Efficacy of Ketogenic Diet in Severe Refractory Status Epilepticus Initiating Fever Induced Refractory Epileptic Encephalopathy in School Age Children (FIRES).
Nabbout R, Mazzuca M, Hubert P, Peudennier S, Allaire C, Flurin V, Aberastury M, Silva W, Dulac O. Epilepsia 2010;51(10):2033–2037.
PURPOSE: Fever induced refractory epileptic encephalopathy in school age children (FIRES) is a devastating condition initiated by prolonged perisylvian refractory status epilepticus (SE) triggered by fever of unknown cause. SE may last more than 1 month, and this condition may evolve into pharmacoresistant epilepsy associated with severe cognitive impairment. We aimed to report the effect of ketogenic diet (KD) in this condition. METHODS: Over the last 12 years we collected data of nine patients with FIRES who received a 4:1 ratio of fat to combined protein and carbohydrate KD. They presented with SE refractory to conventional antiepileptic treatment. RESULTS: In seven patients, KD was efficacious within 2–4 days (mean 2 days) following the onset of ketonuria and 4–6 days (mean 4.8 days) following the onset of the diet. In one responder, early disruption of the diet was followed by relapse of intractable SE, and the patient died. Epilepsy affected the other six responders within a few months. DISCUSSION: KD may be an alternative therapy for refractory SE in FIRES and might be proposed in other types of refractory SE in childhood.
Commentary
Status epilepticus has a high degree of long-term functional poor outcomes, with mortality rates as high as 50% (1). Standard anticonvulsant treatments include benzodiazepines, phenytoin, and phenobarbital; newer agents include levetiracetam and valproate (2). Unfortunately, status epilepticus can remain refractory to these interventions, at times requiring anesthetics such as pentobarbital, midazolam, propofol, and ketamine to achieve burst suppression (2). Yet even these treatments can eventually fail, with patients experiencing persistent seizures when they are weaned off general anesthesia. Sadly, few other options are then available.
The ketogenic diet is a high-fat, low-carbohydrate nonpharmacologic treatment for epilepsy (3). In continuous use since 1921, over the past two decades, there has been a dramatic resurgence in research and clinical interest in this therapy, typically for children with intractable epilepsy. There is a misperception that the ketogenic diet is universally comprised of bacon, eggs, and heavy whipping cream. The reality is that several all-liquid ketogenic formulas exist and can be provided by a trained dietitian, typically for infants and children with gastrostomy tubes (3).
The study by Nabbout and her colleagues from five centers in France and Argentina retrospectively examined their use of the ketogenic diet for refractory status epilepticus caused by the condition FIRES, (fever-induced refractory epileptic encephalopathy) in school age children (4). In this epileptic encephalopathy, previously normal children aged 4 to11 years develop the abrupt onset of typically refractory febrile status epilepticus without a clear pathogen identified. The prognosis for epilepsy and cognitive development is quite poor. Nine children, ages 5 to 8 years were treated with the ketogenic diet after from three to six anticonvulsants used as long as 55 days had failed to control their status epilepticus. One can only imagine the ketogenic diet was perceived a last hope for survival for most of these children.
The ketogenic diet was started using various formulas via nasogastric tubes, and glucose was removed from both medications and intravenous fluids. Within a mean of 2.8 days, all but one of these children developed ketonuria and, remarkably, seven of these eight children rapidly responded to the ketogenic diet. The authors add details regarding one subject, a 6-year-old boy, who became seizure-free but within hours returned to status epilepticus after the ketogenic diet was stopped by the intensivists who did not believe it was helping. He later died of his condition. All six successfully treated children did develop sporadic seizures 1 to 6 months after recovering from status epilepticus, not surprisingly.
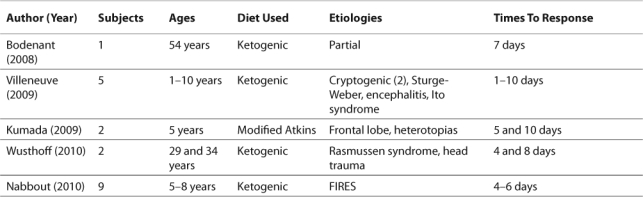
Although this study is not the first to report the successful use of the ketogenic diet for status epilepticus, it is the largest. The first case report was only 2 years prior, from Bodenant and colleagues, also from France (5). Three other retrospective studies, including adults as well as children, the modified Atkins as well as the ketogenic diet, and other etiologies, have since followed (6–8). All five reports share a common finding of success within 10 days when present (see Table).
Table 1.
Studies Examining the Ketogenic Diet for Status Epilepticus to Date
Now is the time for a prospective study of the ketogenic diet for refractory status epilepticus. There are several reasons why this treatment is a logical option for these patients. First, the ketogenic diet has a long track record of success for very refractory epilepsy. Second, all patients in status epilepticus for days will need to have adequate enteral nutrition established, so switching their formula to a ketogenic one is very feasible. In addition, evidence suggests that the ketogenic diet works very rapidly, in one retrospective study within a median of 5 days of diet onset (9). As a nonpharmacologic therapy, the ketogenic diet also does not have any known interactions with antibiotics or anticonvulsants. Lastly, some evidence would suggest a possible anti-inflammatory action, which may explain its success specifically for status epilepticus caused by encephalitis (10).
This approach does have limitations that need to be addressed in further trials. Dietitians need to be not only immediately available to start the diet in an emergency, but also familiar with the ketogenic diet and its adverse effects. These short-term side effects include acidosis, hypoglycemia, weight loss, and gastroesophageal reflux, which can obviously complicate the care for a critically ill patient (3). Adequate nutrition needs to be assured, and at present this therapy is limited to patients who can receive it via gastric or nasogastric feeding tubes. If successful, continued provision of the diet can be arranged upon discharge from the intensive care unit and eventually the hospital. Availability of ketogenic formulas and dietitians might limit this: the diet should not be started if it cannot be continued.
References
- 1.Cooper A. D., Britton J. W., Rabinstein A. A. Functional and cognitive outcome in prolonged refractory status epilepticus. Arch Neurol. 2009;66:1505–1509. doi: 10.1001/archneurol.2009.273. [DOI] [PubMed] [Google Scholar]
- 2.Abend N. S., Dlugos D. J. Treatment of refractory status epilepticus: Literature review and a proposed protocol. Pediatr Neurol. 2008;38:377–390. doi: 10.1016/j.pediatrneurol.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 3.Kossoff E. H., Zupec-Kania B. A., Rho J. M. Ketogenic diets: An update for child neurologists. J Child Neurol. 2009;24:979–988. doi: 10.1177/0883073809337162. [DOI] [PubMed] [Google Scholar]
- 4.Nabbout R., Mazzuca M., Hubert P., Peudennier S., Allaire C., Flurin V., Aberastury M., Silva W., Dulac O. Efficacy of ketogenic diet in severe refractory status epilepticus initiating fever induced refractory epileptic encephalopathy in school age children (FIRES) Epilepsia. 2010;51:2033–2037. doi: 10.1111/j.1528-1167.2010.02703.x. [DOI] [PubMed] [Google Scholar]
- 5.Bodenant M., Moreau C., Sejourne C., Auvin S., Delval A., Cuisset J. M., Derambure P., Destee A., Defebvre L. Interest of the ketogenic diet in a refractory status epilepticus in adults. Rev Neurol (Paris) 2008;164:194–199. doi: 10.1016/j.neurol.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 6.Villeneuve N., Pinton F., Bahi-Buisson N., Dulac O., Chiron C., Nabbout R. The ketogenic diet improves recently worsened focal epilepsy. Dev Med Child Neurol. 2009;51:276–281. doi: 10.1111/j.1469-8749.2008.03216.x. [DOI] [PubMed] [Google Scholar]
- 7.Wusthoff C. J., Kranick S. M., Morley J. F., Bergqvist A. G. C. The ketogenic diet in treatment of two adults with prolonged nonconvulsive status epilepticus. Epilepsia. 2010;51:1083–1085. doi: 10.1111/j.1528-1167.2009.02388.x. [DOI] [PubMed] [Google Scholar]
- 8.Kumada T., Miyajima T., Kimura N., Saito K., Shimomura H., Oda N., Fujii T. Modified Atkins diet for the treatment of nonconvulsive status epilepticus in children. J Child Neurol. 2010;25:485–489. doi: 10.1177/0883073809347597. [DOI] [PubMed] [Google Scholar]
- 9.Kossoff E. H., Laux L. C., Blackford R., Morrison P. F., Pyzik P. L., Hamdy R. M., Turner Z., Nordli D. R., Jr. When do seizures usually improve with the ketogenic diet? Epilepsia. 2008;49:329–333. doi: 10.1111/j.1528-1167.2007.01417.x. [DOI] [PubMed] [Google Scholar]
- 10.Ruskin D. N., Kawamura M., Masino S. A. Reduced pain and inflammation in juvenile and adult rats fed a ketogenic diet. PLoS One. 2009;4:e8349. doi: 10.1371/journal.pone.0008349. [DOI] [PMC free article] [PubMed] [Google Scholar]


