi: 10.1001/archinte.163.5.525. [DOI] [PubMed] [Google Scholar]
- Egede LE, Dagogo-Jack S. Epidemiology of type 2 diabetes: focus on ethnic minorities. Med Clin North Am. 2005;89(5):949–975. doi: 10.1016/j.mcna.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Essock SM, Dowden S, Constantine NT, Katz L, Swartz MS, Meador KG, Osher FC, Rosenberg SD Five-Site Health and Risk Study Research Committee. Risk factors for HIV, hepatitis B, and hepatitis C among persons with severe mental illness. Psychiatr Serv. 2003;54(6):836–841. doi: 10.1176/appi.ps.54.6.836. [DOI] [PubMed] [Google Scholar]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285(19):2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- Frayne SM, Halanych JH, Miller DR, Wang F, Lin H, Pogach L, Sharkansky EJ, Keane TM, Skinner KM, Rosen CS, Berlowitz DR. Disparities in diabetes care: impact of mental illness. Arch Intern Med. 2005;165(22):2631–2638. doi: 10.1001/archinte.165.22.2631. [DOI] [PubMed] [Google Scholar]
- Garcia-Unzueta MT, Herran A, Sierra-Biddle D, Amado JA, Vazquez-Barquero JL, Alvarez C. Alterations of liver function test in patients treated with antipsychotics. J Clin Lab Anal. 2003;17(6):216–218. doi: 10.1002/jcla.10094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goff DC, Sullivan LM, McEvoy JP, Meyer JM, Nasrallah HA, Daumit GL, Lamberti S, D’Agostino RB, Stroup TS, Davis S, Lieberman JA. A comparison of ten-year cardiac risk estimates in schizophrenia patients from the CATIE study and matched controls. Schizophr Res. 2005;80(1):45–53. doi: 10.1016/j.schres.2005.08.010. [DOI] [PubMed] [Google Scholar]
- Goldberg RW, Kreyenbuhl J, Dickerson FB, Wohlheiter K, Fang LJ, Brown CH, Dixon LB. Quality of diabetes care among adults with serious mental illness. Psychiatr Serv. 2007;58(4):536–543. doi: 10.1176/ps.2007.58.4.536. [DOI] [PubMed] [Google Scholar]
- Grant RW, Buse JB, Meigs JB. Quality of diabetes care in US academic medical centers. Diabetes Care. 2005;28(2):337–442. doi: 10.2337/diacare.28.2.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward RA, Hofer TP, Vijan S. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006;145(7):520–530. doi: 10.7326/0003-4819-145-7-200610030-00010. [DOI] [PubMed] [Google Scholar]
- Krein SL, Bingham CR, McCarthy JF, Mitchinson A, Payes J, Valenstein M. Diabetes treatment among VA patients with comorbid serious mental illness. Psychiatr Serv. 2006;57(7):1016–1021. doi: 10.1176/ps.2006.57.7.1016. [DOI] [PubMed] [Google Scholar]
- Kreyenbuhl J, Dickerson FB, Medoff DR, Brown CH, Goldberg RW, Fang L, Wohlheiter K, Mittal LP, Dixon LB. Extent and management of cardiovascular risk factors in patients with type 2 diabetes and serious mental illness. J Nerv Ment Dis. 2006;194(6):404–410. doi: 10.1097/01.nmd.0000221177.51089.7d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreadie RG. Diet, smoking and cardiovascular risk in people with schizophrenia: Descriptive study. Br J Psychiatry. 2003;183(6):534 –539. doi: 10.1192/bjp.183.6.534. [DOI] [PubMed] [Google Scholar]
- McEvoy JP, Meyer JM, Goff DC, Nasrallah HA, Davis SM, Sullivan L, Meltzer HY, Hsiao J, Stroup TS, Lieberman JA. Prevalence of the metabolic syndrome in patients with schizophrenia: baseline results from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE) schizophrenia trial and comparison with national estimates from NHANES III. Schizophr Res. 2005;80(1):19–32. doi: 10.1016/j.schres.2005.07.014. [DOI] [PubMed] [Google Scholar]
- Miller DR, Safford MM, Pogach LM. Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care. 2004;27(Suppl 2):B10–21. doi: 10.2337/diacare.27.suppl_2.b10. [DOI] [PubMed] [Google Scholar]
- Nasrallah HA, Meyer JM, Goff DC, McEvoy JP, Davis SM, Stroup TS, Lieberman JA. Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: data from the CATIE schizophrenia trial sample at baseline. Schizophr Res. 2006;86(1–3):15–22. doi: 10.1016/j.schres.2006.06.026. [DOI] [PubMed] [Google Scholar]
- Nau DP, Garber MC, Herman WH. The intensification of drug therapy for diabetes and its complications: Evidence from 2 HMOs. Am J Manag Care. 2004;10(2 Pt 2):118 –123. [PubMed] [Google Scholar]
- Nau DP, Mallya U. Sex disparity in the management of dyslipidemia among patients with type 2 diabetes mellitus in a managed care organization. Am J Manag Care. 2005;11(2):69 –73. [PubMed] [Google Scholar]
- Newcomer JW. Second-generation (atypical) antipsychotics and metabolic effects: a comprehensive literature review. CNS Drugs. 2005;19(Suppl 1):1–93. doi: 10.2165/00023210-200519001-00001. [DOI] [PubMed] [Google Scholar]
- Osby U, Correia N, Brandt L, Ekbom A, Sparen P. Mortality and causes of death in schizophrenia in Stockholm County, Sweden. Schizophr Res. 2000;45(1–2):21–28. doi: 10.1016/s0920-9964(99)00191-7. [DOI] [PubMed] [Google Scholar]
- Rosen AB. Indications for and utilization of ACE inhibitors in older individuals with diabetes. Findings from the National Health and Nutrition Examination Survey 1999 to 2002, 2006. J Gen Intern Med. 2006;21(4):315–319. doi: 10.1111/j.1525-1497.2006.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen AB, Karter AJ, Liu JY, Selby JV, Schneider EC. Use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in high-risk clinical and ethnic groups with diabetes. J Gen Intern Med. 2004;19(6):669–675. doi: 10.1111/j.1525-1497.2004.30264.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safford M, Eaton L, Hawley G, Brimacombe M, Rajan M, Li H, Pogach L. Disparities in use of lipid-lowering medications among people with Type 2 diabetes mellitus. Arch Intern Med. 2003;163(8):922–928. doi: 10.1001/archinte.163.8.922. [DOI] [PubMed] [Google Scholar]
- Sequist TD, Adams A, Zhang F, Ross-Degnan D, Ayanian JZ. Effect of quality improvement on racial disparities in diabetes care. Arch Intern Med. 2006;166(6):675–681. doi: 10.1001/archinte.166.6.675. [DOI] [PubMed] [Google Scholar]
- Weiss AP, Henderson DC, Weilburg JB, Goff DC, Meigs JB, Cagliero E, Grant RW. Treatment of cardiac risk factors among patients with schizophrenia and diabetes. Psychiatr Serv. 2006;57(8):1145–1152. doi: 10.1176/ps.2006.57.8.1145. [DOI] [PubMed] [Google Scholar]
- Winkelmayer WC, Fischer MA, Schneeweiss S, Wang PS, Levin R, Avorn J. Underuse of ACE inhibitors and angiotensin II receptor blockers in elderly patients with diabetes. Am J Kidney Dis. 2005;46(6):1080–1087. doi: 10.1053/j.ajkd.2005.08.018. [DOI] [PubMed] [Google Scholar]


