Abstract
Background
A hallmark symptom of cancer cachexia is the loss of skeletal muscle. This is at least partially due to a deregulation of the growth hormone/IGF-1 axis and a subsequently impaired protein synthesis in skeletal muscle. Here, we investigated the effect of IGF-1 supplementation in a rat model of cancer cachexia.
Methods
Juvenile rats were inoculated with the Yoshida AH-130 hepatoma and treated once daily with 0.3 mg kg−1 day−1 (low dose) or 3 mg kg−1 day−1 (high dose) IGF-1 or placebo for a period of maximal 16 days. Body weight and body composition (by NMR) were assessed at baseline and at the end of the study or day of death. Locomotor activity and food intake were assessed at baseline and day 10/11 after tumour inoculation for 24 h.
Results
Untreated tumour-bearing rats lost 55.3 ± 2.14 g body weight, which was reduced by low-dose to −39.6 ± 11.1 g (p = 0.0434) and high-dose IGF-1 to −42.7 ± 8.8 g (p = 0.057). Placebo-treated rats lost 41.4 ± 2.0-g lean mass, which was attenuated by low-dose IGF-1 (−28.8 ± 8.3 g, p = 0.041) and high-dose IGF-1 (−30.9 ± 7.4, p = 0.067). Spontaneous activity and food intake were improved by low-dose IGF-1 only. No effect on fat mass was observed. Low-dose IGF-1 significantly reduced mortality (HR = 0.45, 95%CI = 0.21–0.93, p = 0.0315), whilst the high dose did not reach significance (HR = 0.68, 95%CI = 0.26–1.74, p = 0.42).
Conclusion
Low-dose IGF-1 reduced mortality and attenuated loss of body weight as well as muscle mass in the Yoshida hepatoma rat model. Moreover, an improved quality of life was observed in these animals. Further experiments using different doses are necessary.
Keywords: Cancer cachexia, Weight loss, Wasting, Insulin like growth factor-1, Survival, Body composition
Introduction
Patients who suffer from cancer cachexia have a poor quality of life, show increased rates of morbidity and mortality, as well as a poorer responsiveness to antineoplastic therapies [1]. It is estimated that 25% of all cancer patients die as a result of cachexia, which is a multifactorial process [2, 3]. In these patients, both proteins and fat are lost due to wasting. Skeletal muscle accounts for approximately 50% of the body’s protein; hence, it is severely affected by the condition [4]. At the same time, the major intrinsic anabolic factor insulin-like growth factor 1 (IGF-1), which enhances skeletal muscle protein synthesis and proliferation and differentiation of satellite cells, is reduced cancer cachexia [5]. The effects of IGF-1 on skeletal muscle are mediated mainly by the PI3K/Akt pathway leading to the downstream activation of protein synthesis [6] and inhibition of FOXO-1, which regulates the expression of the rate-limiting ubiquitin E3-ligases Murf-1 and MAFbx, thereby reducing proteosomal protein degradation [7, 8]. Recombinant IGF-1 has clinically been used in growth hormone-resistant growth defects in children [9]. However, there have been concerns about side effects that include arthralgia and hyperplasia of lymph nodes, and an increased risk for malignancy has been discussed [10]. Interestingly, a study in children with growth impairment describes the profound effect of IGF-1 leading to increased BMI and fat mass [11].
Anti-cachectic therapy in patients with cancer cachexia is so far limited to anabolic steroids, which have not been very successful and may have serious side effects such as kidney failure [12]; therefore, treatment alternatives are urgently needed. Here, the effects of IGF-1 treatment on body weight, body composition and survival were assessed in the rat Yoshida hepatoma cancer cachexia model.
Methods
Animal model
Juvenile Wistar Han rats (weight approx. 200 g) were injected with 108 AH-130 cells into the peritoneum, and the animals were monitored over a period of maximal 16 days. Before tumour inoculation, the baseline weight, body composition, quality of life indicators (spontaneous activity and food intake) were assessed. Rats were randomized into placebo (n = 37), 0.3 mg kg−1 day−1 IGF-1 (n = 14) and 3 mg kg−1 day−1 IGF-1 (n = 15). IGF-1 was obtained from the National Hormone & Peptide Program (Harbor-UCLA Medical Center, Torrance, USA). IGF-1 or placebo (saline) was injected subcutaneously once daily. Body composition and weight were recorded on day 16 or the respective days of killing, if an animal was killed prematurely due to reaching ethical endpoints. Locomotor activity and food intake were determined on day 10/11. At the end of the study, plasma was collected and the organs were removed and weighed. Tumour cell number was determined using a Neubauer chamber.
Body composition
Body composition (fat and lean body mass) was analysed with an NMR spectroscopy device EchoMRI-700TM (Echo Medical Systems, Houston, TX) as described before [13].
Quality of life indicators
Animals were housed individually and spontaneous movement recorded by an infrared monitoring system (Supermex, Muromachi, Tokyo, Japan) over a 24-h period. Also, food intake was recorded during this period.
Statistics
Data were analysed using GraphPad PRISM 5.0 (GraphPad Software, Inc., La Jolla, CA, USA). The results are shown as mean ± SEM. The data were tested for normal distribution with the Kolmogorov–Smirnov test. Data with normal distribution were analysed with ANOVA followed by Student’s t test, whilst data without normal distribution were analysed by Kruskal–Wallis and Mann–Whitney U test. Survival was assessed by Cox proportional hazard analysis. A p value of <0.05 was considered significant.
Results
No effect of IGF-1 treatment was observed on tumour growth; total cell numbers at the end of the study were 2.83 ± 0.42 × 109 and 2.50 ± 0.28 × 109 cells for 0.3 and 3 mg kg−1 day−1 IGF-1, respectively, whilst untreated rats had a mean of 2.21 ± 0.23 × 109 cells (p > 0.2 vs. both IGF-1 doses). No signs of other malignancies were observed during necropsy.
Body weight and body composition
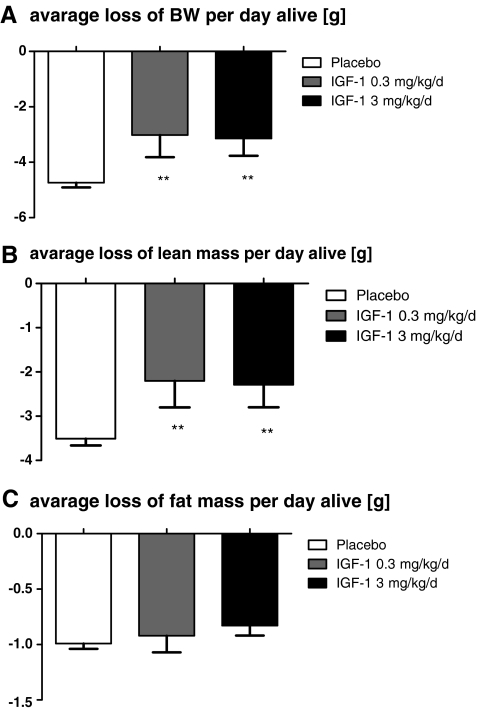
The overall weight loss at the end of the study or day of death was highest in the placebo group (−55.3 ± 2.14 g) and was reduced by both low-dose (−39.6 ± 11.1 g, p = 0.0434) and high-dose IGF-1 (−42.7 ± 8.8 g, p = 0.057). This is also seen when the average weight loss per day alive is calculated (Fig. 1a). As expected, treatment with IGF-1 reduced the wasting of lean body mass, i.e. skeletal muscle. Placebo-treated rats lost 41.4 ± 2.0 g lean mass, which was attenuated by low-dose IGF-1 (−28.8 ± 8.3 g, p = 0.041) and high-dose IGF-1 (−30.9 ± 7.4, p = 0.067), which is also observed in loss of lean mass per day alive (Fig. 1b). Treatment had no effect on overall loss of fat mass (placebo, −11.5 ± 0.5 g; low-dose IGF-1, −12.4 ± 2 g; high-dose IGF-1, −11.0 ± 1.3 g, all p > 0.1) or the loss of fat mass per day alive (Fig. 1c).
Fig. 1.
Average loss of body weight (a), lean body mass (b) and fat mass (c). Data were calculated as change per day alive. IGF-1 reduced loss of body weight and lean mass, but had no effect on fat mass. **p < 0.01
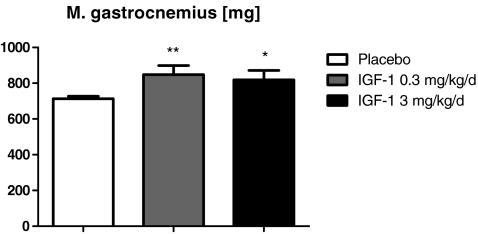
Organ weights
As expected, a strong effect on tumour burden was seen on organ weight. The weight of the liver, spleen, kidney, brown adipose tissue (BAT), M. extensor digitalis longus (EDL), M. tibialis and M. gastrocnemius (Table 1 and Fig. 2) was improved by low-dose IGF-1. The high dose only improved the weight of BAT, EDL, M. tibialis and M. gastrocnemius (Table 1 and Fig. 2). Heart, lung, white adipose tissue (WAT, epididymal fat pad) and M. soleus did not show any changes in weight (Table 1).
Table 1.
Organ and tissue weights at day 16 (end of study) or day of death
| Organ weight (mg) | Placebo (n = 37) | IGF-1 0.3 mg (n = 14) | IGF-1 3 mg (n = 15) |
|---|---|---|---|
| BW baseline (g) | 210 ± 2 | 213 ± 3 | 211 ± 3 |
| BW end of study (g) | 151 ± 3 | 174 ± 11** | 168 ± 10* |
| heart | 505.21 ± 14.00 | 539.56 ± 31.57 | 528.51 ± 25.81 |
| lung | 885.22 ± 29.57 | 1,023.54 ± 108.44 | 925.11 ± 66.35 |
| liver | 6,093.39 ± 227.81 | 7,399.51 ± 440.45* | 6,756.66 ± 490.83 |
| spleen | 163.64 ± 10.01 | 266.42 ± 49.29** | 217.97 ± 41.39 |
| kidney | 698.41 ± 16.58 | 794.21 ± 24.74** | 744.65 ± 25.94 |
| WAT | 86.38 ± 26.43 | 301.20 ± 126.86 | 146.42 ± 70.90 |
| BAT | 78.59 ± 3.14 | 123.18 ± 14.80*** | 109.00 ± 14.39** |
| Gastrocnemius | 713.22 ± 14.07 | 847.58 ± 51.37** | 818.84 ± 52.38* |
| Soleus | 69.73 ± 1.43 | 76.70 ± 3.49 | 73.58 ± 3.91 |
| Tibialis | 262.49 ± 6.10 | 325.06 ± 20.48*** | 295.74 ± 20.11* |
| EDL | 63.66 ± 1.48 | 74.04 ± 5.11* | 71.98 ± 4.24* |
*p < 0.05, **p < 0.001, ***p < 0.001
Fig. 2.
Weight of the M. gastrocnemius at the end of the study or the day of death. IGF-1-treated groups have a higher muscle weight. **p < 0.01
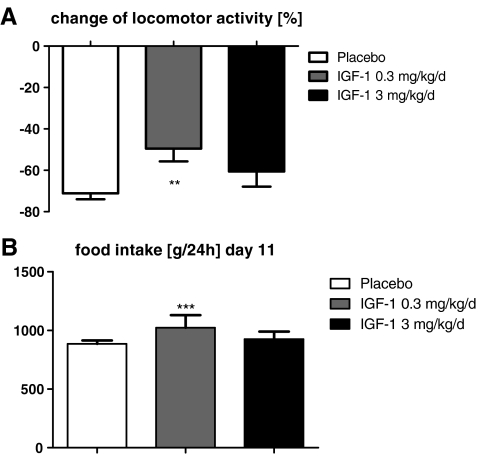
Quality of life
Spontaneous activity and food intake are indicators for the quality of life of an animal. Baseline 24-h spontaneous activity and food intake were similar in all groups (all p > 0.2, data not shown). The activity was reduced by tumour burden in all groups on day 10/11. Low-dose IGF-1 attenuated the reduced movement (Fig. 3a), whilst high-dose IGF-1 was ineffective (p > 0.1). This was also observed for food intake in the high-dose group, whilst low-dose IGF-1 increased food intake vs. placebo (Fig. 3b).
Fig. 3.
Quality of life: 0.3-mg kg−1 day−1 IGF-1 improved spontaneous activity, as shown by an attenuated reduction compared with baseline values (a) and total food intake per 24 h (b) on day 10/11 compared with placebo, whilst 3 mg kg−1 day−1 was ineffective.**p < 0.01, ***p < 0.001
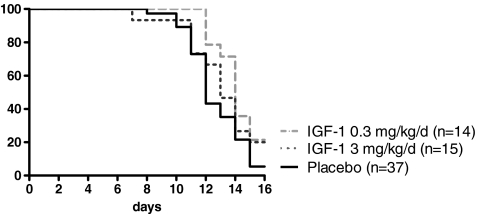
Survival
The overall survival was 5% in the placebo group, 21% in the low-dose and 20% in the high-dose IGF-1 groups (Fig. 4). The median survival was 12 days in the placebo group, 14 days in the low-dose and 13 days in the high-dose IGF-1 groups. Only low-dose IGF-1 significantly reduced mortality (HR = 0.45, 95%CI = 0.21–0.93, p = 0.0315), whilst the high dose did not reach significance (HR = 0.68, 95%CI = 0.26–1.74, p = 0.42).
Fig. 4.
Kaplan–Meier survival curves: 03-mg kg−1 day−1 IGF-1 reduced mortality compared with placebo; 3 mg kg−1 day−1 is ineffective
Discussion
We have shown that the tumour growth was not affected by IGF-1, but the loss of body weight was attenuated, the quality of life was improved, and the survival was increased by treatment with IGF-1.
A previous study has shown that IGF-1 levels are lower in the liver and skeletal muscle of Yoshida AH-130 hepatoma bearing rats, suggesting that impaired IGF-1 signalling is involved in the pathogenesis of muscle wasting in tumour-bearing rats [5]. A recent publication using plasmid gene transfer of IGF-1 into M. tibialis of tumour-bearing mice and rats showed resistance to IGF-1, whilst the same gene transfer in young and old animals increased the fibre size [14]. Contrary to these results, a reduction of weight loss was seen in both Yoshida hepatoma-bearing groups treated with recombinant IGF-1 in the present study, where lean body mass loss was reduced. This finding is supported by the higher weights of the mixed fibre type muscles M. gastrocnemius and M. tibialis, as well as the fast-twitch muscle EDL, whilst the weight of the slow-twitch M soleus was not increased. The contrary results to the study by Penna et al. [14] are likely due to the difference in IGF-1 administration and dose. However, our results also suggest that IGF-1 is not able to fully prevent skeletal muscle wasting in tumour-bearing rats and that increasing the dose does not produce better results as the 0.3-mg kg−1 day−1 dose was superior to 3-mg kg−1 day−1 IGF-1. Together with the lack of effect on the liver, kidney and spleen weight, this may point to the serious side effects of high-dose IGF-1, which do not seem to include increased tumour cell proliferation. Overall, the incomplete prevention of muscle atrophy may be due to the increased expression of negative regulators of muscle mass such as myostatin [15] or the inflammatory cytokines, which can impair IGF-1 bioavailability and signalling [16]. Furthermore, the half-life of IGF-1 is short [17], which limits its activity in our study. Ng et al. [18] used a continuous infusing of IGF-1 in Fischer 344 rats bearing a fibrosarcoma and showed a preservation of lean mass. In the present study, treatment had no effect on overall fat mass, supported by the unchanged weight of the epididymal fat pad, but the weight of brown adipose tissue was higher in IGF-treated rats, suggesting an improved thermogenesis [19].
Locomotor activity and food intake are considered quality of life indicators in animals [20]. Compared with baseline, a strong decrease in activity and food intake was seen in all groups 10 days after tumour inoculation, but the group treated with low-dose IGF-1 had significantly improved food intake and a higher activity compared with placebo, suggesting an improved quality of life. High-dose IGF-1 was ineffective.
The Yoshida hepatoma model has been known to have a high mortality rate in untreated tumour-bearing rats [21], which is in accordance with the results of this study. Both doses of IGF-1 reduced the risk of death (HR = 0.45 and 0.68 for the low and high doses, respectively); however, only the low dose significantly improved outcome compared with placebo.
In the 0.3-mg kg−1 day−1 IGF-1 group, reduced mortality and attenuated loss of body weight, as well as muscle mass, were seen in the Yoshida hepatoma rat model. Moreover, an improved quality of life was observed in these animals. The 3-mg kg−1 day−1 IGF-1 dose was likely too high and had weaker effects compared with the lower dose. This may be due to a decreased sensitivity of target tissue or even general toxic effects. Therefore, further experiments using different doses are necessary.
In conclusion, IGF-1 attenuated the development of cachexia, improved quality of life and survival. The treatment had no effect on tumour growth. The therapeutic approach of IGF-1 for tumour-associated cachexia should be tested in further studies. IGF-1 may be an interesting candidate for a multidrug approach to treat cancer cachexia.
Acknowledgements
The authors have read and complied with the principles of ethical authorship of the Journal of Cachexia, Sarcopenia and Muscle [22].
Conflict of interest
All authors declare that they have no conflict of interests regarding this present study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Kilgour RD, Vigano A, Trutschnigg B, Hornby L, Lucar E, Bacon SL, Morais JA. Cancer-related fatigue: the impact of skeletal muscle mass and strength in patients with advanced cancer. J Cachex Sarcopenia Muscle. 2010;1:177–85. doi: 10.1007/s13539-010-0016-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loberg RD, Bradley DA, Tomlins SA, Chinnaiyan AM, Pienta KJ. The lethal phenotype of cancer: the molecular basis of death due to malignancy. CA Cancer J Clin. 2007;57(4):225–41. doi: 10.3322/canjclin.57.4.225. [DOI] [PubMed] [Google Scholar]
- 3.von Haehling S, Anker SD. Cachexia as a major underestimated and unmet medical need: facts and numbers. J Cachex Sarcopenia Muscle. 2010;1:1–5. doi: 10.1007/s13539-010-0002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Acharyya S, Guttridge DC. Cancer cachexia signaling pathways continue to emerge yet much still points to the proteasome. Clin Cancer Res. 2007;13(5):1356–61. doi: 10.1158/1078-0432.CCR-06-2307. [DOI] [PubMed] [Google Scholar]
- 5.Costelli P, Muscaritoli M, Bossola M, Penna F, Reffo P, Bonetto A, et al. IGF-1 is downregulated in experimental cancer cachexia. Am J Physiol Regul Integr Comp Physiol. 2006;291(3):R674–83. doi: 10.1152/ajpregu.00104.2006. [DOI] [PubMed] [Google Scholar]
- 6.Rommel C, Bodine SC, Clarke BA, Rossman R, Nunez L, Stitt TN, et al. Mediation of IGF-1-induced skeletal myotube hypertrophy by PI(3)K/Akt/mTOR and PI(3)K/Akt/GSK3 pathways. Nat Cell Biol. 2001;3(11):1009–13. doi: 10.1038/ncb1101-1009. [DOI] [PubMed] [Google Scholar]
- 7.Sandri M, Sandri C, Gilbert A, Skurk C, Calabria E, Picard A, et al. Foxo transcription factors induce the atrophy-related ubiquitin ligase atrogin-1 and cause skeletal muscle atrophy. Cell. 2004;117(3):399–412. doi: 10.1016/S0092-8674(04)00400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lenk K, Schuler G, Adams V. Skeletal muscle wasting in cachexia and sarcopenia: molecular pathophysiology and impact of exercise training. J Cachexia Sarcopenia Muscle. 2010;1:9–21. doi: 10.1007/s13539-010-0007-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Clayton PE, Ayoola O, Whatmore AJ. Patient selection for IGF-I therapy. Horm Res. 2006;65:28–34. doi: 10.1159/000090644. [DOI] [PubMed] [Google Scholar]
- 10.Singleton JR, Feldman EL. Insulin-like growth factor-I in muscle metabolism and myotherapies. Neurobiol Dis. 2001;8:541–54. doi: 10.1006/nbdi.2001.0416. [DOI] [PubMed] [Google Scholar]
- 11.Underwood LE, Backeljauw P, Duncan V. Effects of insulin-like growth factor I treatment on statural growth, body composition and phenotype of children with growth hormone insensitivity syndrome. GHIS Collaborative Group. Acta Paediatr Suppl. 1999;88:182–4. doi: 10.1111/j.1651-2227.1999.tb14386.x. [DOI] [PubMed] [Google Scholar]
- 12.Gullett NP, Hebbar G, Ziegler TR. Update on clinical trials of growth factors and anabolic steroids in cachexia and wasting. Am J Clin Nutr. 2010;91:1143S–7S. doi: 10.3945/ajcn.2010.28608E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Palus S, Akashi Y, von Haehling S, Anker SD, Springer J. The influence of age and sex on disease development in a novel animal model of cardiac cachexia. Int J Cardiol. 2009;133:388–93. doi: 10.1016/j.ijcard.2009.01.060. [DOI] [PubMed] [Google Scholar]
- 14.Penna F, Bonetto A, Muscaritoli M, Costamagna D, Minero VG, Bonelli G, et al. Muscle atrophy in experimental cancer cachexia: is the IGF-1 signaling pathway involved? Int J Cancer. 2010;127:1706–17. doi: 10.1002/ijc.25146. [DOI] [PubMed] [Google Scholar]
- 15.Zhou X, Wang JL, Lu J, Song Y, Kwak KS, Jiao Q, et al. Reversal of cancer cachexia and muscle wasting by ActRIIB antagonism leads to prolonged survival. Cell. 2010;142:531–43. doi: 10.1016/j.cell.2010.07.011. [DOI] [PubMed] [Google Scholar]
- 16.Lazarus DD, Moldawer LL, Lowry SF. Insulin-like growth factor-1 activity is inhibited by interleukin-1 alpha, tumor necrosis factor-alpha, and interleukin-6. Lymphokine Cytokine Res. 1993;12:219–23. [PubMed] [Google Scholar]
- 17.Ballard FJ, et al. Effects of interactions between IGFBPs and IGFs on the plasma clearance and in vivo biological activities of IGFs and IGF analogs. Growth Regul. 1993;3:40–4. [PubMed] [Google Scholar]
- 18.Ng EH, Rock CS, Lazarus DD, Stiaino-Coico L, Moldawer LL, Lowry SF. Insulin-like growth factor I preserves host lean tissue mass in cancer cachexia. Am J Physiol. 1992;262:R426–R431. doi: 10.1152/ajpregu.1992.262.3.R426. [DOI] [PubMed] [Google Scholar]
- 19.Richard D, Picard F. Brown fat biology and thermogenesis. Front Biosci. 2011;16:1233–60. doi: 10.2741/3786. [DOI] [PubMed] [Google Scholar]
- 20.Bauhofer A, Witte K, Celik I, Pummer S, Lemmer B, Lorenz W. Sickness behaviour, an animal equivalent to human quality of life, is improved in septic rats by G-CSF and antibiotic prophylaxis. Langenbecks Arch Surg. 2001;386:132–40. doi: 10.1007/s004230100206. [DOI] [PubMed] [Google Scholar]
- 21.Poynter RW. Studies on the mechanism of resistance to alkylating agents of three ascites tumours in the rat. Biochem Pharmacol. 1970;19:1387–97. doi: 10.1016/0006-2952(70)90054-7. [DOI] [PubMed] [Google Scholar]
- 22.Von Haeling S, Morely JE, Coats AJS, Anker SD. Ethical guidelines for authorship and publishing in the Journal of Cachexia, Sarcopenia and Muscle. J Cachex Sarcopenia Muscle. 2010;1:7–8. doi: 10.1007/s13539-010-0003-5. [DOI] [PMC free article] [PubMed] [Google Scholar]