Abstract
Objective
Determine caregiver treatment acceptability and preferences for five preventive dental treatments for early childhood caries (ECC) in young Hispanic children.
Methods
We interviewed 211 parents/caregivers of Hispanic children attending Head Start programs regarding their acceptability of and preferences for five standard preventive dental treatments for young children. Treatments assessed were: toothbrushing with fluoride toothpaste, fluoride varnish, xylitol in food for children; and xylitol gum and chlorhexidine rinse for mothers. The interview assessment included presentation of: illustrated cards with verbal description of treatment; picture/video clip; and treatment samples. Parents rated the acceptability of each treatment (1-5 scale) and treatment preferences within each of 10 possible pairs. Individual treatment preferences were summed to create overall preference scores (range 0–4).
Results
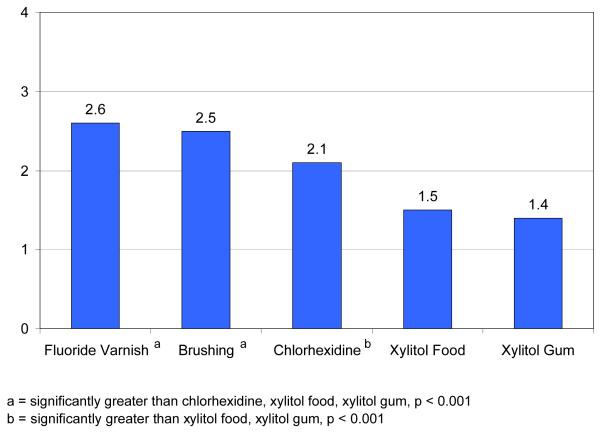
All treatments were rated as highly acceptable, however there were differences (range 4.6-4.9; Friedman Chi Square = 23.4, p< 0.001). Chlorhexidine, toothbrushing, and varnish were most acceptable, not different from each other, but more acceptable than xylitol in food (p< 0.05). Summed treatment preferences revealed greater variability (means ranged 1.4-2.6; Friedman Chi Square=128.2, p< 0.001). Fluoride varnish (2.6) and toothbrushing (2.5) were most highly preferred, and differences between preferences for xylitol in food (1.4), xylitol gum (1.5) and chlorhexidine (2.1) were all significant, p < 0.001. Preferences for chlorhexidine were also significantly greater than those for the xylitol products (p < 0.001).
Conclusions
All 5 treatments were highly acceptable, however when choosing among treatments overall, fluoride varnish and toothbrushing were favored over other treatments.
Keywords: preventive dental treatments, early childhood caries, caregiver acceptability, Hispanic children
Introduction
Treatment acceptability is considered a characteristic of service provision that should be included when planning new services, improving existing services, and measuring service quality (1). Defined as judgments by laypersons, clients, and others of whether treatment procedures are appropriate, fair, and reasonable for the problem or client (2), most acceptability research in this field falls into one of two categories: 1) traditional post-hoc program evaluation approaches including patient acceptability and satisfaction; and less commonly 2) prospective evaluations of acceptability and preferences based on characteristics of established treatments. Post-hoc evaluation may yield valuable information on treatment perception. However, perceptions may be based on individual qualities or competencies of the care provider or the setting and not on the treatment itself. Further, outcomes from this approach are based on samples of individuals who have already deemed the treatments as acceptable, as they have consented to and received the treatment. The post-hoc approach does not provide acceptability information from the broader community or population perspective. In order for treatments, which may be efficacious at the research level, to be effective when implemented within target communities, their prospective acceptability should be established within the communities for which they are intended (1).
In the field of pediatric dentistry, there has been very little research addressing acceptability of preventive treatments for children (3). A few post-hoc acceptability evaluations for children have evaluated preferences within a specific treatment based on taste, color, or some other variable feature of the treatment. For example, Berg et al. compared preferences for two different fluoride varnishes that varied in color and flavor. They found that children preferred white varnish to brown varnish, and some age groups preferred the flavor of the white varnish over the brown varnish (4). Lam et al. studied child preferences for food products containing xylitol and found that most foods were rated as acceptable by the children and that there were significant differences in preferences for specific food types (5). These post hoc studies have concluded that individuals have preferences for particular aspects of treatments, such as flavors or colors of fluoride varnish, or types of foods containing xylitol; however, as noted earlier, the results are from those who have already accepted the treatment. Subsequently, little is known regarding acceptability of and preferences for preventive treatments at the population or community level (3). This is unfortunate because previous research has shown that oral health care utilization and outcomes are determined in part by community and cultural factors that must be taken into account in the effort to improve childrens’ oral health (6-8).
Early childhood caries (ECC) is the most prevalent largely preventable chronic illness in childhood (9-11), and rates of those with caries experience are increasing nationally, particularly in low-income communities (12). Nationally, 20% of children aged 2-5 years have untreated caries, and this rate is far higher for Mexican American children (33%) and children living below the Federal Poverty Level (33%). (12). Children with ECC may suffer both physical and developmental difficulties, including pain, tooth loss, malocclusion, chewing difficulties, malnutrition, sleep disruptions, speech problems, social development delays and attention deficit (11, 13, 14).
While there are several low cost effective treatments to prevent ECC, available dental services are often underutilized in many high-risk communities (15). Better understanding of acceptability of treatments within high-risk communities could lead to greater participation in ECC prevention programs, which could result in improved oral health. Thus, it is crucial to determine acceptability and preferences for effective, low-cost preventive treatments in communities that most need them. The purpose of the present study is to examine parental/caregiver acceptability of, and preferences for preventive dental treatments to prevent ECC within a low-income Hispanic community setting.
Methods
The primary objective of our study was to determine the parental/caregiver acceptability and preferences for 5 standard preventive dental treatments known to prevent ECC either directly by application to the child or indirectly by reducing transmission of cariogenic bacteria from parent to child: tooth brushing with fluoride toothpaste (16); fluoride varnish (17); xylitol in food (18); xylitol gum (19); and chlorhexidine mouth rinse (20). The study took place in two Head Start and Early Head Start Centers within Alameda County in the San Francisco Bay Area and was approved prior to initiation by the University of California San Francisco Institutional Review Board.
Study Design
We developed an acceptability assessment to evaluate parental/caregiver acceptability and preferences for ECC preventive treatments in the Hispanic community. We worked closely with the childcare center directors, health coordinators, and staff to optimize caregiver convenience and participation. The development, reliability, and validity of the assessment have been described previously (3).
The data were collected through personal interviews conducted by a bi-lingual interviewer with a computer-aided personal interview (CAPI) program. As part of the acceptability evaluation, participants completed additional assessments including: demographic questions; the Marín Acculturation Scale, assessing acculturation related to language use, media preferences, and ethnic social relations (21); Dental Knowledge Scale (22) about children’s oral health; a modified version of the Personal Assisted Employment Services Dental Program Patient Satisfaction Survey to assess satisfaction with most recent dental care experience (23); and the Children’s Oral Health Quality of Life Scale, a caregiver report of degree of functional, psychological, and social difficulties related to oral health status (24).
Participants
Participants were recruited through fliers sent home with the children and direct personal contact during arrival and departure times at the centers. One caregiver for each household with a child 1-5 years old at the center was eligible to participate. Informed consent was obtained at the time of the interview and all materials were available in Spanish and English.
The Acceptability Interview
The interviewer first explained that all treatments were safe, effective, required no sedation or restraint, and that generally they were not intended to be done instead of, or to replace, current home care. Each individual treatment assessment consisted of the following three steps. First, the presentation of learning materials included a verbal description of the treatment accompanied by an illustrated treatment card (See Figure 1). The verbal description included information on the cards, as well as additional details on how treatments work to prevent ECC and how they are done. For example, the additional information given about tooth brushing included explaining that fluoride strengthens teeth, that teeth should be brushed for two minutes twice a day with a pea-sized amount of fluoride toothpaste, that parents should brush children’s teeth if child is younger than two years, should assist in brushing if child is between two and six years of age, and that parents should teach children to spit out toothpaste and not swallow it. In the case of the tooth brushing treatment, the interviewer explained that this treatment would potentially modify their home care if tooth brushing was part of home care and if they were doing the brushing differently than the treatment described above. For each treatment, supplies were presented (e.g., a toothbrush and fluoride toothpaste for the brushing treatment), and then a photograph (all treatments except fluoride varnish) or video clip (fluoride varnish) of the treatment was shown. We showed a nine-second video clip of a child receiving a fluoride varnish treatment because earlier focus group results indicated the importance of clarifying that, as a professionally administered treatment, it was not invasive, painful, and did not require sedation. Second, the interviewer confirmed that the participant understood the basic information of the treatment using the “teach-back method”. In the “teach-back method” parents were asked to describe the treatment in their own words. If a parent did not show a basic understanding, the treatment was explained again and the parent was asked again to explain the treatment. Third, the interviewer evaluated acceptability of the particular treatment. Here, participants were asked if they had heard of the treatment prior to the interview. They then rated whether each treatment was appropriate for a 1-2 year old child (yes, no, not sure), for a 3-5 year old child (yes, no, not sure), and how sure they were that they would want their child to receive the treatment (1-5 scale) if it were offered to him/her. For the two treatments for mothers, participants rated whether the treatment was appropriate for mothers (yes, no, not sure), and how sure they were that they would want the treatment (1-5 scale) if it were offered to them.
Figure 1.
Sample Treatment Card: Brushing Teeth with Fluoride Toothpastea
We anticipated that participants might rate all treatments as highly acceptable in the individual assessments, because the treatments are all noninvasive, primarily low in effort needed, and many are already well embedded as daily habits (tooth brushing, chewing gum, etc.); additionally a tendency to respond in a favorable socially desirable manner (rating all treatments as highly acceptable) was possible. Therefore, to obtain more specific information, we followed the individual treatment assessments with a presentation of the treatments in 10 unique pairs, one at a time (e.g. fluoride varnish paired with xylitol gum). Treatment cards were presented in pairs, with a brief review of the treatments as needed, and participants were asked to choose their preferred treatment within each pair. This information allowed us to discern preferences among treatments and to gain a sense of overall preferences. For both the individual and paired evaluations, treatments were presented in a random order to prevent bias from possible ordering effects.
Analysis
Acceptability of Five Treatments
We calculated means and standard deviations of the five individual treatment acceptability ratings, and assessed differences in those ordinal ratings among the five treatments within participants using a nonparametric Friedman rank test. We calculated Wilcoxon signed rank tests to determine whether the treatments targeting children were more acceptable in 3-5 year olds than 1-2 year olds. To compare rates of having previously heard about the preventive treatments, we utilized a nonparametric Friedman rank test and paired Wilcoxon signed rank tests with a Bonferroni-Holm correction (25).
Preferences Based on Paired Comparisons
For the paired comparisons, we used a Bradley-Terry model (26) to test within-pair preference and estimate probabilities of preference along with 95% confidence intervals (CIs). Across the paired preferences, the possible range of any treatment being chosen was 0-4 times. We summed the number of times each treatment was preferred in the 10 pairs and compared among treatment sums with a nonparametric Friedman rank test. We used paired Wilcoxon signed rank tests to evaluate summed times preferred between the five treatments, two at a time. A Bonferroni-Holm post hoc correction was used to adjust for multiple comparisons with initial alpha*=0.05/10=0.005).
Associations between treatment acceptability/preferences and participant characteristics
We assessed potential relationships of acceptability and preferences with other factors (participant’s age, years of education, level of acculturation, having heard of treatment prior to study, dental knowledge, satisfaction with past dental care, and child oral health quality of life) with Pearson correlations. To account for multiple testing, we used a Bonferroni-Holm adjustment (with the initial alpha*=0.05/35 = 0.0014) to determine the minimum reported significance level.
Results
The sample consisted of 211 Hispanic parents/caregivers (94% are parents) of children attending the childcare programs at the Head Start Centers (13% in Early Head Start and 87% in Head Start). Ninety-eight percent were female and the mean age was 30.8 (SD=7.6). Median education was ten years, with a range of 0 – 22 years. All participants identified themselves as Hispanic/Latino and 98% of the interviews were conducted in Spanish. This is consistent with the acculturation assessment that indicated that 97% of the participants would be considered to have a low level of Anglo acculturation (See Table 1). Approximately 50% of those approached agreed to participate.
Table 1.
Descriptive Statistics of Study Variables (N = 211)
| Characteristic | Mean (SDa), Median, or Percent |
Study Range |
|---|---|---|
| Caregiver age (mean years) | 30.8 (7.6) | 17-66 |
| Caregiver female gender (%) | 98% | -- |
| Hispanic/Latino ethnicity (%) | 100% | -- |
| Education (median years) | 9.8 (3.6) | 0 – 22 |
| Acculturation b (mean) | 1.7 (0.5) | 1.0 – 4.3 |
| Satisfaction with most recent dental care scale c (mean) |
2.9 (0.4) | 1.2 – 4.0 |
| Dental knowledge scale d (mean) |
8.4 (1.2) | 5 – 10 |
| Child oral health quality of life scale (caregiver reported) e (mean) |
19.5 (4.1) | 10 – 38 |
SD= Standard Deviation
Low score indicates low level of acculturation, scale range= 1-5
Low score indicates low satisfaction, scale range= 1-5
low score indicates low knowledge, scale range = 0-10
low score indicates high oral health quality of life scale range= 10-40.
Ratings of the Five Preventive Treatments
Table 2 presents results of individual treatment acceptability rating assessments. All five treatments were seen as highly acceptable, with means ranging from 4.6 (SD=0.94) for xylitol in food to 4.9 (SD=0.37) for chlorhexidine rinse. However, there were significant within-person differences in the preference ratings (Friedman Chi Square=23.4, p < 0.001). Ratings for chlorhexidine (4.9), fluoride varnish (4.8) and tooth brushing with fluoride toothpaste (4.8) were not significantly different from each other. However, these three treatments were more acceptable than xylitol in food.
Table 2.
Parental Acceptability Ratings for Five Early Childhood Caries Preventive Agents
| Treatment: N = 211 |
Heard of treatment prior to study |
Dichotomous Rating by Age |
Acceptability Rating (1-5 scale) |
||||
|---|---|---|---|---|---|---|---|
| % yes |
Friedman Chi Square 317.6 (a) *** |
OK for 1-2 year old % yes |
OK for 3-5 year old % yes |
Wilcoxon Signed Rank test between age groups(b) |
Mean (SD) | Friedman Chi Square 23.4 (a) *** |
|
| Child treatments |
Wilcoxon Signed Rank (b) |
Wilcoxon Signed Rank Test (b) |
|||||
| Fluoride varnish |
60 | >Brushing*, CHX*, Food*, Gum* |
72 | 98 | * | 4.8 (.65) | >Food* |
| Brushing with fluoride toothpaste |
45 | >CHX*, Food*, Gum* |
65 | 99 | *** | 4.8 (.66) | >Food* |
| Xylitol in food |
1 | -- | 78 | 91 | -- | 4.6 (.94) | -- |
| Mother Treatments |
OK for Mother (% yes) |
||||||
| Xylitol in gum |
9 | >Food* | 98 | -- | -- | 4.7 (.68) | -- |
| CHX | 6 | >Food* | 100 | -- | -- | 4.9 (.37) | >Food* |
p < 0.001
p < 0.05
p < 0.001
with Bonferroni-Holm correction
Brushing = tooth brushing with fluoride toothpaste , CHX = Chlorhexidine mouth rinse; Food = Xylitol in food; Gum= Xylitol gum
The dichotomous yes-no ratings of whether treatments were acceptable for different age groups (1-2 years or 3-5 years) indicated that acceptability was higher for the older age group than the younger for the tooth brushing and fluoride varnish child-based treatments (Bonferroni-Holm p<0.05).
Percentages of having heard of the treatments prior to participating in the study ranged from a high of 60% for fluoride varnish to 1% for xylitol in food (Friedman Chi Square = 317.6, p < 0.001). Fluoride varnish was significantly higher than brushing with fluoride toothpaste which was significantly higher than chlorhexidine and xylitol in gum which were significantly higher than xylitol in food. Interestingly, more caregivers had heard of fluoride varnish than of the recommended home care routine of tooth brushing with fluoride toothpaste in the prescribed manner. There were no associations between having heard of a particular treatment prior to the study and the ordinal acceptability ratings for that treatment. Likewise, there were no associations between the acceptability ratings and parent age, education, acculturation, dental knowledge, satisfaction with dental care, or child oral health quality of life.
Treatment Preferences Based on Paired Comparisons
Figure 2 presents the results of the 10 paired treatment comparisons with 50% being the reference value (where each treatment would be preferred half the time). Two of the treatments - fluoride varnish and tooth brushing with fluoride toothpaste -were consistently favored over the remaining three treatments - chlorhexidine, and both xylitol products (all p < 0.001). A similar pattern of preferences for fluoride varnish and tooth brushing indicated that both treatments were most often preferred when compared to xylitol in gum, then xylitol in food, and finally chlorhexidine rinse. In the comparison between fluoride varnish and tooth brushing, fluoride varnish was preferred 52% of the time versus 48% for tooth brushing, a non-significant difference (shown in the figure by the 95% CI crossing the 50% reference line). Chlorhexidine was preferred over xylitol in gum and xylitol in food, both p < 0.001. Xylitol in food was never significantly preferred more than any treatment; in comparing xylitol in gum to xylitol in food, there was no significant difference (the 95% CI crosses 50%).
Figure 2.
Paired Preferences Comparing Treatments Within Pairs (Bradley-Terry Model Estimated Percents and 95% Confidence Intervals)
Figure 3 presents the sample means of the preferences summed across the 10 comparisons for each of the five treatments. Summed treatment preferences differed significantly (Friedman Chi Square=128.2, p < 0.001). Fluoride varnish and tooth brushing with fluoride toothpaste were preferred over the other three treatments 2.6 and 2.5 out of 4 times, respectively (all Bonferroni-Holm p < 0.001). Chlorhexidine was preferred 2.1 out of 4 times, significantly more than either xylitol product (both Bonferroni-Holm p < 0.001).
Figure 3.
Mean Number of Times Treatment Preferred in Paired Assessments
Discussion
This is the first study, to our knowledge, to evaluate acceptability and preferences of these low-cost, standard treatments, particularly in a low-income, Hispanic sample of parents. The findings indicate that Hispanic caregivers in this non-dental Head Start setting found a range of preventive treatments for both children and mothers to be highly acceptable options for preventing ECC. The findings also indicate, however, that when given choices among these treatments, caregivers had significant preferences for fluoride varnish treatment and for a home care routine of tooth brushing with fluoride toothpaste over chlorhexidine, xylitol gum, and xylitol in food.
We intentionally targeted a homogeneous sample of Hispanic caregivers for this evaluation because Hispanic children in low-income families have especially high rates of ECC. This homogeneity in ethnicity, acculturation, and gender may in part account for the lack of variability in the individual treatment acceptability ratings. In a more diverse sample, acceptability may be more varied at the individual level. Evaluating preferences among treatment pairs allowed for a more detailed evaluation of treatment preferences.
Our finding that caregivers most preferred fluoride varnish and tooth brushing when asked to choose preferences indicates that they are interested in both receiving professional care as well as developing healthy practices at home. These two treatments were also the most commonly recognized treatments among the five treatments; however, there was no association between prior knowledge of a treatment and its overall acceptability or preference level. Because chlorhexidine and the xylitol products are relatively new and unfamiliar, it is possible that their novelty somehow played a role in their preference status in a manner not captured by our analyses.
It is also notable that a higher percentage of the sample had heard of fluoride varnish applications than had heard of a recommended standard protocol of tooth brushing as a home care routine. The Head Start programs emphasize oral health promotion through their mandatory oral health screenings and tooth brushing activities on site, so it is likely that caregivers were aware of the importance of tooth brushing for oral health, but not aware of the specific recommendations for length of time, type of toothpaste, parental role, and frequency for brushing childrens’ teeth. Throughout the data collection periods, we found that caregivers were very motivated to learn more about access to the treatment products we included in the evaluation. Given this high level of interest, and the relatively low percentage of caregivers who had previously heard of the standard tooth brushing protocol, a health education protocol that focuses on instructing caregivers in proper tooth brushing routines may have the potential to show positive results (27).
In our sample, there were no significant associations between individual factors such as parental age, education, acculturation, dental knowledge, child oral health quality of life, and parent satisfaction to acceptability and the acceptability or preferences for treatments. It is possible that there are individual characteristics that would relate to preferences that were not assessed in this study or that power was low for these assessments. It is also possible that these factors could be of potential importance for evaluating acceptability and preferences in a broader sample.
Because our acceptability evaluation included treatments that were basically low-cost, non-invasive, safe, and effective, we held these common factors constant and focused our presentations of the treatments on aspects that did vary, for instance who receives the treatment, where and how frequently is it given. We intentionally evaluated the treatments as a whole and not by their individual characteristics such as taste or smell as we were interested in caregivers overall impressions and preferences for the basic treatments and not the individual characteristics of them. Some of these preventive agents have been evolving during the last few years. For example, the range of fluoride varnish products has increased with additional flavors and colors available. Costs of professionally applied products will vary depending on reimbursement mechanism and delivery system and personal products by what might be on sale at the local store. We avoided being specific about any particular brand of product. In the presentation of learning materials for the assessment, we showed a video clip of fluoride varnish and a photograph of the other treatments. Because the acceptability and preference results were so close for fluoride varnish and tooth brushing with fluoride toothpaste, we do not think that the difference in presentation format influenced the results, however future research assessing differences in format presentations in acceptability could clarify this issue.
The findings from the study may be utilized in planning future oral health promotion programs or interventions. We chose the five treatments that have shown the greatest efficacy in preventing ECC; however, other treatments could be assessed. Future research could examine acceptability and preferences for preventive treatments in expanded population groups, particularly in groups with high ECC rates. The assessment methodology could be applied to treatment evaluations in other dental and medical settings. This type of assessment may be especially well suited to determine treatment acceptability and preferences for options that are already established with similar levels of risk and cost. This methodology could assist providers or public health planners in decision making about programs to be offered in community settings or more broadly in the public domain. This type of consumer and community involvement in health care service planning may increase population participation in prevention efforts, potentially leading to improvements in health indicators and outcomes, as well as improved quality of life (28). Understanding the acceptability of health interventions is a key component to achieving the goals of improved health and quality of life at a broad population level.
Acknowledgments
Source of Support: This study was funded by cooperative agreement U54 DE14251 from the National Institute of Dental and Craniofacial Research, and the National Center for Minority Health and Health Disparities, National Institutes of Health, US Department of Health and Human Services and grant U45MC 00023 from the Maternal and Child Health Bureau, Health Resources and Services Administration, US Department of Health and Human Services.
Prior Presentation: Findings in this manuscript were presented at the American Association for Dental Research Conference in April 2008 in Dallas.
References
- 1.Newton T. Involving the ‘consumer’ in the evaluation of dental care: a philosophy in search of data. Br Dent J. 2001;191:650–3. doi: 10.1038/sj.bdj.4801260. [DOI] [PubMed] [Google Scholar]
- 2.Kazdin AE. Acceptability of child treatment techniques: the influence of treatment efficacy and adverse side effects. Beh Therapy. 1981;12:493–506. [Google Scholar]
- 3.Hyde S, Gansky SA, Gonzalez-Vargas MJ, Husting SR, Cheng NF, Millstein SG, Adams SH. Developing an acceptability assessment of preventive dental treatments. J Public Health Dent. 2008 July 22; doi: 10.1111/j.1752-7325.2008.00088.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berg J, Riedy CA, Tercero A. Patient and parental perception of a new fluoride varnish. Compendium. 2006;27(11):614–619. [PubMed] [Google Scholar]
- 5.Lam M, Riedy CA, Coldwell SE, Milgrom P, Craig R. Children’s acceptance of xylitol-based foods. Community Dent Oral Epidemiol. 2000;28:97–101. doi: 10.1034/j.1600-0528.2000.028002097.x. [DOI] [PubMed] [Google Scholar]
- 6.Hilton IV, Stephen S, Barker JC, Weintraub JA. Cultural factors and children’s oral health care: a qualitative study of carers of young children. Community Dent Oral Epidemiol. 2007;35(6):429–38. doi: 10.1111/j.1600-0528.2006.00356.x. [DOI] [PubMed] [Google Scholar]
- 7.Kelly SE, Binkley CJ, Neace WP, Gale BS. Barriers to care-seeking for children’s oral health among low-income caregivers. Am J Pub Health. 2005;95(8):1345–1351. doi: 10.2105/AJPH.2004.045286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Butani Y, Weintraub JA, Barker JC. Assessment of the literature on oral health-related cultural beliefs for four racial/ethnic groups. BMC Oral Health. doi: 10.1186/1472-6831-8-26. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.US Department of Health and Human and Services . Oral health in America: a report of the Surgeon General. NIDCR/NIH; Rockville, MD: 2000. [Google Scholar]
- 10.Featherstone JDB, Adair SM, Anderson MH, Berkowitz RJ, Bird WF, Crall JJ, DenBesten PK, Donly KJ, Glassman P, Milgrom P, Roth JR, Snow R, Stewart RE. Caries management by risk assessment: consensus statement, April 2002. J Calif Dent Assoc. 2003;31:257–69. [PubMed] [Google Scholar]
- 11.DenBesten P, Berkowitz R. Early childhood caries; an overview with reference to our experience in California. J Calif Dent Assoc. 2003;31:139–143. [PubMed] [Google Scholar]
- 12.Dye BA, Tan S, Smith V, Lewis BG, Barker LK, Thornton-Evans G, et al. National Center for Health Statistics Trends in oral health status: United States, 1988-1994 and 1999-2004. Vital Health Stat. 2007;11(248) [PubMed] [Google Scholar]
- 13.Alameda County Public Health Department More than a toothache: untreated dental disease in our school children. Office of Dental Health. Available from: URL:http://www.acphd.org/AXBYCZ/Admin/DataReports/morethanatoothacheforemail2106.pdf.
- 14.Ramos-Gomez FJ, Weintraub JA, Gansky SA, Hoover CI, Featherstone JDB. Bacterial, behavioral and environmental factors associated with early childhood caries. J Clin Pediatr Dent. 2002;26:165–73. doi: 10.17796/jcpd.26.2.t6601j3618675326. [DOI] [PubMed] [Google Scholar]
- 15.Flores G, Vega LR. Barriers to health care access for Latino children: a review. Fam Med. 1998;30:196–205. [PubMed] [Google Scholar]
- 16.Marinho VC, Higgins JP, Sheiham A, Logan S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;(1):CD002278. doi: 10.1002/14651858.CD002278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marinho VC, Higgins JP, Logan S, Sheiham A. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2002;(3):CD002279. doi: 10.1002/14651858.CD002279. [DOI] [PubMed] [Google Scholar]
- 18.Alanen P, Isokangas P, Gutmann K. Xylitol candies in caries prevention: results of a field study in Estonian children. Community Dent Oral Epidemiol. 2000;28(3):218–24. doi: 10.1034/j.1600-0528.2000.280308.x. [DOI] [PubMed] [Google Scholar]
- 19.Isokangas P, Soderling E, Pienihakkinen K, Alanen P. Occurrence of dental decay in children after maternal consumption of xylitol chewing gum, a follow-up from 0 to 5 years of age. J Dent Res. 2000;79(11):1885–9. doi: 10.1177/00220345000790111201. [DOI] [PubMed] [Google Scholar]
- 20.Brambilla E, Felloni A, Gagliani M, Malerba A, Garcia-Godoy F, Strohmenger L. Caries prevention during pregnancy: results of a 30-month study. J Am Dent Assoc. 1998;129(7):871–7. doi: 10.14219/jada.archive.1998.0351. [DOI] [PubMed] [Google Scholar]
- 21.Marín G, Sabogal F, VanOss Marín B, Otero-Sabogal F, Pérez-Stable EJ. Development of a short acculturation scale for Hispanics. Hispanic J Behav Sciences. 1987;9:183–205. [Google Scholar]
- 22.Reisine S, Litt M. Social and psychological theories and use for dental practice. Int Dent J. 1993;43:279–87. [PubMed] [Google Scholar]
- 23.Hyde S, Weintraub JA, Satariano WA. An evaluation of the San Francisco Department of Human Services Welfare Dental Program. J Public Health Dent. 2005;65(2):104–9. doi: 10.1111/j.1752-7325.2005.tb02794.x. [DOI] [PubMed] [Google Scholar]
- 24.Filstrup SL, Briskie D, da Fanseca M, Lawrence L, Wandera A, Inglehart MR. Early childhood caries and quality of life: child and parent perspectives. Pediatric Dent. 2003;25(5):431–440. [PubMed] [Google Scholar]
- 25.Holm S. A simple sequentially rejective multiple test procedure. Scandinavian Journal of Statistics. 1979;6:65–70. [Google Scholar]
- 26.Agresti A. Categorical data analyses. 2nd Edition Wiley; New York: 2002. [Google Scholar]
- 27.Plutzer K, Spencer AJ. Efficacy of an oral health promotion intervention in the prevention of early childhood cares. Community Dent Oral Epidemiol. 2007 doi: 10.1111/j.1600-0528.2007.00414.x. doi:10.1111/j.1600-0528.2007.00414.x. [DOI] [PubMed] [Google Scholar]
- 28.Green LW, Kreuter MW. Health program planning: an educational and ecological approach. 4th Edition McGraw Hill; San Francisco: 2005. [Google Scholar]