Abstract
Background
The impact of patients’ perceptions of discrimination in health care on patient-provider interactions is unknown.
Objective
Examine association of past perceived discrimination with subsequent patient-provider communication.
Research Design
Observational cross-sectional study.
Subjects
African American (AA; N=100) and white (N=253) patients treated for osteoarthritis by orthopedic surgeons (N=63) in two Veterans Affairs facilities.
Measures
Patients were surveyed about past experiences with racism and classism in healthcare settings before a clinic visit. Visits were audio-recorded and coded for instrumental and affective communication content (biomedical exchange, psychosocial exchange, rapport-building, patient engagement/activation) and nonverbal affective tone. After the encounter, patients rated visit informativeness, provider warmth/respectfulness, and ease of communicating with the provider. Regression models stratified by patient race assessed the associations of racism and classism with communication outcomes.
Results
Perceived racism and classism were reported by more AA patients than by white patients (racism: 70% vs. 26%; classism: 73% vs. 53%). High levels of perceived racism among AA patients was associated with less positive nonverbal affect among patients (Beta=−0.41, 95% CI=−0.73, −0.09) and providers (Beta=−0.34, 95% CI=−0.66, −0.01) and with low patient ratings of provider warmth/respectfulness (OR=0.19, 95% CI=0.05,0.72) and ease of communication (OR =0.22, 95% CI=0.07,0.67). Any perceived racism among white patients was associated with less psychosocial communication (Beta=−4.18, 95% CI=−7.68, −0.68), and with low patient ratings of visit informativeness (OR=0.40, 95% CI=0.23,0.71) and ease of communication (OR=0.43, 95% CI=0.20,0.89). Perceived classism yielded similar results.
Conclusions
Perceptions of past racism and classism in healthcare settings may negatively impact the affective tone of subsequent patient-provider communication.
Perceived discrimination, defined as the perception of differential and negative treatment because of one’s membership in a particular demographic group,1 is associated with a host of negative mental and physical health outcomes.2–4 One mechanism by which perceived discrimination is hypothesized to affect health is by inhibiting patients’ engagement with the healthcare system.5 Perceived discrimination is associated with clear indicators of disengagement, including delays in obtaining medical care or prescriptions,5–10 less utilization of some preventive services,8, 11–13 less adherence to physician recommendations or treatments,6, 8, 14, 15 more missed medical appointments,14 and substituting alternative medicine for conventional care.16 What remains unknown is whether perceived discrimination also contributes to less positive encounters with the healthcare system prior to patients showing blatant signs of disengagement.
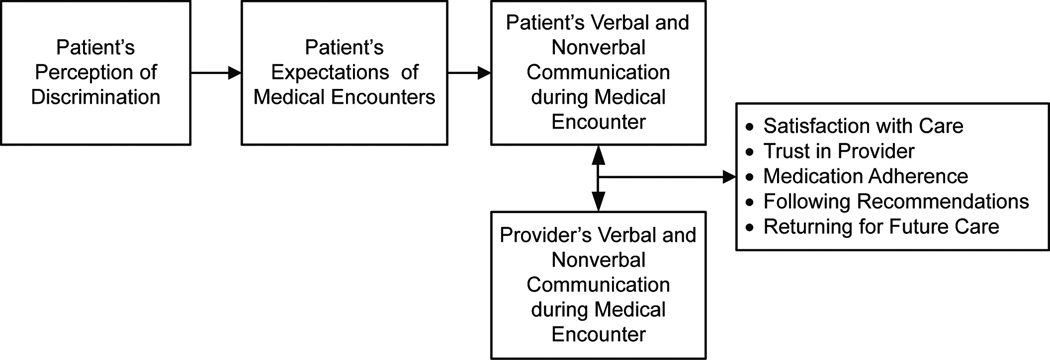
Figure 1 illustrates how perceived discrimination could lead to long-term patient disengagement by negatively affecting intermediate patient-provider interactions. Patients who perceived discrimination in past medical encounters may expect subsequent encounters to be less positive, which can affect their verbal and nonverbal communication during those encounters. Patient behavior can then both influence and be influenced by provider behavior,17, 18 and patient-provider communication can affect patients’ overall reactions to the encounter and subsequent engagement with that provider or the healthcare system.
Figure 1.
Theoretical Path from Perceived Discrimination to Patient Disengagement through Patient-Provider Communication
Evidence supports the link between patient-provider communication and outcomes such as patient satisfaction and adherence.19, 20 Patients who perceive discrimination also report less satisfaction with their care, but studies documenting this link have relied entirely on patient ratings of care.21–23 The effect of perceived discrimination on actual communication during medical encounters has not been empirically validated. The current study examined the relationship between patients’ perceptions of discrimination from past healthcare encounters and patient-provider communication during a subsequent medical visit in a sample of African American and white patients seeking treatment in orthopedic clinics for advanced osteoarthritis. We examined instrumental and affective aspects of communication, both of which are considered to be integral components of successful medical encounters.24–26 Instrumental communication includes verbal information exchange that serves to identify and solve a medical problem, whereas affective communication includes verbal statements that convey socio-emotional content (e.g., concern) and nonverbal aspects of communication that convey emotion (e.g., voice quality).25 We hypothesized that there would be less instrumental communication and less positive affective communication during visits with patients who perceived discrimination in past medical encounters.
Our primary focus was on perceived racial discrimination (i.e., perceived racism), given that studies have found that 8 to 42% of African Americans perceive that they have personally experienced racial discrimination while seeking health care,8, 27–29 and that negative associations between perceived racism and health-related outcomes have been documented among both whites and racial minorities.5, 6, 27 To assess whether the effects of perceived racism generalize to other types of discrimination, we also examined the effects of perceived discrimination attributed to one’s socioeconomic status (i.e., perceived classism).
Methods
Participants and Procedures
This analysis used data from a larger observational study of patient-provider communication and decision-making about joint replacement among patients with knee or hip osteoarthritis (n=526).30 Patients and surgeons were recruited from two orthopedic surgery clinics in Department of Veterans Affairs (VA) hospitals. IRBs at both hospitals approved the study and informed consent was obtained from all participants. Patients were eligible if they were aged 50 or older, had chronic knee or hip pain, had not been diagnosed with an inflammatory arthritis, and had no prior history of joint replacement. All attending orthopedic surgeons and residents who rotated through the clinic during the recruitment period (December 2005 to July 2008) were eligible. Almost all residents in the participating clinics are orthopedic residents in their second through sixth year of residency, with the rest being first-year general surgery residents.
Data were collected before, during, and after a patient’s scheduled clinic appointment. Immediately before their appointment, patients completed a researcher-administered survey of clinical and sociodemographic characteristics as well as patients’ perceptions of racism and classism previously experienced in healthcare settings. Patients’ appointments were then audio-recorded with the knowledge of patients and surgeons. After the appointment, patients’ impressions of the visit were assessed. Electronic medical records were reviewed to determine whether patients had been seen previously at that clinic, as follow-up visits tend to be shorter and patients’ familiarity with the clinic could affect communication patterns.
Of the 526 patients recruited in the parent study, those with complete audio recordings and perceived racism/classism data were included in this analysis (n = 353). Of the 173 patients excluded from this analysis, 60 had no audio recordings because their surgeons had not consented to be audio-taped, 66 had incomplete or unintelligible recordings, and 47 were missing perceived racism/classism data because they enrolled in the study before those measures had been added to the survey. Patients included in the analysis did not differ from excluded patients in age, gender, income, education, or whether they had a previous orthopedic visit, although most of the excluded patients (68%) were from a single study site.
Study Measures
Measures of Perceived Discrimination
We measured perceived discrimination in healthcare settings using adapted versions of Williams’ Everyday Discrimination measure31, 32 that assessed how often unfair treatment based on one’s race and socioeconomic status/class was encountered in healthcare settings.14, 33 The adapted scales have shown excellent reliability in a variety of diverse patient populations.14, 29, 33 Perceived racism and classism scores were created by dichotomizing items within each scale into never experienced vs. ever experienced and summing the number of items on which patients reported perceiving discrimination (Chronbach’s alphas = 0.93 and 0.90 for racism and classism scales, respectively).
Coder-Rated Measures of Patient-Provider Communication
Audio-recordings were coded using the Roter Interaction Analysis System (RIAS).34, 35 RIAS is a method of coding patient-provider communication in which patient and provider utterances are classified into biomedical/instrumental or socio-emotional/affective categories.34, 35 Four composites were derived from RIAS codes for analyses, including an instrumental composite of the number of statements related to biomedical exchange (i.e., information-giving, questions, education, and counseling pertaining to the medical condition or therapeutic regimen), and 3 socio-emotional/affective composites reflecting psychosocial exchange (i.e., information-giving, questions, education, and counseling pertaining to psychosocial issues or lifestyle), rapport building (i.e., social talk, laughter, compliments, and statements that reflect concern, reassurance, approval, agreement, empathy, legitimizing, and partnership), and patient activation/engagement (i.e., providers’ back-channeling, paraphrasing, and asking for the patient’s permission, opinion, reassurance, and understanding; patients’ paraphrasing, request for services, and asking for reassurance, understanding, and clarification from providers).36
Nonverbal affect displayed during the visit was also assessed by coders using rating scales from 1 (low/none) to 5 (high). Patient positive affect scores were created by averaging the ratings of patient interest/attentiveness, friendliness/warmth, responsiveness/engagement, sympathy/empathy, interactivity, and respectfulness (Cronbach’s alpha=0.90). Provider positive affect scores were created by averaging the same dimensions along with hurried/rushed (reverse-coded) (Cronbach’s alpha=0.92).
Two research staff members trained by a RIAS expert completed the coding. After achieving reliability with the RIAS expert and with each other on a subsample of recordings, the coders worked independently to code the remaining recordings. Inter-coder reliability was assessed for 20% of the recordings that were double-coded. Reliability was adequate across the biomedical exchange, psychosocial exchange, rapport building, and patient activation/engagement composites (Intra-class correlation=0.82, 0.68, 0.77, and 0.73, respectively).
Patient-Rated Measures of Patient-Provider Communication
Patient evaluations of visit informativeness, provider warmth/respectfulness, and ease of communicating with the provider were measured using the 3-factor Patient Reactions Assessment.37 Each factor was assessed by 5 items with responses ranging from very strongly disagree (1) to very strongly agree (7). Scale scores were created by summing responses across items (Cronbach’s alpha=0.86, 0.89, 0.88 for visit informativeness, provider warmth/respectfulness, and ease of communication, respectively).
Clinical and Socio-demographic Covariates
We measured several patient characteristics that could affect patients’ experiences with discrimination and/or communication. These included self-identified race (non-Hispanic African American or non-Hispanic white), age (years), gender, annual income (<$20,000, ≥$20,000, or missing), highest educational attainment (high school or less), whether patients had been seen in the orthopedic clinic previously, and quality of life (SF-12 physical and mental components).38
Statistical Analysis
Perceived racism and classism measures were compared for African American and white participants to determine whether it was appropriate to combine races into a single analysis. It was decided to stratify the analysis by race, as low rates of perceived discrimination in the white sample could mask or distort relationships with the outcomes for the African American sample. For African Americans, perceived racism and classism scores in the highest quartile (i.e., those who experienced all seven types of discriminatory treatment) were contrasted with all other cases. For whites, those who perceived any racism or classism (i.e., experienced at least 1 of the 7 examples of discriminatory treatment) were compared to the other cases. We explored alternative cut-points (e.g., use of full scale, tertiles, quartiles) and chose those that best reflected the structure of the data for each racial group. These analyses did not indicate a dose-response relationship between discrimination and communication outcomes.
RIAS-coded outcomes were analyzed as continuous measures. Patient-rated outcomes were heavily skewed and therefore categorized into 2 levels (satisfied vs. unsatisfied) for analyses, with scores in the lowest quartile being categorized as unsatisfied (25th percentile=27, 29, and 29 for visit informativeness, provider warmth, and ease of communication, respectively). Analyses using patient-rated outcomes as continuous variables yielded similar results; results using the dichotomized variables are presented.
We assessed associations of each perceived discrimination measure with communication outcomes in separate analyses using linear regression for continuous outcomes and logistic regression for dichotomized outcomes. All models were clustered by provider. We tested the associations between each perceived discrimination measure and communication outcomes in unadjusted models and in models adjusted for patient age, gender, income, education, previous visits to the orthopedic clinic, physical and mental quality of life, study site, and time of study enrollment (to account for possible trends over the enrollment period). Age, quality of life scores, and time of study enrollment were centered at the mean. The total number of utterances made during the visit was included in all models predicting RIAS count composites to adjust for variation in amount of communication across visits.
Results
Sample Characteristics
The sample included 353 patients (mean age=62 years) who were seen by 63 orthopedic surgeons, with each surgeon seeing a median of 5 patients (range=1–16). The patient sample was 95% male with 42% reporting an annual income <$20,000 and 75% having attained a high school education or less. Less than half (41%) the sample had been seen in the orthopedic clinic previously. The sample included 100 African Americans and 253 whites. African Americans were younger and reported lower incomes than whites (see Table 1).
Table 1.
Characteristics of total sample and of African American and White sub-samples
| Characteristics | Total Sample (N=353) |
African Americans (N=100) |
Whites (N=253) |
P* | |||
|---|---|---|---|---|---|---|---|
| Age (mean ± sd) | 62.2 | ± 8.6 | 60.0 | ± 7.9 | 63.1 | ± 8.8 | .002 |
| Male (n %) | 335 | 95 | 95 | 95 | 240 | 95 | .958 |
| Annual household income | |||||||
| <$20,000 | 148 | 42 | 54 | 54 | 94 | 37 | .004 |
| ≥$20,000 | 169 | 48 | 34 | 34 | 135 | 53 | |
| Missing | 36 | 10 | 12 | 12 | 24 | 10 | |
| High school education or less | 265 | 75 | 76 | 76 | 189 | 75 | .800 |
| Prior visit to this clinic (yes) | 146 | 41 | 48 | 48 | 98 | 39 | .111 |
| Quality of life (SF-12) | |||||||
| Physical component | 28.4 | ± 8.5 | 28.9 | ± 9.0 | 28.2 | ± 8.3 | .534 |
| Mental component | 48.3 | ± 13.3 | 46.3 | ± 13.2 | 49.1 | ± 13.3 | .078 |
| Site | |||||||
| Pittsburgh | 231 | 65 | 40 | 40 | 191 | 76 | <.001 |
| Cleveland | 123 | 35 | 60 | 60 | 62 | 25 | |
P-values compare African Americans and whites using t-tests for continuous measures and chi-square tests for categorical measures
Prevalence of Perceived Racism and Classism
The percentage of patients who perceived that they had experienced racism or classism in healthcare settings varied across the seven types of experiences assessed (see Table 2). For both African Americans and whites, the type of racism and classism perceived most often was feeling like a provider did not listen to them. The type of racism and classism perceived least often was having a provider act afraid of them. The distribution of perceived discrimination scores was quite different for African American and white patients. For perceived racism, African Americans displayed a bimodal pattern where 30% of the sample reported no perceived racism and 24% reported the maximum possible perceived racism, whereas 74% of whites reported no perceived racism. The perceived classism measure showed a similar bimodal distribution for African Americans, and nearly half of whites (47%) reported no perceived classism. Perceived racism and classism were highly correlated for African Americans and for whites (Spearman’s rho=0.92 and 0.62, respectively, p<.0001).
Table 2.
Percentage of African American (N = 100) and white patients (N = 253) who perceived racism and classism in healthcare settings
| Racism | Classism | |||
|---|---|---|---|---|
| African Americans |
Whites | African Americans |
Whites | |
| When getting healthcare, have you ever had any of the following things happen to you because of your race or color (for racism measure)/socioeconomic status or class (for classism measure)? | ||||
| Felt like a doctor or nurse was not listening to what you were saying | 58 | 18 | 62 | 40 |
| Treated with less respect than other people | 57 | 15 | 56 | 27 |
| Received poorer services than other people | 56 | 12 | 55 | 25 |
| Treated with less courtesy than other people | 55 | 11 | 56 | 28 |
| Had a doctor or nurse act as if he or she was better than you | 49 | 14 | 50 | 29 |
| Had a doctor or nurse act as if he or she thinks you were not smart | 48 | 11 | 52 | 27 |
| Had a doctor or nurse act as if he or she was afraid of you | 33 | 6 | 29 | 12 |
Impact of Perceived Racism on Patient-Provider Communication
Table 3 displays the association of perceived racism with each communication outcome. Results were similar across unadjusted and adjusted models and findings from the adjusted models are highlighted in the text. For African Americans, perceived racism was not associated with coder-ratings of verbal biomedical exchange, psychosocial exchange, rapport building, or patient activation/engagement. However, perceived racism was negatively associated with coder-ratings of nonverbal patient positive affect displayed during the visit, such that African American patients in the highest quartile of perceived racism displayed less positive affect (B=−0.41, 95% CI=−0.73, −0.09). Perceived racism also showed a significant negative association with nonverbal provider positive affect, such that surgeons who met with African American patients in the highest quartile of perceived racism displayed less positive affect (B=−0.34, 95% CI=−0.66, −0.01). Perceived racism was also negatively associated with African American patients’ ratings of provider warmth/respectfulness (OR=0.19, 95% CI=0.05, 0.72), as well as with ease of communication (OR=0.22, 95% CI=0.07, 0.67). Patients in the highest quartile of perceived racism were less likely to be satisfied with these domains. Perceived racism was not associated with African American patients’ ratings of visit informativeness.
Table 3.
Association of high (vs. low) perceived racism in past healthcare encounters with dimensions of patient-provider communication*
| African Americans | Whites | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted** | Unadjusted | Adjusted** | |||||||||
| Coder-rated outcomes | B | 95% CI | B | 95% CI | B | 95% CI | B | 95% CI | ||||
| Verbal Measures | ||||||||||||
| Biomedical exchange | 2.64 | −11.42, 16.71 | 6.67 | −9.58, 22.93 | 6.11 | −1.96, 14.17 | 3.12 | −5.88, 12.12 | ||||
| Psychosocial exchange | 1.74 | −4.10, 7.59 | 1.10 | −5.82, 8.02 | −4.66 | −7.60, −1.73 | −4.18 | −7.68, −0.68 | ||||
| Rapport building | −5.39 | −15.13, 4.35 | −6.81 | −17.73, 4.11 | −2.64 | −7.92, 2.65 | −1.65 | −7.56, 4.25 | ||||
| Patient activation/engagement | −3.20 | −9.58, 3.19 | −3.97 | −9.87, 1.94 | −0.34 | −3.05, 2.38 | 1.23 | −1.95, 4.42 | ||||
| Non-verbal Measures | ||||||||||||
| Positive patient affect | −0.36 | −0.68, −0.04 | −0.41 | −0.73, −0.09 | −0.16 | −0.35, 0.04 | −0.15 | −0.35, 0.06 | ||||
| Positive provider affect | −0.26 | −0.53, 0.01 | −0.34 | −0.66, −0.01 | 0.02 | −0.18, 0.22 | 0.09 | −0.11, 0.29 | ||||
| Patient-rated outcomes | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | ||||
| Informativeness of visit | 0.53 | 0.16, 1.72 | 0.60 | 0.15, 2.34 | 0.39 | 0.23, 0.67 | 0.40 | 0.23, 0.71 | ||||
| Provider warmth/respect | 0.23 | 0.08, 0.66 | 0.19 | 0.05, 0.72 | 0.38 | 0.21, 0.72 | 0.48 | 0.22, 1.07 | ||||
| Ease of communicating | 0.27 | 0.10, 0.77 | 0.22 | 0.07, 0.67 | 0.31 | 0.16, 0.57 | 0.43 | 0.20, 0.89 | ||||
Level of perceived racism was defined separately for African Americans and whites due to different distributions of discrimination reported by these subgroups. For African Americans, high perceived racism was defined as reporting 7 out of 7 possible experiences of race-based discrimination. For whites, high perceived racism was defined as reporting any (0) versus no (1–7) experiences of race-based discrimination. Analyses were stratified by race.
All models were clustered by provider. Total number of utterances was also included as a covariate in all models predicting biomedical exchange, psychosocial exchange, rapport building, and patient activation/engagement. Adjusted models also included the following covariates: patient gender, age, SF-12 physical and mental components, education, income, whether patients had a prior visit to the orthopedic clinic, study site, and time of study enrollment.
For whites, perceived racism was negatively associated with verbal psychosocial exchange (B=−4.18, 95% CI=−7.68, −0.68). Whites who perceived at least 1 instance of perceived racism in past healthcare encounters had approximately 4 fewer statements about psychosocial topics during their visits than did whites who perceived no past racism. Perceived racism was not associated with any other coder-rated verbal or nonverbal communication outcomes for whites. Perceived racism among whites was negatively associated with patient ratings of visit informativeness (OR=0.40, 95% CI=0.23, 0.71) and ease of communication (OR=0.43, 95% CI=0.20, 0.89).
Impact of Perceived Classism on Patient-Provider Communication
Results for perceived classism were similar to those for perceived racism (see Table 4). Among African Americans, perceived classism showed marginally significant negative associations with nonverbal positive affect displayed by patients (B=−0.35, 95% CI=−0.72, 0.02, p=.07) and providers (B=−0.29, 95% CI=−0.60, 0.03, p=0.07). Furthermore, perceived classism was negatively associated with African American patients’ ratings of provider warmth/respectfulness (OR=0.20, 95% CI=0.06, 0.66) and ease of communication (OR=0.24, 95% CI=0.08, 0.70), but not visit informativeness. Among whites, perceived classism was not associated with any coder-rated communication outcomes, but was negatively associated with patient ratings of visit informativeness (OR=0.51, 95% CI=0.29, 0.89) and ease of communication (OR = 0.47, 95% CI= 0.22, 1.00, p=.05).
Table 4.
Association of high (vs. low) perceived classism in past healthcare encounters with dimensions of patient-provider communication*
| African Americans | Whites | |||||||
|---|---|---|---|---|---|---|---|---|
| Unadjusted | Adjusted** | Unadjusted | Adjusted** | |||||
| Coder-rated outcomes | B | 95% CI | B | 95% CI | B | 95% CI | B | 95% CI |
| Verbal Measures | ||||||||
| Biomedical exchange | 2.69 | −12.43, 17.81 | 6.64 | −9.27, 22.54 | .004 | −9.27, 9.28 | −4.74 | −13.75, 4.26 |
| Psychosocial exchange | 5.10 | −2.55, 12.74 | 4.26 | −4.08, 12.60 | −0.48 | −3.08, 2.13 | −0.08 | −2.39, 2.24 |
| Rapport building | −6.28 | −16.69, 4.13 | −7.68 | −17.43, 2.08 | 0.06 | −5.51, 5.63 | 2.57 | −3.77, 8.91 |
| Patient activation/engagement | −4.22 | −10.63, 2.19 | −4.75 | −10.30, 0.81 | −1.70 | −4.81, 1.42 | −0.91 | −4.24, 2.42 |
| Non-verbal Measures | ||||||||
| Positive patient affect | −0.33 | −0.67, 0.01 | −0.35 | −0.72, 0.02 | −0.09 | −0.27, 0.09 | −0.08 | −0.27, 0.12 |
| Positive provider affect | −0.24 | −0.51, 0.03 | −0.29 | −0.60, 0.03 | −0.02 | −0.16, 0.12 | 0.03 | −0.16, 0.21 |
| Patient-rated outcomes | OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Informativeness of visit | 0.51 | 0.17, 1.51 | 0.46 | 0.14, 1.54 | 0.45 | 0.27, 0.77 | 0.51 | 0.29, 0.89 |
| Provider warmth/respect | 0.27 | 0.10, 0.72 | 0.20 | 0.06, 0.66 | 0.47 | 0.28, 0.79 | 0.64 | 0.33, 1.20 |
| Ease of communicating | 0.32 | 0.13, 0.82 | 0.24 | 0.08, 0.70 | 0.35 | 0.18, 0.67 | 0.47 | 0.22, 1.00 |
Level of perceived classism was defined separately for African Americans and whites due to different distributions of discrimination reported by these subgroups. For African Americans, high perceived classism was defined as reporting 7 out of 7 possible experiences of class-based discrimination. For whites, high perceived classism was defined as reporting any (0) versus no (1–7) experiences of class-based discrimination. Analyses were stratified by race.
All models were clustered by provider. Total number of utterances was also included as a covariate in all models predicting biomedical exchange, psychosocial exchange, rapport building, and patient activation/engagement. Adjusted models also included the following covariates: patient gender, age, SF-12 physical and mental components, education, income, whether patients had a prior visit to the orthopedic clinic, study site, and time of study enrollment.
Discussion
To our knowledge this is the first study to demonstrate that patient perceptions of racism and classism previously encountered in healthcare settings are associated with patient-provider communication in future medical encounters. Our results suggest that African American patients’ experiences with discrimination in healthcare settings are negatively associated with nonverbal affective aspects of subsequent interactions with providers, rather than with verbal instrumental or verbal affective communication, and that these effects are strong enough to be detected by independent coders and by patients themselves. In contrast, we found that perceptions of past racism and classism in healthcare settings among white patients had little impact on coder ratings of verbal or nonverbal communication, but were associated with patient ratings of visit informativeness and ease of communicating with the provider.
Although we expected past discrimination to have a negative impact on all aspects of communication, the effects were primarily observed for nonverbal affective behavior. This may be because the residual effects of discrimination occur outside of our awareness and therefore get communicated in subtle ways rather than through conscious verbal behavior. This is consistent with research showing that unconscious biases often get communicated through nonverbal, unintentional channels.39–41
Our work suggests possible ways to reduce the impact of perceived discrimination on patient-provider communication during medical encounters. First, the most common types of racism and classism reported by patients were feeling that a provider was not listening to them and being treated with less respect than others. This highlights the need for better training of healthcare providers on listening to patients and on communicating to patients that their concerns and preferences are being considered. Second, providers should be educated about the potential impact of patients’ past discriminatory experiences on their current interactions so providers can better understand what may underlie patients’ interactive styles. This could be done in conjunction with strategies to reduce the impact of unintentional biases of providers on healthcare provision, such as raising providers’ self-awareness of unintentional biases and providing more opportunities to interact with patients of diverse backgrounds (e.g., via standardized patients).42 Third, our findings suggest the need to promote positive affective tone during the medical encounter. This could be accomplished by means such as educating providers about how their tone often mirrors that of their patients, which can lead to a downward spiral of negative communication. Affective tone may also be improved by training providers to be aware of negative emotional states (e.g., stress) and how to respond in a positive manner through role-playing, use of imagery, or mindfulness training.42
Several limitations should be noted. Our sample was relatively homogeneous and included older, predominantly male, African American and white patients from orthopedic clinics in VA medical facilities that were located in urban, mid-western, predominantly white cities. Our findings may not generalize to other patient populations or clinical settings. Our sub-sample of African American patients was also rather small, which may have limited our statistical power.
Another limitation is that we did not have access to provider characteristics for use as covariates. It would have been interesting to examine whether provider gender or level of training (e.g., resident vs. attending) affected communication in our sample, as other studies have reported differences in communication based on these provider characteristics.34, 43 The lack of provider race/ethnicity is particularly unfortunate, as the effects of perceived racism on communication may depend on whether or not patients are communicating with a provider of their own race. However, patient-provider racial concordance should not be an issue when considering the effects of perceived classism on communication, and the effects of perceived racism and classism were very similar in this study.
Our measures of perceived discrimination were not distributed in a way that allowed us to make direct comparisons across African American and white patients. We used reliable, multi-item measures of perceived discrimination that have been shown to be more sensitive than single-item measures often used in studies of discrimination in healthcare settings29. Even so, we found low rates of discrimination among whites, and conclusions about whether the effects of discrimination on patient-provider communication depend on patient race should be drawn with caution. The low rates of discrimination among white patients make it difficult to draw firm conclusions about the effects of discrimination, racism in particular, on communication outcomes for that group. Our results may have been different if our sample had come from a more diverse region where white patients are not the racial majority and have more interactions with medical staff of different racial and ethnic backgrounds.
Administering the perceived discrimination measures prior to the observed visit is also a potential limitation, as patients who were able to recall instances of discrimination may have been in a less positive frame of mind when they began their visit. Although this is possible, we felt it was important to measure past discrimination before the visit in which communication outcomes were being assessed so we could be sure we were measuring past discrimination and not discrimination that occurred during the observed visit. To do our best to minimize negative priming effects, the discrimination measures were embedded in a longer survey and most patients had at least 20 minutes between completing that survey and starting their orthopedic consultation.
Finally, in Figure 1 we proposed that patient expectations about future medical encounters mediate the effects of perceived discrimination on patient-provider communication, but expectations were not measured in this study. Prior work has shown that not all patients who have experienced discrimination are concerned about encountering it in future medical visits.44 More work is therefore needed to determine the conditions under which discrimination shapes expectations, and the extent to which expectations shape communicative behavior.
This study had two important strengths. First, it examined a rich set of communication outcomes that were based on coder assessments of audio-recorded visits and patient ratings of visits. Previous studies that have found negative associations between perceived discrimination and perceived quality of care have relied solely on patient ratings of care.21, 22 Second, by assessing both perceived racism and classism, this study demonstrated that the effects of perceived discrimination on patient-provider communication are not restricted to discrimination based on race. This is consistent with evidence that experiencing unfair treatment in general has negative health effects, regardless of whether it is because of one’s race, class, or other characteristics.45, 46
This study illustrates the pervasive effects of perceived discrimination by demonstrating its negative association with nonverbal affective components of patient-provider communication for African American patients. This work suggests that instances of perceived discrimination in healthcare settings could have a long-term impact on patients’ interactions with the healthcare system by fostering less positive medical encounters in the future. Training programs should be developed to raise provider awareness about the effects of discrimination on patient-provider interactions and to enhance provider communication skills that facilitate more positive affect during medical encounters.
Acknowledgements
This study was supported by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development Service (IIR 04-137, PI: Said A. Ibrahim). Dr. Hausmann's effort was supported by the Veterans Affairs Health Services Research and Development Career Development Program (RCD 06-287 and ER 0280-1). Dr. Ibrahim was also supported by a K24 Award (1K24AR055259-01) from the National Institutes of Musculoskeletal and Skin Disorders. The views expressed here are those of the authors and do not represent those of the Department of Veterans Affairs or the United States Government.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smedley BD, Stith AY, Nelson AR, editors. Unequal treatment: Confronting racial and ethnic disparities in health care. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Paradies Y. A systematic review of empirical research on self-reported racism and health. Int J Epidemiol. 2006 Aug;35(4):888–901. doi: 10.1093/ije/dyl056. [DOI] [PubMed] [Google Scholar]
- 3.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009 Feb;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pascoe EA, Smart Richman L. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009 Jul;135(4):531–554. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burgess DJ, Ding Y, Hargreaves M, van Ryn M, Phelan S. The association between perceived discrimination and underutilization of needed medical and mental health care in a multi-ethnic community sample. J Health Care Poor Underserved. 2008 Aug;19(3):894–911. doi: 10.1353/hpu.0.0063. [DOI] [PubMed] [Google Scholar]
- 6.Casagrande SS, Gary TL, Laveist TA, Gaskin DJ, Cooper LA. Perceived discrimination and adherence to medical care in a racially integrated community. J Gen Intern Med. 2007 Mar;22(3):389–395. doi: 10.1007/s11606-006-0057-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wamala S, Merlo J, Bostrom G, Hogstedt C. Perceived discrimination, socioeconomic disadvantage and refraining from seeking medical treatment in Sweden. J Epidemiol Community Health. 2007 May;61(5):409–415. doi: 10.1136/jech.2006.049999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Fam Pract. 2004 Sep;53(9):721–730. [PubMed] [Google Scholar]
- 9.Van Houtven CH, Voils CI, Oddone EZ, et al. Perceived discrimination and reported delay of pharmacy prescriptions and medical tests. J Gen Intern Med. 2005;20:578–583. doi: 10.1111/j.1525-1497.2005.0123.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lee C, Ayers SL, Kronenfeld JJ. The association between perceived provider discrimination, healthcare utilization and health status in racial and ethnic minorities. Ethn Dis. 2009 Summer;19(3):330–337. [PMC free article] [PubMed] [Google Scholar]
- 11.Trivedi AN, Ayanian JZ. Perceived discrimination and use of preventive health services. J Gen Intern Med. 2006 Jun;21(6):553–558. doi: 10.1111/j.1525-1497.2006.00413.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan AM, Gee GC, Griffith D. The effects of perceived discrimination on diabetes management. J Health Care Poor Underserved. 2008 Feb;19(1):149–163. doi: 10.1353/hpu.2008.0005. [DOI] [PubMed] [Google Scholar]
- 13.Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and use of preventive health services. J Gen Intern Med. 2008 Oct;23(10):1679–1684. doi: 10.1007/s11606-008-0730-x. PMCID: PMC2533365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bird ST, Bogart LM, Delahanty DL. Health-related correlates of perceived discrimination in HIV care. AIDS Patient Care and STDs. 2004;18(1):19–26. doi: 10.1089/108729104322740884. [DOI] [PubMed] [Google Scholar]
- 15.Brener L, von Hippel W, von Hippel C, Resnick I, Treloar C. Perceptions of discriminatory treatment by staff as predictors of drug treatment completion: utility of a mixed methods approach. Drug Alcohol Rev. 2010 Sep;29(5):491–497. doi: 10.1111/j.1465-3362.2010.00173.x. [DOI] [PubMed] [Google Scholar]
- 16.Bazargan M, Norris K, Bazargan-Hejazi S, et al. Alternative healthcare use in the under-served population. Ethn Dis. 2005 Autumn;15(4):531–539. [PubMed] [Google Scholar]
- 17.Ashton CM, Haidet P, Paterniti DA, et al. Racial and ethnic disparities in the use of health services. J Gen Intern Med. 2003;18:146–152. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Street RL, Jr, Gordon H, Haidet P. Physicians' communication and perceptions of patients: Is it how they look, how they talk, or is it just the doctor? Soc Sci Med. 2007;65:586–598. doi: 10.1016/j.socscimed.2007.03.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ong LM, de Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995 Apr;40(7):903–918. doi: 10.1016/0277-9536(94)00155-m. [DOI] [PubMed] [Google Scholar]
- 20.Beck RS, Daughtridge R, Sloane PD. Physician-patient communication in the primary care office: a systematic review. J Am Board Fam Pract. 2002 Jan–Feb;15(1):25–38. [PubMed] [Google Scholar]
- 21.Sorkin DH, Ngo-Metzger Q, De Alba I. Racial/ethnic discrimination in health care: impact on perceived quality of care. J Gen Intern Med. 2010 May;25(5):390–396. doi: 10.1007/s11606-010-1257-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perez D, Sribney WM, Rodriguez MA. Perceived discrimination and self-reported quality of care among Latinos in the United States. J Gen Intern Med. 2009 Nov;24 Suppl 3:548–554. doi: 10.1007/s11606-009-1097-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.LaVeist TA, Nickerson KJ, Bowie JV. Attitudes about racism, medical mistrust, and satisfaction with care among African American and White cardiac patients. Med Care Res Rev. 2000;57 Suppl 1:146–161. doi: 10.1177/1077558700057001S07. [DOI] [PubMed] [Google Scholar]
- 24.Bensing JM, Dronkers J. Instrumental and affective aspects of physician behavior. Med Care. 1992 Apr;30(4):283–298. doi: 10.1097/00005650-199204000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Hall JA, Roter DL, Katz NR. Task versus socioemotional behaviors in physicians. Medical Care. 1987;25(5):399–411. doi: 10.1097/00005650-198705000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Ben-Sira Z. Affective and instrumental components in the physician-patient relationship: an additional dimension of interaction theory. J Health Soc Behav. 1980 Jun;21(2):170–180. [PubMed] [Google Scholar]
- 27.Hausmann LR, Jeong K, Bost JE, Ibrahim SA. Perceived discrimination in health care and health status in a racially diverse sample. Med Care. 2008 Sep;46(9):905–914. doi: 10.1097/MLR.0b013e3181792562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Blendon RJ, Buhr T, Cassidy EF, et al. Disparities in health: perspectives of a multi-ethnic, multi-racial America. Health Aff (Millwood) 2007 Sep–Oct;26(5):1437–1447. doi: 10.1377/hlthaff.26.5.1437. [DOI] [PubMed] [Google Scholar]
- 29.Hausmann LRM, Kressin NR, Hanusa BH, Ibrahim SA. Perceived racial discrimination in health care and its association with patients’ healthcare experiences: Does the measure matter? Ethn Dis. 2010 Winter;20:40–47. [PubMed] [Google Scholar]
- 30.Hausmann LR, Mor M, Hanusa BH, et al. The effect of patient race on total joint replacement recommendations and utilization in the orthopedic setting. J Gen Intern Med. 2010;25(9):982–988. doi: 10.1007/s11606-010-1399-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 32.Taylor TR, Kamarck TW, Shiffman S. Validation of the Detroit Area Study Discrimination Scale in a community sample of older African American adults: the Pittsburgh healthy heart project. Int J Behav Med. 2004;11(2):88–94. doi: 10.1207/s15327558ijbm1102_4. [DOI] [PubMed] [Google Scholar]
- 33.Bird ST, Bogart LM. Perceived race-based and socioeconomic status (SES)-based discrimination in interactions with health care providers. Ethn Dis. 2001 Autumn;11(3):554–563. [PubMed] [Google Scholar]
- 34.Roter DL, Larson S. The relationship between residents' and attending physicians' communication during primary care visits: An illustrative use of the roter interaction analysis system. Health Communication. 2001;13(1):33–48. doi: 10.1207/S15327027HC1301_04. [DOI] [PubMed] [Google Scholar]
- 35.Roter DL, Larson S. The roter interaction analysis system (RIAS): Utility and flexibility for analysis of medical interactions. Patient Education and Counseling. 2002;46:243–251. doi: 10.1016/s0738-3991(02)00012-5. [DOI] [PubMed] [Google Scholar]
- 36.Cene CW, Roter D, Carson KA, Miller ER, 3rd, Cooper LA. The effect of patient race and blood pressure control on patient-physician communication. J Gen Intern Med. 2009 Jul 3;24(9):1057–1064. doi: 10.1007/s11606-009-1051-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Galassi JP, Ware WB, Schanberg R. The patient reactions assessment: A brief measure of the quality of patient-provider medical relationship. Psychological Assessment. 1992;4(3):346–351. [Google Scholar]
- 38.Ware J, Jr, Kosinski M, Keller SD. A 12-Item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Dovidio JF. Psychology. Racial bias, unspoken but heard. Science. 2009 Dec 18;326(5960):1641–1642. doi: 10.1126/science.1184231. [DOI] [PubMed] [Google Scholar]
- 40.Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol. 2002 Jan;82(1):62–68. doi: 10.1037//0022-3514.82.1.62. [DOI] [PubMed] [Google Scholar]
- 41.Dovidio JF, Kawakami K, Johnson C, Johnson B, Howard A. On the nature of prejudice: Automatic and controlled processes. Journal of Experimental Social Psychology. 1997;33:510–540. [Google Scholar]
- 42.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007 Jun;22(6):882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Roter DL, Hall JA, Aoki Y. Physician gender effects in medical communication: a meta-analytic review. JAMA. 2002 Aug 14;288(6):756–764. doi: 10.1001/jama.288.6.756. [DOI] [PubMed] [Google Scholar]
- 44.Malat J, Hamilton MA. Preference for same-race health care providers and perceptions of interpersonal discrimination in health care. J Health Soc Behav. 2006 Jun;47(2):173–187. doi: 10.1177/002214650604700206. [DOI] [PubMed] [Google Scholar]
- 45.Williams DR, Gonzalez HM, Williams S, Mohammed SA, Moomal H, Stein DJ. Perceived discrimination, race and health in South Africa. Soc Sci Med. 2008 Aug;67(3):441–452. doi: 10.1016/j.socscimed.2008.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Troxel WM, Matthews KA, Bromberger JT, Sutton-Tyrrell K. Chronic stress burden, discrimination, and subclinical carotid artery disease in African American and Caucasian women. Health Psychol. 2003 May;22(3):300–309. doi: 10.1037/0278-6133.22.3.300. [DOI] [PubMed] [Google Scholar]