Abstract
Background
Outpatient management is appropriate for chronic pilonidal sinuses. Even though there are different surgical treatments for pilonidal sinuses, the outcome may not be uniformly satisfactory. The aim of this paper was to examine the ambulatory treatment of chronic pilonidal sinuses with lateral incision and primary suture.
Methods
We present our experience with outpatient management of asymptomatic chronic pilonidal disease. We prospectively studied patients presenting with pilonidal disease from Mar. 20, 2005, to Mar. 20, 2008. All were managed as outpatients. We reviewed presentation, treatment, healing, time off work and recurrences.
Results
In all, 150 patients (131 men and 19 women) with chronic pilonidal sinuses underwent ambulatory plain lateral excision and primary repair during the study period. The mean age of patients was 22.1 years. The mean duration of surgery was 18.4 minutes. No general complications occurred. Local complications consisted of 3 wound infections and 4 wound hematomas. No sinus recurrence occurred. The healing rate was fast in all patients.
Conclusion
Advantages of ambulatory plain lateral excision and primary repair include immediate treatment, minimal pain and a quick return to normal activities. This method is a simple and effective procedure in the treatment of uncomplicated pilonidal sinuses.
Abstract
Contexte
La prise en charge en service externe convient dans le cas de sinus pilonidaux chroniques. Même s’il existe divers traitements chirurgicaux pour les sinus pilonidaux, le résultat peut ne pas être uniformément satisfaisant. Cette communication visait à examiner le traitement ambulatoire des sinus pilonidaux chroniques par incision latérale et suture immédiate.
Méthodes
Nous présentons notre expérience de la prise en charge en service externe de la maladie pilonidale chronique asymptomatique. Nous avons étudié de façon prospective les patients qui se sont présentés avec une maladie pilonidale du 20 mars 2005 au 20 mars 2008. Tous ont été traités en service externe. Nous avons passé en revue la présentation, le traitement, la guérison, l’absence du travail et les récidives.
Résultats
Au total, 150 patients (131 hommes et 19 femmes) qui avaient des sinus pilonidaux chroniques ont subi une excision latérale ordinaire et une réparation immédiate en service ambulatoire au cours de la période à l’étude. Les patients avaient en moyenne 22,1 ans. L’intervention chirurgicale a duré en moyenne 18,4 minutes. Il n’y a pas eu de complications généralisées. Il y a eu 3 plaies infectées et 4 hématomes à la plaie comme complications locales. Le sinus n’est pas réapparu. La guérison a été rapide chez tous les patients.
Conclusion
Les avantages de l’excision latérale ordinaire et de la réparation immédiate en service ambulatoire comprennent le traitement immédiat, une douleur minimale et la reprise rapide des activités normales. Cette méthode est simple et efficace pour traiter les sinus pilonidaux sans complication.
The management of chronic pilonidal disease is variable, contentious and problematic. Principles of treatment require eradication of the sinus tract, complete healing of the overlying skin and prevention of recurrence. The surgical wound may be left open to heal (secondary intention). Advocates of this technique state that reduced wound tension facilitates trouble-free healing without recurrence if all sinus tracts are fully excised. Alternatively, the wound may be closed to heal by primary closure (primary intention). Methods can be broadly categorized as midline closure techniques (with the wound lying within the natal cleft) or other techniques (where the wounds are located out of the midline). Advocates of primary closure perceive benefits of faster tissue healing. The current literature describes a wide spectrum in patient outcomes for different open and closed surgical techniques.1–6
Treatment of pilonidal sinuses is controversial, and multiple therapeutic approaches have been described in the literature.7–10 The principal requirements of an ideal treatment are high rate of cure, low rate of postoperative complications, low rate of recurrence, avoidance of hospital admission, avoidance of general and spinal anesthesia and minimal inconvenience and time off work for the patient. We sought to examine the ambulatory treatment of chronic pilonidal sinuses with lateral incision and primary suture.
Methods
This study was planned prospectively in the surgical unit of Sina Hospital, University of Medical Sciences of Tabriz, Iran, and the study period spanned between Mar. 20, 2005, and Mar. 20, 2008. Our surgical unit is a referral centre for anorectal problems and other general surgical procedures. Chronic pilonidal sinus is the term applied to patients with pilonidal sinuses who have had pilonidal abscesses drained or to patients with pilonidal sinuses associated with chronic discharge without acute abscess. We included patients with nonrecurrent, asymptomatic, chronic discharging pilonidal sinuses. Patients with recurrent pilonidal sinuses and acute abscesses were excluded. We obtained informed consent from all patients, and the designated review board of our institution approved our study.
We obtained a detailed history, including family history and risk factors, from each patient. A special model was prepared to study epidemiologic, demographic and therapeutic data. Data collected for each patient included age, sex, duration of the disease, duration of surgery and postoperative complications. Body mass index (BMI) was measured for all patients. We performed a thorough clinical examination to exclude other conditions that resemble pilonidal sinuses. All patients were treated on an outpatient basis (we have a day-surgery facility within the main hospital). All patients were seen daily until healing was achieved and subsequently every 2 months after discharge for a period of 1–4 years. During this period, we called and visited patients in their homes to assess the patients for recurrence and any other postoperative complications, and to determine how long the patient was unable to work. We defined recurrence as a redevelopment of pain, pit and discharge. Healing, recurrence and other postoperative complications were assessed by 2 observers who were independent from the operating surgeon (H.M.), who performed all the surgeries. The findings were entered on a computer by means of an SPSS 14 database file that was designed by one of us (H.M.).
Surgical technique
Patients were placed in the prone position. The buttocks were retracted with adhesive tape. The sacral area was completely shaved and disinfected with povidine iodine solution, and drapes were arranged. The surgeries were performed under local anesthesia with 8 mL of a 2% solution of lidocaine and 2 mL of a 0.25% solution of bupivacaine (field block). No patients needed supplementary sedation. The place of injection of local anesthesia is shown in Figure 1. We did not use methylene blue to stain the sinus tract.
Fig. 1.
Local anesthetic: 8 mL of a 2% solution of lidocaine and 2 mL of a 0.25% solution of bupivacaine was injected into the sinus area.
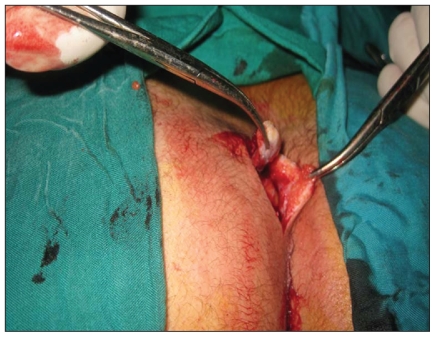
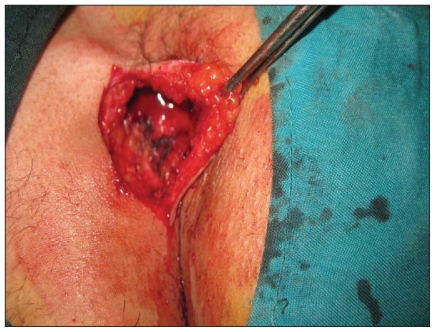
The lateral incision (3–7 cm according to the extent of disease) was made 1 cm from the midline, and the incision was deepened and kept as close as possible to the sinus tract (Figs. 2 and 3). All diseased tissue was removed enbloc. Careful hemostasis was performed. All pilonidal openings were débrided and stayed open for drainage (Fig. 4). Skin edges and the immediate subcutaneous fat were then approximated with 3–0 nylon sutures (Fig. 4). We avoided a “dead space” using pressure dressing. All patients received 2 days of oral antibiotic (400 mg of cefixime daily).
Fig. 2.
Lateral incision and removal of sinus tract.
Fig. 3.
Residual cavity after removal of the pilonidal sinus.
Fig. 4.
Skin sutures were made and sinus pits débrided and left open for drainage.
The specimens of all patients were examined pathologically, and culture and sensitivity was performed. The dressings of all patients were changed daily for 1 week. The sutures were removed on day 14. Shaving the natal cleft and area twice monthly after surgery for 1 year was strongly recommended. Postoperative pain was recorded using a visual analog scale, with a score of 1 indicating mildest pain and 10 indicating the worst pain.
Statistical analysis
We performed statistical analyses using SPSS 14. We completed a univariate analysis using the Fisher exact test and the Mann–Whitney U test. The level of significance was set at p < 0.05.
Results
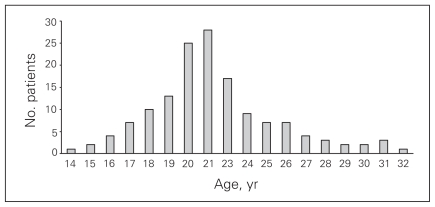
There were 131 (87.3%) male and 19 (12.7%) female patients included in our study; their mean age was 22.1 (standard deviation [SD] 11.3, range 14.0–32.0) years. The male:female ratio was 7:1, with a substantial male preponderance. The average duration of symptoms before surgery was 12.4 (SD 18.5) days. The mean duration of symptoms (e.g., occasional discharge and pain) was 3.2 (range 0.6–4.2) years. Sixty-five patients (43.3) had 1–2 midline pits; the remainder had more than 2 midline pits. Most patients were between the ages of 15 and 25, and the incidence decreased thereafter. The age distribution is shown in Figure 5.
Fig. 5.
Age distribution of patients with pilonidal sinus disease.
Among the male patients, 103 were obese (BMI > 30 kg/m2), 17 were overweight (BMI > 25 but < 30 kg/m2) and 11 had a healthy weight (BMI < 25 kg/m2). Among the 19 female patients, 9 were obese (BMI > 30 kg/m2), 6 were overweight (BMI > 25 but < 30 kg/m2) and 4 had a healthy weight (BMI < 25 kg/m2). The average BMI for both sexes was 29.3 (SD 2.8, range 22.0–31.0) kg/m2. All of the patients were followed for a mean of 29.7 (range 12.0–48.0, median 29.0, SD 11.0) months. There were no recurrences in the follow-up period.
We observed no complications from the local anesthesia. Local complications included 4 hematomas (2.6%) and 3 wound infections (2%). The sacral fascia was not included in the excision because no patient had evidence of its involvement at the time of surgery. The mean duration of surgery was 18.4 minutes. Bacteriologic examination revealed aerobic or anaerobic organisms in all patients. The cultures showed that the common organisms were Staphylococcus aureus, hemolytic streptococcus, bacteroides and gram-negative cocci. Hairs were found in the cystic cavity in all specimens. Time needed for wound healing was 7–10 (mean 7) days. Patients had no pain for 4–6 hours after surgery owing to the long-acting local anesthesia. After that time, pain was scored at 1–3, which was significantly lower than pain scores associated with other techniques. No patient was lost to follow up. No midline pits redeveloped in our patients during the follow-up period. No further problems or symptoms were observed. Surgical and outcome data for our patients is provided in Table 1.
Table 1.
Surgical and outcome data for 150 patients with pilonidal sinuses
| Variable | No. |
|---|---|
| Sex, male:female | 131:19 |
| Duration of symptoms,* mo | 7–51 |
| Duration of increase of symptoms, mean (SD) d | 12.39 (18.5) |
| Duration of surgery, mean (range) min | 18.4 (15–20) |
| Wound hematoma | 4 |
| Wound infection | 3 |
| Dehiscence | 0 |
| Removal of suture, d | 10–14 |
| Wound healing, d | 7–10 |
| Return to work, mean (SD) d | 9.3 (1.6) |
| Sinus recurrence, no. | 0 |
SD = standard deviation.
Defined as occasional discharge and pain.
Discussion
Pilonidal sinus is a common infective process that occurs in the natal cleft and sacrococcygeal region, almost always in adolescents and young adults. Pilonidal sinus is not a new disease entity, but the management still needs a lot of attention to prevent recurrence, which is a disturbing complication requiring frequent hospital admissions and loss of work days.11 Bascom12 and Edwards13 reported their experience with removal of the follicles and hairs. In the study by Bascom,12 50 patients were treated by excision of the enlarged follicles from the midline skin. One to 10 follicles were removed, individually if possible. The specimens weighed under 1 g in all patients. Incisions were kept smaller than 7 mm. Follow-up averaged 24 months. The mean disability was 1 day, and the mean wound healing time was 3 weeks. Recurrences appeared in 4 patients (8%); all were healed 3 weeks following reoperation. There was no incident of a second recurrence. A later report by Bascom14 involving 161 patients treated in the same way revealed comparable results. In the study by Edwards,13 102 patients were treated using this same technique. The median number of days off work was 10, and the median wound healing time 39 days. The 91 (89%) patients who attended the follow-up clinic were free of recurrent disease. Since a number of patients failed to attend, it is difficult to interpret the results of this study. It appears, however, that the author was not as successful as Bascom.
Zimmerman15 reported outpatient excision and primary closure in 32 patients. The mean follow-up was 24 months. In all patients, primary healing was achieved, a result that is similar to our own experience. Kronborg and colleagues16 reported the results of a randomized trial of treatment by 1 of 3 methods: excision, excision with suture and excision with suture and antibiotic coverage with clindamycin. Recurrences rates were 13%, 25% and 19%, respectively. As expected, healing was much quicker after primary suture than after excisional therapy alone (median 14 d v. 64 d). In our series, most patients were male (male:female ratio 7:1), the mean age was 22.1 years, and these data compare with that in other series. Obesity and overweight were risk factors; 112 of 150 patients were obese (74.7%) and 23 (15.3%) were overweight.
When considering how to treat pilonidal sinus, physicians should keep in mind that this condition is more than merely a specific form of foreign body granuloma. An ideal surgery should be a simple excision of ill-defined tissues, should not require hospital stay, should decrease the patient’s time off work or school and should be minimally invasive.17–19 The depth and width of the surgical wound, depending on the size of the pilonidal sinus cavity and associated sinus tract, do not routinely include deeper layers and should not be extended beyond the ill-defined tissue.
In our series, sacrococcygeal fascia and ligaments were not found to be involved and were saved in all patients, which helped reduce or even eliminate the residual dead space. Drainage by débrided sinus pits also favours a satisfactory early postoperative outcome. A low and overall satisfactory number of early postoperative wound complications was observed in our series. Overall, the rate of surgical site infection (SSI) after pilonidal surgery is low, except in 2 studies that reported SSI rates with open healing of 14% and 22%, respectively. In 1 systematic review, the SSI rates were 10.4% after midline closure and 6.3% after off-midline closure. Our study identified an infection rate of 2%, which was less than that reported in other systematic reviews.
Overall, recurrence of pilonidal sinus was more common with midline closure (59 of 503, 11.7%) than with open healing (22 of 491, 4.5%), with a 58% lower risk of recurrence at 1 year postoperatively.1,18,20 This equates to 14 patients per 100 undergoing primary closure (5 per 100 undergoing open healing) experiencing a recurrence. In a recent review of literature, the recurrence rates were 1.4% with off-midline closure and 10.3% with midline closure.1,18,20 In our series, no recurrences occurred.
In our study, the rate of postoperative hematoma was 2.7%. In another study, postoperative bleeding was 4%, which was greater than in our study.1,17,21 Midline excision of pilonidal sinus has been considered to be responsible for postoperative skin problems, early and late breakdown, recurrences and chronic pain because the natal cleft needs to be maintained.16,19–23 With our technique, midline skin is preserved and prevents postoperative skin problems. In our series, lateral incisions healed promptly and with reasonable strength in all patients. Furthermore, these wounds were associated with a negligible recurrence rate. In our opinion, the causes of this satisfactory early outcome are 3-fold: limited excision, preservation of midline skin and anatomy, and sensible postoperative management.
In the United States, pilonidal sinus disease affects about 26 per 100 000 people.4 The onset of pilonidal sinus disease is rare both before puberty and after the age of 40 years. Men are more affected than women (ratio 3:1 or 4:1);17 in our series the ratio was 7:1. The average age of presentation is 21 years for men and 19 years for women;17 in our study, the mean age for both sexes was 22.1 years. The risk factors include sedentary occupation, positive family history, obesity and local irritation and trauma.20 Hormones, hair, friction and infection all play a role in the pathogenesis of the disease.19,20
It is now generally agreed that minimally invasive surgery should be used to treat pilonidal disease whenever possible. Data suggest that ambulatory plain excision with lateral incision and primary suture is an appropriate approach for most patients with pilonidal sinuses. Every attempt should be made to avoid admission to hospital and to limit the morbidity of the procedure. However, there are some patients who benefit from a more extensive excision, and in those circumstances, inpatient hospital treatment with excision and primary closure with or without grafting or flap may offer a lower morbidity.
Footnotes
Competing interests: None declared.
Contributors: Dr. Maghsoudi designed the study. Drs. Maghsoudi and Nezami acquired the data, which Drs. Maghsoudi and Ghamari analyzed. All authors wrote the article, which Drs. Maghsoudi and Ghamari reviewed. All authors approved the final version for publication.
References
- 1.McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systemic review and meta-analysis. BMJ. 2008;336:868–71. doi: 10.1136/bmj.39517.808160.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Senapati A, Cripps NPJ, Thompson MR. Bascom’s operation in the day-surgical management of symptomatic pilonidal sinus. Br J Surg. 2000;87:1067–70. doi: 10.1046/j.1365-2168.2000.01472.x. [DOI] [PubMed] [Google Scholar]
- 3.Chintapatla S, Safarani N, Kumar S. Sacrococcygeal pilonidal sinus: historical review, pathological insight and surgical options. Tech Coloproctol. 2003;7:3–8. doi: 10.1007/s101510300001. [DOI] [PubMed] [Google Scholar]
- 4.Hodges RM. Pilonidal sinus. Boston Med Surg J. 1880;103:485–6. [Google Scholar]
- 5.Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992;62:385–9. doi: 10.1111/j.1445-2197.1992.tb07208.x. [DOI] [PubMed] [Google Scholar]
- 6.da Silva JH. Pilonidal cyst: cause and treatment. Dis Colon Rectum. 2000;43:1146–56. doi: 10.1007/BF02236564. [DOI] [PubMed] [Google Scholar]
- 7.Shafik A. Electrocauterization in the treatment of pilonidal sinus. Int Surg. 1996;81:83–4. [PubMed] [Google Scholar]
- 8.Wood RAB, Hughes LE. Silicon foam sponge for pilonidal sinus: a new technique for dressing open granulating wounds. BMJ. 1975;4:131–3. doi: 10.1136/bmj.4.5989.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hege HG, Vos GA, Pakta P, et al. Treatment of complicated or infected pilonidal sinus disease by local application of phenol. Surgery. 1987;102:52–4. [PubMed] [Google Scholar]
- 10.Duchateau J, DeMol J, Bostoen H, et al. Pilonidal sinus. Excision —marsupialization — phenolization. Acta Chir Belg. 1985;85:325–8. [PubMed] [Google Scholar]
- 11.Allen-Mersh TG. Pilonidal sinus: finding the right track of treatment. Br J Surg. 1990;77:123–32. doi: 10.1002/bjs.1800770203. [DOI] [PubMed] [Google Scholar]
- 12.Bascom J. Pilonidal disease: origin from follicles of hairs and results of follicle removal as treatment. Surgery. 1980;87:567–72. [PubMed] [Google Scholar]
- 13.Edwards MH. Pilonidal sinus: a 5-year appraisal of the Millar-Lord treatment. Br J Surg. 1977;64:867–8. doi: 10.1002/bjs.1800641209. [DOI] [PubMed] [Google Scholar]
- 14.Bascom J. Pilonidal disease: long-term results of follicle removal. Dis Colon Rectum. 1983;26:800–7. doi: 10.1007/BF02554755. [DOI] [PubMed] [Google Scholar]
- 15.Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Am J Surg. 1978;136:640–2. doi: 10.1016/0002-9610(78)90326-4. [DOI] [PubMed] [Google Scholar]
- 16.Kronborg O, Christensen K, Zimmermann-Nielsen C. Chronic pilonidal disease: a randomized trial with a complete 3-year follow-up. Br J Surg. 1985;72:303–4. doi: 10.1002/bjs.1800720418. [DOI] [PubMed] [Google Scholar]
- 17.Ringelheim R, Silverberg MA, Johnson-Villanueva NJ. Pilonidal cyst and sinus. eMedicine. [accessed 2009 Sept. 28]. Available: http://emedicine.medscape.com/article/788127-overview.
- 18.Sondenaa K, Nesvik I, Anderson E, et al. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995;10:39–42. doi: 10.1007/BF00337585. [DOI] [PubMed] [Google Scholar]
- 19.Jones DJ. ABC of colorectal diseases. Pilonidal sinus. BMJ. 1992;305:410–2. doi: 10.1136/bmj.305.6850.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miller D, Harding K. Pilonidal sinus disease. World Wide Wounds. [accessed 2008 Dec. 19]. Available: wwwworldwidewoundscom/2003/December/Miller/Pilonidal-Sinushtml.
- 21.Akinci OF, Coskun A, Uzunkoy A. Simple and effective surgical treatment of pilonidal sinus. Asymmetric excision and primary closure using suction drain and subcuticular skin closure. Dis Colon Rectum. 2000;43:701–6. doi: 10.1007/BF02235591. [DOI] [PubMed] [Google Scholar]
- 22.McLaren CA. Partial closure and other techniques in pilonidal surgery: an assessment of 157 cases. Br J Surg. 1984;71:561–2. doi: 10.1002/bjs.1800710731. [DOI] [PubMed] [Google Scholar]
- 23.Tocchi A, Mazzoni G, Bononi M, et al. Outcome of chronic pilonidal disease treatment alter ambulatory plain midline excision and primary suture. Am J Surg. 2008;196:28–33. doi: 10.1016/j.amjsurg.2007.05.051. [DOI] [PubMed] [Google Scholar]