Abstract
Background
The effective management of wait times is a top priority for Canadians. Attention to date has largely focused on wait times for adult surgery. The purpose of this study was to develop surgical wait time access targets for children.
Methods
Using nominal group techniques, expert panels reached consensus on prioritization levels for 574 diagnoses in 10 surgical disciplines for wait 1 (W1; time from primary care visit to surgical consultation) and wait 2 (W2; time from decision to operate to receipt of surgery).
Results
A 7-stage priority classification reflects the permissible timeframe for children to receive consultation (W1) or surgery (W2). Access targets by priority were linked to 574 diagnoses in 10 pediatric surgical subspecialties.
Conclusion
The pediatric surgical wait time access targets are a standardized, comprehensive and consensus-based model that can be systematically applied to children’s hospitals across Canada. Future research and evaluation on outcomes from this model will evaluate improved access to pediatric surgical care.
Abstract
Contexte
La gestion efficace des temps d’attente constitue une priorité de premier plan pour les Canadiens. Jusqu’à maintenant, l’attention a été concentrée surtout sur les temps d’attente en chirurgie pour les adultes. Cette étude visait à établir des objectifs de temps d’attente pour l’accès à la chirurgie chez les enfants.
Méthodes
En se basant sur des techniques de groupe nominal, des groupes d’experts ont dégagé un consensus sur les priorités à accorder à 574 diagnostics dans 10 disciplines de la chirurgie pour les temps d’attente 1 (T1; temps écoulé entre la consultation en soins primaires et la consultation en chirurgie) et 2 (T2; temps écoulé entre la decision d’opérer et l’intervention chirurgicale).
Résultats
Une classification des priorités en 7 niveaux traduit les délais permissibles pour que les enfants soient vus en consultation (T1) ou subissent une intervention chirurgicale (T2). Les objectifs d’accès selon la priorité ont été reliés à 574 diagnostics dans 10 surspécialités de la chirurgie pédiatrique.
Conclusion
Les objectifs de temps d’attente pour l’accès à la chirurgie pédiatrique constituent un modèle normalisé, complet et consensuel qu’il est possible d’appliquer systématiquement dans les hôpitaux pédiatriques du Canada. Des recherches et des évaluations à venir portant sur les résultats issus de ce modèle permettront d’évaluer l’amélioration de l’accès aux soins en chirurgie pédiatrique.
Access to timely, quality health care is highly valued by Canadians.1,2 Current wait times are unacceptable, prompting both federal and provincial government attention.3 Until recently, wait lists in Canada have been poorly monitored.4 Furthermore, reducing wait times has been difficult because prioritization of surgery has been largely dependent on individual doctors and hospitals.5 As a result, wait times have been shown to vary widely by practitioner and jurisdiction, and timeliness of care does not always correspond to the severity of patients’ conditions.
Wait time reduction requires attention to many issues, including identification, prioritization and triage of patients’ medical conditions; monitoring and management of wait times for care; sufficient physical capacity, such as the number of operating rooms; resources to address care backlogs; and appropriate health human resources, including sufficient numbers of nurses and physicians. In Canada, attention to date on wait time reduction has focused largely on adult health care needs, such as cataract surgery, magnetic resonance imaging (MRI), computed tomography (CT), hip and knee arthroplasty, cardiac care and cancer surgery. In addition to the known consequences of prolonged wait times for adults, including continued suffering, emotional distress and personal economic hardship, young patients are at particular risk. A 6-month surgical wait for a 1-year-old is half the child’s life. Furthermore, children often require treatment at critical times to ensure appropriate development. The objective of this study was to develop access targets for pediatric surgical procedures across 10 subspecialties.
Methods
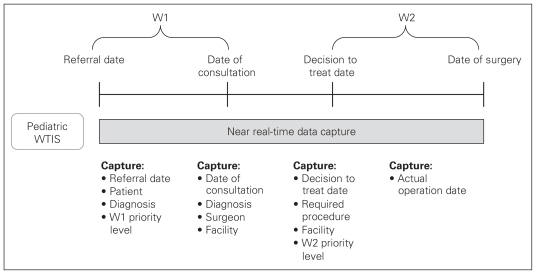
The project was lead by a steering group of the Ontario Children’s Health Network (OCHN). The OCHN was a collaborative group with representatives from all 6 pediatric academic health science centres in Ontario. The initiative was funded by a health innovation grant from the Ontario Ministry of Health and Long-term Care. Five of the 6 hospitals provide surgical care. The chiefs of surgery from these 5 hospitals were all members of the steering committee. Table 1 describes the key terms and definitions used in this study. For the purposes of this project, access target was defined as the permissible timeframe for children to receive consultation or surgery. Although the total wait for patients and families includes all steps, such as waiting for primary care or diagnostic tests, our work focused on the time between the referral from the primary care provider and specialist consultation (W1) and the time between decision to operate and receipt of surgery (W2; Fig. 1).
Table 1.
Definitions of key terms and criteria for implementation of the Pediatric Wait Time Strategy
| Term | Definition |
|---|---|
| Access target | Acceptable timeframe waiting for consultation and surgery |
| Wait 1 (W1) | Time period between referral from primary care provider to consultation with specialist/surgeon |
| Wait 2 (W2) | Time period between decision by surgeon and family for surgery and receipt of surgical procedure |
| Pediatric patient | Age is from birth to patient’s eighteenth birthday, excluding healthy newborns and obstetric surgery |
| Surgical subspecialty | Areas or disciplines within pediatric surgery |
Fig. 1.
Time frame description of Pediatric Wait Time Strategy and points of outcome derivation. W1 = time from primary care visit to surgical consultation; W2 = time between the decision to operate and receipt of surgery; WTIS = wait time information system.
There are 2 approaches for developing criteria for prioritization of surgical wait times: evidence-based and consensus-based approaches. An evidence-based approach is preferred because the duration of the wait time is directly related to health outcomes.6 A PubMed MEDLINE search identified 209 English publications dating from 1994 to September 2004 using the keywords “wait list,” “wait list management” or “wait list priorities” with terms “health priorities,” “health services accessibility” or “health care rationing.” An Internet search was also conducted to retrieve relevant articles and institutional reports, including those from the Cardiac Care Network (www.ccn.on.ca), the Western Canada Waiting List Project (www.wcwl.ca), the Canadian Policy Research Network (http://cprn.org/index.cfm) and the Fraser Institute (www.fraserinstitute.org). No evidence-based guidelines for pediatric surgical wait times were identified in these searches, and thus a consensus-based approach was used.
Two methods are commonly used for consensus-based guidelines: nominal group or Delphi.7 The nominal technique involves repeated discussions in a round-table setting, with a mediator facilitating the process by soliciting differing perspectives and reducing misunderstandings. In the Delphi method, 2 or more rounds of postal surveys are used with feedback of results to participants after each round. Because the Delphi approach is not conducive to clarification and resolution of differences in viewpoints, the nominal group method was used in this study.
Workshops were conducted with volunteer surgical representatives from each subspecialty from the 5 academic pediatric health centres in Ontario that perform surgery: Children’s Hospital of Eastern Ontario (Ottawa), Children’s Hospital of Western Ontario (London), McMaster’s Children’s Hospital (Hamilton), South Eastern Ontario Health Sciences Centre (Kingston) and The Hospital for Sick Children (Toronto). The 10 pediatric disciplines included cardiovascular surgery, dental surgery, general surgery, gynecology, neurosurgery, ophthalmology, orthopedic surgery, otolaryngology, plastic surgery and urology.
A consultant facilitated the workshops, and a member of the OCHN steering group was present for all 10 discipline-specific expert panels. First, expert panels chose an appropriate priority scoring system for W1 and W2. Second, the panels reviewed a list of diagnoses for their subspecialties. In advance of the workshops, 1 member of each expert panel prepared a list of diagnoses for the subspecialty to initiate the panel discussion. The instructions to the clinicians in the consensus meeting were to consider all the diagnoses they encountered in their specialties as patients presented for consultation and surgery. The diagnostic list was meant to be comprehensive for each specialty, and the mixture of emergent, urgent and diagnostic procedures reflected interdisciplinary differences. The consensus group modified, collapsed, clarified or added diagnoses to ensure that most were addressed (Appendix 1, available at cma.ca/cjs). Third, participants had a round-table discussion about acceptable wait times for consultation (W1) and surgery (W2) for each diagnosis. Discussion continued around the table until consensus was achieved and all diagnoses had been assigned a priority score for consultation and surgery. Most diagnoses could be assigned a W1 and W2 priority score without subcategorization. However, a few diagnoses required subclassification by severity or age. The draft access targets for each subspecialty were collated and sent out to the specific subspecialty panelists after the workshops for feedback and revision.
There were a small number of diagnoses that were identified and assigned access targets by more than 1 subspecialty group. Minor ranking inconsistencies for the same diagnoses between consensus groups were identified and resolved through meetings between representatives from the affected surgical disciplines. The access targets were then distributed to all pediatric surgeons across Ontario for feedback. Finally, the access targets were pilot-tested at The Hospital for Sick Children and received minor modifications. In this pilot study, the access targets were applied to patients receiving surgery over a 1-month period. Based on the pilot study, a few diagnoses were added to the list. The access targets were adopted by all 16 pediatric health science centres from across Canada at a group meeting in February 2006. In the future, 11 discipline-specific pan-Canadian groups will meet in person or by teleconference to review the list of diagnoses and associated access targets.
Results
The Saskatchewan Classification System from the Western Canada Waiting List Project was chosen as the most appropriate priority rating score for children. The system was modified by dividing the priority classification level II into 2 levels. The 7-category scale was judged to be clinically most appropriate to accommodate the needs of a rapidly developing pediatric patient (Table 2). A 7-grade scale also had the advantage of easily allowing collapse into fewer categories, if required, to comply with the Provincial Wait Time Information System.
Table 2.
Wait time from referral to consultation and surgery
| Priority classification level | Target time for consultation |
|---|---|
| Priority I | Within 24 hr |
| Priority IIa | 24 hr to 1 wk |
| Priority IIb | 1–3 wk |
| Priority III | Within 6 wk |
| Priority IV | Within 3 mo |
| Priority V | Within 6 mo |
| Priority VI | Within 12 mo |
| All cases | Within 18 mo |
Access targets were applied to 574 diagnoses for both W1 and W2 (Appendix 1). In developing access targets for W1, surgeons specifically considered the uncertainty of diagnostic information. For example, a teenager referred with a nonspecific hip problem might have a slipped capital femoral epiphysis and, therefore, require urgent referral.
Discussion
Although management of wait lists requires accurate data and standardized definitions, wait time information continues to be subjective and/or use nonstandardized definitions, thereby varying among institutions, jurisdictions and provinces.8,9 Our pediatric wait time strategy was a systematic approach to begin to address surgical wait times for children through interinstitutional dialogue and cooperation. The need to create and apply standardized priority ratings was the underlying impetus for our pediatric wait time strategy.
Information from applying these access targets can be used in multiple ways. Surgeons, as individuals or as a group, can manage and triage patients on their surgical wait lists. Surgeons and institutions can share best practices to improve wait list management. Institutions can make decisions about shifting or investing resources to address patient needs. Regions can better understand interinstitutional capacity and possibly manage referrals to better address capacity. Funders like provincial ministries of health can provide targeted funding to reduce wait lists on a provincial basis, as has occurred in Ontario.
Our approach was distinct from the approach for the adult wait time strategy in several ways. First, in contrast to the adult model, the pediatric wait time system captures wait times by diagnoses. This approach was taken because general practitioners and community pediatricians are usually not able to determine the specific appropriate surgical procedure required by the child and, thus, the wait time for consultation is better captured by diagnosis. In addition, not all referrals require surgery; therefore, W1 is better assigned to diagnosis. Furthermore, the total duration of the wait is, at minimum, the summation of W1 and W2, and by using diagnoses the total duration of the wait can be more easily captured. Because the diagnoses are automatically linked to a priority score, using diagnoses reduces the potential for “gaming” by clinicians: deviations from the consensus targets by diagnosis can be easily monitored to ensure clinicians are not persistently and inappropriately altering patient priority. Furthermore, the access targets are explicit and, therefore, reduce the risk that targets are unrealistic or self-serving. Second, in contrast to the adult model, the pediatric wait time strategy, in developing access targets, considered both W1 and W2. Although W1 access targets have not yet been applied, having both W1 and W2 access targets allows the potential to provide a more complete appraisal of surgical wait times for children. Third, whereas the adult model addresses only 5 services, the pediatric wait time strategy is comprehensive, allowing monitoring of service delivery to determine whether an increased volume of targeted procedures is having a detrimental effect on the wait times for other procedures.
The availability of access targets is just 1 aspect of the multifaceted approach needed to reduce wait times for children. First, effective disease and referral management must be in place so that children receive the appropriate diagnosis, referral and triage to a specialist. Second, a wait list management system is needed to monitor wait times and determine trends. Third, information on wait times needs to be shared among physicians, patients, institutions and governments to ensure appropriate responses to excessive wait times for surgery. Fourth, appropriate capacity, such as hospital beds, equipment, operating rooms, surgeons, anesthesiologists and nurses, must be available to respond to service demand and reduce surgical backlogs. Finally, infrastructure should be maximally used and resources should be used in the most efficient manner.
Limitations
This study has several potential limitations. First, our access targets were developed by consensus using clinical expertise and judgment rather than evidence. The strategy, however, involved clinicians who best understood the clinical conditions and the consequences of delayed treatment. Early use of the access targets in Ontario suggests that the targets are clinically sensible. Furthermore, the strategy was based on diagnoses, rather than on a subjective appraisal of acuity, to provide a transparent and objective access target. Finally, these access targets can now be tested in future research to develop evidence-based outcomes. This type of research should initially evaluate cohorts of patients and determine the relation between duration of wait and health consequences. For example, a recent study using administrative data validated that 2 weeks was an appropriate access target for the treatment of inguinal hernia in infants to minimize the risk of incarceration.10 A second limitation is that the access targets need to be applied across Canada.5 Differences between jurisdictions may require future modification of the pediatric wait times model. Finally, the list of diagnoses will inevitably require changes as the lists are used and surgical diagnoses modified.
Conclusion
Timely access to high-quality care is a complex issue requiring immediate attention. The access targets developed in this study provide a comprehensive and standardized approach to prioritizing surgical care for children.
Acknowledgement
We acknowledge the hard work and dedication of the Ontario Children’s Health Network (OCHN) and the OCHN Wait Time Task Force, Paediatric Surgery Subcommittee.
Footnotes
Competing interests: Research was supported by the Wait Time Innovation Fund and the Ontario Ministry of Health and Long-Term Care. Otherwise, none declared.
Contributors: Drs. Wright, Seguin and Booth designed the study. Drs. Wright, Li, Fitzgerald, Jones, Leitch and Willis acquired the data, which was analyzed by Drs. Wright and Li. Drs. Wright and Li wrote the article. All authors reviewed the article and approved its publication.
References
- 1.Mendelsohn M. Canadians’ thoughts on their health care system: preserving the Canadian model through innovation. Ottawa (ON): Commission on the Future of Health Care in Canada; 2002. [accessed 2006 May 16]. Available: www.hc-sc.gc.ca/english/pdf/romanow/pdfs/MendelsohnEnglish.pdf. [Google Scholar]
- 2.Canadian Institute for Health Information. Waiting for health care in Canada: what we know and what we don’t know. Ottawa (ON): The Institute; 2006. [accessed 2010 Dec. 21]. Available: http://secure.cihi.ca/cihiweb/products/WaitTimesReport_06_e.pdf. [Google Scholar]
- 3.Health Canada. Wait times in Canada. 2006. [accessed 2006 Jun. 1]. Available: www.hc-sc.gc.ca/hcs-sss/qual/acces/wait-attente/index_e.html.
- 4.Edwards NC, Riley BL. Can we develop wait lists for public health issues. CMAJ. 2006;174:794–6. doi: 10.1503/cmaj.050731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadorn DC. Setting priorities for waiting lists: defining our terms. Steering Committee of the Western Canada Waiting List Project. CMAJ. 2000;163:857–60. [PMC free article] [PubMed] [Google Scholar]
- 6.Sheldon TA, Guyatt GH, Haines A. Getting research findings into practice: when to act on the evidence. BMJ. 1998;317:139–42. doi: 10.1136/bmj.317.7151.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raine R, Sanderson C, Black N. Developing clinical guidelines: a challenge to current methods. BMJ. 2005;331:631–3. doi: 10.1136/bmj.331.7517.631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Canadian Institute for Health Information. Surgical Volume Trends, 2008 Within and beyond wait time priority areas. Ottawa (ON): The Institute; 2008. [Google Scholar]
- 9.Lewis S, Barer ML, Sanmartin C, et al. Ending waiting-list mismanagement: principles and practice. CMAJ. 2000;162:1297–300. [PMC free article] [PubMed] [Google Scholar]
- 10.Zamakhshary M, To T, Guan J, et al. Risk of incarceration of inguinal hernia among infants and young children awaiting elective surgery. CMAJ. 2008;179:1001–5. doi: 10.1503/cmaj.070923. [DOI] [PMC free article] [PubMed] [Google Scholar]