Abstract
Background
Evidence indicates Alcoholics Anonymous (AA) can play a valuable role in recovery from alcohol use disorder. While AA itself purports it aids recovery through “spiritual” practices and beliefs, this claim remains contentious and has been only rarely formally investigated. Using a lagged, mediational analysis, with a large clinical sample of adults with alcohol use disorder, this study examined the relationships among AA, spirituality/religiousness, and alcohol use, and tested whether the observed relation between AA and better alcohol outcomes can be explained by spiritual changes.
Method
Adults (N = 1,726) participating in a randomized controlled trial of psychosocial treatments for alcohol use disorder (Project MATCH) were assessed at treatment intake, and 3, 6, 9, 12, and 15 months on their AA attendance, spiritual/religious practices, and alcohol use outcomes using validated measures. General linear modeling (GLM) and controlled lagged mediational analyses were utilized to test for mediational effects.
Results
Controlling for a variety of confounding variables, attending AA was associated with increases in spiritual practices, especially for those initially low on this measure at treatment intake. Results revealed AA was also consistently associated with better subsequent alcohol outcomes, which was partially mediated by increases in spirituality. This mediational effect was demonstrated across both outpatient and aftercare samples and both alcohol outcomes (proportion of abstinent days; drinks per drinking day).
Conclusions
Findings suggest that AA leads to better alcohol use outcomes, in part, by enhancing individuals’ spiritual practices and provides support for AA’s own emphasis on increasing spiritual practices to facilitate recovery from alcohol use disorder.
Keywords: Alcoholics Anonymous, Spirituality, self help groups, alcoholism, alcohol dependence
1. Introduction
“Three years ago when my head doctor, Silkworth, began to tell me of the idea of helping drunks by spirituality, I thought it was crackpot stuff, but I’ve changed my mind. One day this bunch of ex-drunks of yours is going to fill Madison Square Garden…” (AA, 1952, p. 136).
The kind of skepticism initially expressed by this hospital administrator in 1937 (Hartigan, 1998) still persists today. Discourse surrounding Alcoholics Anonymous (AA) and its spiritual emphasis can be contentious (Bufe, 1991; Ferr et al., 2006; Peele, 1990; Trimpey and Ellis, 1995; Vaillant, 1983). However, as predicted by this individual at a time when the organization numbered less than one hundred members, AA has grown exponentially into a fellowship with more than 1.2 million members meeting in more than 55,000 groups across the United States, and with at least one million additional members in 114 countries around the world (Alcoholics Anonymous [AA], 2001; Mäkela, 1996). Furthermore, increasingly rigorous research conducted in the past 15 years supports the notion that AA participation is associated with better short and long-term outcomes and may be a cost-effective treatment adjunct (Emrick et al., 1993; Humphreys, 2004; Humphreys and Moos, 2001, 2007; Kelly and Yeterian, 2008; Tonigan et al., 2003). How AA achieves this relative efficacy and efficiency is a topic of only recent inquiry.
AA and related 12-step mutual-help organizations, such as Narcotics Anonymous (NA), possess an explicitly spiritual or quasi-religious orientation. They encourage reliance on a personally-defined God or “Higher Power” and encourage the use of prayer and meditation (AA, 1952,AA, 2001). In fact, the main purported mechanism of recovery from “alcoholism” is identified as a “spiritual awakening” (AA, 1939,AA, 2001) or “spiritual experience” (AA, 2001, Appendix II) brought about by completion of the 12-step program. An emerging empirical literature examines the mechanisms through which AA participation may lead to better alcohol use outcomes and recovery. To date, studies suggest that AA works through increased self-efficacy, coping, and motivation for abstinence (Kelly et al., 2009; Morgenstern et al., 2002), by facilitating changes in social networks (Bond et al., 2003; Connors et al., 2001, Humphreys and Woods, 1993; Kaskutas et al, 2002; Kelly et al., 2009; Longabaugh et al., 1998), by reducing depression, but not anger, symptoms (Kelly et al., 2010a, 2010b) and by engagement in AA-related helping (Pagano et al., 2004, 2009). Surprisingly little research has been conducted in the area of spirituality, despite its place as the central mechanism of recovery in the AA literature (AA, 1939,AA, 2001).
Recent research examining the role of spirituality/religiousness (S/R) in recovery, in general, has produced mixed results. Kaskutas and colleagues (2003) found that while initial spiritual orientation did not predict outcome 3-years following SUD treatment, those who reported a recent “spiritual awakening” had a four-fold increased odds of abstinence. In contrast, an analysis of a large clinical alcohol dependent sample, showed that a high spirituality score at baseline predicted better alcohol use outcomes at one-year follow-up (Connors et al., 2001). Similar to Kaskutas and colleagues (2003) above, an outpatient study examined changes between treatment intake and a 6-month follow-up across ten measures of S/R in relation to a dichotomized measure of heavy drinking in the past 90 days at 6 months. The study found that measures of spiritual practices and experiences increased over the follow-up, but spiritual and religious beliefs did not. These increases were associated with less heavy drinking at the 6-month follow-up (Robinson et al., 2007).
Regarding the specific influence of AA on S/R, AA participation has been associated with increased spirituality, which in turn partially mediated the relationship between AA and drinking outcomes 12 months after treatment (Zemore, 2007). This study used a partially lagged design, but nevertheless suggests a spiritual pathway through which AA and other 12-step groups may operate. A study also employing a partially, lagged, design, found that greater AA participation in the first 6 months following treatment was associated with greater 6-month spirituality, but spirituality did not predict alcohol outcome at 3-year follow-up (Tonigan et al., 2003). Differences in causal model (i.e., spirituality as a predictor vs. a mediator), measurement, or time-frame (i.e., 1 vs. 3 years) may account for these discrepant findings, but suggest a proximal effect of S/R on alcohol outcomes.
Recent research has also examined S/R as a moderator of AA’s effects. For example, studies have investigated whether those who are less S/R inclined will be less likely benefit from AA. Findings revealed that atheists and agnostics are less likely to seek recovery assistance through AA, but those who do, appear to benefit equally compared to more religious/spiritual individuals (Kelly et al., 2006; Tonigan et al., 2002; Winzelberg and Humphreys, 1999). Similarly, a study of mutual-help group participants from five different organizations, including AA, found the degree of initial S/R beliefs was unrelated to staying sober (Atkins and Hawdon, 2007). This suggests that for some, certain affiliation factors (e.g., greater perceived addiction severity) may outweigh other barriers, such as opposition to spiritual involvement. These individuals may subsequently change and adopt new S/R beliefs, or benefit through other means (Kelly et al., 2009).
Spirituality has been examined among mutual-help participants with co-occurring substance use and mental health disorders (i.e., in Double Trouble in Recovery). Spirituality was found to mediate pro-health behaviors but not substance use outcomes in this study (Magura et al., 2003). Research has examining spirituality in differing mutual aid organizations as well and suggests AA members have more spiritual beliefs compared to members of a more cognitive behaviorally-oriented organization, SMART Recovery (see Ellis and Velten, 1992; Li et al., 2000).
In summary, S/R variables have been of great interest within the treatment and recovery field and more recently have become a central focus (e.g., Galanter and Kaskutas, 2008). However, despite the central importance of S/R within the AA program, it has seldom been investigated as a mechanism of behavior change. Studies that have been conducted have varied considerably in methodology and scope, and causal inferences have been limited by a lack of temporal sequencing where measurement of the independent variable is followed by the mediator, which is followed by the dependent variable (i.e., fully lagged; Nock, 2007; Kazdin and Nock, 2003). In the present study, we employ a large, clinical, sample, of individuals with alcohol use disorder, and use a prospective, mediational design, controlling for a number of confounding variables. In addition, we test whether the potential influence of AA on subsequent S/R practices depends on the initial level of S/R at treatment entry. We hypothesize that AA attendance will be associated with positive alcohol use outcomes as well as enhanced S/R. We also predict that AA will increase S/R more for those initially low on this variable at treatment intake. In turn, we predict that greater S/R will also be associated with positive alcohol outcomes, and that the effect of AA on subsequent alcohol use, will be partially mediated by enhanced S/R.
2. Methods
2.1 Subjects
This study conducts analyses of the Project MATCH outpatient (n = 952; 72% male) and aftercare (n = 774; 80% male) participants followed through 15 months. Inclusion/exclusion criteria. Inclusion criteria study were: current DSM-III-R diagnosis of alcohol abuse or dependence alcohol as the principal drug of abuse; actively drinking during the 3 months prior to entrance into the study; minimum age of 18; and minimum sixth grade reading level. Exclusion criteria were: a DSM-III-R diagnosis of current dependence on sedative/hypnotic drugs, stimulants, cocaine or opiates; any intravenous drug use in the prior 6 months; currently a danger to self or others; on probation/parole requirements that might interfere with protocol participation; lack of clear prospect for residential stability; inability to identify at least one “locator” person to assist in tracking for follow-up assessment; psychosis or organic impairment; or involvement (current or planned) in alternative treatment for alcohol-related problems other than that provided by Project MATCH (defined as more than 6 hours of non-study treatment, except f or self-help groups such as AlcoholicsA nonymous [AA], during the 3 months of study treatment). Outpatient participants were significantly younger, more residentially stable, and less dependent on alcohol than those in aftercare (Timko et al., 1993). In addition, a smaller proportion of outpatients (45%) than aftercare patients (62%) reported prior alcohol use disorder treatment. Patients in both arms (95% outpatient, 98% aftercare) primarily met criteria for alcohol dependence (SCID for DSM-III-R; Spitzer and Williams, 1985). See Table 1 for additional sample characteristics.
Table 1.
Demographic characteristics by study arm
| Aftercare | Outpatient | |
|---|---|---|
| n = 764 | n = 942 | |
| Age | 41.9(11.1) | 38.8(10.7) |
| Years Education | 13.1(2.0) | 13.4(2.1) |
| Gender | ||
| Female | 20.3% | 27.3% |
| Ethnicity | ||
| White | 80.5% | 79.8% |
| Hispanic | 14.8% | 5.6% |
| Black | 3.5% | 12.3% |
| Other | 1.2% | 2.2% |
| Married/Non-Married | ||
| Married/Cohabiting | 33.8% | 35.7% |
| Employment | ||
| Full-time | 47.5% | 51.06% |
2.2 Procedures
Subjects were randomly assigned to one of three individually-delivered, psychosocial interventions: Cognitive Behavioral Therapy (CBT; Kadden et al., 1992), Motivational Enhancement Therapy (MET; Miller et al., 1992), and Twelve-Step Facilitation Therapy (TSF; Nowinski et al., 1995). TSF and CBT were delivered in 12 weekly sessions; MET sessions were delivered only at weeks 1, 2, 6 and 12. Participants were reassessed at 3, 6, 9, 12 and 15 months following treatment, and follow-up rates remained over 90%. More complete details can be found elsewhere (e.g., Project MATCH Research Group, 1997). Our focus in this secondary data analysis centers on 3, 9, and 15 month follow-up assessments since only these time points contained the necessary variables needed for our lagged model.
2.3 Measures
2.3.1 Alcohol use
Alcohol consumption was assessed using the Form 90 (Miller and Del Boca, 1994), which combines an interview procedure with calendar-based and drinking pattern estimation methods. The Form 90 also collects data on drug use, treatment, incarceration, and AA attendance in the past 90 days.
2.3.2 Alcoholics Anonymous attendance
AA attendance was assessed using the Form 90, which captured the number of AA meetings attended during the past 90 days at intake and 3, 6, 9, 12, and 15 months. The proportion days attending AA was created by dividing the number of days attended by the total number of days in the assessment period.
2.3.3 Spirituality/Religiousness measure
Spirituality/religiousness was assessed with the Religious Background and Behavior instrument (RBB; Connors et al., 1996). It is a 13-item multidimensional scale (alpha = .86) that measures self-reported religious status on a 5-point scale (“I do not believe in God”, [Atheist] coded “0”, “I believe we can’t really know about God” [Agnostic] coded “1”, through “Unsure”, coded “2”, “I believe in God, but I’m not religious [Spiritual] coded “3”, “I believe in God and practice religion [religious], coded “4”); and lifetime, and past year, engagement in religious practices. Because in the current study we are examining change in S/R over time, questions pertaining to “lifetime” S/R practices were excluded from our total RBB score, producing a 7-item scale that, in addition to the self-reported S/R status mentioned above, asked 6 additional questions: “For the past 90 days how often have you done the following?: 1. Thought about God, 2. Prayed, 3. Meditated, 4. Attended worship services, 5. Read or studied scriptures/holy writings, 6. Had direct experiences of God”. These items were coded on an 8-point Likert-scaled index ranging from Never (coded “0”) to More than Once a Day (coded “7”). Thus, the total possible score for the RBB in this study was 0–46. The RBB was administered at intake and the 3, 9, and 15 month follow-ups.
2.4 Statistical methods
2.4.1 Data preparation and descriptive analyses
The dependent variables (percent days abstinent [PDA], drinks per drinking day [DDD]) and the independent AA attendance variable were transformed prior to analyses (PDA/arcsine transformed; DDD/square root transformed, and AA attendance/log transformed; Tabachnick and Fidell, 2001). We ran the models with and without log transformation of AA attendance and no differences were found. For easier interpretation, we report descriptive statistics using the untransformed variables.
2.4.2 Lagged, controlled mediation analyses
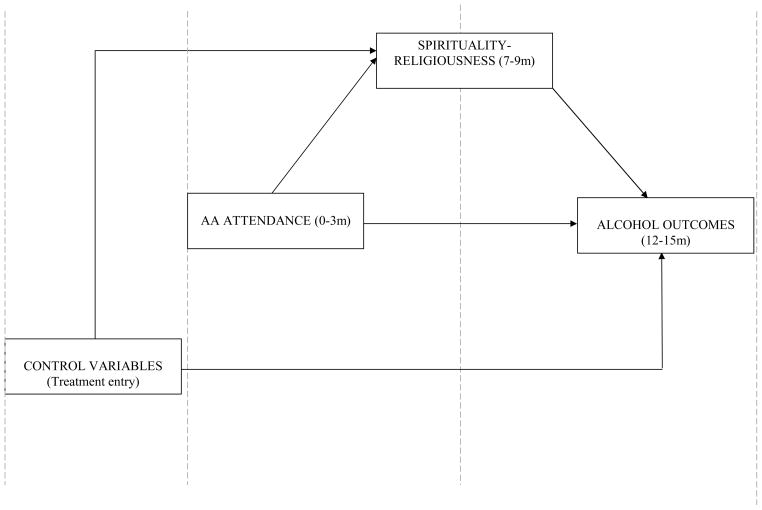
To examine the relationship between AA attendance, spirituality, and alcohol use, we used a prospectively lagged, modeling approach. We ran these models separately for the aftercare and outpatient samples and for each alcohol use outcome variable (PDA, DDD) to examine: (1) the independent (AA attendance) to dependent variable path, (2) the independent to mediator (S/R) path, and (3) the mediator to dependent variable path (Baron and Kenny, 1986) To make the tests prospective (lagged), we used AA attendance in the past 90 days at month 3 follow-up to predict S/R practices (practiced during the past 3 months) at month 9, and drinking outcomes (PDA and DDD) at months 1315. Similarly, we used S/R practices during the past 90 days at month 9 to predict the drinking outcomes during months 13–15. Figure 1 shows this lagged model with pre-treatment control variablesBased on univariate analyses and theory the included covariates were age, ethnicity, gender, marital status, employment status, number of prior alcohol-related treatments, treatment site, treatment assignment, and the relevant baseline level of the dependent variable (S/R, PDA, DDD). We also included an interaction term to test whether the potential influence of AA attendance on subsequent S/R depended on the level of reported spirituality at treatment entry..
Figure 1.
Lagged Mediational Model
2.4.3 Missing data
To address missing data, we used multiple imputation (Little and Rubin, 2002). Missing data for key variables ranged from 0.05% for baseline AA attendance to 7.8% for drinking data at months 13–15. Since missing data patterns were non-monotone (i.e., many data were intermittently missing), the Markov Chain Monte Carlo (MCMC) method for multiple imputation was used (Gilks et al., 1996). We performed ten imputations using MI and MIANALYZE in SAS 9.1.3, and reported statistics are averaged across imputations. The degrees of freedom for the reported t-statistics vary by analysis due to adjustment (Barnard and Rubin, 1999).
2.4.4 Tests of statistical mediation
Mediation analyses were conducted using methods described by MacKinnon and colleagues (MacKinnon and Dwyer, 1993; MacKinnon et al., 2002). The method tests directly for the existence of a significant path from the independent variable (A) through the mediator (B) to the outcome (C) by computing a product of the standardized regression coefficients for the A-B and B-C associations. The Z score can then be compared to critical significance levels developed by MacKinnon. This joint significance test has been shown to produce optimal power and the most accurate Type I error rates in all cases compared to other methods, including the Sobell t-test of the mediated effect (see MacKinnon et al., 2002).
3. Results
3.1 Sample descriptive data
Demographic data by study arm are shown in Table 1. Table 2 provides descriptive data on the primary variables for analyses. As noted previously (Tonigan et al., 2003), the rates of AA attendance were high across study treatments and consistently higher among aftercare compared to outpatient participants. However, there were substantial numbers from both patient groups that declined in rate of attendance over the first year following treatment. The total S/R score as measured by the RBB was slightly higher at treatment intake among the aftercare than the outpatient sample, rose significantly during treatment and stayed at this slightly higher level throughout follow-up.
Table 2.
AA attendance, spirituality-religiousness, and alcohol use outcomes by study arm*
| Aftercare | Outpatient | |||||||
|---|---|---|---|---|---|---|---|---|
| n = 774 | n = 952 | |||||||
| 0m | 3m | 9m | 15m | 0m | 3m | 9m | 15m | |
| Any AA | 62.9% | 83.8% | 55.6% | 54.2% | 37.1% | 44.9% | 30.0% | 30.9% |
| AA M (SD) | 23.3(42.2) | 32.5(32.3) | 18.9(27.3) | 17.4(26.2) | 9.8(33.4) | 11.0(20.2) | 7.8(18.9) | 7.7(18.5) |
| S/R M (SD) | 25.4(9.2) | 28.0(10.3) | 27.4(10.0) | 27.3(10.2) | 22.8(8.8) | 24.3(9.9) | 24.4(10.1) | 24.6(10.2) |
| PDA M (SD) | 26.9(29.6) | 90.1(21.3) | 80.9(29.9) | 79.6(31.9) | 34.3(29.8) | 79.8(27.4) | 73.9(31.2) | 72.7(33.5) |
| DDD M (SD) | 20.5(12.1) | 3.7(6.3) | 5.3(7.9) | 4.9(7.7) | 13.5(8.0) | 5.8(6.5) | 5.2(5.5) | 5.0(5.6) |
A significant time effect was observed for all variables (p<.001).
3.2 Relation between AA, spirituality/religiousness, and alcohol use over time
3.2.1 AA and alcohol use outcomes
Table 3 shows the relationship between AA and subsequent (lagged) alcohol use outcomes (PDA; DDD) in the outpatient and aftercare samples. As anticipated, there were robust associations between more frequent AA attendance and less frequent, and less intense, subsequent alcohol use over time, and in both study arms. Regarding significant covariates, among aftercare patients, a younger age (b = − .0141, p < .01; β= .12) and greater number of prior treatment episodes (b = .1714, p < .0005; β= −.10) was associated with higher DDD. There were no significant covariates among outpatient participants.
Table 3.
GLM results for AA attendance at 0–3m predicting transformed PDA and DDD for the Outpatient and Aftercare samples at 12–15ma
| Variable | b (se) | β | t (df) | p |
|---|---|---|---|---|
| Outpatient Sample | ||||
| baseline PDA | .0046(.0008) | 0.30 | 9.31(425) | <.0001 |
| AA attendance | .0047(.0005) | 0.21 | 5.76(341) | <.0001 |
| Aftercare Sample | ||||
| baseline PDA | .0028(.0006) | 0.18 | 5.01(466) | <.0001 |
| AA attendance | .0035(.0005) | 0.24 | 6.48(400) | <.0001 |
| Outpatient Sample | ||||
| baseline DDD | .0282(.0061) | 0.16 | 4.63(454) | <.0001 |
| AA attendance | −.0119(.0026) | −0.18 | −4.58(261) | <.0001 |
| Aftercare Sample | ||||
| baseline DDD | .0236(.0051) | 0.17 | 4.67(446) | <.0001 |
| AA attendance | −.0125(.0019) | −0.25 | −6.61419) | <.0001 |
Control and other variables included in models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, motivation, treatment site, treatment assignment..
3.2.2 AA and spirituality/religiousness
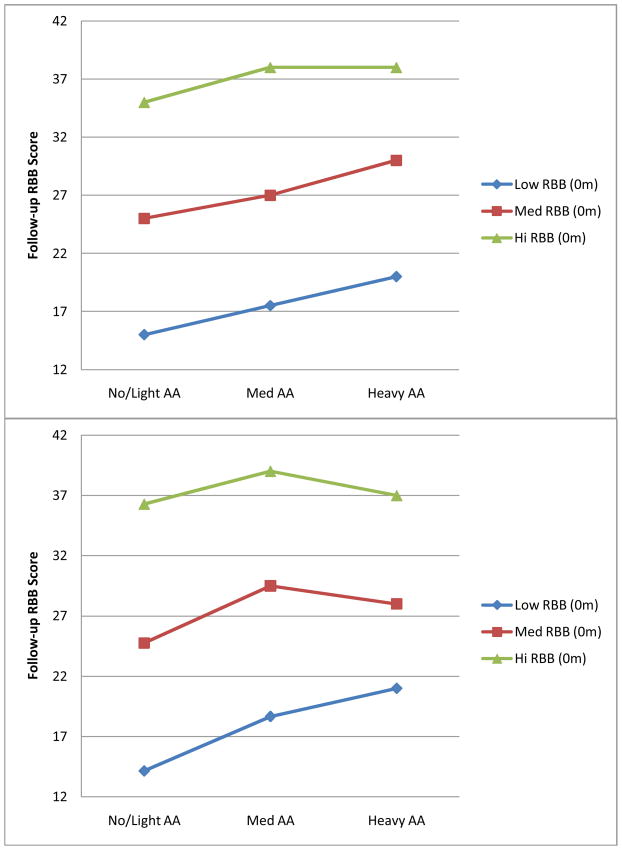
Table 4 shows the relationships between AA attendance and S/R. Among aftercare and outpatient participants, greater AA attendance was associated with increased S/R scores over time. This relationship was of similar magnitude across study arms. Minority patients had significantly higher S/R than White patients, but only among outpatients (b = 1.140, p < .005; β= .08). In addition, Figure 2 shows a significant AA x S/R interaction such that AA attendance was most strongly associated with increases in S/R among those with lower S/R scores at baseline; this interaction was present in both aftercare (b = −.0029, p = .0175; β −.08) and outpatient arms (b = −.0023, p = .0115; β −.06).
Table 4.
GLM results for AA attendance 0–3m predicting spirituality/religiousness 7–9m for the Outpatient and Aftercare samplesa
| Variable | b (se) | β | t (df) | p |
|---|---|---|---|---|
| Outpatient Sample | ||||
| baseline S/R | .8246(.0425) | 0.72 | 19.40(245) | <.0001 |
| AA attendance | .0659(.0111) | 0.14 | 5.94(420) | <.0001 |
| AA attendance X S/R | −.0029(.0012) | −0.06 | −2.41(130) | .0175 |
| Aftercare Sample | ||||
| baseline S/R | .7775(.0509) | 0.71 | 15.28(197) | <.0001 |
| AA attendance | .0721(.0087) | 0.23 | 8.26(250) | <.0001 |
| AA attendance X S/R | −.0023(.0009) | −0.08 | −2.54(253) | .0115 |
Control and other variables included in these tested models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, motivation, treatment site, treatment assignment.
Figure 2.
Ordinal Interaction showing that AA attendance increases spirituality more at follow-up for those with lower initial spirituality at baseline for both aftercare (top) and outpatient (bottom) samples
3.2.3 Spirituality/religiousness and alcohol use outcomes
Table 5 shows the relationship between S/R and subsequent PDA and DDD among aftercare and outpatient participants. As shown, S/R was positively associated with PDA and negatively associated with DDD among both aftercare and outpatient participants. Finally, among covariates only greater prior treatment episodes (b = .1398, p < .005; β = .12) was associated with higher DDD among aftercare patients.
Table 5.
GLM results for spirituality/religiousness at 7–9m predicting PDA and DDD at 13–15m for the Outpatient and Aftercare samplesa
| Variable | b (se) | β | t (df) | p |
|---|---|---|---|---|
| Outpatient Sample | ||||
| baseline S/R | −.0049(.0028) | −0.09 | −1.76(286) | .0801 |
| baseline PDA | .0048(.0005) | 0.30 | 9.39(434) | <.0001 |
| S/R | .0099(.0024) | 0.21 | 4.05(288) | <.0001 |
| Aftercare Sample | ||||
| baseline S/R | −.0058(.0028) | −0.11 | −2.12(279) | .0353 |
| baseline PDA | .0028(.0006) | 0.18 | 5.01(435) | <.0001 |
| S/R | .0134(.0026) | 0.29 | 5.17(131) | <.0001 |
| Outpatient Sample | ||||
| baseline S/R | .0096(.0089) | 0.06 | 1.07(186) | .2866 |
| baseline DDD | .0269(.0061) | 0.15 | 4.42(473) | <.0001 |
| S/R | −.0243(.0079) | −0.17 | −3.08(206) | .0024 |
| Aftercare Sample | ||||
| baseline S/R | .0251(.0097) | 0.14 | 2.60(285) | .0098 |
| baseline DDD | .0238(.0005) | 0.18 | 4.67(458) | <.0001 |
| S/R | −.0411(.0091) | −0.25 | −4.53(145) | <.0001 |
Control and other variables included in these tested models but not shown above include age, gender, ethnicity, marital status, employment status, number of prior alcohol treatments, motivation, treatment site, treatment assignment.
3.2.4 Lagged mediation analyses: Spirituality as a mediator of AA’s effect on drinking
All predicted paths in the lagged models in both study arms were statistically significant. Consequently, the final tests were those examining mediation, which, as mentioned above, were conducted using methods outlined by MacKinnon et al. (2002). Results indicated that for aftercare patients, 28% of the direct effect of AA on frequency of alcohol consumption (PDA) was explained by S/R (Mack Z = 4.38, p < .01), and 24% of the direct effect of AA on intensity of alcohol consumption (DDD) was explained by S/R (DDD; Mack Z = −3.97, p < .01). Similarly, among outpatients, 14% of the direct effect of AA on frequency of alcohol consumption (PDA) was explained by S/R (Mack Z = 3.35, p < .01) and 13% of the direct effect of AA on intensity of drinking (DDD) was explained by S/R (Mack Z = −3.31, p < .01).
4. Discussion
Using a prospective lagged controlled mediational analysis this study found that AA attendance was associated with increases in S/R over and above a number of confounding control variables, such as age and ethnicity. S/R was also found to increase more among those who initially were low on this variable. Furthermore, a consistent effect of AA attendance on subsequent drinking outcomes was observed, which was partially explained by AA’s effect on increasing S/R. These effects were significant and stable across time for both aftercare and outpatient samples and on both drinking outcomes. Results from this study, using a large multi-site clinical sample, exhibiting a broad range of alcohol-related involvement and impairment, support the central idea espoused by AA that spirituality is important in recovery, and that AA appears to mobilize spiritual changes, which help explain AA’s beneficial effects on recovery from alcohol dependence.
4.1 Spirituality/religiousness as a mechanism of AA-related change
Defining and operationalizing spirituality has been challenging(Connors et al., 2008; Johnson and Robinson, 2008). Viewed from a psychological perspective our results raise further questions as to how exactly spiritual practices may aid recovery from alcohol use disorder. One possibility is that since these spiritual practices appear to be mobilized within the specific alcohol recovery context of AA, their prescribed regular use outside of AA meetings (e.g., using the Serenity Prayer; AA, 1975, pg 18) may serve to activate an associated global “recovery schema” that in turn mobilizes additional motivation and behavioral coping. From a stress and coping perspective (Lazarus and Folkman, 1984), spiritual practices and beliefs may help AA members to attribute different meaning to stressful events or life experiences (e.g., “I have come to believe that hard times are not just meaningless suffering and that something good might turn up at any moment. That’s a big change for someone who used to come to in the morning feeling sentenced to another day of life.” AA, 2001, p. 374; “…pain is the touchstone of all spiritual progress.” AA, 1953, p. 93). Similar processes have been implicated among those coping with other psychological and physical illnesses (Carrico et al., 2006; Frazier et al., 1995). Emphases on recovery-specific S/R practices in AA also may lead to heightened cognitive vigilance that protects against lapses to drinking (e.g., altruism/reaching out to others with the same problem; mindfulness meditation; Zemore and Kaskutas, 2008; Zemore and Pagano, 2008). It may help some achieve a sense of belonging with others suffering from the same condition that satisfies an affiliative need and desire for secure attachment often evoked by fear-induced stress (e.g., Baker, 1979). Some have described spirituality as a complex entity comprised of a spectrum of positive emotions such as joy, compassion, love, and forgiveness similar to how white light is split into its constituent colors when striking a glass prism (Vaillant, 2008). Because AA encourages members to find their own conception of a “Higher Power”, whatever form that may take (AA, 1953), AA may help reduce oppositional barriers to trying out spiritual practices and beliefs which, in turn, may give rise to rewards in psychological well-being that reinforce ongoing recovery-related changes (e.g., Kelly et al., 2010; Pearce et al., 2008).
The S/R orientation of AA is additionally conscious and intentional. AA states firmly that its program is one of persistent action (e.g., “The spiritual life is not a theory we have to live it”; “Faith without works is dead” AA, 2001, p. 76). Pargament and colleagues (1988, 2004) discuss three types of S/R coping styles that an individual may adopt when faced with problems: (1) a “Self-Directing” coping style is when an individual is very active and God is completely passive; (2) in a “Deferring” style, an individual takes no active steps, but passively awaits for God to intervene; and the “Collaborative” coping style is when an individual and God both take active roles in a partnership to solve a problem. The collaborative style has been associated with more effective coping with chronic illnesses (Dunn and Horgas, 2004). Given the proactive emphasis of AA, this may be the style most associated with its program. Further research using detailed measurement methods may elucidate how spiritual beliefs and behaviors aid recovery, coping, and psychological well-being among AA members (Pardini et al., 2000).
Despite our finding that spiritual practices mediated the effect of AA attendance on later alcohol use, this was only a partial mediation effect. Clearly, there are multiple theoretical mechanisms across multiple levels of scale (e.g., psychological, social, neurobiological) that could explain AA-related benefit, some of which have been tested formally (see Kelly et al, 2009). These mechanisms are also likely to exert dynamic reciprocal influences. Nevertheless, future work should attempt to conduct analyses that investigate the dynamic nature of mediators as well as how multiple mediators complement and/or compete with one another in order to identify the relative influence of broad therapeutic mechanisms (see Kazdin and Nock, 2003; Nock, 2007; Pardini et al, 2000). . The present work is a central step toward this end, providing sound support for S/R as a partial mediator of AA-related behavior change.
4.2 The conditions under which spirituality/religiousness may serve as a mechanism of AA-related change
AA may confer its greatest benefit through spiritual means among those reporting low S/R beliefs and behaviors initially. This study found an interaction between the baseline S/R level and AA’s effect on later measures of the same construct. AA increased S/R more for those initially low at intake. For those initially high on this variable, AA did not produce such large increases, which could reflect a ceiling effect of the mechanism or measure. For those patients showing increases in S/R as a function of AA attendance, this could be indicative of AA’s notion of a “spiritual awakening”. Specifically, as alluded to in the study by Robinson and colleagues (2007), one pathway to recovery may be through a marked shift in consciousness or existential meaning (AA, 2001). Half of the initial membership of AA was comprised of atheists or agnostics, but these individuals found recovery through AA (AA, 2001), and prior research has found that although atheists and agnostic individuals may be less likely to attend groups like AA, those that do, achieve a similar benefit (Kelly et al, 2006; Winzelberg and Humphreys, 1999). The present findings support this notion that, despite minimal spiritual beliefs, AA may facilitate increases in S/R which can, in turn, aid recovery from alcohol addiction.
It is unclear the extent to which S/R may mediate the effects of AA attendance in other countries as strongly as it has done in this U.S. sample. It is estimated that approximately 85% of Americans report being “religious” and 70% state that “there is definitely a personal God” (Kosmin and Keysar, 2009). AA originated and grew up in this overtly religious socio-historical context, but other English speaking countries where AA is also popular, report lower rates of religiousness and spiritual beliefs. In more secular societies, such as the UK where preliminary research has shown that AA produces similar beneficial effects (e.g., Gossop et al., 2005), it is possible that AA may operate more strongly through other mechanisms, such as social network changes and related increases in coping and self-efficacy. However, such speculative cross-cultural variation in the relative importance of AA’s mechanisms awaits validation.
4.2 Spirituality/religiousness in the broader context of addiction recovery
AA remains popular and appears helpful to many different types of individuals seeking recovery from alcohol use disorder (Humphreys, 2004; Kelly and Yeterian, 2008; National Survey on Drug Use and Health, 2009). Other fellowships too, such as Narcotics Anonymous and Cocaine Anonymous, are based on this same spiritual template. One reason why these spiritually-oriented recovery programs have grown so much during the past 75 years may relate to the disinhibiting effects of substance use on behavior. Specifically, effects from chronic, heavy, alcohol use often generate increasingly regrettable deviations from an individual’s personal values. Repeated over and over this “Jekyll and Hyde” scenario can lead to a sense of profound moral failing and self-loathing. Such negative feelings may be intensified and deepened further by the reproach of affected onlookers and significant others. For many, the sense of “redemption”, historically and implicitly embedded within AA philosophy (AA, 1939; Oxford Group, 1933) may provide a compassionate framework for self-forgiveness.
We have noted previously (Kelly et al., 2009, 2010a, 2010b) that while explicitly spiritual, AA is a multi-faceted social organization, that mobilizes common process changes in the social network of its members, helps reduce depression and enhances well-being, and mobilizes intra-individual cognitive and behavioral changes in coping, motivation, and self-efficacy. These putative mechanisms help explain at least some of AA’s benefits and suggest that AA facilitates recovery-related change through multiple mechanisms. However, the magnitude of mediational effects found here were comparatively large (i.e., 24–28% for aftercare and 13–14% for outpatients) in relation to that found previously for other mechanisms (e.g., Kelly et al., 2010), suggesting that AA’s mobilization of S/R beliefs and behaviors may be important. However, the larger magnitude mediational effects for the more severely alcohol-involved aftercare patients suggest that AA may confer its benefits more strongly through some mechanisms than others for some patients. In fact, mediators may be moderated by a number of factors, such as this. As has been shown in psychotherapy research more generally (e.g., Bohart and Tollman, 1999), individuals may adopt and utilize certain aspects of AA that work well in their own particular case. Yet, we do not believe that S/R as a mechanism of behavior change in recovery from alcohol dependence should be taken out of context. Spiritual beliefs and behaviors by themselves may be less likely to initiate and sustain recovery from alcohol dependence without other, more abstinence-specific, coping skills and support offered by other members of AA (Zemore, 2007).
4.4 Limitations
This study has some limitations, which should be considered. The sample consists of mostly Caucasian men, recruited to participate in a randomized controlled trial and it is unknown to what extent these mediational findings extend to other samples or groups, particularly non-treatment-seeking populations. Also, although we found that our measure of S/R behaviors was sensitive to change and was a successful mediator of AA attendance, consensus on the contents and conceptual boundaries of the construct of “spirituality” and how to best measure them remain a challenge for the field (Galanter, 2007; Pardini et al., 2000). The specific nature of what is meant by “spirituality” and how increases in such behaviors as prayer and meditation, for example, may influence other recovery-related changes should be clarified in future research. Only a single mediator was examined in this study. It will be necessary in future research to test potential mediators against each other to help determine the relative magnitude of mediating effects. It may also be that S/R is a proxy for intensive AA involvement, with members reporting higher S/R practices and beliefs because they have been indoctrinated into the 12-step model. Also related to measurement is the reliance on self-report that could be susceptible to demand characteristics resulting in over- or under-reporting. Finally, although our measure of AA attendance was predictive of S/R and alcohol use outcomes, there is some evidence to suggest that more detailed measures of AA involvement may yield different results. Unfortunately, missing data on the AA involvement measure prevented such analyses in the current study. This should be pursued in future research.
4.4 Conclusions
Spiritual concepts and practices continue to play a role in common conceptualizations and treatments for addictions. From some perspectives, this persistence in the current age of neuroscience can seem archaic and odd. However, this apparent incongruity may be merely superficial. Recovery-related change operates through multiple mechanisms and at multiple levels of scale. Thus, participation in groups like AA is not only likely to produce changes in spirituality, and coping, abstinence self-efficacy, motivation, negative affect, and social networks, but also change at the neurobiological level (Kelly et al., 2009). At a behavioral level, this study suggests that AA leads to better alcohol use outcomes, in part, by enhancing individuals’ spiritual practices. For those viewing these findings from a purely spiritual or metaphysical frame of reference, further explanation of the results may not be necessary. Viewed through a psychological lens these results raise further questions as to how exactly spiritual practices may aid recovery from alcohol use disorder. Whether it is because these practices, learned within the specific alcohol recovery context of AA, serve as cues that activate a global recovery schema, help individuals attribute more adaptive meanings to stressors, or something else, remains to be clarified. Whatever the exact downstream mechanism of this mediator turns out to be, findings herein provide empirical support for AA’s own emphasis on increasing spiritual practices to facilitate recovery from alcohol use disorder.
Acknowledgments
This research was supported by a grant from the US National Institute on Alcohol Abuse and Alcoholism (R21 AA016762; Mechanisms and Moderators of Behavior Change in Alcoholics Anonymous).
Contributor Information
John F. Kelly, Center for Addiction Medicine, Department of Psychiatry, Massachusetts General Hospital and Harvard Medical School, 60 Staniford St., Suite 120, Boston, MA 02114
Robert L. Stout, Decision Sciences Institute/PIRE, 1005 Main St., Pawtucket, RI 02860-7802
Molly Magill, Brown University, Center for Alcohol and Addiction Studies, Providence RI 02912
J. Scott Tonigan, Center on Alcoholism, Substance Abuse and Addiction (CASAA), 2650 Yale SE., Suite 243, Albuquerque, NM 87106
Maria E. Pagano, Case Western Reserve University School of Medicine, Department of Psychiatry, Division of Child Psychiatry, W.O. Walker Center, 10524 Euclid Avenue
References
- Alcoholics Anonymous. Alcoholics Anonymous: The story of how thousands of men and women have recovered from alcoholism. 3. Alcoholics Anonymous World Services; New York: 1939. [Google Scholar]
- Alcoholics Anonymous. Twelve steps and twelve traditions. Alcoholics Anonymous World Services; New York: 1952. [Google Scholar]
- Alcoholics Anonymous. Twelve Steps and twelve traditions. Alcoholics Anonymous World Services; New York: 1953. [Google Scholar]
- Alcoholics Anonymous. Alcoholics Anonymous: The story of how thousands of men and women have recovered from alcoholism. 4. Alcoholics Anonymous World Services; New York: 2001. [Google Scholar]
- Atkins RG, Hawdon JE. Religiousness and participation in mutual-aid support groups for addiction. J Subst Abuse Treat. 2007;33:321–331. doi: 10.1016/j.jsat.2007.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker CR. Defining and measuring Affiliation Motivation. J Soc Psychol. 1979;9:97–99. [Google Scholar]
- Barnard J, Rubin DB. Miscellanea. Small-sample degrees of freedom with multiple imputation. Biometrika. 1999;86:948–955. [Google Scholar]
- Bergin AE, Jensen JE. Religiousness of psychotherapists: A national survey. Psychotherapy. 1990;27:3–7. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Personal Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Bond J, Kaskutas LA, Weisner C. The persistent influence of social networks and Alcoholics Anonymous on abstinence. J Stud Alcohol. 2003;64:579–588. doi: 10.15288/jsa.2003.64.579. [DOI] [PubMed] [Google Scholar]
- Bufe C, Ellis A. Alcoholics Anonymous: Cult or Cure? See Sharp Press; Tuscon: 1991. [Google Scholar]
- Carrico AW, Antoni MH, Durán RE, Ironson G, Penedo F, Fletcher MA, et al. Reductions in depressed mood and denial coping during cognitive behavioral stress management with HIV-positive gay men treated with HAART. Ann Behav Med. 2006;31:155–164. doi: 10.1207/s15324796abm3102_7. [DOI] [PubMed] [Google Scholar]
- Connors GJ, Tonigan JS, Miller WR. The Religious Background and Behavior Psychometric and normed findings. Psychol Addict Behav. 1996;1:90–96. [Google Scholar]
- Connors GJ, Tonigan JS, Miller WR. Religiousness and Responsiveness to Alcoholism Treatments. Department of Health and Human Services; Bethesda, MD: 2001. [Google Scholar]
- Connors GJ, Walitzer KS, Tonigan JS. Spiritual change in recovery, in Recent Developments in Alcoholism. In: Galanter M, Kaskutas LA, editors. Research on alcoholics anonymous and spirituality in addiction recovery. Vol. 18. Springer; New Jersey: 2008. pp. 209–228. [DOI] [PubMed] [Google Scholar]
- Dunn KS, Horgas AL. Religious and nonreligious coping in older adults experiencing chronic pain. Pain Manag Nurs. 2004;5:19–28. doi: 10.1016/s1524-9042(03)00070-5. [DOI] [PubMed] [Google Scholar]
- Ellis A, Velten E. When AA doesn’t work for you: Rational steps to quitting alcohol. Barricade Books; New York: 1992. [Google Scholar]
- Emrick CD, Tonigan JS, Montgomery H, Little L. Alcoholics Anonymous: What is currently known? In: McCrady BS, Miller WR, editors. Research on Alcoholics Anonymous: Opportunities and Alternatives. Rutgers Center of Alcohol Studies; Piscataway, NJ: 1993. pp. 41–76. [Google Scholar]
- Ferri M, Amato L, Davoli M. Alcoholics Anonymous and other 12-step programmes for alcohol dependence. Cochrane Database of Systematic Reviews 2006. 2006;(3) doi: 10.1002/14651858.CD005032.pub2. Art. No.: CD005032. [DOI] [PubMed] [Google Scholar]
- Frazier PA, Krasnoff AS, Port CL. The role of religion in coping with chronic medical conditions. Paper presented at the 103rd Annual Conference of the American Psychological Association; New York, NY. 1995. [Google Scholar]
- Galanter M. Spirituality and recovery in 12-step programs: An empirical model. J Subst Abuse Treat. 2007;33:265–272. doi: 10.1016/j.jsat.2007.04.016. [DOI] [PubMed] [Google Scholar]
- Galanter M, Kaskutas LA, editors. Research on alcoholics anonymous and spirituality in addiction recovery. Vol. 18. Springer; New Jersey: 2008. Recent developments in alcoholism. [Google Scholar]
- Gilks WR, Richardson S, Spiegelhalter DJ, editors. Markov Chain Monte Carlo in practice. Chapman and Hall; London: 1996. [Google Scholar]
- Goldman A. Portrait of Religion in U.S. Holds Dozens of Surprises. The New York Times; 1991. Apr 10, p. A1. [Google Scholar]
- Gossop M, Trakada K, Stewart D, Witton J. Reductions in criminal convictions after addiction treatment: 5-year follow-up. Drug Alcohol Depend. 2005;79:295–302. doi: 10.1016/j.drugalcdep.2005.01.023. [DOI] [PubMed] [Google Scholar]
- Hartigan F. Bill W: A biography of Alcoholics Anonymous cofounder Bill Wilson. Routledge; London: 1998. [Google Scholar]
- Humphreys K. Circles of recovery: Self-help organizations for addictions. Cambridge University Press; Cambridge, UK: 2004. [Google Scholar]
- Humphreys K, Moos RH. Can encouraging substance abuse patients to participate in self-help groups reduce demand for health care? A quasi-experimental study. Alcohol Clin Exp Res. 2001;25:711–716. [PubMed] [Google Scholar]
- Humphreys K, Moos RH. Encouraging post-treatment self-help group involvement to reduce demand for continuing care services: Two-year clinical and utilization outcomes. Alcohol Clin Exp Res. 2007;31:64–68. doi: 10.1111/j.1530-0277.2006.00273.x. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Woods MD. Researching mutual help group participation in a segregated society. J Appl Behav Sci. 1993;29:181–201. [Google Scholar]
- Johnson T, Robinson E. Issues in measuring spirituality and religiousness in alcohol research, in Recent Developments in Alcoholism. In: Galanter M, Kaskutas LA, editors. Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. 18. Vol. 18. Springer; New Jersey: 2008. pp. 167–186. [DOI] [PubMed] [Google Scholar]
- Kadden RM, Carroll K, Donovan D, Cooney N, Monti P, Abrams D, et al., editors. DHHS Publication No. (ADM) 92-1895. Vol. 4. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. Cognitive-Behavioral Coping Skills Therapy Manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence, in Project MATCH Monograph Series. [Google Scholar]
- Kaskutas LA, Bond J, Humphreys K. Social networks as mediators of the effect of Alcoholics Anonymous. Addiction. 2002;97:891–900. doi: 10.1046/j.1360-0443.2002.00118.x. [DOI] [PubMed] [Google Scholar]
- Kaskutas LA. Alcoholics Anonymous Effectiveness: Faith Meets Science. J Addict Dis. 2009;28:145–157. doi: 10.1080/10550880902772464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaskutas LA, Turk N, Bond J, Weisner C. The role of religion, spirituality and Alcoholics Anonymous in sustained sobriety. Alcohol Treat Q. 2003;21:1–16. [Google Scholar]
- Kazdin AE, Nock MK. Delineating mechanisms of change in child and adolescent therapy: Methodological issues and research recommendations. J Child Psychol Psychiatry. 2003;44:1116–1129. doi: 10.1111/1469-7610.00195. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Magill M, Stout RL. How do people recover from alcohol dependence? A systematic review of the research on mechanisms of behavior change in Alcoholics Anonymous. Addict Res Theory. 2009;17:236–259. [Google Scholar]
- Kelly JF, Stout R, Magill M, Tonigan JS, Pagano M. Mechanisms of behavior change in Alcoholics Anonymous: Does AA improve alcohol outcomes by reducing depression symptoms? Addiction. 2010a;105:626–636. doi: 10.1111/j.1360-0443.2009.02820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout R, Tonigan JS, Magill M, Pagano M. Negative affect, relapse, and Alcoholics Anonymous: Does AA work by reducing anger? J Stud Alcohol Drugs. 2010b;71:434–444. doi: 10.15288/jsad.2010.71.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Stout R, Zywiak W, Schneider R. A 3-year study of addiction mutual-help group participation following intensive outpatient treatment. Alcohol Clin Exp Res. 2006;30:1381–1392. doi: 10.1111/j.1530-0277.2006.00165.x. [DOI] [PubMed] [Google Scholar]
- Kelly JF, Yeterian JD. Mutual-help groups. In: O’Donohue W, Cunningham JR, editors. Evidence-Based Adjunctive Treatments. Elsevier; New York: 2008. pp. 61–105. [Google Scholar]
- Kosmin BA, Keysar A. American Religious Identification Survey (ARIS) Trinity Colleg; Hartford Connecticut: 2009. [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer; New York: 1984. [Google Scholar]
- Li EC, Feifer C, Strohm M. A pilot study: Locus of control and spiritual beliefs in Alcoholics Anonymous and SMART Recovery members. Addict Behav. 2000;25:633–640. doi: 10.1016/s0306-4603(99)00052-0. [DOI] [PubMed] [Google Scholar]
- Little RA, Rubin DB. Statistical Analysis with Missing Data. 2. John Wiley; New York: 2002. [Google Scholar]
- Longabaugh R, Wirtz PW, Zweben A, Stout RL. Network support for drinking, Alcoholics Anonymous and long-term matching effects. Addiction. 1998;93:1313–1333. doi: 10.1046/j.1360-0443.1998.93913133.x. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17:144–158. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magura S, Knight E, Vogel HS, Mahmood D, Laudet AB, Rosenblum A, et al. Mediators of effectiveness in dual-focus self-help groups. Am J of Drug Alcohol Abuse. 2003;29:301–322. doi: 10.1081/ADA-120020514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mäkela K. Alcoholics Anonymous as a mutual-help movement: A study in eight societies. University of Wisconsin Press; Madison, WI: 1996. [Google Scholar]
- Miller W, Del Boca F. Measurement of drinking behavior using the Form 90 family of instruments. J Stud Alcohol. 1994;12:112–118. doi: 10.15288/jsas.1994.s12.112. [DOI] [PubMed] [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational Enhancement Therapy manual: A clinical research guide for therapists treating individuals with alcohol abuse and dependence. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1992. [Google Scholar]
- Morgenstern J, Bux D, Labouvie E, Blanchard KA, Morgan TJ. Examining mechanisms of action in 12-step treatment: The role of 12-step cognitions. J Stud Alcohol. 2002;63:665–672. doi: 10.15288/jsa.2002.63.665. [DOI] [PubMed] [Google Scholar]
- Murray TS, Malcarne VL, Goggin K. Alcohol-related God/higher power control beliefs, locus of control, and recovery within the Alcoholics Anonymous paradigm. Alcohol Treat Q. 2003;21:23–39. [Google Scholar]
- National Survey on Drug Use and Health. The NSDUH Report. Office of Applied Studies; 2009. Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Nock M. Conceptual and design essentials for evaluating mechanisms of change. Alcohol Clin Exp Res. 2007;31:4s–12s. doi: 10.1111/j.1530-0277.2007.00488.x. [DOI] [PubMed] [Google Scholar]
- Nowinski J, Baker S, Carroll KM. NIAAA Project MATCH Monograph Series. Vol. 1. National Institute on Alcohol Abuse and Alcoholism; Rockville, MD: 1995. Twelve-Step Facilitation Therapy Manual: A Clinical Research Guide for Therapists Treating Individuals with Alcohol Abuse and Dependence. [Google Scholar]
- Oxford Group. What is the Oxford Group? London: Oxford University Press; 1933. [Google Scholar]
- Pagano M, Friend K, Tonigan J, Stout R. Helping other alcoholics in Alcoholics Anonymous and drinking outcomes: Findings from project MATCH. J Stud Alcohol Drugs. 2004;65:766–773. doi: 10.15288/jsa.2004.65.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagano M, Zemore S, Onder C, Stout R. Predictors of initial AA-related helping: Findings from project MATCH. J Stud Alcohol Drugs. 2009;70:117–125. doi: 10.15288/jsad.2009.70.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardini DA, Plante TG, Sherman A, Stump JE. Religious faith and spirituality in substance abuse recovery: Determining the mental health benefits. J Subst Abuse Treat. 2000;19:347–354. doi: 10.1016/s0740-5472(00)00125-2. [DOI] [PubMed] [Google Scholar]
- Pargament K, Kennell J, Hathaway W, Grevengoed N. Religion and the problem-solving process: Three styles of coping. J Sci Study Relig. 1988;27:90–104. [Google Scholar]
- Pargament KI, Koenig HG, Tarakeshwar N, Hahn J. Religious coping methods as predictors of outcomes of psychological, physical, and spiritual outcomes among medically ill elderly patients: A two-year longitudinal study. J Health Psychol. 2004;9:713–730. doi: 10.1177/1359105304045366. [DOI] [PubMed] [Google Scholar]
- Pearce MJ, Rivinoja CM, Koenig HG. Spirituality and health: Empirically based reflections on recovery, in Recent Developments in Alcoholism. In: Galanter M, Kaskutas LA, editors. Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. 18. Vol. 18. Springer; New Jersey: 2008. pp. 187–208. [DOI] [PubMed] [Google Scholar]
- Peele S. Research issues in assessing addiction treatment efficacy: how cost effective are Alcoholics Anonymous and private treatment centers? Drug Alcohol Depend. 1990;25(2):179–182. doi: 10.1016/0376-8716(90)90060-r. [DOI] [PubMed] [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Robinson EA, Cranford J, Webb JR, Brower KJ. Six-month changes in spirituality, religiousness, and heavy drinking in a treatment-seeking sample. J Stud Alcohol Drugs. 2007;68:282–290. doi: 10.15288/jsad.2007.68.282. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB. Structured Clinical Interview for DSM-III (SCID) Biometrics Research Division, New York State Psychiatric Institute; New York: 1985. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4. Harper Collins; New York: 2001. [Google Scholar]
- Timko C, Finney J, Moos R, Moos B. The process of treatment selection among previously untreated help-seeking problem drinkers. J Subst Abuse. 1993;5:203–220. doi: 10.1016/0899-3289(93)90064-i. [DOI] [PubMed] [Google Scholar]
- Tix AP, Frazier PA. The use of religious coping during stressful life events: Main effects, moderation, and mediation. J of Consult Clin Psychol. 1998;66:411–422. doi: 10.1037//0022-006x.66.2.411. [DOI] [PubMed] [Google Scholar]
- Tonigan JS, Connors GJ, Miller WR. Participation and involvement in Alcoholics Anonymous. In: Babor T, DelBoca F, editors. Treatment Matching in Alcoholism. Cambridge University Press; New York: 2003. pp. 184–204. [Google Scholar]
- Tonigan JS, Miller WR, Schermer C. Atheists, agnostics, and Alcoholics Anonymous. J Stud Alcohol. 2002;63:534–541. doi: 10.15288/jsa.2002.63.534. [DOI] [PubMed] [Google Scholar]
- Trimpey J, Ellis A. The Small Book: A Revolutionary Approach To Overcoming Drug And Alcohol Dependence. Random House Publishing Group; New York: 1995. [Google Scholar]
- Vaillant GE. The natural history of alcoholism: Causes, patterns, and paths to recovery. Harvard University Press; Cambridge, MA: 1983. [Google Scholar]
- Vaillant GE. Spiritual Evolution: A Scientific Defense of Faith. Broadway Books; New York: 2008. [Google Scholar]
- Walitzer KS, Derman KH, Barrick C. Facilitating involvement in Alcoholics Anonymous during out-patient treatment: A randomized clinical trial. Addiction. 2009;104:391–401. doi: 10.1111/j.1360-0443.2008.02467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winzelberg A, Humphreys K. Should patients’ religiousness influence clinicians’ referral to 12-step self-help groups? Evidence from a study of 3,018 male substance abuse patients. J Consult Clin Psychol. 1999;67:790–794. doi: 10.1037//0022-006x.67.5.790. [DOI] [PubMed] [Google Scholar]
- Ye Y, Kaskutas LA. Using propensity scores to adjust for selection bias when assessing the effectiveness of Alcoholics Anonymous in observational studies. Drug Alcohol Depend. 2009;104:56–64. doi: 10.1016/j.drugalcdep.2009.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zemore SE. A role for spiritual change in the benefits of 12-step involvement. Alcohol Clin Exp Res. 2007;31:76s–79s. doi: 10.1111/j.1530-0277.2007.00499.x. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Kaskutas LA. 12-step involvement and peer helping in day hospital and residential programs. Subst Use Misuse. 2008;43:1882–1903. doi: 10.1080/10826080802297534. [DOI] [PubMed] [Google Scholar]
- Zemore SE, Pagano ME. Research on Alcoholics Anonymous and Spirituality in Addiction Recovery. Vol. 18. New York: Springer; 2008. Kickbacks from helping others: Health and recovery; pp. 141–66. [DOI] [PubMed] [Google Scholar]