Abstract
In the last decade, laparoscopy has been the most innovative surgical movement in general surgery. Minimally invasive surgery performed through a few small incisions, laparoscopy is the standard of care for the treatment of gallbladder disease and the gold standard for the treatment of reflux disease. The indications for a laparoscopic approach to abdominal disease continue to increase, and many diseases may be treated with laparoscopic techniques. At Ochsner, laparoscopic techniques have demonstrated better cosmetic results, shorter recovery times, and an earlier return to normal activity compared with open surgery.
Open abdominal surgery is performed through large incisions so that the area being operated on is in direct view. This is effective but leads to lengthy recovery times, significant absence from work and regular activities, and large cosmetic defects. First used in general surgery in 1988 to remove a gallbladder (1, 2), laparoscopy is minimally invasive surgery performed through small incisions. Compared with traditional open surgery, laparoscopic procedures shorten recovery times, allow patients to return to work and regular activities faster, and produce better cosmetic results. The development of laparoscopic techniques began a revolution in general surgery, and now minimally invasive techniques are used for many different abdominal procedures. At Ochsner, we are developing new and better ways to care for patients with a program in advanced laparoscopy designed to perfect established techniques, find new applications, and teach laparoscopic surgery.
Laparoscopy begins with small incisions kept open with tubes called trocars. The abdomen is insufflated with carbon dioxide gas to make room for the surgery to be performed, and a camera is attached to a laparoscope allowing a view of the procedure on a video monitor. All laparoscopic instruments are long and thin enabling them to be inserted through trocars to reach the area of surgery.
Contraindications to laparoscopic surgery are only relative. Uncorrectible coagulopathy, severe chronic obstructive pulmonary disease, late pregnancy, and surgical inexperience may necessitate open surgery. Scarring from previous operations is usually not an indication for open surgery. For malignant diseases, laparoscopy has been used mainly as a staging procedure.
Gallbladder Diseases and Common Bile Duct Stones
Cholecystectomy is recommended for patients with complications due to gallstones (duct obstruction and biliary pancreatitis) or related symptoms varying from minor right upper quadrant pains lasting from a few seconds to a few hours (biliary colic or chronic cholecystitis) to pain lasting longer than 12 hours that sends the patient to the emergency department (acute cholecystitis). The patient may also feel pain when the gallbladder is pressed. An abdominal ultrasound should be performed before cholecystectomy to confirm the presence of gallstones. Although the results of the ultrasound will be normal in 5% of patients with gallstones, this remains the single best test. The ultrasound may also show signs of acute or chronic cholecystitis (thickened gallbladder wall, fluid around the gallbladder) or common duct stones. Results of liver function tests should also be obtained to rule out other liver diseases and assess the risk of common duct stones.
Traditional open cholecystectomy is performed through a 5-inch incision under the right rib cage and requires a minimal 3-day hospital stay and 4-week absence from work. The laparoscopic operation is performed through four trocar sites (one in the umbilicus for the laparoscope and three under the right costal margin to perform the surgery) and can often be performed as an outpatient procedure.
Laparoscopic cholecystectomy begins with the identification of the cystic duct and artery and, if indicated, a cholangiogram. A laparoscopic common duct exploration and stone retrieval is performed for choledocholithiasis, saving the patient either open surgery for common duct stones or postoperative endoscopic retrograde cholangiopancreatography (ERCP). The gallbladder is then removed through the umbilical trocar site.
A recent unpublished review of our experience with outpatient laparoscopic cholecystectomies attempted between 1990 and 1997 demonstrated no major complications due to same day surgery. Of 2288 patients, 847 (37%) were scheduled as outpatients. Of those, 74% completed their course as outpatients, an additional 24% stayed only one night, and 3% were converted to open procedure. Two-thirds of patients preferred outpatient surgery and most returned to work in 1–2 weeks.
Gastroesophageal Reflux Disease
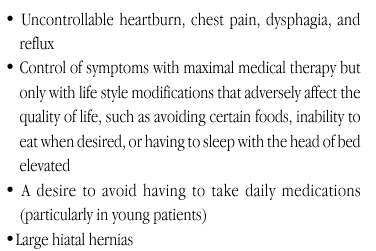
Laparoscopic fundoplication for gastroesophageal reflux disease is the fastest growing area of laparoscopic surgery. Symptoms of severe reflux disease can usually be relieved with proton pump inhibitors; however, there are several indications for surgery (Table 1). Rarely will side effects of medical therapy cause a patient to choose surgery.
Table 1.
Indications for surgery in patients with severe gastroesophageal reflux disease
Complications of reflux disease include esophageal stricture, esophageal ulceration, and Barrett's esophagus (which carries a cancer risk). It is important to emphasize the use of medical or surgical therapy to avoid these complications and to make sure that therapy is adequate when complications occur in order to avoid progression of the disease. There is no conclusive evidence that either maximal medical or surgical therapy is more beneficial for these complications though some evidence has suggested that surgery decreases the need for recurrent dilation of esophageal strictures.
Before surgery, all patients undergo esophagogastro-duodenoscopy to evaluate esophagitis from reflux, hiatal hernia, stricture, or Barrett's esophagus. An esophageal motility study is performed to rule out the possibility of achalasia, which can mimic reflux disease, and to evaluate esophageal peristalsis. A 24-hour esophageal pH probe is used when the diagnosis is in doubt. A barium swallow examination is useful in patients with large hiatal hernias, strictures, or Barrett's esophagus to help determine esophageal length.
Open surgery, performed through an upper midline incision, requires a hospital stay of at least 4–7 days, during which time the bowel begins to function as the ileus resolves. Patients generally return to work in 4–6 weeks. The laparoscopic procedure generally necessitates a single day of hospital stay; patients can generally return to light work in about 2 weeks. Patients are kept on a strict soft diet for 2 weeks postoperatively to allow swelling of the surgical area to abate.
Laparoscopic fundoplication is performed through five trocar sites. The laparoscope is placed near the umbilicus on the left side, and two trocars are placed just below the costal margin on both sides of the midline. The operation involves identification of the crura of the diaphragm and dissection around the esophagus, dissection of the short gastric vessels, and wrapping the fundus of the stomach around the esophagus. If esophageal peristalsis is normal, the wrap will be placed completely around the esophagus (called a Nissen fundoplication), or, if the peristalsis is poor, the wrap will be placed only partially around the esophagus. A partial gastric wrap puts less pressure than a full wrap on the lower esophageal sphincter and decreases the risk of the wrap causing dysphagia. A partial wrap is usually placed posteriorly around the esophagus, called a Toupet fundoplication. If the esophagus is too short, a laparoscopic esophageal lengthening procedure is performed. The stomach is stapled in such a way that a tube is formed distal to the lower esophageal sphincter and the fundoplication is performed around this tube.
Between January 1998 and December 1999, we performed 96 laparoscopic fundoplications for reflux disease at Ochsner. Average hospital stay was 1.7 days, less than half the average stay for open procedures. With short-term follow-up, 98% of patients were free of heartburn and none had symptoms of regurgitation. Dysphagia was experienced by 5.5% of patients but all responded to dilation. One patient was readmitted and required operation for bleeding.
Achalasia
Achalasia is a disease of the esophagus in which the lower esophageal sphincter does not relax with swallowing and there is no peristalsis. Symptoms are dysphagia and weight loss. There are currently three treatment options. A substance called Botulina toxin can be injected into the lower esophageal sphincter to relax the sphincter—this is usually reserved for patients who are too ill to undergo surgery and is effective in only 50% of patients, in most of whom dysphagia will recur. Forced balloon dilation of the lower esophageal sphincter is effective in 80% of patients, but again the disease will recur in many, and this therapy carries a 5% risk of esophageal perforation, a devastating complication. Surgery is 90% effective, recurrence is rare, and when ineffective, it is usually because the esophagus is very dilated.
The most important aspect of treating achalasia is performing definitive treatment as soon as possible. If treatment is delayed, the esophagus becomes dilated. Since patients with achalasia have no peristalsis, they rely on gravity to bring food boluses down the esophagus. When the esophagus becomes dilated, food tends to remain in the esophagus even after the lower esophageal sphincter is adequately opened. If surgery has not already been attempted in a patient with a dilated esophagus, it is worth trying, but the chances that it will be effective are reduced. The next best treatment option is then esophagectomy, a much more involved procedure.
Open surgery for achalasia is performed through an upper midline incision. Bowel function returns over 4–7 days, which is the usual length of hospital stay, and return to work is in 4–6 weeks. Laparoscopic patients spend 1–2 days in the hospital and are discharged on a full liquid diet. They are advanced to a soft diet 1 week postoperatively and then to a regular diet 2 weeks postoperatively when they may return to work on light duty.
Although we have performed some minimally invasive procedures through the chest, we currently favor the abdominal approach, a modified form of an operation described by Heller in 1913 involving severing the muscle of the lower esophageal sphincter (3). Laparoscopic Heller myotomy requires five trocar sites and is similar in many ways to laparoscopic fundoplication except that a myotomy of the lower esophageal sphincter is followed by a partial fundoplication by wrapping the fundus of the stomach posteriorly around the lower esophagus. This helps prevent reflux without an increased risk of dysphagia.
By the time of the last review of our series we had performed 21 Heller myotomies, 16 of which were through the laparoscopic (abdominal) approach (4). Hospital length of stay averaged 2.25 days, and of the 21 patients, four had postoperative dysphagia but only one was severe enough to require the medical intervention of dilation.
Groin Hernia
Hernias are often found on routine physical examination, and patients are asymptomatic on presentation to the surgeon. Unlike many other surgical procedures, hernia surgery is most often performed to prevent complications, including hernia growth, and incarceration or infarction of hernia contents and pain.
Open herniorrhaphy can be performed with general, spinal, or local anesthesia with intravenous sedation and most patients leave the same day as surgery. Recovery time is 2 weeks for light duty and 4–6 weeks for heavy duty; however, surgery for bilateral and recurrent hernias requires a more prolonged recovery time.
All patients with groin hernias, including recurrent and bilateral hernias, can be considered for laparoscopic surgery, except those with prior midline lower abdominal incisions or those who cannot undergo the general anesthesia required for laparoscopic groin hernia repair. Most patients are discharged the same day as surgery and most (with desk jobs) can go back to work 1 week after surgery, and can increase activity after 2 weeks. A longer recuperative time, usually 4 weeks, is necessary for heavy activity. This quick recovery can be expected even after surgery for bilateral and recurrent hernias.
In the laparoscopic procedure, three trocars are placed in the midline between the navel and the pubic symphysis. Both groins can be accessed through the same trocar sites. Dissection is performed in the preperitoneal space between the peritoneum and the musculature of the abdominal wall. After the groins are dissected and the hernias reduced into the abdomen, a large patch is placed over the hernia defect and stapled in place.
Ventral or Incisional Hernia
Laparoscopic ventral hernia repair is indicated for complicated hernias such as recurrent hernias, multiple defects in the abdominal wall, or defects that are hard to find on physical examination. The overall cosmetic result of laparoscopic repair of an incisional hernia may not be different from open repair because of the prior incision. Discharge is usually the same day as surgery, and recovery time is shorter than for open surgical repair.
Laparoscopy is performed to evaluate the size of the defect and to find the exact site of the defect to minimize scarring. For small defects, a primary repair uses two trocar sites. For larger defects, three trocar sites are used and a large patch is stapled around its perimeter on the inside of the abdominal wall overlaying the defect and spreading well beyond the defect edges.
Splenic Diseases
Laparoscopic splenectomy is performed mostly for hematologic diseases such as idiopathic thrombocytopenic purpura (ITP), thrombotic thrombocytopenic purpura (TTP), autoimmune hemolytic anemia, and heredity spherocytosis. Laparoscopic splenectomy is very difficult if the spleen is much enlarged.
Open splenectomy is performed through an upper midline incision or an incision below the rib cage on the left side, a procedure requiring a 4-day hospital stay and 4–6 weeks off work.
The laparoscopic procedure is performed through four trocar sites under the left costal margin. In the laparoscopic procedure, the spleen is detached from the stomach, diaphragm, colon, and retroperitoneum. The hilum is divided and the edges of a bag are brought through one of the trocar incisions. The spleen is then removed in small pieces. Most patients are discharged the day after surgery and return to normal physical activities in 2 weeks.
Ochsner's experience with splenectomy from 1992 to 1999 (unpublished) involved 33 attempted cases, 79% of which were completed laparoscopically with most of the conversions to open surgery in the early experience. Results were similar for laparoscopic and open splenectomy with improvement in 86% of ITP patients, 100% of TTP patients, and 40% of patients with autoimmune hemolytic anemia.
Adrenal Gland Diseases
Adrenal disease requiring surgery is rare. Most adrenal resections are for benign lesions called adenomas that can be functional and secrete adrenal hormones such as aldosterone which causes hypertension (primary hyperaldosteronism). Other lesions are removed because their size, growth, or appearance on CAT scan suggests the possibility of adrenal cancer.
Laparoscopic adrenalectomy is indicated for any adrenal lesion less than 10 cm. Both the right and left adrenal glands are easily resected laparoscopically, and bilateral adrenalectomy can also be performed. We perform laparoscopic adrenalectomy through the flank on the side of the lesion with three to four trocars placed just below the costal margin. On the left side, the spleen is freed from its lateral attachments and brought medially, and, once the adrenal gland is identified in the retroperitoneum, the adrenal vein is ligated and divided. The gland is then separated from the surrounding tissue, placed in a visceral bag, and removed from the abdomen. On the right side, the liver edge is lifted up to reveal the posterior edge of the liver. The peritoneum is incised along the posterior edge of the liver from lateral to medial until the inferior vena and the incision is brought along the inferior vena cava caudad. The adrenal vein is found along the lateral border of the inferior vena cava, ligated, and divided. The gland is identified, freed from the surrounding tissue, placed in a visceral bag, and removed from the abdomen.
In a recent review of our experience with laparoscopic and open surgery for primary hyperaldosteronism (5), 10 procedures were performed open and 14 laparoscopically; the size of the lesions was similar in both groups. Four of the laparoscopic cases were converted to open surgery early on, but none since we adopted the technique described above. Unlike most laparoscopic procedures, operative time and response to surgery were similar to those for open surgery; however, blood loss and complications were less in the laparoscopic group. For open adrenalectomy patients, hospital length of stay was twice that of the laparoscopic group (6.7 days compared with 3.3 days), many of whom required only 1 day in the hospital after laparoscopic adrenalectomy.
Appendicitis
Laparoscopic appendectomy, which has several advantages over open appendectomy, is indicated whenever appendicitis is suspected. Although the recovery time is shorter than for open appendectomy, the length of hospital stay is nearly the same. The main advantages of the laparoscopic approach are for cosmesis, a difficult appendectomy, or a diagnosis that turns out not to be appendicitis. The latter two are advantages for laparoscopy because in open surgery these difficulties often require enlarging an incision, which increases recovery time. Laparoscopy allows the surgeon to evaluate the entire abdomen without changing incisions.
The laparoscopic procedure is performed through three trocar sites, one within the navel and two in the midline below the navel. After the appendiceal mesentery is divided with a bipolar electrocautery, the appendix is resected from the cecal base between ligatures, placed in a visceral bag, and removed from the abdomen. If the appendix appears normal, the abdomen is explored and the appendix is removed unless contraindicated.
Open surgery is performed through a right lower quadrant incision 2–4 inches long requiring an average hospital stay of 2 days and a 1–4 week recovery period depending on the difficulty of the operation. Laparoscopic surgery can require only 1 day in the hospital, particularly if the appendicitis is of recent onset. If not, several days of intravenous antibiotics are usually required before the patient is discharged. (We have not yet compiled definitive data on laparoscopic appendectomy recovery times.)
Other Laparoscopic Alternatives
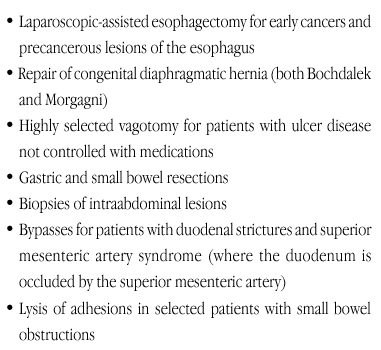
As our experience with laparoscopy grows, so does the number of diseases amenable to this surgical technique. Several laparoscopic procedures recently performed at Ochsner are shown in Table 2. For all of these procedures, cosmetic results have been better and hospital stays and return to work and regular activities have been shorter than for typical open surgery.
Table 2.
Laparoscopic procedures recently performed at Ochsner
Conclusion
Laparoscopy is now the standard of care for cholecystectomy, and many surgeons would call it the gold standard for reflux disease and achalasia. Laparoscopic cholecystectomy and appendectomy are relatively easy to perform, but many other procedures require advanced laparoscopic techniques and should be performed by experienced surgeons. Laparoscopic procedures provide a better cosmetic outcome, shorter recovery time, and an earlier return to normal activity than open surgery and with ever increasing experience are becoming viable alternatives to an ever increasing variety of traditional open surgical procedures.

Dr. Richardson is Ochsner's Director of Laparoscopic Surgery
References
- McKernan J. B., Saye W. B. Laparoscopic general surgery. J Med Assoc Ga. 1990;79:157–159. [PubMed] [Google Scholar]
- Reddick E. J., Olsen D. O., Daniel J. F. Laparoscopic laser cholecystectomy. Laser Med Surg News. 1989;7:38–40. [Google Scholar]
- Heller E. Extramucosal cardioplasty in chronic cardiospasm with dilation of the esophagus. (Extramuköse Cardioplastik beim chronischen Cardioplasmus mit Dilation des Oesophagus) Mitt Grenzgeb Med Chir. 1913;27:141. [Google Scholar]
- Richardson W. S., Bowen J. C. Minimally invasive esophageal surgery. Surg Clin N Am. 1998;78:795–803. doi: 10.1016/s0039-6109(05)70351-0. [DOI] [PubMed] [Google Scholar]
- Duncan J. L., Fuhrman G. M., Bolton J. S. Laparoscopic adrenalectomy is superior to open approach to treat primary hyperaldosteronism. Am Surg 2000, in press. [PubMed] [Google Scholar]


