Abstract
Background
Deaf American Sign Language (ASL) users face communication and language barriers that limit healthcare communication with their providers. Prior research has not examined preventive services with ASL-skilled clinicians.
Purpose
The goal of this study was to determine whether provider language concordance is associated with improved receipt of preventive services among deaf respondents.
Methods
This cross-sectional study included 89 deaf respondents aged 50–75 years from the Deaf Health Survey (2008), a BRFSS survey adapted for use with deaf ASL users. Association between the respondent's communication method with the provider (i.e., categorized as either concordant–doctor signs or discordant–other) and preventive services use was assessed using logistic regression adjusting for race, gender, income, health status, health insurance, and education. Analyses were conducted in 2010.
Results
Deaf respondents who reported having a concordant provider were more likely to report a greater number of preventive services (OR 3.42; 95% CI:1.31, 8.93; p=0.0122) when compared to deaf respondents who reported having a discordant provider even after adjusting for race, gender, income, health status, health insurance, and education. In unadjusted analyses, deaf respondents who reported having a concordant provider were more likely to receive an influenza vaccination in the past year (OR 4.55; p=0.016) when compared to respondents who had a discordant provider.
Conclusions
Language-concordant patient–provider communication is associated with higher appropriate use of preventive services by deaf ASL users.
Introduction
Individuals with limited English proficiency or communication abilities are at high risk for health disparities and adverse health effects.1,2 Poor health communication can lead to lower patient satisfaction, adherence, use of health services, and education regarding healthy behaviors. 2–6 Linguistic concordance between patients and providers is an important determinant of whether patients seek, understand and adhere to providers' preventive services recommendations which has been associated with improved healthcare utilization.7,8,9–11
Deaf linguistic minority refers to deaf American Sign Language (ASL) users, a group of individuals who identify themselves as a minority community, with their own unique language and culture.12,13 Deaf ASL users struggle to understand spoken English and may lack proficiency in written English. Historically health-related research and education programs have excluded deaf ASL users. Communication and language barriers isolate this group from mass media and healthcare messages.14–16 Documented health disparities experienced by deaf ASL users include sexual health17–19, cancer20, preventive health16, 21, and cardiovascular disease.22 Cultural and linguistic differences pose a challenge for many clinicians who care for deaf ASL users. Results from an ASL-accessible survey were used to test the hypothesis that deaf ASL users who report language-concordant healthcare communication are more likely to receive preventive services.
Methods
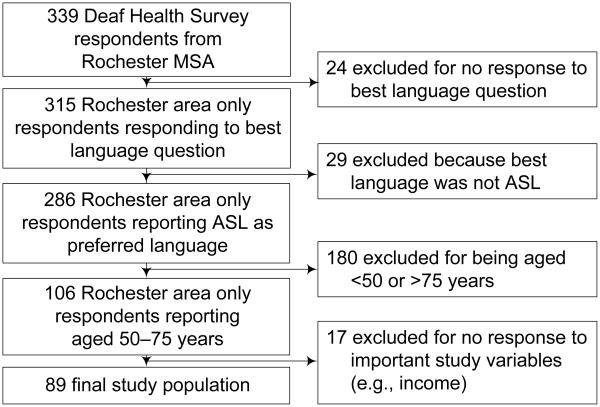
The data source is the National Center for Deaf Health Research's (NCDHR) Deaf Health Survey (DHS), adapted from the Behavioral Risk Factor Surveillance System Survey (BRFSS)23 for deaf individuals. The DHS is self-administered on a touch-screen computer. Deaf respondents chose the survey language—ASL, signed English, and written English. The Rochester NY Metropolitan Statistical Area (MSA) was selected to administer the survey due to its high per capita population of deaf ASL users. The data collection occurred from March, 2008 until September, 2008. The NCDHR DHS is the largest cross-sectional public health survey of deaf individuals ever conducted in the U.S. 339 adults took the DHS. For analyses reported here, deaf people who reported that ASL was not their best language were excluded. Only respondents aged 50–75 years were included in the analyses (n=89, Figure 1). The research was approved by the University of Rochester Research Subjects Review Board.
Figure 1. Determination of Study Population.
Note: ASL, American Sign Language; MSA, Rochester NY metropolitan statistical area
Measures
The analyses examined receipt of the three non-gender-specific preventive services in the DHS (i.e., influenza vaccination in previous 12 months and if ever colonoscopy/sigmoidoscopy and cholesterol screening) recommended for adults aged 50–75 years in 2008 24. The authors analyzed each preventive service individually and also created a score (range 0–3) of the number of these preventive services reported. Respondents' healthcare communication was categorized as concordant if they reported that their doctor signs.
Statistical Analyses
SAS 9.2 was used for all analyses. The authors conducted univariate and bivariate analyses, and then used logistic regression to evaluate the dependent variables' (preventive services use) association with the primary independent variable (communication concordance) while adjusting for race, gender, income, health status, health insurance and education.
Results
Demographics and most healthcare variables were similar for respondents who reported concordant and discordant healthcare communication (Table 1). Ages between the two groups were comparable (mean age was 57.9 for the concordant group and 57.2 for the discordant group). Only one respondent with provider language concordant reported receiving none or only one preventive service (influenza, colonoscopy and cholesterol screening), whereas 17% of the respondents in the provider language discordant group reported only 0–1 preventive service. Respondents who reported having ASL-concordant communication were more likely to report influenza vaccinations than respondents who reported discordant communication (OR 4.55; p=0.016). Reported rates for colon and cholesterol screening were similar for the two groups.
Table 1. Respondent Demographics by Mode of Communication with Provider.
| Characteristics | Provider Signs (%) |
Other Modes (%) |
p-value (χ2) |
|---|---|---|---|
| Gender | 0.748 | ||
| Female | 16 (51.6) | 32 (55.2) | |
| Male | 15 (48.4) | 26 (44.8) | |
| Race | 0.174* | ||
| White | 31 (100) | 54 (93.1) | |
| Other | 0 (0) | 4 (6.9) | |
| Household Income ($) | 0.381 | ||
| <25,000 | 7 (22.6) | 19 (32.8) | |
| 25,000–50,000 | 10 (32.2) | 21 (36.2) | |
| >50,000 | 14 (45.2) | 18 (31.0) | |
| Education | 0.129 | ||
| High school or less | 11 (35.5) | 12 (20.7) | |
| Some college or higher | 20 (64.5) | 46 (79.3) | |
| Medical Insurance | 0.085* | ||
| Public | 12 (38.7) | 17 (29.3) | |
| Private | 19 (61.3) | 40 (69.0) | |
| None | 0 (0) | 1 (1.7) | |
| Health Status | 0.224 | ||
| Excellent–Good | 28 (90.3) | 56 (96.6) | |
| Fair–Poor | 3 (9.7) | 2 (3.4) | |
| Sum of Preventive Services | 0.055* | ||
| 0–1** | 1 (3.2) | 10 (17.2) | |
| 2 | 10 (32.3) | 24 (41.4) | |
| 3 | 20 (64.5) | 24 (41.4) | |
| Preventive Services | |||
| Flu Shot (in previous 12 months) | 0.016 | ||
| Yes | 28 (90.3) | 39 (67.2) | |
| No | 3 (9.7) | 19 (32.8) | |
| Colonoscopy/sigmoidoscopy (if ever) | 0.141 | ||
| Yes | 24 (77.4) | 36 (62.1) | |
| No | 7 (22.6) | 22 (37.9) | |
| Cholesterol Screening (if ever) | 0.340* | ||
| Yes | 29 (93.5) | 54 (93.1) | |
| No | 2 (6.5) | 4 (6.9) |
=Fisher's Exact
only 1 (Other Modes) reported 0 preventive services
In logistic regression analysis (adjusted for sociodemographics, health and health insurance), respondents who reported having concordant communication were more likely to report a greater number of preventive services (OR 3.42; 95% CI:1.31, 8.93; p=0.012) compared with respondents with discordant communication (Table 2).
Table 2. AOR for Sum of Received Preventive Services by American Sign Language Concordant Provider.
| Factor | Adjusted Rate Ratio (95% CI) | p-value |
|---|---|---|
| Gender | ||
| Female | 1.96 (0.81, 4.27) | 0.136 |
| Male | 1 | |
| Race | ||
| White | 1 | |
| Other | 1.49 (0.21, 10.76) | 0.696 |
| Income ($) | ||
| <25,000 | 3.62 (1.08, 12.19) | 0.038 |
| 25,000–50,000 | 2.51 (0.85, 7.43) | 0.096 |
| >50,000 | 1 | |
| Education | ||
| High school or less | 1.13 (0.41, 3.13) | 0.817 |
| Some college or higher | 1 | |
| Health Status | ||
| Excellent–Good | 1 | |
| Fair–Poor | 1.26 (0.18, 8.75) | 0.814 |
| Insurance | ||
| Public | 1.52 (0.56, 4.15) | 0.409 |
| Private | 1 | |
| None | 0.760 (0.02, 34.62) | 0.888 |
| Communication with Provider | ||
| Provider Signs | 3.42 (1.31, 8.93) | 0.012 |
| Other Modes | 1 |
Discussion
The findings support the hypothesis that deaf ASL users with language-concordant healthcare communication are more likely to receive preventive services than deaf ASL users with language-discordant healthcare communication. These findings are consistent with research showing an association between language-concordant healthcare communication and appropriate healthcare services, including preventive services. 7, 10 With poor communication, preventive services may be relegated to a low priority or delayed for a variety of reasons, including time constraints and inability to communicate complex medical information for shared decision making and informed consent.
Influenza vaccination was the only individual preventive service significantly associated with ASL-concordant communication. Influenza vaccination is a recommended annual preventive service. The authors believe that better adherence here may reflect better communication, trust and patient–clinician continuity relationships associated with concordant communication. Future research should explore the reasons for influenza vaccination adherence.
Cholesterol screening (if ever) and colonoscopy/sigmoidoscopy (if ever) were not significantly associated with language concordance. The DHS did not ask follow-up questions regarding the preventive services. One possible reason the analyses did not find an association with language concordance and cholesterol is that cholesterol screening starts relatively young which leads to a higher number of opportunities for deaf ASL users to be screened, regardless of whether discordant communication occurs. This likely explains the high prevalence of cholesterol screening (if ever) rates seen for both concordant and discordant groups. For colon cancer, there are several approved methods available for screening, including the use of fecal occult blood tests (FOBT). The DHS did not ask about FOBT use. It may be that concordant communication results in higher rates of colon cancer screening via FOBT. Future research should include items on FOBT.
Communication is vital to appropriate, effective and successful healthcare. Many people, including clinicians, believe that deaf ASL users can understand non-sign-based communication. Research shows that note-writing and speech-reading, while commonly used by clinicians to communicate with deaf patients, are likely ineffective. According to one study, only 20% of deaf individuals demonstrated fluency in written English11, and that the average English reading level of deaf high school seniors is at or below a 4th-grade level.25,26 Speech reading is also inadequate, when the majority of English sounds are not clearly visible on the lips.27
The results suggest that ASL-fluent clinicians may be crucial to addressing healthcare communication barriers experienced by deaf ASL users. Research with other language minority groups suggests that bilingual clinicians have better health outcomes, including better patient satisfaction and understanding, lowered healthcare expenditures, avoidance of diagnosis and treatment errors, and improved patient–provider relationships, than healthcare using other modes of communication, including the use of professional interpreter services.28,29 ASL-fluent clinicians are uncommon, and it is important to note that the use of sign language interpreter services is still associated with better adherence with recommended preventive services compared with healthcare without sign language accessible communication.11 The use of interpreter services may also protect clinicians from malpractice concerns generated by poor communication.
This research would be difficult to do outside of Rochester NY, a city with a high per capita population of deaf ASL users. One third (31 of 89) of the respondents reported seeing a clinician who signs (language-concordant healthcare communication); this broad access to ASL-skilled clinicians is likely unique to Rochester and few other areas around the country. The participants were also predominately white (95.5%), similar to demographics in other published studies.30–32 Future research should explore the epidemiologic, genetic and/or biobehavioral reasons for the strong association between white race and deafness. The educational attainment of the DHS participants was higher than reported for deaf adults in published research using national data sets.30,31 The high educational attainment may mean that concordant communication is more important for preventive services adherence in deaf communities outside of Rochester NY.
The DHS data are all self-reported – the authors did not confirm the use of preventive services. The DHS question on healthcare communication asks about the most recent healthcare visit. It is possible that some respondents were misclassified as discordant who usually see an ASL-skilled clinician (but not at the most recent healthcare visit). This misclassification would likely result in the analyses underestimating the magnitude of the benefit of language concordant healthcare communication. Future studies could include chart audits (or other measures of preventive services use) and more detailed questions regarding healthcare communication and continuity relationships with a physician.
Conclusion
This study demonstrated for the first time with deaf ASL users the relationship between preventive services use and having a language-concordant clinician. Increasing the number of ASL-fluent clinicians (hearing or deaf themselves), and expanding their geographic reach through the use of tele-health technology, would likely improve healthcare services use and health in this underserved language minority population.
Acknowledgments
NCDHR and the DHS were supported by Cooperative Agreements U48 DP000031 and U48 DP001910 from the CDC (Pearson, PI), K08 HS15700 from the Agency for Healthcare Research and Quality (Barnett, PI) and KL2 RR 024136 from the National Center for Research Resources (Block, PI). This publication was made possible by Grant Number T32 HL007937 (Pearson, PI) and K01 HL103140-01 (McKee, PI) from the National Heart, Lung, and Blood Institute (NHLBI) of the NIH. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the CDC or the NIH. The authors want to acknowledge and thank Kimberly Schmitt McKee, MPH, Erika Sutter, MPH; Kelly Thevenet-Morrison, MS; Paul Winters, MS; and the members of the Deaf Health Community Committee for their input. The authors also wanted to thank the many deaf respondents who volunteered their time to participate in the Deaf Health Survey (DHS).
Footnotes
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Waters EA, Sullivan H, Finney Rutten L. Cancer Prevention Information-Seeking among Hispanic and Non-Hispanic Users of the National Cancer Institute's Cancer Information Service: Trends in Telephone and LiveHelp Use. J Health Commun. 2009;14(5):476–486. doi: 10.1080/10810730903032952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Woloshin S, Bickell N, Schwartz L, et al. Language barriers in medicine in the U.S. JAMA. 1995;273:724–728. [PubMed] [Google Scholar]
- 3.Carrasquillo O, Orav E, Brennan T, Burstin H. Impact of language barriers on patient satisfaction in an emergency department. J Gen Intern Med. 1999;14:82–87. doi: 10.1046/j.1525-1497.1999.00293.x. [DOI] [PubMed] [Google Scholar]
- 4.Flores G, Vega L. Barriers to health care access for Latino children: a review. Fam Med. 1998;30:196–205. [PubMed] [Google Scholar]
- 5.Torres R. The pervading role of language on health. J Health Care Poor Underserved. 1998;9:S21. [Google Scholar]
- 6.Stewart M. Effective physician–patient communication and health outcomes: a review. CMAJ. 1995;152(9):1423–1433. [PMC free article] [PubMed] [Google Scholar]
- 7.Graham E, Jacobs T, Kwan-Gett T, Cover J. Health services by low-income limited English proficiency adults. J Immigr Minor Health. 2008;10(3):207–217. doi: 10.1007/s10903-007-9069-3. [DOI] [PubMed] [Google Scholar]
- 8.Crane J. Patient comprehension of doctor–patient communication on discharge from the emergency department. J Emerg Med. 1997;15:1–7. doi: 10.1016/s0736-4679(96)00261-2. [DOI] [PubMed] [Google Scholar]
- 9.Fernandez A, Schillinger D, Grumbach K, et al. Physician language ability and cultural competence. J Gen Intern Med. 2004;19:167–174. doi: 10.1111/j.1525-1497.2004.30266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilson E, Chen A, Grumbach K, et al. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20:800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mackinney TG, Walters D, Bird GL, Nattinger AB. Improvements in preventive care and communication for deaf patients: results of a novel primary health care program. J Gen Intern Med. 1995;10(3):133–137. doi: 10.1007/BF02599667. [DOI] [PubMed] [Google Scholar]
- 12.Padden C, Humphries T. Inside Deaf Culture. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 13.Preston P. Mother father deaf: the heritage of difference. Soc Sci Med. 1995 Jun;40(11):1461–1467. doi: 10.1016/0277-9536(94)00357-y. [DOI] [PubMed] [Google Scholar]
- 14.Barnett S. Clinical and cultural issues in caring for deaf people. Fam Med. 1999;31(1):17–22. [PubMed] [Google Scholar]
- 15.Zazove P, Niemann L, Gorenflo D, Carmack C, et al. Health status and health care utilization of the deaf and hard-of-hearing persons. Arch Fam Med. 1993;2(7):745–752. doi: 10.1001/archfami.2.7.745. [DOI] [PubMed] [Google Scholar]
- 16.Tamaskar P, Malia T, Stern C, Gorenflo D, Meador H, Zazove P. Preventive attitudes and beliefs of deaf and hard-of-hearing individuals. Arch Fam Med. 2000 Jun;9(6):518–525. doi: 10.1001/archfami.9.6.518. discussion 526. [DOI] [PubMed] [Google Scholar]
- 17.Woodroffe T, Gorenflo DW, Meador HE, Zazove P. Knowledge and attitudes about AIDS among deaf and hard of hearing persons. AIDS Care. 1998 Jun;10(3):377–386. doi: 10.1080/09540129850124154. [DOI] [PubMed] [Google Scholar]
- 18.Peinkofer JR. HIV education for the deaf, a vulnerable minority. Public Health Rep. 1994 May–Jun;109(3):390–396. [PMC free article] [PubMed] [Google Scholar]
- 19.Heuttel KL, Rothstein WG. HIV/AIDS knowledge and information sources among deaf and hearing college students. Am Ann Deaf. 2001 Jul;146(3):280–286. doi: 10.1353/aad.2012.0067. [DOI] [PubMed] [Google Scholar]
- 20.Zazove P. Cancer Prevention Knowledge of People with Profound Hearing Loss. J Gen Intern Med. 2009;24(3):320–326. doi: 10.1007/s11606-008-0895-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wollin J, Elder R. Mammograms and Pap smears for Australian deaf women. Cancer Nurs. 2003 Oct;26(5):405–409. doi: 10.1097/00002820-200310000-00010. [DOI] [PubMed] [Google Scholar]
- 22.Margellos-Anast H, Estarziau M, Kaufman G. Cardiovascular disease knowledge among culturally Deaf patients in Chicago. Prev Med. 2006 Mar;42(3):235–239. doi: 10.1016/j.ypmed.2005.12.012. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Chronic Disease Prevention and Health Promotion. About the BRFSS. 2008 Available at http://www.cdc.gov/brfss/about.htm.
- 24.U.S. Preventive Services Task Force. The Guide to Clinical Preventive Services 2008. Rockville MD: Agency for Health Care Research and Quality; 2008. [Google Scholar]
- 25.Traxler C. Measuring up to performance standards in reading and mathematics: Achievement of selected deaf and hard-of-hearing students in the national norming of the 9th Edition Stanford Achievement Test. J Deaf Stud Deaf Educ. 2000;5:337–348. doi: 10.1093/deafed/5.4.337. [DOI] [PubMed] [Google Scholar]
- 26.Allen T. Patterns of academic achievement among hearing impaired students. In: Schildroth A, K M, editors. Deaf Children in America. San Diego: College Hill Press; 1986. [Google Scholar]
- 27.Barnett S. Cross-cultural communication with patients who use American Sign Language. Fam Med. 2002;34(5):376–382. [PubMed] [Google Scholar]
- 28.Hornberger J, Gibson C, Jr, Wood W, et al. Eliminating Language Barriers for Non-English-Speaking Patients. Med Care. 1996;34:845–856. doi: 10.1097/00005650-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Timmins C. The impact of language barriers on the health care of Latinos in the U.S.: A review of the literature and guidelines for practice. J Midwifery Womens Health. 2002;47:80–96. doi: 10.1016/s1526-9523(02)00218-0. [DOI] [PubMed] [Google Scholar]
- 30.Barnett S, Franks P. Health care utilization and adults who are deaf: relationship with age at onset of deafness. Health Serv Res. 2002 Feb;37(1):105–120. [PubMed] [Google Scholar]
- 31.Agrawal Y, Platz EA, Niparko JK. Prevalence of hearing loss and differences by demographic characteristics among U.S. adults: data from the National Health and Nutrition Examination Survey, 1999–2004. Arch Intern Med. 2008;168:1522–1530. doi: 10.1001/archinte.168.14.1522. [DOI] [PubMed] [Google Scholar]
- 32.Schoenborn CA, Heyman K. Health disparities among adults with hearing loss: U.S., 2000–2006. Health E-Stats. 2008:1–14. [Google Scholar]