Abstract
Objectives
Unrecognized dislodgement of an endotracheal tube (ETT) during the transport of an intubated patient can have life-threatening consequences. Standard methods to monitor these patients, such as pulse oximetry and physical examination, are both subject to inaccuracies with patient movement and ambient noise. Capnography provides a continuous and objective measure of ventilation that can alert a provider immediately to an airway problem. The objective of this study was to determine through simulation if capnography decreases time to correction of dislodged ETTs during the transport of intubated patients, in comparison to standard monitoring.
Methods
Paramedics and paramedic students were randomized as to whether or not they had capnography available to them in addition to standard monitoring during a simulated scenario. In the scenario, subjects monitored an intubated baby who subsequently experiences a dislodgement of the ETT during interfacility transport. Time to correction of the ETT dislodgement was the primary outcome. The secondary outcome was correction of dislodgement prior to decline in pulse oximetry.
Results
Fifty-three subjects were enrolled in the study, with complete data on 50 subjects. Median time to correction of ETT dislodgement was 2.02 minutes (95% CI = 1.22 to 4.12 minutes) for the capnography group versus 4.00 minutes (95% CI = 3.35 to 5.50 minutes) in the standard monitoring group (p = 0.05). Forty-eight percent of subjects using capnography corrected the ETT dislodgement prior to decline in pulse oximetry compared with 12% of controls (p = 0.01). There were no differences in time to correction of dislodgement based on years of experience, perceived comfort, reported adequacy of teaching, or past use of capnography.
Conclusions
The addition of capnography to standard monitoring significantly improves recognition of ETT dislodgement and reduces the time to correction of dislodged ETTs by prehospital providers in a simulated pediatric transport setting.
INTRODUCTION
Intubated patients who undergo transport require careful monitoring as there is a risk that the endotracheal tube (ETT) may become dislodged due to patient movement, improper securing of the ETT, or inadvertent movement of the ETT. Unrecognized dislodgement of the ETT can lead to serious adverse events, including hypoxia and subsequent cardiac arrest. Clinical exam findings such as chest rise and auscultation are often inaccurate.1,2 Standard pulse oximetry monitors may not alert the provider to a problem for several minutes.2,3
Prehospital personnel have the challenges of working in cramped and noisy environments. They routinely move intubated patients on and off of stretchers, and via ambulances, helicopters, and fixed-wing aircraft to receiving facilities. Dislodged ETTs are not uncommon, and are often unrecognized using standard methods of confirmation.4–6 Capnography, or continuous end-tidal carbon dioxide monitoring, may offer advantages in these situations. Capnography is the graphic representation of carbon dioxide expired during the respiratory cycle. It can be measured via an inline attachment to the ETT. It has several advantages over pulse oximetry and physical exam findings during transport of the intubated patient.2 It is a measure of ventilation that is continuous and objective.7–9 There is no delay in detection of ventilatory problems with the capnograph, unlike the slower changes seen with pulse oximetry.2,3,10 Furthermore, capnography has also shown to malfunction less than pulse oximetry in the out-of-hospital setting.11 However, while secondary confirmation of endotracheal intubation is recommended by the American Heart Association, a continuous end-tidal carbon dioxide monitor is not a required piece of equipment in some EMS systems, and may not be universally available.12
The objective of this study was to determine in prehospital providers using simulation if there is a significant difference in time to correction of ETT dislodgement when capnography is used in addition to standard methods. We hypothesized that the addition of capnography will significantly reduce the time to correction of ETT dislodgement. This would provide evidence for the value of continuous monitoring with capnography during transport of the intubated patient.
METHODS
Study Design
This was a randomized controlled study of paramedics and paramedic students. Our Human Investigations Committee approved this study. All participants provided informed consent.
Study Setting and Population
All scenarios took place in a dedicated medical simulation center. Two identical simulation suites were used. A computerized control room where scenarios were monitored and remotely controlled adjoins each suite. Professional audio and video equipment and the Laerdal Advanced Video System (Laerdal Medical, Wappingers Falls, NY) were used to record each scenario for later viewing. The advanced video system allows the audio and video streams to be synchronized with the simulated data log and patient monitor in a single file. Thus, actions that are viewed via the video recordings can be measured exactly against the timing of simulated events.
Paramedic students were recruited from a local paramedic training program towards the end of their training. The paramedic program provides education to all students on the use of capnography with didactics as well as with patient scenarios. The subjects also have had practical experience with intubations and the monitoring of intubated patients in the operating suites where capnography is routinely used. Practicing paramedics were recruited during monthly continuing education sessions held by the same institution. All participation was voluntary. There were no exclusion criteria.
Subjects were randomized into two groups via stratified block randomization: those with access to capnography in addition to a standard cardiac monitor and pulse oximetry (cases) and those with only access to a cardiac monitor and pulse oximetry (controls). Block randomization was by computer generated random number list in a 1:1 ratio. Paramedics and paramedic students were randomized as separate groups. Participants received sequentially numbered, opaque, sealed envelopes that held their group assignments.
Study Protocol
The Laerdal SimBaby (Laerdal Medical, Wappingers Falls, NY) was used for this study. SimBaby is a portable high fidelity patient simulator with realistic airway anatomy and clinical functionality that allows for the creation of authentic scenarios. The realistic upper airway and esophagus allows a variety of airway procedures, including bag-mask ventilation and intubation of either the trachea or esophagus with corresponding physiologic responses. Respiration is simulated with chest rise and fall, as controlled via the computer with synchronized respiratory rate and tidal volumes. Vital signs are either directly detectable on the manikin or displayed on the simulated patient monitor. Subjects were oriented to the functions of the manikin prior to the study and told to perform all actions on the manikin during the simulation as they would in a real life scenario. They were provided with an ambulance stretcher, a standard prehospital transport bag with advanced life support equipment, including intubation equipment, additional airway devices, a self-inflating bag and appropriate size mask, oxygen, medications, and a monitor.
With the exception of the presence or absence of capnography on the patient monitor, two identical scenarios were programmed with the SimBaby software (Laerdal Medical). This allowed for all simulated events to occur at the same time and in the same order for all subjects. Three investigators ran the scenarios during this study and did not alter the program for any participant.
In the simulated scenario, subjects were given a case where an infant intubated for respiratory depression secondary to antiepileptic medications required transfer to a tertiary care facility. Standardized scripts were used. The acting physician reported that the ETT was confirmed to be endotracheal via colorimetry as well as radiography. The infant in the scenario had normal vital signs, normal pulse oximetry, bilateral chest rise, and breath sounds, and had a peripheral intravenous line in place. The patient monitor was positioned across from the subject where it could be easily seen, and alarm values were set for all vital signs. For the purpose of the study, the endotracheal tube was placed in the esophagus and secured to the manikin with tape. The esophagus was detached from the stomach so as not to distend with bag-valve ventilation during the simulation.
The acting physician and the subject physically transferred the manikin from the bed to a stretcher and bag-valve ventilation through the ETT was transitioned from the acting physician to the study subject. Subsequently, the physician exited the simulation suite. The physical movement of the manikin during patient transport was theorized to be the event causing ETT dislodgement in this scenario. Simulated dislodgement was programmed to occur two minutes after initiation of the scenario. This occurred soon after transfer of the patient from the bed to the stretcher and when the subjects were solely responsible for the care of the patient. At the time of dislodgement, there was an immediate loss of chest rise and breath sounds in the manikin. There was also immediate loss of the capnography waveform for cases. If no correction occurred, there was a slow decline in the pulse oximetry values that was programmed to begin two minutes after dislodgement. Similarly, heart rate began to gradually decline four minutes after dislodgement. The scenario ended either at 10 minutes, or when the outcome (as outlined below) was reached, whichever was sooner.
If the subjects verbalized any questions during the simulation, they received a prompt that they were in the middle of a patient transport and should physically do whatever they deemed necessary for the patient.
Additional data were collected at the end of each scenario via written survey. Data included years of experience as a prehospital provider and within the medical field, prior experience with capnography, location of paramedic training, perceived comfort with capnography, perceived sufficiency of teaching regarding capnography, and number of intubations performed in the last year.
Outcome Measures
Our primary outcome measure was time to correction of ETT dislodgement. This was defined as removal of the ETT, bag-mask ventilation around the ETT, or repositioning of the ETT under direct visualization. Resumption of appropriate ventilation was not necessary for our outcome, as it was not our intention to assess intubation or bag-valve ventilation skills for this study. The scenario ended upon reaching an outcome or at 10 minutes, at which point the simulated infant was severely hypoxic and bradycardic. Our secondary outcomes included rates of correction of ETT dislodgement at any point within the 10-minute scenario and prior to changes in pulse oximetry, defined as the time period within 2 minutes from ETT dislodgement.
Two research assistants blinded to the objectives of this study, as well as to each subject's group assignment, observed the subjects on the video recordings. Two different angles of each subject were available for review. Video-stamping present in the Laerdal video system allowed the research assistants to note precisely when the ETT dislodgement occurred. They recorded the time from ETT dislodgement to the time of correction. Inter-rater reliability of the research assistants was measured. If the two assistants disagreed on whether or not the outcome was met, a third reviewer analyzed the videos and the two congruent reviewers determined the final outcome.
Data Analysis
A one-sided log-rank test with an overall sample size of 50 subjects would achieve 80% power at an alpha of 0.05 to detect a significant difference between a median time to ETT dislodgement correction of 4.0 minutes in the control group and 1.85 minutes in the group with access to capnography. Characteristics of enrolled subjects are summarized with descriptive statistics including mean (with minimum and maximum), median, and frequencies with percents. Categorical variables were compared between cases and controls with Fisher's exact test or chi-square statistic, and the Wilcoxon rank sum test was used for years of paramedic experience. Time to outcome between groups and subject characteristics was compared using the Kaplan-Meier approach, and p-values were obtained from the log-rank test. The data are presented as median time to correction with 95% confidence intervals (CI). Proportions of subjects who corrected the dislodged ETT within the first two minutes after dislodgement, within the first four minutes after dislodgement, and at any time during the simulation were compared between cases and controls using Fisher's exact test or chi-square statistic. Statistical significance was established with alpha of 0.05. Analyses were performed with SAS 9.2 (SAS Institute, Cary, NC).
RESULTS
The study was conducted between August 2009 and March 2010 over three sessions (one for students and two for practicing paramedics). Thirteen paramedic students and 40 practicing paramedics were enrolled. Three practicing paramedics were excluded from the analyses due to video malfunction, removal of ETT prior to dislodgement, and subject withdrawal. Of the students, seven were randomized to the capnography group (cases), and six were randomized to the standard monitor group (controls). Eighteen practicing paramedics were cases, and 19 were controls. Characteristics of study participants are summarized in Table 1. The intraclass correlation coefficient for the two research assistants was 0.80 (95% CI = 0.68 to 0.88).
Table 1.
Characteristics of Subjects.
| Characteristic | Cases | Controls | p-value* |
|---|---|---|---|
|
| |||
| Paramedic students | n = 7 | n = 6 | |
| Mean years of prehospital experience (min, max) | 5.7 (2.0, 10.0) | 4.6 (1.0, 10.0) | |
| Felt teaching on capnography was sufficient | 7 (100) | 6 (100) | |
| Stated comfortable using capnography | 6 (86) | 4 (67) | |
| Used capnography in past | 4 (57) | 2 (33) | |
| Mean number of intubations (min, max) | 15.3 (0, 26) | 17.7 (11, 36) | |
|
| |||
| Practicing paramedics | n = 18 | n = 19 | |
| Mean years of paramedic experience (min, max) | 10.1 (1.0, 20.0) | 12.6 (2.0, 35.0) | 0.49^ |
| Felt teaching on capnography was sufficient | 13 (72) | 14 (74) | 0.79† |
| Stated comfortable using capnography | 13 (72) | 16 (84) | 0.45† |
| Used capnography in past | 18 (100) | 18 (95) | 1.00† |
| Trained at local paramedic training program | 9 (50) | 8 (42) | 0.63† |
| >5 intubations in last year | 6 (33) | 9 (47) | 0.32† |
Values are reported as n (%) unless otherwise stated.
Statistical comparisons not performed due to small sample size for students
Wilcoxon rank sum test
Chi-square or Fisher's exact test
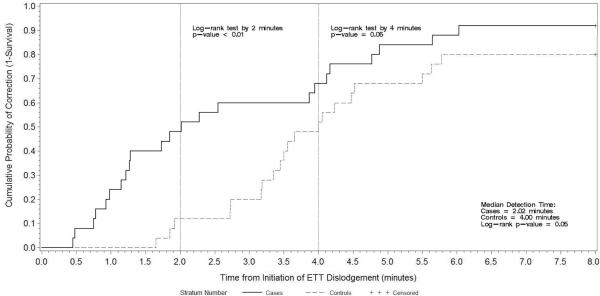
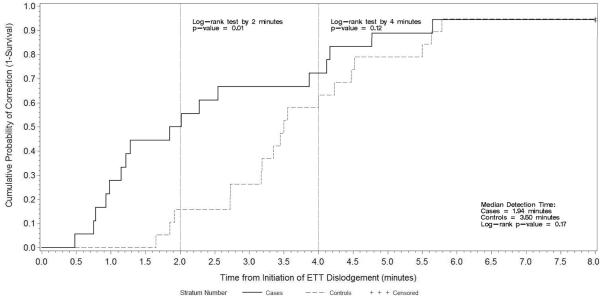
There was a positive relationship between the availability of capnography and meeting the primary outcome of the study (Table 2). For all subjects combined, the time to correction of ETT dislodgement was significantly shorter among cases than among controls (p = 0.05). Figure 1 shows the cumulative probability of correction over the length of simulated dislodgement. A significantly greater proportion of subjects with access to capnography recognized and corrected ETT dislodgement by two minutes (p < 0.01), and four minutes (p = 0.05). When examined by the type of participant, we found that paramedics had significantly shorter time to correction than students (median time of 3.18 minutes vs. 4.88 minutes, p = 0.01). Therefore, we stratified our analyses of the primary and secondary outcomes by the type of participant. Figure 2 depicts the rate of correction over time between cases and controls among paramedics. Although the overall time to correction (p = 0.17) and correction within the first four minutes (p = 0.12) were not significantly different between the two groups, a significantly greater number of paramedics in the capnography group performed correction within the first two minutes (p = 0.01) than their counterparts in the control group. There were no differences in time to correction based on years of experience, perceived comfort with capnography, perceived teaching on capnography, training institution, previous use of capnography, or other clinical parameters (Table 2).
Table 2.
Unadjusted Time to Correction of ETT Dislodgement (minutes) during Total Simulation.
| Characteristic | All Subjects Median (95% CI) | Students Median (95% CI) | Paramedics Median (95% CI) |
|---|---|---|---|
|
| |||
| Cases | 2.02 (1.22–4.12)* | 3.95 (0.45–6.03) | 1.94 (0.98–3.87) |
| Controls | 4.00 (3.35–5.50) | NA^ | 3.5 (2.73–4.47) |
|
| |||
| Sufficient teaching on capnography | 3.65 (2.28–4.47) | NA‡ | 3.18 (1.85–4.23) |
| No sufficient teaching on capnography | 2.73 (1.22–4.52) | 2.64 (1.15–4.00) | |
|
| |||
| Very or somewhat comfortable with capnography | 3.50 (2.28–4.17) | NA† | 3.18 (1.92–4.00) |
| Neutral or uncomfortable with capnography | 3.65 (1.28–6.03) | 2.69 (1.22–4.52) | |
|
| |||
| Used capnography in past | 3.27 (2.02–4.05) | 4.47 (NA¥) | NA£ |
| Not used capnography in past | 4.99 (NA¥) | 6.03 (NA¥) | |
|
| |||
| Trained at local sponsor hospital | 3.80 (1.85–5.50) | NA‡ | 2.72 (1.22–4.77) |
| Trained at other institution | 3.40 (2.02–4.12) | 3.40 (2.02–4.12) | |
Significantly different at alpha 0.05 using Log-rank test
Less than 50% of subjects achieved correction of ETT dislodgement
All students responded as having sufficient teaching on capnography and trained at local sponsor hospital
10 out of 13 students responded as being comfortable with capnography
95% CI for median survival could not be calculated due to small sample size
36 out of 37 paramedics reported using capnography in the past
Figure 1.
Time to Correction of ETT Dislodgement based on Kaplan-Meier Method. All Subjects (n = 50).
Figure 2.
Time to Correction of ETT Dislodgement based on Kaplan-Meier Method. Practicing Paramedics (n = 37).
Our findings from the analyses of rates of correction between and among students and practicing paramedics mirrored the findings from the time to correction (Table 3). Five students and two paramedics did not correct the ETT dislodgement at any point during the simulation, five of whom were in the standard monitoring group. Forty-eight percent of cases met the outcome prior to any decline in pulse oximetry (within 2 minutes of ETT dislodgement), compared with 12% of controls (p = 0.01).
Table 3.
Rates of Correction of ETT Dislodgement.
| Sample | Group | At Any Time During Simulation | Within 2 Minutes of ETT Dislodgement | Within 4 Minutes of ETT Dislodgement |
|---|---|---|---|---|
|
| ||||
| All Subjects | Cases | 23 (92) | 12 (48)* | 17 (68) |
| Controls | 20 (80) | 3 (12) | 13 (52) | |
|
| ||||
| Students | Cases | 6 (86) | 3 (43) | 4 (57) |
| Controls | 2 (33) | 0 (0) | 1 (17) | |
|
| ||||
| Paramedics | Cases | 17 (94) | 9 (50)* | 13 (72) |
| Controls | 18 (95) | 3 (16) | 12 (63) | |
All values are reported as n (%)
Statistically significant at alpha = 0.05
DISCUSSION
Our study demonstrated the advantages of capnography in the detection of ETT dislodgement in the simulated prehospital setting. Prehospital providers with access to capnography had significantly shorter times to correct ETT dislodgement in comparison to those using only standard monitoring devices and physical examination findings (2 minutes vs. 4 minutes). Paramedic students also had improved rate of recognition of ETT dislodgement when using this device (86% vs. 33%).
One interesting finding is the delay in recognition to dislodged ETT without the use of capnography. Despite absence of both chest rise and breath sounds in the simulated patients, only 12% of providers in the group without capnography were able to recognize and correct the ETT dislodgement prior to changes in other vital signs such as pulse oximetry. While it may take greater than four minutes for pulse oximetry to begin to decline in patients who have been receiving supplemental oxygen due to elevated arterial oxygen content, the mean time for this decline is approximately two minutes.10,13 Furthermore, prehospital providers are often unable to hear breath sounds due to high levels of ambient noise during transport.14 Capnography provides prominent visual and auditory signals for providers reflecting the ventilatory status of their patients. Similarly, the change in auditory tones of the pulse oximetry monitor is a potent prompt to providers, thus the reason the initiation of decline in pulse oximetry was chosen as a secondary outcome measure instead of a clinically significant numeric value for hypoxemia.
The American Heart Association's Advanced Cardiac Life Support and Pediatric Advanced Life Support guidelines state that providers should monitor exhaled carbon dioxide during transport and diagnostic procedures that require patient movement.15 The National Association of EMS Physicians also states that any time a patient is moved or dislodgement of the ETT is suspected, placement should be verified, and the best way to accomplish this is by end-tidal carbon dioxide detection.16 Despite the fact that capnography is useful for prehospital personnel, these monitors are not always available in the transport setting.17–20 While the hope is for capnography to be universally adopted by EMS systems, and while many systems (including the system where this study was conducted) already mandate capnography, there may be barriers to more widespread change. Primarily, the purchase of new portable capnography monitors or modules to be used in existing monitors may be cost prohibitive in some systems. Disposable sampling lines needed to measure exhaled carbon dioxide concentrations from each patient are an additional expense.
Capnography has been shown to be highly effective in diagnosing non-endotracheal intubations.2,10,21 In an observational study of EMS providers, the effectiveness of capnography on the incidence of unrecognized misplaced intubations was evaluated. This study demonstrated that providers who did not use capnography had a much higher rate of unrecognized misplaced intubations, with an odds ratio of 28.6.4 Although capnography was shown to be superior to standard monitoring for the detection of non-endotracheal intubations, this study had several limitations. Provider sites in this study were not randomized nor did it take into account individual experience levels which could influence rates of intubation and their success.4 It is possible that the differences found in this study could be attributed to differences in intubation skills and not due to the addition of capnography.
While there has been evidence regarding the superiority of capnography for detecting non-endotracheal intubations, there are few data evaluating this tool specifically for endotracheal tube dislodgement.21,22 Our study adds to the existing evidence of the advantages of capnography. In comparison to the Silvestri study, through a randomized design we demonstrated capnography alone, and not variables such as experience or comfort, did in fact did affect time to correction of ETT dislodgement.
LIMITATIONS
This was a simulated scenario requiring participants to function in a state of suspended reality. However, simulation-based training has been previously used in a variety of scenarios and has been shown to improve technical skills.23,24 All subjects were acting individually and there was a lack of ambient noise and actual patient movement other than from the bed to the stretcher. A small number of participants verbalized their actions instead of physically performing them; however, no participants verbalized an action consistent with any of the predefined outcomes. Although all subjects had a uniform introduction to the simulation equipment and its functions, subjects may have had varying degrees of comfort with the simulation manikin. Similarly, in simulated scenarios participants are often expecting sentinel events to occur and thus have a heightened awareness. However, these limitations likely caused our subjects to more closely monitor the simulated patients and with less distractions than would occur during real patient encounters. This potentially led to a smaller difference between groups in our study than might otherwise be found.
While it was requested of subjects not to share their experiences with others prior to their participation, all scenarios were identical. Thus, it remains possible that later participants became aware of the objective of the scenario prior to participating in the simulation.
We did not expect to find such significant differences between the performance of the paramedic students and the practicing paramedics. This decreased the observed effect size, in terms of the time to correction, compared to the expected effect size as was proposed in the sample size calculation. We then needed to stratify our analyses by the type of participant, thereby effectively lowering the sample size, which reduced our power in the sub-group analyses. Nevertheless, we were able to observe clinically meaningful and statistically significant differences for the primary outcome for the overall sample, and for the secondary outcomes among all subjects and among paramedics. Because we observed very high p-values for the associations of such subject characteristics as their perceived comfort or prior experiences with the primary and secondary outcomes, we do not attribute these to low statistical power of our sample size.
Second, although we have shown that capnography improved the time to correction of ETT dislodgement, this does not demonstrate that there is an improvement in patient outcomes with the addition of this device. It may be reasonable to presume that patients with faster correction of ETT dislodgement suffer less serious adverse events such as cardiac arrest or hypoxic brain injury. Larger studies in a non-simulated patient population would need to be performed in order to evaluate this effect.
Last, subjects responded to a written survey about their perceived comfort with capnography at the end of their simulation. The timing of this question may have influenced their responses.
CONCLUSIONS
The addition of capnography significantly improves recognition of ETT dislodgement and reduces the time to correction of ETT dislodgement by prehospital providers during simulation of pediatric transport.
Acknowledgments
The authors would like to acknowledge Antonio Riera, MD, Lawrence Siew, MD and Lilia Reyes, MD for their assistance in study enrollment.
Funding Sources/Disclosures: This study was funded by the Yale Pediatric Faculty Scholar Program.
Footnotes
Prior Presentations: Presented at the Eastern Society of Pediatric Research meeting, Philadelphia PA, March 2010 and the American Academy of Pediatrics National Conference and Exhibition, San Francisco CA, October 2010.
Publisher's Disclaimer: This publication was made possible by CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH. Information on Reengineering the Clinical Research Enterprise can be obtained from the NIH website.
REFERENCES
- 1].Bair AE, Smith D, Lichty L. Intubation confirmation techniques associated with unrecognized non-tracheal intubations by pre-hospital providers. J Emerg Med. 2005;28:403–7. doi: 10.1016/j.jemermed.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 2].Vaghadia H, Jenkins LC, Ford RW. Comparison of end-tidal carbon dioxide, oxygen saturation and clinical signs for the detection of oesophageal intubation. Can J Anaesth. 1989;36:560–4. doi: 10.1007/BF03005386. [DOI] [PubMed] [Google Scholar]
- 3].Guggenberger H, Lenz G, Federle R. Early detection of inadvertent oesophageal intubation: pulse oximetry vs. capnography. Acta Anaesthesiol Scand. 1989;33:112–5. doi: 10.1111/j.1399-6576.1989.tb02871.x. [DOI] [PubMed] [Google Scholar]
- 4].Silvestri S, Ralls GA, Krauss B, et al. The effectiveness of out-of-hospital use of continuous end-tidal carbon dioxide monitoring on the rate of unrecognized misplaced intubation within a regional emergency medical services system. Ann Emerg Med. 2005;45:497–503. doi: 10.1016/j.annemergmed.2004.09.014. [DOI] [PubMed] [Google Scholar]
- 5].Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37:32–7. doi: 10.1067/mem.2001.112098. [DOI] [PubMed] [Google Scholar]
- 6].Denver Metro Airway Study Group A prospective multicenter evaluation of prehospital airway management performance in a large metropolitan region. Prehosp Emerg Care. 2009;13:304–10. doi: 10.1080/10903120902935280. [DOI] [PubMed] [Google Scholar]
- 7].Ahrens T, Sona C. Capnography application in acute and critical care. AACN Clin Iss. 2003;14:123–32. doi: 10.1097/00044067-200305000-00002. [DOI] [PubMed] [Google Scholar]
- 8].Bhende MS, LaCovey DC. End-tidal carbon dioxide monitoring in the prehospital setting. Prehosp Emerg Care. 2001;5:208–13. doi: 10.1080/10903120190940146. [DOI] [PubMed] [Google Scholar]
- 9].Castioni C. Capnography in EMS. Emerg Med Serv. 2003;32:80–2. 4, 6–8. [PubMed] [Google Scholar]
- 10].Poirier MP, Gonzalez Del-Rey JA, McAneney CM, DiGiulio GA. Utility of monitoring capnography, pulse oximetry, and vital signs in the detection of airway mishaps: a hyperoxemic animal model. Am J Emerg Med. 1998;16:350–2. doi: 10.1016/s0735-6757(98)90125-5. [DOI] [PubMed] [Google Scholar]
- 11].Kober A, Schubert B, Bertalanffy P, et al. Capnography in non-tracheally intubated emergency patients as an additional tool in pulse oximetry for prehospital monitoring of respiration. Anesthes Analg. 2004;98:206–10. doi: 10.1213/01.ANE.0000090145.73834.2F. [DOI] [PubMed] [Google Scholar]
- 12].Subcommittees and Task Force of the American Heart Association Emergency Cardiovascular Care Committee 2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2005;112(24 suppl):IV1–203. doi: 10.1161/CIRCULATIONAHA.105.166550. [DOI] [PubMed] [Google Scholar]
- 13].Patel R, Lenczyk M, Hannallah RS, McGill WA. Age and the onset of desaturation in apnoeic children. Can J Anaesthes. 1994;41:771–4. doi: 10.1007/BF03011582. [DOI] [PubMed] [Google Scholar]
- 14].Hunt RC, Bryan DM, Brinkley VS, Whitley TW, Benson NH. Inability to assess breath sounds during air medical transport by helicopter. JAMA. 1991;265:1982–4. [PubMed] [Google Scholar]
- 15].Cummins RO, Hazinski MF. Guidelines based on the principle “first, do no harm”: new guidelines on tracheal tube confirmation and prevention of dislodgment. Circulation. 2000;102:I380–4. doi: 10.1161/01.cir.102.suppl_1.i-380. [DOI] [PubMed] [Google Scholar]
- 16].O'Connor RE, Swor RA. Verification of endotracheal tube placement following intubation. National Association of EMS Physicians Standards and Clinical Practice Committee. Prehosp Emerg Care. 1999;3:248–50. doi: 10.1080/10903129908958945. [DOI] [PubMed] [Google Scholar]
- 17].Langhan ML, Chen L. Current utilization of continuous end-tidal carbon dioxide monitoring in pediatric emergency departments. Pediatr Emerg Care. 2008;24:211–3. doi: 10.1097/PEC.0b013e31816a8d31. [DOI] [PubMed] [Google Scholar]
- 18].Bhende MS, Thompson AE, Orr RA. Utility of an end-tidal carbon dioxide detector during stabilization and transport of critically ill children. Pediatrics. 1992;89:1042–4. [PubMed] [Google Scholar]
- 19].Donnelly JA, Smith EA, Hope AT, Alexander RJ. An assessment of portable carbon dioxide monitors during interhospital transfer. Anaesthesia. 1995;50:703–5. doi: 10.1111/j.1365-2044.1995.tb06098.x. [DOI] [PubMed] [Google Scholar]
- 20].Deiorio NM. Continuous end-tidal carbon dioxide monitoring for confirmation of endotracheal tube placement is neither widely available nor consistently applied by emergency physicians. Emerg Med J. 2005;22:490–3. doi: 10.1136/emj.2004.015818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21].Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Inten Care Med. 2002;28:701–4. doi: 10.1007/s00134-002-1290-x. [DOI] [PubMed] [Google Scholar]
- 22].Takeda T, Tanigawa K, Tanaka H, Hayashi Y, Goto E, Tanaka K. The assessment of three methods to verify tracheal tube placement in the emergency setting. Resuscitation. 2003;56:153–7. doi: 10.1016/s0300-9572(02)00345-3. [DOI] [PubMed] [Google Scholar]
- 23].Eppich WJ, Adler MD, McGaghie WC. Emergency and critical care pediatrics: use of medical simulation for training in acute pediatric emergencies. Curr Opin Pediatr. 2006;18:266–71. doi: 10.1097/01.mop.0000193309.22462.c9. [DOI] [PubMed] [Google Scholar]
- 24].Hunt EA, Fiedor-Hamilton M, Eppich WJ. Resuscitation education: narrowing the gap between evidence-based resuscitation guidelines and performance using best educational practices. Pediatr Clin N Am. 2008;55:1025–50. doi: 10.1016/j.pcl.2008.04.007. [DOI] [PubMed] [Google Scholar]