Abstract
Colonoscopies are usually regarded as safe procedures with low complication rates and are recommended for anyone over the age of fifty for colon cancer screening. Splenic rupture is a rare complication of colonoscopy with few reported cases in the English literature. We present the only reported case of such a complication in the state of Hawai‘i and the 44th reported case in the English literature. Physicians need to be more aware of the possibility of splenic rupture following colonoscopy to avoid delay of diagnosis and treatment of this life-threatening complication.
Introduction
According to the Centers for Disease Control and Prevention (CDC), approximately 14.2 million colonoscopies were performed in 2002.1 Although the procedure is considered safe, complications such as perforation and bleeding with rates ranging between 0.029% to 0.72% and 0.2% to 2.67% respectively have been reported.2 The major risk factors for these complications include inflammatory bowel disease, therapeutic procedures performed during colonoscopy and intraabdominal adhesions from prior abdominal surgeries. The three mechanisms of perforation during colonoscopy include mechanical perforation, over-zealous air insufflation, and a therapeutic procedure (e.g. polypectomy).3 Other less common complications of colonoscopies include: infection, post-polypectomy coagulation syndrome, complications of anesthesia, and splenic rupture.
The authors present a case of massive hemoperitoneum from splenic rupture following a colonoscopy with polypectomy.
Case Report
A 55-year-old part Caucasian, part Hawaiian woman, with past medical history significant for hypertension, myocardial infarction and two coronary artery stents at age 47, coronary artery bypass graft at age 51, underwent diagnostic colonoscopy at an outside facility with removal of three sigmoid polyps. Following the procedure, the patient returned home without any pain or bleeding and restarted her Plavix (which had not been taken for one week prior to the procedure) and beta blocker. Twelve hours following the completion of the procedure, she presented to our institution with nausea and increasing abdominal pain, described as 9 out of 10 in intensity, worse on the left side.
On physical examination, the patient was afebrile, with a blood pressure of 90/59, heart rate of 70 and 11 respirations/per minute. After administration of three liters of normal saline, the blood pressure temporarily rose to 110/70. Her abdomen was somewhat taut and tender to palpation with guarding, slight distention, rebound tenderness in left lower quadrant, and decreased bowel sounds throughout consistent with an acute abdomen. She had good rectal tone and guaiac test was negative for occult blood. Patient's laboratory findings showed a hemoglobin/hematocrit of 9.3/26.4. Although the abdominal films did not demonstrate free air, it was decided to take patient for exploratory laparotomy as she demonstrated an acute abdomen likely due to perforation from colonoscopy.
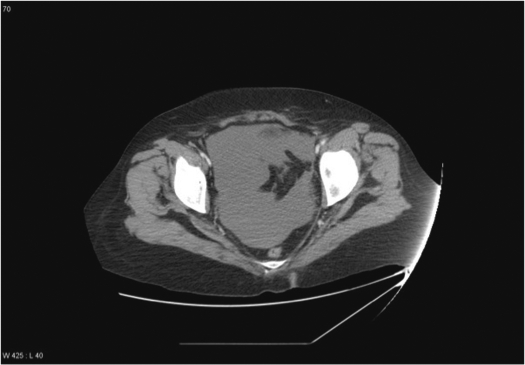
While the operating room was prepared, the emergency room physician completed a stat CT of the abdomen and pelvis, revealing a large splenic hematoma with fluid around the liver and filling the abdomen (Figures 1 and 2). As the patient was already in the operating room and becoming hemodynamically unstable when the scan became available, it was decided to proceed with surgery rather than manage with splenic artery embolization by an interventional radiologist. Surgical findings included 1.5 liters of hemoperitoneum and at least another one liter of clotted blood around the spleen where the source of the bleeding was localized. The splenorrhaphy attempted in controlling the active bleeding was without success and thus splenectomy was performed. The patient received four units of packed red blood cells and two liters of crystalloid infusion intraoperatively.
Figure 1.
Large Splenic Hematoma and Blood Around the Liver
Figure 2.
Massive Hemoperitoneum
Postoperatively the patient remained hemodynamically stable with hemoglobin of 12.0. Her hemoglobin and hematocrit (H/H) were monitored throughout the rest course of her hospital stay, and she received two more units of packed red blood cells prior to discharge given cardiac history. The drop in H/H was thought to be most likely secondary to mobilization of third space fluid rather than acute bleeding.
Discussion
Upon arrival to the emergency department, the patient was hypotensive secondary to active bleeding and antihypertensive medication. Her seemingly normal pulse was attributed to beta-blocker taken after the procedure, thus masking the normal physiologic response to blood loss. The abdominal x-rays were taken to rule out bowel perforation, which represents one of the more common complications of colonoscopy. Although free air was not present, the peritoneal signs exhibited by the patient demanded prompt exploratory laparotomy. Given that the CT scan showed massive hemoperitoneum around the spleen and patient was exhibiting signs of hemodynamic instability, the decision to undergo exploratory laparotomy rather than conservative management with splenic artery embolization may have been justified.
Complications of colonoscopy are relatively rare despite its frequency. In a recent study of over 230,000 outpatient colonoscopies only 0.31% suffered complications, with the most common three being bleeding (0.22%), perforation (0.03%) and cardiorespiratory complications (0.06%).4 Factors identified with increased chances of bleeding include male sex, higher age, nonscreening indication, biopsies, polypectomies and absence of sedation/analgesia, whereas increased chances of perforation include biopsies and polypectomies. The only discernable risk factor for cardiorespiratory complications was advanced age.
Among other rare complications of colonoscopy, splenic rupture following the procedure is one of the rarest and documented only in case reports. Although not completely elucidated, it is postulated that injury to the spleen may occur from traction of the splenocolic ligament, which may be complicated by adhesions from previous abdominal surgeries or disease processes (Crohn's disease and pancreatitis) or technical maneuvers slide-by, alpha maneuver, straightening of the sigmoid loop and externally applied pressure.5 Patients typically present within 24 hours following the procedure with diffuse abdominal pain or localized left upper quadrant pain with positive Kehr's sign, hypovolemia, tachycardia and anemia due to massive hemoperitoneum.6 Splenic rupture is a rare but potentially lethal complication with an overall estimated incidence of 0.004 percent.7
The goal of management of splenic injury is nonoperative, but splenectomy seems to be difficult to avoid following injury after colonoscopy. In a review of 40 case reports of splenic injury, 30 patients underwent splenectomy.8 The rest underwent conservative management which included hospital monitoring, serial hemoglobin checks and serial examinations and only one embolization. Most of the splenectomy cases predate the advent and ease of CT scanning, hence the high rate of surgical intervention. Nonetheless, splenic injury following colonoscopy should probably fall in the same category as splenic injury following blunt trauma. In a study of 815 patients with blunt splenic injury, splenic artery embolization was associated with greater success of non operative management, decline in mortality, an increase in overall splenic salvage and shorter length of stay when compared with operative management.9 Therefore it is imperative that the primary provider is aware of the options to treatment of splenic injuries and the non-operative modalities available at his/her institution.
Since the first case of splenic rupture after colonoscopy was reported in 1974, there have been a total of 54 new cases as of 2008, 43 of which are in the English language.10 Over half of these followed diagnostic procedures and the remaining occurred after removal of polyps or following biopsies.11 The number of both diagnostic and therapeutic colonoscopies will likely increase yearly with the aging population. Awareness of colonoscopy complications, such as splenic rupture, treatment modalities and their availability at one's institution need to be addressed. Early diagnosis and treatment of splenic injury following colonoscopy prevents morbidity and mortality in this rarely encountered complication.
Footnotes
There were no sources of support for this paper.
References
- 1.Seeff LC, Richards TB, Shapiro JA, Nadel MR, Manninen DL, Given LS. How many endoscopies are performed for colorectal cancer screening? Results for the CDC's survey of endoscopic capacity. Gastroent. 2004;127:1670–1677. doi: 10.1053/j.gastro.2004.09.051. [DOI] [PubMed] [Google Scholar]
- 2.Pignone M, Rich M, Teutsch SM, et al. Screening for colorectal cancers in adults at average risk: a summary of the incidence for the US preventive services task force. Ann Int Med. 2002;137:132–141. doi: 10.7326/0003-4819-137-2-200207160-00015. [DOI] [PubMed] [Google Scholar]
- 3.Holubar S, Dwivedi A, Eisendorfer J, Levine R, et al. Splenic Rupture: An Unusual Complication of Colonoscopy. Am Surgeon. 2007;73:393–396. [PubMed] [Google Scholar]
- 4.Crispin A, Birkner B, Munte A, et al. Process quality and incidence of acute complications in a series of more than 230,000 outpatient colonoscopies. Endoscopy. 2009;41(12):1018–1025. doi: 10.1055/s-0029-1215214. [DOI] [PubMed] [Google Scholar]
- 5.Shatz DV, Rivas LA, Doherty JC. Management options of colonoscopic splenic injury. JSLS. 2006;10:239–243. [PMC free article] [PubMed] [Google Scholar]
- 6.Guerra JF, San Francisco I, Pimentel F, et al. Splenic Rupture following Colonoscopy. World J Gastroent. 2008;14:6410–6412. doi: 10.3748/wjg.14.6410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wexner SD, Garbus JE, Singh JJ. A prospective analysis of 13.580 colonoscopies: Re-evaluation of credentialing guidelines. Surg Endo. 2001;15:251–261. doi: 10.1007/s004640080147. [DOI] [PubMed] [Google Scholar]
- 8.Lalar PF, Mann BD. Splenic rupture after colonoscopy. JSLS. 2007;11:151–156. [PMC free article] [PubMed] [Google Scholar]
- 9.Sabe AA, Claridge JA, Rosenblum DI, et al. The effects of splenic artery embolization on nonoperative managent of blunt splenic injury: a 16 year experience. J Trauma: Injury, Infection and Critical Care. 2009;67(3):565–572. doi: 10.1097/TA.0b013e3181b17010. [DOI] [PubMed] [Google Scholar]
- 10.Cappellani A, Di Vita M, Zanghi A, et al. Splenic rupture after colonoscopy: Report of a case and review of literature. World J Emer Surg. 2008;3:1–5. doi: 10.1186/1749-7922-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lewis SR, Ohio D, Rowley G. Splenic injury as a rare complication of colonoscopy. Emer Med J. 2009;26:147. doi: 10.1136/emj.2008.061200. [DOI] [PubMed] [Google Scholar]