Abstract
In contemporary clinical practice, the prevalence of neck pain in the general population is approximately 15%. The challenge for the primary care specialist is to be able to recognize the more serious disorders that require early referral. Additionally, it is important to have the confidence to institute specific treatment for nonurgent conditions in order to avoid unnecessary referral of patients with generally self-limiting conditions.
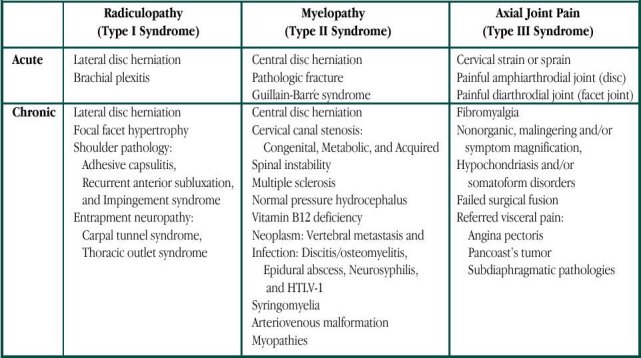
Cervical spondylosis is a general and nonspecific term that encompasses a broad spectrum of afflictions but, for purposes of clarity, can be organized into three clinical syndromes: Type I Syndrome (Cervical Radiculopathy); Type II Syndrome (Cervical Myelopathy); and Type III Syndrome (Axial Joint Pain). It is important to remember that shoulder problems can masquerade as cervical problems, and vice versa (e.g. adhesive capsulitis, recurrent anterior subluxation, impingement syndrome, rotator cuff tear, etc.). A number of management options, including pharmaceutical, physical therapy, and psychological therapies, are available once a diagnosis has been made.
The diagnosis and treatment of painful conditions affecting the cervical spine has always challenged physicians. At the turn of the last century, with the development of roentgen ray examinations, spinal “arthritis” was recognized to be a potential cause of neurologic compromise. In the mid-1930s, the independent and simultaneous appearance in the medical literature of two landmark articles, one by Mixter and Barr and the other by Peet and Echols, led to the rapid and widespread acceptance of the clinical importance of the intervertebral disc (1, 2). Dr. Dean Echols subsequently founded the Department of Neurosurgery at Ochsner Clinic. His pioneering efforts have been continued and extended by his neurosurgical colleagues, residents, and successors.
In contemporary clinical practice, several epidemiological studies indicate that the prevalence of neck pain in the general population is approximately 15%. In the workers compensation arena, the prevalence of various sorts of neck complaints is even higher. Not even physicians are immune to this affliction as it seems the frequent performance of procedures requiring awkward neck positions predispose the practitioner to the development of cervical pain (3).
Most people who develop neck problems never seek medical attention. Those that do present for treatment generally have relatively minor disorders that tend to resolve with or without specific treatment. The challenge for the primary care specialist is early recognition of the more serious disorders for early referral and knowing when to refer those other patients who fail to respond to treatment. Therefore, the emphasis of this brief review is on the differential diagnosis, focusing especially on the more commonly encountered disorders, and management options.
Cervical Spondylosis
The basic concepts that relate to similar conditions in the lumbar spine are essentially identical to those that apply in the neck; the following discussion, however, will focus on the cervical spine. Cervical spondylosis is a general and nonspecific term that refers to the degenerative changes that develop either spontaneously with age, or secondarily as the result of trauma or other pathological condition. These changes develop slowly. The earliest event is probably a biochemical change in the substance of the disc, resulting in decreased water content. This causes an alteration in the biomechanics of the spine due to loss of the shock absorber-like action of the discs. As a result, secondary changes occur in the other component tissues (facet joints and ligaments) comprising the other elements of articulation between the vertebrae. The human body reacts to this abnormal state by attempting to heal the spine in the same way it deals with long bone fractures—by producing bridging bony deposits called marginal osteophytes (i.e. “spurs”). If this process successfully goes to completion, it results in an auto-fusion. Kirkaldy-Willis conceived of this process as passing through three phases:
I. Dysfunction
II. Instability
III. Stabilization (4)
The instability in phase II may either be painful micromotion or frank subluxation (i.e. degenerative spondylolisthesis). Ultimately, the elder spine becomes shorter (due to loss of disc height) and stiffer (due to the spontaneous auto-fusion). Sometimes this process goes all the way to completion whereas in other patients it will stop and fail to progress. Occasionally the chronic clinical course is complicated by a superimposed acute disc herniation. The displaced nucleus pulposus and/or bulging annulus fibrosis is called a “soft” disc herniation. In contrast, the slowly developing calcified enlargement of a posterior marginal osteophyte is called a “hard” disc herniation. Both types may coexist, as they are different manifestations of the same clinical spectrum.
Like death and taxes, cervical spondylosis would seem to be unavoidable. The radiographic appearance of human spines reflects this fact. By age 60–65, 95% of nonsymptomatic men and 70% of nonsymptomatic women show a least one degenerative change on plain films (5). Therefore, the mention of degenerative change on an x-ray report is not necessarily a cause for concern. As our radiological colleagues correctly point out, “clinical correlation is recommended.”
The Clinical Syndromes of Cervical Spondylosis
From a statistical standpoint, cervical spondylosis is usually associated with mild self-limiting aches and pains or is not symptomatic at all. Nevertheless, individual patients may develop symptoms. Three distinct clinical syndromes can result from cervical spondylosis:
Type I. Cervical Radiculopathy
Type II. Cervical Myelopathy
Type III. Axial Joint Pain, a.k.a. mechanical neck pain, motion segment pain, “discogenic” pain, facet syndrome, painful instability, etc. (6).
The first two reflect neurologic involvement, whereas the third represents painful joint dysfunction. There is often overlap between these syndromes, which can coexist simultaneously. For purposes of clarity, however, they will be discussed separately.
Cervical Radiculopathy (Type I Syndrome)
Cervical radiculopathy is the easiest syndrome to recognize and its clinical manifestations of neck pain with radiating upper extremity pain and/or weakness and/or numbness are familiar to every physician. Radiculopathy is caused by combined compression and inflammation of a spinal nerve. Both factors are necessary. This can be caused by either an acute “soft” disc, chronic “hard” disc, or more rarely by posterior compression from a hypertrophied facet joint.
The distribution of the upper extremity signs and symptoms correspond to a specific nerve root, with characteristic reflex, motor, and sensory loss. The two most common sites are the C5–6 disc (C6 nerve root) and the C6–7 disc (C7 nerve root). In the fully developed form, C6 deficit includes a decreased bracialradialis reflex, weakness of the biceps muscle, and pain and/or paresthesias radiating down the arm to the thumb and index finger (“six-shooter” pattern). In contrast, involvement of the C7 root would cause loss of the triceps reflex, weakness of the triceps muscle, and pain and/or paresthesias radiating to the middle finger.
In the absence of objective neurologic deficit, three clinical signs are useful in diagnosing the presence of cervical radiculopathy. The first is the Spurling sign. Bending the neck laterally so that the ear approximates the shoulder safely performs the Spurling maneuver. This should be done without rotation but with some cervical extension. In other words, the patient looks straight ahead and up while attempting to touch the ear to the shoulder. If pain is increased with lateral bending toward the painful arm, radiculopathy is suggested (this maneuver tends to close the neural foramen). On the other hand, if it is more painful to laterally bend away from the side of the painful arm, then a nonspecific soft tissue etiology is presumed (pain from further stretching of bruised or stretched musculo-ligamentous structures).
Two additional mechanical signs strongly suggest the presence of cervical radiculopathy: One is the relief of radiating extremity pain by applying manual traction to the neck. The other is relief of pain by placing and resting the patient's forearm on the top of the head. In fact, a few patients will have discovered the latter maneuver by themselves and adopt that position spontaneously.
These three mechanical signs have high specificity but only about 50% sensitivity. Therefore, the presence of these signs strongly suggests cervical radiculopathy. If these signs are absent, however, the diagnosis of cervical radiculopathy is by no means excluded (7).
Cervical Myelopathy (Type II Syndrome)
The posterior longitudinal ligament is strongest in the midline, which directs most disc herniations off to one side or the other—toward a nerve root and away from the spinal cord. Sometimes, however, either from acute or chronic processes, the spinal cord itself is involved. The recognition of severe cervical myelopathy is straightforward because the clinical manifestations are so dramatic. There is weakness of all four extremities together with a sensory level below which there is reduced or absent appreciation of pain, touch, vibration, or position sense. Reflexes are too brisk and may be self-sustaining as with ankle clonus. Muscular tone is increased and some degree of rigidity of the extremities is present. This increased muscle tone is also present in the bladder wall, producing frequency and nocturia. In advanced cases, there may even be sphincter disturbance, although this is rare in the absence of significant trauma.
Pathological reflexes are also present. Hoffmann's sign and Babinski's sign are important clinical manifestations. Flicking the middle finger nail and observing a reflex clawing flexion of the thumb and the other digits elicit Hoffman's sign. Babinski's sign is familiar to most physicians and describes extension of the big toe and fanning of the other toes in response to stroking the sole of the foot. With acute or advanced cervical myelopathy, the diagnosis is usually clear and the need for early referral for neurosurgical consultation is obvious.
The diagnosis of chronic or early cervical myelopathy can be extremely difficult as the signs and symptoms are notoriously subtle. The patient will often complain of difficulty with fine movements and control of the fingers. Fastening and unfastening buttons, for example, can become difficult. The gait disturbance may be described as a sense of unsteadyness, rather than weakness. Sensory loss is highly variable and sometimes takes the form of “glove-and-stocking” distribution that is often seen in peripheral neuropathy. A mild peripheral neuropathy often occurs normally in the elderly and is often nonsymptomatic except for loss of the ankle reflex. When this coexists with chronic myelopathy, the expected increase in deep tendon reflexes may be masked. Increased tone may be the only abnormal sign in the lower extremities. This is checked by asking the seated patient to dangle the legs as loosely as possible off the edge of the examination table. Grasp the lower leg and shake it gently back and forth—the foot and ankle should be floppy. If instead the lower leg, ankle, and foot move together stiffly as a unit, myelopathy should be suspected.
Two clinical signs are useful in detecting subtle myelopathy in the upper extremities. Ono et al described both of these: the Finger Escape and Grip-and-Release signs (8). To perform the Grip-and-Release test, the examiner measures the speed at which the patient's hand can alternate between closing into a fist and full finger extension. Normal adults can perform rapid complete grip and release to full finger extension 20 times in 10 seconds. This not only becomes slower but, in advanced cases, exaggerated wrist flexion occurs with attempted finger extension and exaggerated wrist extension occurs with finger flexion. Care must be taken to keep the wrist in a neutral position. The Finger Escape sign is elicited by observing that it is impossible for the patient to keep the fully extended fingers completely adducted. Instead, there is an irresistible tendency for the fingers, especially the little finger, to spread apart.
It is important to keep a high index of suspicion of this clinical entity because the diagnosis by physical examination alone is quite challenging. In addition, the natural history of relatively mild cervical spondylitic myelopathy is still poorly defined. The rate of progression of myelopathy is unpredictable. Deterioration usually occurs slowly and long periods of constancy are commonly observed. Rapid worsening can, however, tragically occur. Once severe neurologic deficits are present, they are unlikely to resolve spontaneously. Indeed, even appropriate surgical intervention may not be able to recover lost function.
Type III Syndrome
The world can be divided into “lumpers” and “splitters” and, because this article is intended for a general audience, we will fall in with the former group and consider Type III Syndrome to be a single entity. In reality, however, it encompasses a heterogeneous collection of etiologies. These diverse conditions share in common the fact that joint dysfunction in the spine can be painful. In the appendicular skeleton, it is well known that pathologic hip and shoulder joints, for example, can be sources of pain. By extension, it should be clear that joints in the axial skeleton could produce pain syndromes as well.
The two types of joints in the adult spine include 1) diarthrodial joints (synovial joints of the gliding variety including not only the facet joints but also the costovertebral, atlantoaxial, and sacroiliac joints) and 2) amphiarthrodial joints, which are slightly moveable nonsynovial joints with two subtypes: Symphysis Type (the fibrocartilage of the intervertebral disc) and the Syndesmotic Type (the ligamentum flava, as well as the intertransverse, intraspinous, and supraspinous ligaments). The point is that the structures, which join the vertebral bones together to form the spinal column, are complex joints.
Type III syndrome is characterized by neck pain together with radiation to one or more of the following: the medial scapula, chest wall, shoulder area, and head. There may be a vague aching referred to the proximal upper extremity but pain referred below the elbow suggests nerve root involvement. In a pure Type III Syndrome there is no neurologic deficit because the symptoms stem from a joint(s). Headaches are usually associated with cervical muscle spasm and present occipitally, sometimes with secondary frontal radiation. Pain referred to the medial border of the scapula is particularly important to recognize since lack of awareness of this common symptom can lead to unnecessary scans of the thoracic spine. As with motion of painful joints elsewhere, movement of the neck produces pain, and pain is relieved by rest and immobilization. There should be a significant correlation between activity and pain. Theoretically, a neck brace should cause improvement, but in fact, the response is inconsistent. This is because even a hard collar is unable to completely immobilize the neck.
Differential Diagnosis
The differential diagnosis of cervical spondylosis is presented in Table 1. A complete discussion is beyond the scope of this article; however, a few points are worth mentioning. Brachial plexitis, or brachial plexus neuropathy, is a rare condition but one with a dramatic presentation. Onset of pain is sudden and severe. After a variable period of usually a few weeks, the pain is replaced by weakness. The prognosis is generally favorable with spontaneous recovery, but the rate of recovery is over months to years. The etiology is unknown, and about half of patients report antecedent illness or immunization.
It is important to remember that shoulder problems can masquerade as cervical problems, and vice versa. Adhesive capsulitis, or “Frozen Shoulder,” is characterized by loss of passive range of motion in all degrees, especially external rotation, and can be seen in conjunction with cervical radiculopathy, especially in the elderly. Whether it is secondary to disuse of the joint because of the painful radiculopathy or whether it represents a forme fruste of reflex sympathetic dystrophy is unclear. Recognition of this entity is important because it may persist following resolution of the radiculopathy, and specific treatment may be required.
Recurrent anterior subluxation, or “Dead Arm Syndrome,” occurs primarily in young throwing athletes. Partial anterior dislocation at the glenohumeral joint is associated with vague distal numbness and tingling of the arm, which can superfically resemble a radiculopathy. Impingement Syndrome includes tendinitis of the supraspinatus tendon (less commonly, long head of the biceps tendon) and can result in radiation of pain distally down the arm, mimicking a cervical radiculopathy. Calcific deposits can occur in a chronically inflamed tendon causing sudden intense pain (sometimes referred to as bursitis). Ultimately, a tear may occur at the tendinous insertion of the supraspinatus muscle into the joint capsule (Rotator Cuff Tear). Unlike the situation in Frozen Shoulder, there is full passive range of motion – but it hurts. External rotation is weak, and power in the first 90 degrees of abduction is often lost (“falling arm sign”). In summary, when the patient reports pain when the examiner moves the shoulder – suspect a shoulder joint problem.
Carpal Tunnel Syndrome is a very common condition, and may occur in association with a cervical radiculopathy (“double crush syndrome”). Painful numbness occurs especially at night, characteristically awakening the patient. In the morning, many patients try to shake the hand awake. Tinel's sign is positive at the wrist, and palmar thumb abduction (perpendicular to the plane of the palm) is weak. A wrist splint at night coupled with a NSAID and Vitamin B6 (pyridoxine) is therapeutic in mild cases.
Fibromyalgia, or fibrocytis, is a common syndrome of unknown cause. There is widespread pain, tenderness to palpation at many different points, and associated symptoms including some or all of the following: fatigue, morning stiffness, tingling paresthesias, anxiety, headache, prior depression, and irritable bowel. There is no specific diagnostic test, and indeed, it is a diagnosis of exclusion that responds poorly to treatment. Management is frustrating for both the physician and the patient as illustrated by the following quotation: “Usually when I go to see the doctors I tell them about the pain that's worst. If I tell them about everything, they think I'm nuts” (9). Recognition of this affliction is essential in order to avoid well-intentioned efforts at surgical intervention.
Management Options
Most patients who develop symptoms because of cervical spondylosis have self-limiting conditions. A double blind, controlled, multicenter trial of placebo versus NSAID plus muscle-relaxer was conducted on patients with acute musculoskeletal pain and associated spasm of the neck or low back. There was initial improvement in the treatment group, and this difference was statistically significant. However, by 10 days the difference had disappeared. The explanation was not that the medicines lost their effectiveness, but rather that the placebo group spontaneously improved (10). In patients with a normal neurological examination, it might make sense to treat initially with acetaminophen and avoid the potential side effects of NSAIDs.
When patients present with signs or symptoms of cervical radiculopathy, the neurologic examination is important. Significant motor weakness indicates the need for early but nonemergent surgical referral; otherwise, a nonsurgical regimen can be considered. Lateral flexion and extension cervical X-rays should be obtained to exclude the presence of frank instability or other significant structural problems. The mainstay of treatment is the combination of an NSAID and cervical traction. Simple over-the-door home traction devices are available, and sometimes, personal instruction by a therapist reassures the patient. Recommendations are based on body habitus and normal x-rays. Usually starting with 8 pounds for 20 minutes 3 times daily is a safe approach. In muscular males with large necks, it may be necessary to slowly work up to 15 pounds. Traction will aggravate cervical muscle spasm but is usually successful in reducing the radicular component of pain down the arm. Temporal mandibular joint problems are a relative contraindication to traction. Supervised traction in a physical therapy setting can also be helpful, but generally, home treatment is just as effective. Muscle relaxers and analgesics may also be added. Although 4 to 6 weeks is a reasonable duration for this approach, earlier surgical referral is always at the discretion of the treating physician. MRI scans are usually diagnostic, but occasionally the surgical consultant may also need to obtain a myelogram/CT scan combination. The referring physician generally should not order an ordinary CT scan since this test by itself is rarely helpful in the management of cervical spondylosis. The results of surgical intervention in cases of persistent cervical radiculopathy with a clear radiological diagnosis are usually very good.
A diagnosis of cervical myelopathy calls for specialty referral, and it is often helpful if a cervical MRI scan is available at the time of consultation. The decision for surgery is individualized since the natural history and rate of progression of mild myelopathy are uncertain. However, surgical intervention is more strongly considered when the symptoms are advanced or the radiographic findings are impressive. Because the older technique of simple laminectomy often yielded low rates of improvement in advanced cases, more complete and thorough surgical approaches have been developed. In these very difficult patients, some gratifying results have been obtained (11, 12).
The primary treatment for a patient with the symptoms of Type III Syndrome is “tincture of time.” In fact, they will initially be identified as suffering with cervical “sprain” or “strain.” Usually these symptoms resolve; however, in a few patients the symptoms become chronic. It is in this group that the diagnosis of Type III Syndrome may be considered.
Some experienced physicians deny the existence of Type III Syndrome as a bona fide entity. There are several understandable reasons for this skeptical attitude. The neurological examination is normal. The manifestations are primarily subjective, as no one yet has invented a “pain meter.” Cervical muscle spasm can be objectively assessed with biofeedback equipment, but its presence is not a requirement for the diagnosis. The radiographic correlation is poor since asymptomatic cervical spondylosis on plain films, myelograms, and MRIs is found with normal aging (5, 13, 14).
The management of Type III Syndrome is difficult as well. Indeed, some patients are incurable. If significant cervical spasm is present with secondary muscle contraction-type headaches, a specific treatment can be offered. Biofeedback training in the Department of Psychiatry for the development of muscle relaxation techniques is often very helpful for this particular symptom (15) and can also provide a back door entry to a psychological pain management approach that might otherwise be unacceptable to the patient. Sometimes a “conservative” approach employing long-term physical therapy as well as many “therapeutic” injections is adopted. The real utility of these expensive modalities should be examined as carefully, and with as much scrutiny, as surgical interventions. Chronic undiagnosed pain is frustrating for the physician, and well-intentioned efforts are laudable. However, in the chronic low back pain arena, a double blind, prospective, controlled study showed that epidural steroid treatment worked well but was no better than intramuscular injection (16). Similarly a double blind, placebo controlled trial evaluating facet injections with steroids failed to produce any sustained improvement (17).
While therapeutic injections have questionable value, diagnostic injections can be very helpful. The main difficulty in Type III Syndrome is finding the source of the pain, the so-called “pain generator.” Diagnostic injections help to identify the pain generator(s) either by re-recreating the pain or by temporarily relieving the pain. While details would be beyond the scope of this article, a brief exposition of this concept may be helpful. In general, the spinal column can be divided into an anterior column (discs and vertebrae) and a posterior column (facet joints). MRI scans and discography (validated by the presence of a normal control level) is used to evaluate the anterior column, whereas single photon emission computed tomography (SPECT) scans and facet injections are used to investigate the posterior column (18, 19). If the pain generator(s) can be identified, surgical intervention can be considered. Careful psychological evaluation is essential in order to maximize the potential for improvement. This is done before even considering discography (20, 21). A Minnesota Multiphasic Personality Inventory (MMPI) with an interview by a clinical psychologist is used for screening, with referral to a pain management psychiatrist/psychologist team if indicated. Any coexistent depression and/or anxiety must be recognized and treated prior to surgery. In one long-term follow-up study, the adverse effects of compensation status on surgical results diminished over time. However, psychological disturbance continued to exert a statistically significant negative effect on clinical outcome even 10 years after fusion surgery (22). It is also essential to treat nicotine addiction, as both experimental and clinical studies confirm a strong negative effect on outcome (23–25).
Even with very thorough screening and diagnosis, the surgical results in patients with Type III syndrome are the least favorable as a group. Nevertheless, it is possible to obtain satisfactory results in carefully selected cases (26).
Acknowledgments
The author would like to thank Michael Wilson, MD, Associate Chairman and Director of Residency Training of the Department of Orthopedics at Ochsner Clinic and Alton Ochsner Medical Foundation, for assistance in preparing the discussion on shoulder pain.

Dr. Voorhies is the Chariman of Ochsner's Neuorsurgery Department.
Table 1.
Differential Diagnosis of Clinical Syndromes Resembling Cervical Spondylosis.
References
- Mixter W. J., Barr J. S. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–215. [Google Scholar]
- Peet M. M., Echols D. H. Herniation of the nucleus pulposus. A cause of compression of the spinal cord. Arch Neurol Psychiat. 1934;32:924–932. [Google Scholar]
- Whitaker R. H., Green N. A., Notley R. G. Is cervical spondylosis an occupational hazard for urologists? Brit J Urol. 1983;55:585–587. doi: 10.1111/j.1464-410x.1983.tb03380.x. [DOI] [PubMed] [Google Scholar]
- Yong-Hing K., Kirkaldy-Willis W. H. The three-joint complex. :80–87. In: The Lumbar Spine. Weinstein JN, Wiesel SW, International Society for the Study of Lumbar Spine. Philadelphia: W.B.Saunders, 1990. p. [Google Scholar]
- Gore D. R., Sepic S. B., Gardner G. M. Roentgenographic findings of the cervical spine in asymptomatic people. Spine. 1986;11:521–524. doi: 10.1097/00007632-198607000-00003. [DOI] [PubMed] [Google Scholar]
- Voorhies R. M. Managing the more common cervical disorders. IM Int Med. 1996;17:18–41. [Google Scholar]
- Viikari-Juntura E., Porras M., Laasonen E. M. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine. 1989;14:253–257. doi: 10.1097/00007632-198903000-00003. [DOI] [PubMed] [Google Scholar]
- Ono K., Ebara S., Fuji T. Myelopathy hand. New clinical signs of cervical cord damage. J Bone Joint Surg Br. 1987;69:215–219. doi: 10.1302/0301-620X.69B2.3818752. [DOI] [PubMed] [Google Scholar]
- Wolfe F. Fibromyalgia. Seminars in Spine Surgery. 1995;7:200–212. [Google Scholar]
- Basmajian J. V. Acute back pain and spasm. A controlled multicenter trial of combined analgesic and antispasm agents. Spine. 1989;14:438–439. [PubMed] [Google Scholar]
- Awasthi D., Voorhies R. M. Anterior cervical vertebrectomy and interbody fusion. Technical note. J Neurosurg. 1992;76:159–163. doi: 10.3171/jns.1992.76.1.0159. [DOI] [PubMed] [Google Scholar]
- Ratliff J., Thomas N., Voorhies R. M. Treatment of Severe Cervical Sponylosis via Combined Anterior and Posterior (360 degree) Decompression and Fusion. 2000 Initial Results. (poster presentation). Presented to the American Association of Neurological Surgeons / Congress of Neurological Surgeons Joint Section on Spine and Peripheral Nerves: Section of Spine and Peripheral Nerves: Indian Wells, California. [Google Scholar]
- Hitselberger W. E., Witten R. M. Abnormal myelograms in asymtomatic patients. J Neurosurg. 1968;28:204–206. doi: 10.3171/jns.1968.28.3.0204. [DOI] [PubMed] [Google Scholar]
- Boden S. D., McCowin P. R., Davis D. O. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:1178–1184. [PubMed] [Google Scholar]
- Hudzinski L. G. Neck musculature and EMG biofeedback in treatment of muscle contraction headache. Headache. 1983;23:86–90. doi: 10.1111/j.1526-4610.1983.hed2302086.x. [DOI] [PubMed] [Google Scholar]
- Goupille P., Gouthiere C., Jattiot F. Epidural versus intramuscular steroids in 31 patients with chronic low back pain. Double-blind, perspective study. Arthritis Rheum. 1993;36S:S170, B173. [Google Scholar]
- Carette S., Marcoux S., Truchon R. A controlled trial of corticosteroid injections into facet joints for chronic low back pain. N Engl J Med. 1991;325:1002–1007. doi: 10.1056/NEJM199110033251405. [DOI] [PubMed] [Google Scholar]
- Dolan A. L., Ryan P. J., Arden N. K. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996;35:1269–1273. doi: 10.1093/rheumatology/35.12.1269. [DOI] [PubMed] [Google Scholar]
- Aprill C. N. R. Diagnostic disc injection. :403–442. In: Adult Spine: Principles and Practice. Frymoyer JW, Editor in Chief. New York: Raven Press, Ltd, 1991. p. [Google Scholar]
- Block A. R., Vanharanta H., Ohnmeiss D. D. Discographic pain report. Influence of psychological factors. Spine. 1996;21:334–338. doi: 10.1097/00007632-199602010-00017. [DOI] [PubMed] [Google Scholar]
- Carragee E. J., Chen Y., Tanner C. M. Can discography cause long-term back symptoms in previously asymptomatic subjects? Spine. 2000;25:1803–1808. doi: 10.1097/00007632-200007150-00011. [DOI] [PubMed] [Google Scholar]
- Penta M., Fraser R. D. Anterior lumbar interbody fusion. A minimum 10-year follow-up. Spine. 1997;22:2429–2434. doi: 10.1097/00007632-199710150-00021. [DOI] [PubMed] [Google Scholar]
- Carpenter C. T., Dietz J. W., Leung K. Y. Repair of a pseudarthrosis of the lumbar spine. A functional outcome study. J Bone Joint Surg Am. 1996;78:712–720. doi: 10.2106/00004623-199605000-00011. [DOI] [PubMed] [Google Scholar]
- Silcox D. H., III, Daftari T., Boden S. D. The effect of nicotine on spinal fusion. Spine. 1995;20:1549–1553. doi: 10.1097/00007632-199507150-00001. [DOI] [PubMed] [Google Scholar]
- Daftari T. K., Whitesides T. E., Jr, Heller J. G. Nicotine on the revascularization of bone graft. An experimental study in rabbits. Spine. 1994;19:904–911. doi: 10.1097/00007632-199404150-00007. [DOI] [PubMed] [Google Scholar]
- Ratliff J., Voorhies R. M. Surgical Treatment of Axial Neck Pain. South Med J. (2001 in press) [PubMed] [Google Scholar]


