Abstract
Endoscopic plantar fasciotomy (EPF) is a minimally invasive and minimally traumatic surgical treatment for the common problem of chronic plantar fasciitis. This procedure is indicated only for the release of the proximal medial aspect of the fascia in cases that do not respond to aggressive conservative, nonsurgical treatment. In the literature, an overall 87% success rate has been reported in 1228 procedures, in addition to an 83% success rate reported by Burke at the Northwest Podiatric Foundation Surgical Seminar in January 2000. The author's personal experience with 41 procedures over 5 years is consistent with an overall average success of 90%. EPF complications are reduced in comparison with traditional open procedures and can be avoided in many cases when identified early and treated properly. EPF is recommended as the procedure of choice when conservative treatment measures have been exhausted.
Plantar fasciitis, with or without an inferior calcaneal spur, is one of the most common foot problems reported to primary care physicians, orthopedic surgeons, or podiatric physicians. Fortunately, 85–90% of these cases will respond to conservative treatment including stretching, taping, orthotic devices, and anti-inflammatory medications (steroidal and nonsteroidal), along with local physical therapy measures. When these treatments fail, the remaining option is surgical intervention for the release of the fascia, with or without excision of the calcaneal spur. The endoscopic plantar fasciotomy (EPF) is a minimally traumatic procedure among many surgical alternatives for release of the fascia. (This procedure does not involve removal of the calcaneal spur.)
First described and recommended by Barrett and Day in 1991 (1) as an alternative to the traditional open technique, EPF significantly minimizes the surgical trauma that is normally associated with conventional heel spur surgery and allows patients to return to regular activities sooner and with less pain and discomfort than with other techniques. The indications for the procedure are the same as with traditional heel spur surgery/plantar fasciotomy. However, this procedure is not a replacement for aggressive conservative therapy, nor should it be considered a conservative treatment modality before an open fasciotomy is performed.
Surgical Technique
After appropriate anesthesia is achieved, the foot is prepared and draped in the usual sterile orthopedic manner. The foot is exsanguinated, and a pneumatic tourniquet is inflated. A 5mm vertical incision is made at the medial aspect of the heel, located immediately anterior and inferior to the medial calcaneal tubercle. This point can be determined by the examination of a nonweightbearing lateral radiograph or by direct palpation of the surgical site. Blunt dissection is performed to the level of the fascia, and a fascial elevator is used to create a channel immediately inferior to the plantar fascia through which the obturator/cannula system is introduced and advanced to the lateral aspect of the foot (Figure 1). A 5mm vertical incision is made to allow exit of the cannula, and the endoscope is introduced medially to visualize the inferior surface of the plantar fascia on the monitor (Figure 2a). The interior wall of the cannula is marked to correspond with the average medial band width (to be used only as a guide) obtained from cadaver dissection (2). When the medial investment of the fascia has been visualized and probed, the retrograde knife is introduced and the medial band severed (Figure 2b). The endoscope is then introduced laterally and the probe medially to provide 180° perspective, and any remaining fibers are severed. It is crucial that the medial slip be completely released. The lateral one half to two thirds of the fascial band is left intact, and the underlying musculature should be easily visualized (Figure 2c).
Figure 1.

Intraoperative photograph of instrumentation in place
Figure 2.
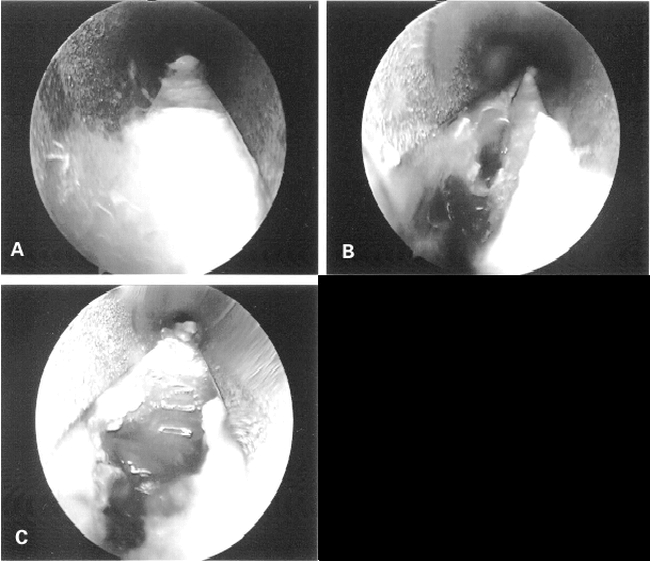
A. Intact plantar fascia. B. Releasing the medial band of the fascia. C. Visualizing the musculature after the fasciotomy
When the fasciotomy is completed, the area is irrigated, and the cannula removed, the incisions are reapproximated and the area is infiltrated with bupivacaine and dexamethasone. A sterile compression dressing is applied and the tourniquet deflated. Patients should begin weightbearing to tolerance within the first 24 hours. The dressings are changed at 3 days with medial suture removal at 10 days and lateral suture removal at 21 days. After the medial sutures are removed, an athletic shoe can be worn as tolerated.
Literature Review
Barrett and Day's original presentation described a 100% success rate with seven procedures (1). In 1993, they followed up with a review of 65 procedures reporting 95.3% total relief of symptoms (3). The same year, Kinley et al compared the endoscopic procedure (66 cases) with traditional surgery (26 cases) demonstrating an 80% resolution of symptoms with EPF 4 weeks sooner than with traditional treatment, as well as less postoperative pain and fewer complications (4). Visser et al subsequently reported a series of 50 procedures with 90% of the patients reporting the elimination of heel pain (5). The largest review to date, a prospective analysis of 652 cases, involved 25 surgeons who completed the same accredited cadaveric training symposium (6). All patients returned to normal shoe gear in 1–26 days (mean 5 days). The range of days until pain was less than preoperatively was 1–180 days (mean 6 days). Overall, heel pain was successfully relieved in 633 of the 652 cases.
In an early (1992–1994) review of 40 cases by Stone and Davies, 70% of the patients stated they would recommend the procedure to others with heel pain or would undergo the procedure again given the same choice (7). Stone and McClure reviewed 25 additional cases from 1994–1997 using identical criteria and found that 92% would recommend the procedure to others and 84% would do it again (8). In Brekke and Green's comparison of surgical treatments to correct plantar fasciitis (n=54), the 17 EPF patients had the least postoperative pain and returned to their feet the fastest, returning to normal activities 5 weeks sooner than those undergoing minimal incision or open approach procedures (9).
Ongoing Study
At the Northwest Podiatric Foundation Surgical Seminar in January 2000, Dr. Harry Burke reported an 83% success rate (with 2-year follow-up) with 265 EPF patients over a 6-year period. Additionally, he reported 34 complications, most involving lateral column pain (generally presenting as pain of the calcaneal-cuboid and metatarsal-cuboid joints) and extensor tendonitis. Most patients responded to conservative treatments. (Dr. Burke intends to publish his results upon completion of 500 procedures.)
Author's Experience
The author performed 41 EPF procedures from January 1995 through December 1999. Chart review and patient interviews regarding preoperative and postoperative status of 40 cases indicated that 36 have resulted in the resolution of heel pain and two cases were unchanged from the previous pain level—a beautician working 12–15 hours per day and a postal worker with a walking delivery route of 12 miles daily. The two remaining patients related less pain than preoperatively but were not pain-free. As of February 2000, the most recent patient (early December 1999) had returned to work without the original heel pain.
Overall published data reflect an average success of nearly 87% with 922 procedures. In comparison with Dr. Burke's yet to be published data reflecting an 83% success rate involving 265 procedures, the author's experience is consistent with a 90% success rate involving 41 procedures.
Discussion
As demonstrated with many other surgical procedures (laparoscopic, general, gynecologic, and vascular), minimally traumatic techniques decrease postoperative pain and facilitate an earlier return to regular activity. Minimization of tissue dissection and the earliest return to daily activities are goals of any surgical procedure. The EPF procedure is not without complications; however, the rate of complications is lower compared with traditional techniques (4, 6, 9). The most commonly encountered complications include lateral column pain and instability, possibly secondary to releasing more than one third to one half of the fascia. Other complications included medial arch strain and compensatory tendonitis. When identified early and treated properly, long-term complications can be avoided in many cases.
Summary
Plantar fasciitis accounts for a large percentage of cases seen by podiatric physicians and is often seen by general practitioners and orthopedic surgeons. Although most cases respond to 4–6 months of conservative nonsurgical treatment, 10–15% require surgery. If aggressive conservative treatment for plantar fasciitis fails and surgery is indicated, the endoscopic approach is superior to conventional open procedures and significantly minimizes surgical trauma resulting in an earlier return to regular activities with fewer complications.

Dr. Hake is a member of the Ochsner Clinic Department of Orthopedics- Podiatry Section. He is Board Certified by the American Board of Podiatric Surgery and practices in Slidell, Louisiana
References
- Barrett S. L., Day S. V. Endoscopic plantar fasciotomy for chronic plantar fasciitis/heel spur syndrome: Surgical technique- early clinical results. J Foot Surg. 1991;30:568–570. [PubMed] [Google Scholar]
- Barrett S. L., Day S. V., Pignetti T. T. Endoscopic heel anatomy: Analysis of 200 fresh frozen specimens. J Foot Ankle Surg. 1995;34:51–56. doi: 10.1016/S1067-2516(09)80101-4. [DOI] [PubMed] [Google Scholar]
- Barrett S. L., Day S. V. Endoscopic plantar fasciotomy: Two portal endoscopic surgical techniques- Clinical results of 65 procedures. J Foot Ankle Surg. 1993;32:248–256. [PubMed] [Google Scholar]
- Kinley S., Frascone S., Calderone D. Endoscopic plantar fasciotomy versus traditional heel spur surgery: A prospective study. J Foot Ankle Surg. 1993;32:595–603. [PubMed] [Google Scholar]
- Visser H. J., Grebosky R. D., Stark T. G. The instep plantar fasciectomy/fasciotomy and endoscopic plantar fasciotomy for management of recalcitrant plantar fasciitis. Foot and Ankle Quarterly. 1994;7:77–83. [Google Scholar]
- Barrett S. L., Day S. V., Pignetti T. T. Endoscopic plantar fasciotomy: A multi-surgeon prospective analysis of 652 cases. J Foot Ankle Surg. 1995;34:400–406. doi: 10.1016/S1067-2516(09)80011-2. [DOI] [PubMed] [Google Scholar]
- Stone P. A., Davies J. L. Retrospective review of endoscopic plantar fasciotomy- 1992 through 1994. J Am Podiatr Med Assoc. 1996;86:414–420. doi: 10.7547/87507315-86-9-414. [DOI] [PubMed] [Google Scholar]
- Stone P. A., McClure L. P. Retrospective review of endoscopoic plantar fasciotomy- 1994 through 1997. J Am Podiatr Med Assoc. 1999;89:89–93. doi: 10.7547/87507315-89-2-89. [DOI] [PubMed] [Google Scholar]
- Brekke M. K., Green D. R. Retrospective analysis of minimal incision, endoscopic, and open procedures for heel spur syndrome. J Am Podiatr Med Assoc. 1998;88:64–72. doi: 10.7547/87507315-88-2-64. [DOI] [PubMed] [Google Scholar]


