Abstract
Background
The evidence base for trauma-focused cognitive behavioral therapy (TF-CBT) to treat posttraumatic stress disorder (PTSD) in youth is compelling, but the number of controlled trials in very young children is few and limited to sexual abuse victims. These considerations plus theoretical limitations have led to doubts about the feasibility of TF-CBT techniques in very young children. This study examined the efficacy and feasibility of TF-CBT for treating PTSD in three through six year-old children exposed to heterogeneous types of traumas.
Methods
Procedures and feasibilities of the protocol were refined in Phase 1 with 11 children. Then 64 children were randomly assigned in Phase 2 to either 12-session manualized TF-CBT or 12-weeks wait list.
Results
In the randomized design the intervention group improved significantly more on symptoms of PTSD, but not on depression, separation anxiety, oppositional defiant, or attention deficit/hyperactivity disorders. After the waiting period, all participants were offered treatment. Effect sizes were large for PTSD, depression, separation anxiety, and oppositional defiant disorders, but not attention-deficit/hyperactivity disorder. At six-month follow-up, the effect size increased for PTSD, while remaining fairly constant for the comorbid disorders. The frequencies with which children were able to understand and complete specific techniques documented the feasibility of TF-CBT across this age span. The majority were minority race (Black/African-American) and without a biological father in the home, in contrast to most prior efficacy studies.
Conclusions
These preliminary findings suggest that TF-CBT is feasible and more effective than a wait list condition for PTSD symptoms, and the effect appears lasting. There may also be benefits for reducing symptoms of several comorbid disorders. Multiple factors may explain the unusually high attrition, and future studies ought to oversample on these demographics to better understand this understudied population.
Keywords: posttraumatic stress disorder, cognitive behavioral therapy, children
Introduction
Among interventions available for posttraumatic stress disorder (PTSD) in youth, trauma-focused cognitive-behavioral therapy (TF-CBT) has the largest controlled evidence base and has consistently been shown to be effective (Silverman et al., 2008). These conclusions were based on randomized trials that involved primarily school-aged and adolescent youth. However, only two randomized studies have focused exclusively on young children and both were limited to those exposed to sexual abuse. Thirty-nine 3–6 year old children were randomly assigned to 12 individual sessions of TF-CBT or nondirective supportive therapy (Cohen & Mannarino, 1996). The TF-CBT group improved significantly more than the supportive therapy group on Total Behavior Problems and the Internalizing scale of the Child Behavior Checklist, however a PTSD measure was not employed in this study. In a second study, 44 2–8 year old children were randomly assigned to 11 group sessions of TF-CBT group or supportive educational group treatment (Deblinger, Stauffer, & Steer, 2001). Both groups improved on PTSD symptoms, however the TF-CBT group did not improve more, perhaps because the TF-CBT group was not asked to speak about their own experiences due to their young ages.
While both of these randomized studies with young children were encouraging, several limitations needed addressing. First, only the Deblinger et al study used an outcome measure of PTSD, and found no difference between TF-CBT and supportive groups. The evidence for reducing PTSD symptoms in young children is thus slim. Second, both studies were limited to children with sexual abuse. Noting such gaps, rightly or wrongly, when the first federally-funded programs to train clinicians to treat children for PTSD were created, following the 2001 World Trade Center attacks and the 2004 Florida hurricane season, preschool children were left out of these large and important programs because of the perception that there were no sufficient protocols for disasters for this age group (Allen, Saltzman, Brymer, Oshri, & Silverman, 2006; CATS Consortium, 2007). Voicing similar concerns, Grave and Blisset (2004) published a theoretical review questioning whether CBT was developmentally appropriate for “young children.” At question has been whether young children have developed mature enough skills in causal reasoning, perspective taking, self-reflection, linguistic ability, and memory to engage in the cognitive aspects of CBT. However, their age span for young children was 5–8 years, tacitly indicating that the use of CBT for children younger than 5 years of age was perhaps even more out of reach (Grave & Blissett, 2004).
To this extent there is a gap of documented feasibility for young children to be able to understand and cooperate with the essential TF-CBT techniques across the range of elements needed in a full protocol. While the Cohen and Mannarino (1996) and Deblinger et al (2001) studies both used rigorous methods to ensure therapist fidelity to the treatment protocols, there were no data published on the actual feasibility of the TF-CBT techniques for the children. In other words, the therapists appropriately followed the protocols, but there were not separate ratings on whether children appeared to understand each element of the protocol. These concepts may obviously go hand in hand, but apparently are not assumed in this age group (Allen et al., 2006; CATS Consortium, 2007). Thus, another major aim of this project was to provide the first systematic data on the feasibility of specific TF-CBT techniques in very young children.
In sum, the goals of this study were to provide efficacy and feasibility data to extend the TF-CBT model in young children beyond those exposed to sexual abuse. Hypothesis 1 was that PTSD symptoms would significantly decrease with a 12-session TF-CBT intervention compared to those on a 12-week wait list. If children in the wait condition still met inclusion criteria following the wait period, they received the TF-CBT treatment and were combined to form a single group for the purpose of estimating effect sizes, for 6-month follow-up, and for examining feasibility (content understanding). Hypothesis 2 was that the effect size for the treatment would be large (Cohen’s d 0.7 or larger) (Cohen, 1988) and therefore comparable to TF-CBT studies in older youth. Given the common finding of comorbid disorders with PTSD, an ancillary goal was to examine the treatment effect sizes on major depression disorder (MDD), separation anxiety disorder (SAD), oppositional defiant disorder (ODD), and attention-deficit/hyperactivity disorder (ADHD). Finally, to demonstrate the feasibility of the TF-CBT techniques, hypothesis 3 was that the main content would be successfully understood and completed by the majority of the children. Moving beyond therapist fidelity checklists, this study collected the first explicit data on the feasibility of young children to accomplish specific TF-CBT techniques.
Methods
Methods and results were reported following the Consolidated Standards of Reporting Trials (CONSORT) statement (Altman et al., 2001) Participants
Inclusion criteria were (1) experienced a life-threatening traumatic event. (2) Age between 36 and 83 months at the time of the most recent trauma and at the time of enrollment. (3) Four or more PTSD symptoms with at least one of them being a reexperiencing symptom from criterion B or an avoidance symptom from criterion C. A reexperiencing or avoidance symptom was required for the exposure exercises to be salient in TF-CBT. Exclusion criteria: (1) Head trauma with Glascow Coma Scale score of 7 or less in the emergency room. (2) Mental retardation, autistic disorder, blindness, deafness, and foreign language speaking families.
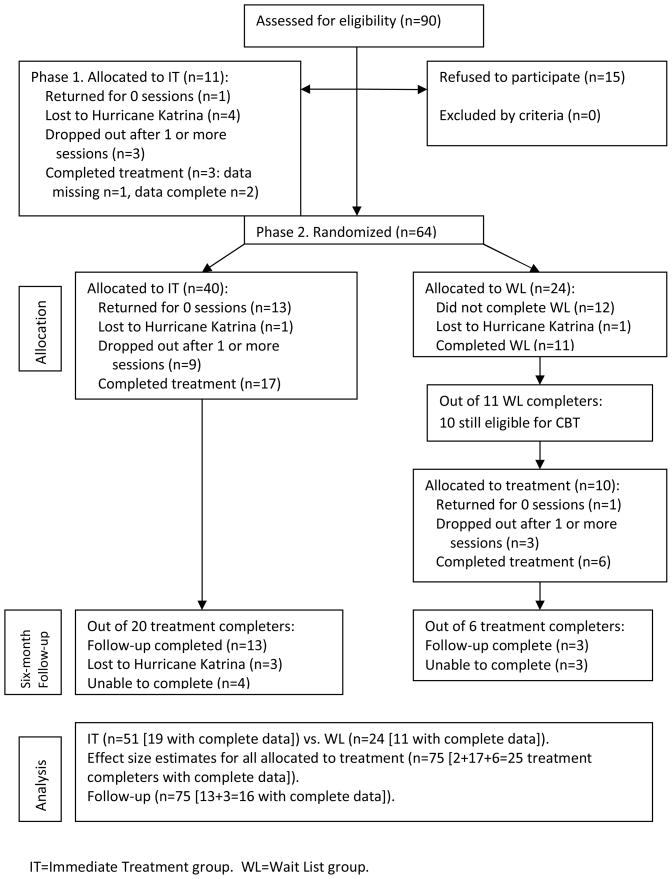
The main source of participants was an ongoing assessment study of trauma-exposed 3–6 year old children (R01MH065884). These participants were recruited for three types of trauma exposures. Children who suffered acute single blow trauma victims were recruited from a Level I Trauma Center. Children who suffered chronic repeated events were recruited through the three main battered women’s programs in the New Orleans metropolitan area. The staff at these programs gave the mothers our phone number. Children who were victims of the Hurricane Katrina disaster were recruited primarily through newspaper ads. After it was known that children met the inclusion and exclusion criteria from being evaluated in the assessment study, then caregivers were approached about participation in this treatment study. Eight-five participants were approached through this process. An additional five participants were enrolled by word of mouth outside of this process, giving a total of 90 participants assessed for eligibility and approached. Fifteen caregivers refused. Figure 1 shows the flow of participants through each stage.
Figure 1.
Flow chart of group assignment, attrition, treatment completers, and six-month follow-up assessment.
Procedure
Phase 1
The study began March 2005. The first five months of the study were used to pilot the full manual on the initial participants. Eleven children were enrolled in Immediate Treatment (IT). This planned phase was used to systematically measure the success in adapting each technique to this age group and therapist adherence, and then feed back any corrective revisions into the manual for the larger Phase 2. Minor but not major revisions were made in the manual between Phases 1 and 2 (e.g., the teaching of relaxation exercises was broken out of session 3 and moved in to session 4).
Phase 2
The remaining 32 months were used to randomize children to either IT or the Wait List group (WL). A blocked randomization procedure randomly assigned two IT and two WL cases in a block of four to prevent long runs of assignment to either condition. Successive blocks of four were then linked to create a random assignment list with more than enough assignments for the total cases that needed to be randomized. Participants were enrolled by research assistants and then assigned to either IT or WL according to this list that was generated beforehand by the principal investigator (first author). When Hurricane Katrina struck five months after starting the study, all active participants were unable to resume therapy while the city and the university were closed (four participants in Phase 1 and three participants in Phase 2). When Phase 2 was re-started after a six-month hiatus, all new participants were enrolled in IT until therapists were at capacity in order to maximize sample size because of the lost time due to the disaster. Because of this imbalance there were 40 children randomized to IT and 24 children randomized to WL.
After Phase 2, children in the WL group whose PTSD symptoms did not fully remit during the 12 week waiting interval and who still met all the inclusion and exclusion criteria were enrolled in the TF-CBT treatment. Provision of treatment ended in November 2008. After all IT and WL participants completed TF-CBT treatment they were followed up after six months and re-assessed.
Children’s mean age was 5.3 years(SD 1.1), 66.2% male, 59.5% Black/African-American, 35.1% White and 5.4% Other race. Maternal caregivers mean age was 34.8 years (SD 9.7) on average with 13.5 years (SD 2.7) of education. In the United States, 12 years of education represents completion of high school and 16 years represents completion of college. In 2003, 28% of American adults completed college degrees (Stoops, 2004). This was not a highly educated sample. Only 28.4% had biological fathers living in the homes. Phase 1, Phase 2 IT, and Phase 2 WL groups did not differ statistically on these variables.
This study was approved by the Tulane University Institutional Review Board. After being screened for inclusion and exclusion criteria over the phone, caregivers arrived alone at the lab and informed consents obtained. Participants were monetarily compensated for their participation in the assessments but not for the treatment.
Measures
The Preschool Age Psychiatric Assessment (PAPA) (Egger et al., 2006) is a structured psychiatric interview with the caregiver about the child. Modules administered for this study were PTSD, MDD, SAD, ODD, and ADHD. Published test-retest reliability kappas were .73 for PTSD, .72 MDD, .60 for SAD, .57 for ODD, and .74 for ADHD. The PTSD module included developmental modifications to wording of A2 acute reaction, B1 intrusive recollections, B2 nightmares, B3 dissociative experiences, C5 detachment or estrangement, and D2 irritability based on prior empirical work (Scheeringa, Zeanah, Myers, & Putnam, 2003). Two different PTSD diagnoses were calculated with syntax in SAS 9.1 (SAS, Cary, NC): (1) the DSM-IV algorithm; and (2) the alternative algorithm diagnosis that has been validated in multiple studies in young children and is similar to that being proposed for DSM-V (Scheeringa, Zeanah, & Cohen, in press). The alternative algorithm (PTSD-AA) requires only one symptom in criterion C instead of the DSM-IV requirement of three symptoms. Interviewers received extensive training prior to their first live interviews and then throughout the study the principal investigator met individually with interviewers weekly to watch their most symptomatic interviews on videotape in order to prevent drift, critique technique, and correct coding errors.
The Adverse Events Checklist (AEC) is an 8-item yes/no checklist designed for this study. It measures suicidality, homicidality, gravely disabled, hallucinations, worsening of any old symptom, appearance of any new symptom, exposure to new domestic violence, and a category for other.
The Treatment Fidelity Checklist (TFC) is a 141-item checklist created to match the content of the 12 sessions for whether the therapist completed the prescribed tasks. The Adaptability Checklist-Child (ACC) is a 62-item checklist created to match the content of the 12 sessions and is the measure of feasibility for children’s capacities to complete the TF-CBT techniques. TFC and ACC items were rated yes/no. Credit was not given for partial attempts or partial completion of tasks. The therapists completed the ratings after every session. An independent rater (the project coordinator) checked them for reliability from videotape by rating 80.3% of the Phase 1 sessions and 19.6% of the Phase 2 sessions, for a total of 30.7% of the sessions.
Treatment
The therapists followed a highly structured 12 session protocol. TF-CBT techniques that could be applied to this age group were adapted from a manual used in a study to treat sexually abused preschool children (Cohen & Mannarino, 1996). Manual formatting and some treatment elements were adapted from a manual used in one study to treat older children (March, Amaya-Jackson, & Murray, 1998). Other developmental modifications were based on the first author’s clinical and research experience with very young traumatized children.
Specific techniques included psychoeducation about PTSD, recognition of feelings, trainings in coping skills, graduated exposures to trauma-related reminders with three modalities (drawings, imaginal, and in vivo), and safety planning. Primary maternal caregivers were in the room with the children for all of sessions 1, 2, and 12. For all other sessions they observed the children’s sessions on TV (with the children’s knowledge) in order to learn the material simultaneously and with the hope of increasing parents’ attunement to their children, and then the caregivers spent the second half of the sessions alone with the therapists. Caregivers and therapists spent this time alone to help the therapists interpret the children’s words and body language, and to discuss and troubleshoot homework. It was also used in a supportive therapy model for caregivers to provide emotional support and give advice when desired by the caregivers. The manual and the TFC and ACC checklists are available online at http://www.infantinstitute.com/.
Four therapists were used in the study. The experience of the therapists, all licensed social workers, consisted of 10 years experience for one, and the other three were either completing or had recently completed training. They treated 6, 7, 10, and 23 cases respectively. Their self-rated degrees of fidelity to the protocol were 93.0%, 94.6%, 97.4%, and 97.5% respectively, for a total of 96.3%.
An independent rater scored 30.7% of the treatment sessions (n=116 sessions, 1,362 items) for therapist fidelity from videotape and agreed with the therapists 97.1% of the time. The rater and therapists interrater kappa agreement was good at 0.61.
Statistical Analyses
The changes from pre- to post-treatment number of symptoms were tested as repeated measures in random effects regression models with the proc mixed procedure in SAS 9.1 (Cary, NC). The interaction term of group by time was used to identify whether the effect of IT varied significantly from WL. Drop outs and treatment completers were compared on baseline measures with Wilcoxon rank sum tests. Effect sizes for the treatment protocol were estimated as Cohen’s d (Cohen, 1988) with pooled standard deviations. Interrater agreements were compared with the kappa statistic.
Results
Hypothesis 1: Treatment vs. Wait List
Drop outs (not counting those lost to Hurricane Katrina) occurred in equal proportions among the groups (56.4%, n=22, dropped in IT; 52.2%, n=12, dropped in WL), and there were no significant difference on the pre-treatment/pre-wait number of PTSD, MDD, SAD, ODD, or ADHD symptoms between drop outs (n=34) and treatment/wait list completers (n=28) (Wilcoxon rank sum tests). Blacks/African-Americans dropped out at a significantly higher frequency (68.6%, 24 of 35) than Whites (41.7%, 10 of 24) (chi square 4.2, df=1, p<.05). For the test of the participants randomized to IT versus WL groups, the interaction term for Time by Group was significant for PTSD, F=12.97, df=28, p<.005, indicating one group changing differentially in respect to the other over time. The pre- and post-treatment means in Table 1 show a nearly complete absence of improvement in the WL group and substantial improvement in the IT group. When race was entered as a covariate to the model, the Time by Group interaction was unaffected and still significant, F=5.71, df=24, p=.05. Type of traumatic event was entered as a covariate in the model with the index type of trauma for which they were being treated coded as three types, acute injury (n=18), witnessed domestic violence (n=18), and victim of the Hurricane Katrina disaster (n=39). The Time by Group interaction was still significant, F=13.87, df=28, p<.001.
Table 1.
Pre- and post-treatment mean number of symptoms for Wait List group versus Immediate Treatment group comparisons. Means are for treatment completers only. Random effects model tests include all subjects with missing data (n=75).
| Pre-treatment Mean (SD) | Post- treatment Mean(SD) | Effect size per group | Test | ||
|---|---|---|---|---|---|
| Posttraumatic | IT | 7.9 (2.9 | 3.6 (2.9) | 1.48 | Time by Group interaction F=12.97, df=28, |
| stress disorder | WL | 7.7 (2.5) | 7.2 (3.8) | 0.16 | p<.005 |
| Major depressive | IT | 2.8 (2.0) | 0.9 (1.0) | 1.20 | Time F=19.04, df=28, p<.0005. |
| disorder | WL | 3.1 (2.6) | 1.8 (1.9) | 0.57 | Time x Group interaction NS (p=.38). |
| Separation anxiety | IT | 2.1 (1.8) | 0.8 (1.0) | 0.89 | Time F=9.58, df=25, p<.005. |
| disorder | WL | 3.7 (1.6) | 2.0 (2.3) | 0.86 | Time x Group interaction NS (p=.54). |
| Oppositional | IT | 4.5 (2.6) | 2.2 (1.8) | 1.03 | Time F=8.28, df=26, p<.01. |
| defiant disorder | WL | 3.9 (1.8) | 3.6 (2.6) | 0.13 | Time x Group interaction NS (p=.26). |
| Attention-deficit/ | IT | 7.8 (5.1) | 5.0 (5.1) | 0.55 | Time (p=.58) and Time x Group interaction |
| hyperactivity disorder | WL | 7.7 (6.3) | 8.4 (5.4) | -0.12 | (p=.16) both NS. |
Degrees of freedom vary in the tests because a few subjects were missing data on some disorders because caregivers could not complete full interviews. NS=not significant.
For the tests of comorbid disorders, the Time effects were significant for MDD, SAD, and ODD but the Group by Time interactions were not significant. ADHD did not show improvement in either group.
Hypothesis 2: Measures of Efficacy
The children in the WL group who did not remit during the waiting interval were subsequently treated with the same research protocol as the children in the IT group. These 10 WL treated cases were combined with the IT cases to form a single group to examine follow-up effects and also to estimate effect sizes with the full treated sample. Moreover, analyses indicated that PTSD in the WL group did not improve during the wait period, which would justify combining their treatment results with the IT group. The two cases that completed treatment in the intervention development phase (Phase 1) were also combined for these analyses.
The pre- and post-treatment means and effects sizes for PTSD and each comorbid disorder are shown in Table 2. As hypothesized, the Cohen’s d measure of effect size for PTSD was large. The results in the table also indicate that the effect size for PTSD was larger than those for the comorbid disorders, however, all effect sizes except that for ADHD were in the moderate to large range. Effect sizes for PTSD for the three types of trauma events were also estimated separately: acute injury (n=5) d=0.87, witnessed domestic violence (n=6) d=0.56, and victim of the Hurricane Katrina disaster (n=14) d=1.24.
Table 2.
Mean number of symptoms pre- and post- active treatment with Immediate Treatment group and those treated from the Wait Listgroup combined. Means calculated for treatment completers only, n=25. Random effects model tests included cases with missing data, n=75.
| Disorder | Pre | Post | Pre-Post effect sizes Cohen’s d | Six months follow up Mean (SD) | Six months effect sizes Cohen’s d |
|---|---|---|---|---|---|
| Mean (SD) | |||||
| Posttraumatic stress disorder | 8.04 (2.84) | 4.76 (3.62)*** | 1.01 | 2.44 (3.12)*** | 1.88 |
| Major depressive disorder | 3.0 (2.22) | 1.24 (1.54)*** | 0.92 | 1.06 (1.57)*** | 1.01 |
| Separation anxiety disorder | 2.48 (1.83) | 1.21 (1.67)** | 0.72 | 1.25 (2.08)** | 0.63 |
| Oppositional defiant disorder | 4.32 (2.48) | 2.38 (1.84)* | 0.89 | 2.31 (2.36)** | 0.83 |
| Attention-deficit/hyperactivity disorder | 7.84 (5.19) | 5.75 (5.37)1 | 0.40 | 7.31 (6.72) | 0.09 |
| p=.40 | |||||
Random effects model p<.0001,
p<.0005,
p<.005.
p=.28
Because clinicians often deal with categorical outcomes of diagnoses, diagnostic outcomes were also described descriptively. Of the 75 subjects enrolled, 54 (72.0%) had the PTSD-AA diagnosis at baseline. The other 21 had enough PTSD symptoms for inclusion but not enough for the PTSD-AA diagnosis. Eighteen had the DSM-IV diagnosis (24.0%). Of the 25 treatment completers with data, 17 had the PTSD-AA diagnosis pre-treatment and only three still had the diagnosis post-treatment for an 82.4% reduction.
Six Month Follow Up
Of the 25 participants who completed treatment, 16 could be located and assessed for a six month follow-up. There were no differences between those located and not located on the post-treatment number of PTSD, MDD, SAD, ODD, or ADHD symptoms (Wilcoxon rank sum tests). The six month follow-up test with a random effects model for PTSD symptoms was significant, F=29.01, df=2,44, p<.0001 (Table 2). Follow-up tests were also significant for MDD, SAD, and ODD, but not for ADHD.
Adverse Event Data
Four possible adverse events were reported for four participants. The mother of a five year-old female reported on the AEC checklist at session 4 that a pre-existing fear of the dark worsened. This disappeared by session 8. A six year-old female developed enuresis by session 4, and then disappeared by session 8. A four year-old female developed enuresis after session 1 but this seemed related to a thunderstorm rather than the therapy session according to the caregiver. The enuresis had stopped by session 6. A six year-old female defecated in her underwear at home one time during the course of treatment. In the investigation of the attribution of this event with the mother it was not clearly related to the treatment.
Hypothesis 3: Feasibility of TF-CBT techniques
Forty-six children participated in at least one treatment session and were rated for feasibility on the TF-CBT techniques. Overall, children were judged to understand and complete 83.5% of the items rated (out of 1,793 possible from a total of 388 treatment sessions). An independent rater scored 30.7% of the treatment sessions from video (n=116 sessions, 530 items), and this rater agreed with the therapists’ ratings 96.2% of the time. The rater and therapists interrater agreement kappa was substantial at 0.86. The therapists’ ratings were used in the results reported below.
The three year-old children had difficulty with some tasks but careful reading of Table 3 shows that they achieved nearly all of the tasks with time. For example, three year-old children could not complete the “In-office exposures, facilitated with drawings” in sessions 6 and 7, but then 100% of them completed them in session 8 when the anxiety level was raised and/or they had more practice.
Table 3.
Frequencies that 3, 4, 5, and 6 year-old children understood and successfully completed TF-CBT techniques.
| Task to be accomplished by children | 3 year -olds | 4 year -olds | 5 year -olds | 6 year -olds | Total | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | n1 | % | n | % | n | % | n | % | n | |
| Session 1. Psychoeducation: understood concepts of posttraumatic stress disorder: | ||||||||||
| from verbal discussion | 0 | 8 | 53.9 | 13 | 83.3 | 12 | 92.3 | 13 | 63.0 | 46 |
| from cartoons | 62.5 | 8 | 100 | 13 | 91.7 | 12 | 100 | 13 | 91.3 | 46 |
| Session 3. Identify four feelings: | ||||||||||
| from verbal discussion | 25.0 | 4 | 75.0 | 12 | 80.0 | 10 | 100 | 13 | 79.5 | 39 |
| with drawing on body outline | 50.0 | 4 | 100 | 12 | 100 | 10 | 100 | 13 | 94.9 | 39 |
| Session 4. Practiced relaxation techniques | 75.0 | 4 | 100 | 12 | 90.0 | 10 | 90.9 | 11 | 91.9 | 37 |
| Session 5. Recounted trauma with 3 details | 66.7 | 3 | 81.8 | 11 | 80.0 | 10 | 100 | 10 | 85.3 | 34 |
| Session 5. Recounted trauma with 3 details that were negative. | 0 | 3 | 54.6 | 11 | 60.0 | 10 | 90.0 | 10 | 61.7 | 34 |
| In-office exposures, facilitated with drawings: | ||||||||||
| Session 6, mildly anxiety provoking | 0 | 2 | 100 | 11 | 80.0 | 10 | 100 | 9 | 87.5 | 32 |
| Session 7, moderately anxiety provoking | 0 | 2 | 70.0 | 10 | 100 | 9 | 100 | 9 | 83.3 | 30 |
| Session 8, moderately anxiety provoking | 100 | 2 | 77.8 | 9 | 100 | 9 | 100 | 7 | 92.6 | 27 |
| Session 9. worst anxiety provoking | 100 | 1 | 90 | 10 | 100 | 8 | 100 | 7 | 96.2 | 26 |
| Session 10, worst anxiety provoking | 0 | 1 | 88.9 | 9 | 100 | 8 | 100 | 7 | 92.0 | 25 |
| Cumulative | 90.0 | 140 | ||||||||
| In-office exposures, imaginal eyes closed: | ||||||||||
| Session 6, mildly anxiety provoking | 0 | 2 | 72.7 | 11 | 60 | 10 | 88.9 | 9 | 68.8 | 32 |
| Session 7, moderately anxiety provoking | 0 | 2 | 100 | 10 | 66.7 | 9 | 100 | 9 | 83.3 | 25 |
| Session 8, moderately anxiety provoking | 50.0 | 2 | 66.7 | 9 | 77.8 | 9 | 85.7 | 7 | 74.1 | 27 |
| Session 9, worst moment anxiety provoking | 0 | 1 | 60.0 | 10 | 62.5 | 8 | 85.7 | 7 | 65.4 | 26 |
| Session 10, worst moment anx. provoking | 100 | 1 | 66.7 | 9 | 87.5 | 8 | 100 | 7 | 84.0 | 25 |
| Cumulative | 75.0 | 140 | ||||||||
| Self-rating anxiety down to at least a 2 before the end of the session: | ||||||||||
| Session 6 | 0 | 2 | 72.7 | 11 | 66.7 | 9 | 88.9 | 9 | 71.0 | 31 |
| Session 7 | 0 | 2 | 88.9 | 9 | 57.1 | 7 | 87.5 | 8 | 73.1 | 26 |
| Session 8 | 0 | 2 | 100 | 9 | 57.1 | 7 | 83.3 | 6 | 75.0 | 24 |
| Session 9 | 0 | 1 | 100 | 10 | 100 | 6 | 83.3 | 6 | 91.3 | 23 |
| Session 10 | 0 | 1 | 88.9 | 9 | 100 | 8 | 100 | 6 | 91.7 | 24 |
| Cumulative | 79.7 | 128 | ||||||||
| Completed homework assigned at previous session: | ||||||||||
| Session 4 (Session 3’s assignment) | 50.0 | 4 | 91.7 | 12 | 90.0 | 10 | 100 | 11 | 89.2 | 37 |
| Session 5 (Session 4’s assignment) | 33.3 | 3 | 81.8 | 11 | 80.0 | 10 | 80 | 10 | 76.5 | 34 |
| Session 6 (Session 5’s assignment) | 50.0 | 2 | 81.8 | 11 | 80.0 | 10 | 66.7 | 9 | 75.0 | 32 |
| Session 7 (Session 6’s assignment) | 50.0 | 2 | 90.0 | 10 | 100 | 9 | 66.7 | 9 | 83.3 | 30 |
| Session 8 (Session 7’s assignment) | 100 | 2 | 77.8 | 9 | 100 | 9 | 57.1 | 7 | 81.5 | 27 |
| Session 9 (Session 8’s assignment) | 100 | 1 | 80.0 | 10 | 75.0 | 8 | 71.4 | 7 | 76.9 | 26 |
| Session 10 (Session 9’s assignment) | 100 | 1 | 88.9 | 9 | 87.5 | 8 | 85.7 | 7 | 88.0 | 25 |
| Session 11 (Session 10’s assignment) | 0 | 1 | 88.9 | 9 | 100 | 8 | 71.4 | 7 | 84.0 | 25 |
| Cumulative | 82.2 | 236 | ||||||||
| Session 11. Understood a “tomorrow” event | 0 | 1 | 70.0 | 10 | 100 | 7 | 85.7 | 7 | 80.0 | 25 |
| Completed drawing worksheet | 0 | 1 | 50.0 | 10 | 100 | 7 | 85.7 | 7 | 72.0 | 25 |
| Understood a “distant future” event | 0 | 1 | 30.0 | 10 | 85.7 | 7 | 100 | 7 | 64.0 | 25 |
| Completed drawing worksheet | 0 | 1 | 40.0 | 10 | 85.7 | 7 | 100 | 7 | 68.0 | 25 |
| Session 12. Reviewed Roadway Book | 100 | 1 | 90.0 | 10 | 100 | 7 | 85.7 | 7 | 92.0 | 25 |
n=number of children in that age group who were rated. The number who was rated to understand and complete a task successfully can be calculated by multiplying this number by the percentage.
The three year-old children had low ratings for “Self-rating anxiety down to at least a 2 before the end of the session”. This reflects the difficulty in recognizing gradations of emotion states at this age, even though they were successful at doing the exposure exercises that generated the emotion states. They also had low ratings for “Understood new homework assignments” (meaning verbalizing the understanding to their therapists in the planning stage) even though they were successful at actually doing the homework assignments with their caregivers. Both of these ratings do not mean the CBT techniques were not working; rather it reflects that the youngest children did not yet have the self-reporting capacities of the older children, which was not surprising.
The usefulness of the cartoons for psychoeducation to teach children about PTSD symptoms was illustrated in session 1. When teaching the symptoms verbally, supported with a handout, an age gradient was obvious; none of the 3-year-olds and about half of the 4-year-olds, but most of the 5- and 6-year-olds understood the concepts. However, when teaching the symptoms with cartoons, the majority of children in all age groups appeared to understand the concepts.
Three methods of therapeutic exposures were used for every child in sessions 6 through 11 – drawing, eyes closed imaginal, and in vivo homework. It should be noted that 100% of children were able to cooperate with exposure techniques and relaxation exercises, but the percentages were not always 100% because they did not complete them in every single session. Table 3 shows that children were usually able to understand and complete these types of exposures, with imaginal exposures being more difficult, and younger children sometimes had more difficulty.
Discussion
Results indicated that in 3–6 year-old children TF-CBT treatment (IT group) was more effective in reducing PTSD symptoms than an equivalent period of waiting used to control for the passage of time (WL group). Those in the WL group showed no significant mean decrease in symptoms, raising an ethical concern that future use of wait list control groups may be unwarranted. While two previous studies had shown effectiveness for young children with sexual abuse (Cohen & Mannarino, 1996; Deblinger et al., 2001) this is the first to show effectiveness for a variety of types of traumatic events. The lack of differential improvement in the comorbid disorders in the IT condition relative to the WL condition appeared due to different factors. MDD and SAD improved in both conditions. ODD and ADHD did show improvement in the IT group and not in the WL group, but the wide variability in scores (large standard deviations, see Table 1) appeared to prevent this from reaching statistical significance.
While noting it as tentative due to the low retention and awaiting replication The effect size estimate for PTSD in this study (d = 1.01) would be considered large (Cohen, 1988). TF-CBT studies in older youth have all produced large effect sizes also (Silverman et al., 2008) but differences in sampling and designs make direct comparisons speculative.
The feasibilities for specific TF-CBT techniques were in general good, with frequencies of completions of most tasks around 80–90%, and completion rates often relatively higher for older children. Where wider age discrepancies were apparent in feasibility between the younger children (3- and 4-year olds) as compared with the older children (5- and 6-year olds), the tasks tended to center around the need to understand or express verbal narratives. Examples include understanding the concept of PTSD from verbal discussion (session 1), identify their feelings from verbal discussion (session 3), and identify at least three aspects of the trauma as distinct upsetting events (session 5). Each of these was made more feasible with visual aids and drawing.
Limitations include that attrition was unusually high in this study. This was due in part to Hurricane Katrina striking six months into the study, resulting in the loss of six participants who may have completed treatment, and leaving a devastated metropolitan infrastructure for the remainder of the study. Also, the study was conducted in a very young population that was mostly minority and single parent, and few prior efficacy studies have been conducted in this population with which to compare. For example, a good rate of 85% retention was achieved treating sexually abused children treated with a TF-CBT model (Cohen & Mannarino, 1996) in a randomized design for 3–6 year old children, but it was not a majority single parent and minority sample. It is premature to conclude, but as more studies are conducted in the future with diverse populations, better generalizations may be possible about attrition rates in younger children samples. Attrition may be higher with younger children because their externalizing behaviors are relatively less extreme and their internalizing behaviors are relatively less verbalized, so their parents may feel less motivated to return for appointments. Nevertheless, given the high attrition, any conclusions about efficacy (i.e., effect size estimates) should be considered tentative, and ought to await future studies with better retention and perhaps an active treatment as a control group. Another limitation was the small size of the samples and the attrition of the 6-month follow-up.
In conclusion, this study provided support for both the effectiveness and feasibility of a structured treatment protocol for very young children who have posttraumatic stress symptoms from a variety of traumatic experiences. PTSD did not improve with the passage of time in the WL group in the randomized design and the effect size for treating PTSD was large. Additional strengths included that outcomes were measured with diagnostic interview measures, multiple comorbid disorders showed significant effects, and tentative findings from a limited six-month follow-up indicated lasting effects of the treatment.
Key Points.
The two previous trials of treatment for posttraumatic stress in young children were limited to those exposed to sexual abuse, no direct measures of feasibility for the children, and only one study used an outcome measure of PTSD.
Key points of this study were:(1) TF-CBT was more effective than the passage of time for reducing PTSD symptoms in a randomized design; (2) improvements in comorbid disorders were also evident but in different patterns relative to PTSD and required thoughtful interpretations; and (3) the feasibility of young children’s capacities to complete TF-CBT techniques were demonstrated by moving beyond therapist fidelity measures, although 3-and 4-year old children initially had difficulty with tasks that required narratives.
Acknowledgments
Supported by NIMH grant 5R34MH070827. The author thanks the Medical Center of Louisiana Charity Hospital Trauma Center and staff, the Metropolitan Battered Women’s Program, Crescent House, and the St. Bernard Battered Women’s Program.
References
- Allen A, Saltzman WR, Brymer MJ, Oshri A, Silverman WK. An empirically informed intervention for children following exposure to severe hurricanes. The Behavior Therapist. 2006;29(6):118–124. [Google Scholar]
- Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, et al. The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Annals of Internal Medicine. 2001;134:663–694. doi: 10.7326/0003-4819-134-8-200104170-00012. [DOI] [PubMed] [Google Scholar]
- CATS Consortium. Implementing CBT for traumatized children and adolescents after September 11: Lessons learned from the Child and Adolescent Trauma Treatment Services (CATS) Project. Journal of Clinical Child and Adolescent Psychology. 2007;36(4):581–592. doi: 10.1080/15374410701662725. [DOI] [PubMed] [Google Scholar]
- Cohen J, Mannarino A. A treatment outcome study for sexually abused preschool children: Initial findings. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:42–50. doi: 10.1097/00004583-199601000-00011. [DOI] [PubMed] [Google Scholar]
- Cohen JC. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- Deblinger E, Stauffer L, Steer R. Comparative efficacies of supportive and cognitive behavioral group therapies for young children who have been sexually abused and their nonoffending mothers. Child Maltreatment. 2001;6:332–343. doi: 10.1177/1077559501006004006. [DOI] [PubMed] [Google Scholar]
- Egger HL, Erkanli A, Keeler G, Potts E, Walter BK, Angold A. Test-retest reliability of the Preschool Age Psychiatric Assessment (PAPA) Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):538–549. doi: 10.1097/01.chi.0000205705.71194.b8. [DOI] [PubMed] [Google Scholar]
- Grave J, Blissett J. Is cognitive behavior therapy developmentally appropriate for young children? A critical review of the evidence. Clinical Psychology Review. 2004;24:399–420. doi: 10.1016/j.cpr.2004.03.002. [DOI] [PubMed] [Google Scholar]
- March J, Amaya-Jackson L, Murray M. Cognitive-behavioral psychotherapy for children and adolescents with posttraumatic stress disorder after a single-incident stressor. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37(6):585–593. doi: 10.1097/00004583-199806000-00008. [DOI] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Cohen JA. PTSD in children and adolescents: Towards an empirically based algorithm. Depression and Anxiety. doi: 10.1002/da.20736. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Zeanah CH, Myers L, Putnam FW. New findings on alternative criteria for PTSD in preschool children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(5):561–570. doi: 10.1097/01.CHI.0000046822.95464.14. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Ortiz CD, Viswesvaran C, Burns BJ, Kolko DJ, Putnam FW, et al. Evidence-based psychosocial treatments for children and adolescents exposed to traumatic events. Journal of Clinical Child and Adolescent Psychology. 2008;37(1):156–183. doi: 10.1080/15374410701818293. [DOI] [PubMed] [Google Scholar]
- Stoops N. Educational Attainment in the United States: 2003. 2004 June; Retrieved July 31, 2010, from http://www.census.gov/prod/2004pubs/p20-550.pdf.