Abstract
Background
There are approximately 1,000,000 persons living with HIV/AIDS (PLH) in the United States; to reduce rates of new infection and curb disease progression, adherence to HIV medication among PLH is critical. Despite elevated trauma rates in PLH, no studies to date have investigated the relationship between dissociation, a specific symptom of trauma, and HIV medication adherence. We hypothesized that Post-Traumatic Stress Disorder (PTSD) symptoms would be associated with lower adherence, and that dissociation would moderate this relationship.
Methods
Forty-three individuals with HIV were recruited from community-based clinics to participate in a cross-sectional study. The relationship of trauma, dissociation, and their interaction to the probability of antiretroviral adherence was assessed using a hierarchical binary logistic regression analysis.
Results
Among 38 eligible participants, greater PTSD was associated with lower odds of adherence (OR = .92, p < .05). Dissociation moderated the effect of PTSD on adherence, resulting in lower odds of adherence (OR = .95, p < .05). PTSD symptoms were significantly associated with lower odds of adherence in individuals reporting high levels of dissociation (OR = .86, p < .05) but not in those reporting low levels of dissociation (OR = 1.02, p > .05).
Conclusions
This is the first study to demonstrate a relationship between dissociation and medication adherence. Findings are discussed in the context of clinical management of PLH with trauma histories and the need for interventions targeting dissociative symptomatology to optimize adherence.
Keywords: dissociation, posttraumatic stress disorder, depression, HIV/AIDS, adherence, medication
Introduction
There are estimated to be over 1,000,000 persons living with HIV/AIDS in the United States and approximately 55,000 new HIV infections every year (Center for Disease Control and Prevention, 2010). With the development of highly active antiretroviral therapy (HAART), the number of persons living with HIV (PLH) continues to increase. Adherence to a HAART regimen, defined as correspondence between the behavior of a patient and the health care recommendations received (Haynes, Sackett, & Taylor, 1980), has the potential to decrease HIV-1 RNA (viral load), increase immune function, and enhance quality of life (Hammer et al., 2006). By contrast, inconsistent adherence to antiretroviral regimens is correlated with elevated viral load and decreased CD4 cell count (Paterson et al., 2000), as well as increased HIV-related morbidity (Roca, Gomez, & Arnedo, 2000) and mortality (Jensen-Fangel et al., 2004).
HAART regimens have low tolerance of nonadherence such that optimal viral suppression requires correct use of HAART 90 to 95% of the time (Paterson et al., 2000). Moreover, nonadherence to antiretroviral medications may increase viral resistance to numerous classes of medications, thereby rendering various medication options ineffective (Bangsberg, Moss, & Deeks, 2004). This is problematic because increased transmission of resistant HIV strains raises a variety of public health concerns (Wainberg & Friedland, 1998), including increased morbidity and mortality rates. Thus, it is critical to identify individuals living with HIV/AIDS who are likely to be non-adherent so that they can receive targeted interventions designed to increase adherence to HAART.
Adherence to antiretroviral therapy is a problem for many HIV-positive individuals, with an estimated 50% to 80% of PLH unable to practice adequate adherence (Belzer, Fuchs, Luftman, & Tucker, 1999; Johnson et al., 2003; Spire et al., 2002). The reasons for nonadherence are varied. Adherence to antiretroviral regimens is logistically challenging, as the therapy often consists of three or four separate medications. If first-line or second-line treatments have been ineffective, the patient may be expected to take over twenty pills each day while following a strict diet (Berg, Michelson, & Safren, 2007). Additionally, side effects of HAART include nausea, vomiting, anemia, and peripheral neuropathy, which can contribute to nonadherence (Ammassari et al., 2001). Furthermore, a variety of patient-related psychosocial factors have been associated with poor HAART adherence (Vervoort, Borleffs, Hoepelman, & Grypdonck, 2007), including low patient self-efficacy, psychological distress, depression, exposure to trauma, forgetfulness, substance use disorders, low social support from family and friends, inadequate confidence in treatment effectiveness, and poor understanding of the relationship between nonadherence and viral resistance (Ammassari et al., 2002; Deschamps et al., 2004; Leserman, 2008). Moreover, depression has been associated with disease progression among PLH (Leserman, 2008). Although the mechanism by which psychosocial factors result in nonadherence is not fully known, there is evidence that the occurrence of psychological symptoms of distress is associated with disease progression through a decrease in adherence among PLH (Gore-Felton & Koopman, 2008).
Posttraumatic Stress Disorder in Persons Living With HIV
High rates of trauma exist among both women and men living with HIV (Brief et al., 2004; Gore-Felton, Koopman, Bridges, Thoresen, & Spiegel, 2002). Studies have shown a 33% lifetime prevalence of physical assault and 30% to 68% lifetime prevalence of sexual assault among HIV-positive individuals, versus 6.9% and 9.2% in the general population, respectively (Kalichman, Sikkema, DiFonzo, Luke, & Austin, 2002; Kessler, Sonnega, Bromet, Hughes, & Nelson, 1995; Kimerling et al., 1999b). A study among 242 primarily African American gay or bisexual HIV-positive men found that 35% of the sample had a history of sexual assault (Kalichman et al., 2002). This is considerably higher than rates reported in the general population, in which 1% of men report a lifetime history of rape and 2.8% report past molestation (Kessler et al., 1995). Similarly, PLH have higher rates of childhood physical and sexual abuse compared to the general population (Brief et al., 2004). The psychological sequelae of trauma experiences have been well documented and often result in acute or chronic anxiety symptoms (Gore-Felton, 1999b).
According to the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (APA, 2000), post-traumatic stress disorder (PTSD) is an anxiety disorder that can occur after an individual witnesses or experiences a traumatic event involving the threat of injury or death. The hallmark symptoms of PTSD include re-experiencing, avoidance/numbing, and hyperarousal (APA, 2000).
PTSD is a debilitating disorder that is prevalent at greater rates among PLH than in the general population; furthermore, it has been shown to negatively impact HIV-related health outcomes (Kimerling, Armistead, & Forehand, 1999a; Kimerling et al., 1999b). A study among HIV-positive women found that more than one-third (35%) reported a history of trauma and currently met criteria for PTSD diagnosis (Kimerling et al., 1999b). In contrast, the lifetime prevalence of PTSD among women in the general population is 9.7% (Kessler et al., 2005). A similar finding among HIV-positive gay and bisexual men showed that 36% met criteria for PTSD (Kelly, Otto-Salaj, Sikkema, Pinkerton, & Bloom, 1998b), whereas 3.6% of men in the general population have a lifetime history of PTSD diagnosis (Kessler et al., 2005). Additionally, the diagnosis of HIV itself can be a traumatic stressor. In fact, 32% of HIV-positive men meet criteria for PTSD as a result of being diagnosed with HIV (Kelly et al., 1998a). This is higher than the rates of PTSD following diagnosis of other life-threatening illnesses: for example, only 5% of patients meet PTSD criteria after being diagnosed with breast cancer (Andrykowski & Cordova, 1998). Among persons living with hepatitis C, a population whose psychosocial profile is similar to that of PLH, the estimated prevalence of PTSD is 19% to 33.5% (Lehman & Cheung, 2002; El-Serag et al., 2002; Yovtcheva et al., 2001). One study showed a PTSD prevalence of 33.5% among veterans diagnosed with hepatitis C versus 24.5% among uninfected veterans (El-Serag et al., 2002). The increased rate of PTSD following a positive HIV diagnosis may combine with the already higher rate of traumatic experiences found in PLH, resulting in a cumulative stress effect. More research is needed to understand the increased psychiatric morbidity found among PLH who also report a trauma history.
Posttraumatic Stress Disorder, Dissociation, and Antiretroviral Adherence
In addition to their general negative impact on health outcomes, there is a growing body of evidence suggesting that symptoms of traumatic stress are associated with antiretroviral nonadherence. A positive correlation exists between depression and nonadherence to antiretrovirals (Ammassari et al., 2004), and PLH with past trauma report more depressive symptoms than PLH with no history of trauma (Kalichman et al., 2002). Also, emotional distress has been shown to increase nonadherence to antiretrovirals (Singh et al., 1996), and PLH with a history of trauma report greater distress than PLH with no past trauma (Kimerling et al., 1999a).
More than half of patients living with HIV who report inconsistent adherence to HAART regimens meet diagnostic criteria for PTSD (Safren, Gershuny, & Hendriksen, 2003). Although several studies have reported an association between PTSD and antiretroviral nonadherence (Boarts, Sledjeski, Bogart, & Delahanty, 2006; Cohen, Alfonso, Hoffman, Milau, & Carrera, 2001; Safren et al., 2003; Whetten, Reif, Whetten, & Murphy-McMillan, 2008), it has not always been clear whether it is PTSD alone or in fact comorbid depression that drives this relationship (Boarts et al., 2006; Delahanty, Bogart, & Figler, 2004; Sledjeski, Delahanty, & Bogart, 2005; Vranceanu et al., 2008). Additionally, the relationship of specific symptoms of PTSD to HAART nonadherence has yet to be clarified.
Dissociative symptoms are a common but little-understood response to trauma. Dissociation is defined as a disruption or breakdown of memory, awareness, identity and/or perception. It can develop following long-term physical, sexual or psychological abuse (Vermetten, Dorahy, & Spiegel, 2007), or following an acute life stressor (Morgan et al., 2001). A dissociative coping style in the face of an inescapable traumatic experience may prevent subsequent cognitive and emotional processing of the pain associated with the trauma (Spiegel, 1997; Spiegel & Cardena, 1991); in fact, acute dissociative responses to psychological trauma increase the risk of developing chronic dissociation and chronic PTSD (Bremner et al., 1992; Butler, Duran, Jasiukaitis, Koopman, & Spiegel, 1996; Marmar et al., 1994).
There is substantial clinical and neurobiological evidence for the existence of a dissociative subtype of PTSD that involves emotional overmodulation and is mediated by prefrontal inhibition of the limbic system (Lanius et al., 2010). In contrast, the more common PTSD subtype is marked by reexperiencing and hyperarousal symptoms, and is thought to involve emotional undermodulation mediated by a failure of the prefrontal cortex to inhibit limbic regions.
Despite the dramatically elevated rates of past trauma in PLH, no studies to date have investigated the relationship between dissociative disorders (or dissociative symptoms) and antiretroviral adherence in HIV-positive individuals. Therefore, this study examined the relationships between PTSD symptoms, dissociation and antiretroviral adherence among adults with HIV/AIDS. Specifically, we hypothesized that PTSD and dissociation would be associated with lower antiretroviral adherence, and that dissociation would moderate the relationship between PTSD and nonadherence.
Methods
Procedure
Forty-three individuals with HIV were recruited from community-based clinics in the San Francisco Bay Area to participate in a cross-sectional, audio computer-assisted self interview (ACASI) survey examining the relationships of trauma symptoms, particularly PTSD and dissociation, to antiretroviral medication adherence. While some of these individuals were recruited either through advertising or their HIV health care providers, the majority were recruited from a larger Bay Area study of the effects of a group therapy intervention to reduce trauma-induced stress and high-risk behaviors in HIV-positive individuals. The participants recruited for our study were ineligible for the group therapy study because they did not meet the larger study’s inclusion criteria of HIV transmission risk behavior. The current study did not have HIV transmission risk behavior as an inclusion criterion and thus we were able to enroll them. Participants were primarily male, ethnically diverse, predominantly low-income and unemployed (see Table 1 for descriptive characteristics of the sample). Inclusion criteria were as follows: 18 years or older, English-speaking, HIV-positive, and currently in treatment with a health care provider who had prescribed antiretroviral medications for HIV.
Table 1.
Summary of Demographic Characteristics (N = 38).
| Variable | M (SD) | Range | % |
|---|---|---|---|
| Age in Years | 45.8 (7.4) | 30–60 | |
|
| |||
| Variable | N | % | |
|
| |||
| Race/Ethnicity | |||
| African-American | 8 | 21.1 | |
| Latino | 10 | 26.3 | |
| Caucasian | 14 | 36.8 | |
| Other | 6 | 15.8 | |
| Unemployed | 28 | 73.7 | |
| Income | |||
| Under $20,000 | 34 | 89.5 | |
| $20,000 or over | 4 | 10.5 | |
| Education | |||
| High School or higher | 34 | 89.5 | |
| College or higher | 8 | 21.1 | |
| In a Relationship | 18 | 47.3 | |
| In a Sexual Relationship but not Living with Partner | 10 | 26.3 | |
| Living Monogamously with Partner | 5 | 13.2 | |
| Married or Living as Married | 3 | 7.9 | |
Participants were given an overview of the study; after complete description of the study, written informed consent was obtained from each participant. The ACASI survey took approximately 45 minutes to complete. Participants answered the computerized questionnaire individually and in a private setting, with a trained interviewer present for assistance if needed. Participants were paid $20 after completing the survey, plus the cost of transportation to the assessment site.
Each participant completed measures assessing demographic characteristics, medication adherence (Modified ACTG), distress regarding stressful events (Impact of Events Scale-Revised; IES-R), depression (Center for Epidemiologic Studies-Depression Scale) and dissociative symptoms (Dissociative Experiences Scale-II). All aspects of the study were approved by the Stanford University Institutional Review Board.
Measures
Demographics
The following demographic and substance use information was assessed: age, ethnicity, education level, relationship status, employment status, income, living arrangements and alcohol/recreational drug use.
Antiretroviral Adherence
Information regarding antiretroviral adherence was obtained using two items. The first item was the following question taken from the AIDS Clinical Trial Group (ACTG) Adherence Questionnaire (Chesney et al., 2000): “Most anti-HIV medications need to be taken on a schedule, such as ‘2 times a day’ or ‘3 times a day’ or ‘every 8 hours’. How closely did you follow your specific schedule over the last four days?” Response options for this item were “Never,” “Some of the time,” “About half of the time,” “Most of the time,” “All of the time” and “Refuse to answer.” Patients who answered this question by selecting the option, “All of the time” and who also responded to the question, “Did you miss any doses of HIV medication during the past four days?” by answering “No” instead of “Yes” or “Refuse to answer” were classified as “adherent.” All other patients were classified as “nonadherent.” Patients also listed the names of specific medications they were taking as part of the ACTG questionnaire, thus allowing for evaluation of antidepressant use in the sample.
Traumatic Experiences
The Revised Impact of Events Scale (IES-R) was used to assess trauma-related symptoms (Weiss, 2007). It is a 22-item survey with each item rated on a 5-point scale ranging from 0 (“not at all”) to 4 (“extremely”), yielding an overall score that ranges from 0 to 88. The cut-off score indicative of PTSD is 33 (Creamer, Bell, & Failla, 2003). The scale has good test-retest reliability, good split-half reliability, and good construct validity (Weiss, 2007). The IES-R demonstrated good reliability in the current study, α = .94.
Dissociative Experiences
The Dissociative Experiences Scale-II (DES-II) (Carlson, 1993) is a 28-item questionnaire that was used to quantify dissociative experiences. The DES-II total score is the mean of all item scores and ranges from 0 to 100. The scale is notable for its good test-retest reliability, good construct validity, and good criterion-related validity (Bernstein & Putnam, 1986; Carlson et al., 1993). The DES-II demonstrated good reliability in the current study, α = .94.
Depressive Symptoms
Depressive symptoms were measured with the Center for Epidemiologic Studies–Depression Scale (Radloff, 1977), which consists of 20 items assessing mood, somatic symptoms, and interpersonal relationships during the past 7 days on a 4-point scale based on frequency of occurrence, ranging from 0 (rarely or none of the time [less than one day]) to 3 (most or all of the time [5 to 7 days]). Following the recommendation of Kalichman et al. (Kalichman, Rompa, & Cage, 2000), we looked only at those items measuring the cognitive and affective symptoms of depression, as somatic symptoms tend to be highly correlated with HIV symptoms and may lead to inflated diagnoses of depression among individuals living with HIV. This cognitive-affective subscale ranged from 0 to 31 in the current sample. A cut-off score of 16 or greater is indicative of depression (Weissman et al., 1977). The CES-D cognitive-affective subscale demonstrated good reliability in the current study, α = .83.
Data Analysis
Predictor variables (dissociative experiences and posttraumatic stress) were analyzed as continuous variables. Antiretroviral adherence was dichotomized: patients who answered that in the last 4 days they followed their HIV medication schedule “All of the time” and also answered that they did not miss any doses of their HIV medication during the past 4 days were classified as “adherent” and coded “1.” All other subjects who completed the survey were classified as “nonadherent” and coded “0.”
Dissociation scores were positively skewed and therefore a square root transformation was performed on DES-II scores. The relationship of trauma symptoms, dissociative symptoms, and their interaction to the probability of HIV medication adherence was assessed using a hierarchical binary logistic regression analysis (Aiken & West, 1991). In the first block of the model, we entered participants’ scores on the CES-D cognitive-affective scale to control for any effect of depression symptoms on medication adherence. In the second block, we entered centered scores for both trauma symptoms and dissociation. In the third block, we entered interaction of trauma symptoms and dissociation to assess any moderating relationships between the variables. As a post hoc analysis, we parsed moderating relationships to clarify the nature of the interaction by using a median split on the moderating variable. All statistical analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, IL).
Results
Participant characteristics
Of the 43 participants who were surveyed, 38 subjects provided sufficient information to determine factors related to HIV antiretroviral adherence. A total of 32 of these subjects were males and 6 were females.
A total of 57.9% of the subjects (n=22) reported that, in the four days preceding assessment, they followed their HIV medication schedule all of the time and did not miss any HIV medication doses. These participants were classified as “adherent”, and the remaining 42.1% (n=16) of subjects were classified as “nonadherent.”
Prevalence of trauma, depression and dissociation
Overall, 44.7% (n = 17) of the sample screened positive for PTSD and 31.6% (n = 12) screened positive for depression, (21.0%, n = 8) reported co-morbid PTSD and depression. A total of 46.7% (n = 8) of participants who screened positive for PTSD reported antidepressant use. Half (50.0%, n = 6) of those screening positive for depression reported antidepressant use. For those screening positive for both PTSD and depression, 50.0% (n = 4) reported antidepressant use.
With regards to dissociation, 15.8% (n = 6) of the sample met threshold criteria for clinically significant dissociation according the DES-II, based on a cut-off score of 30 previously validated for screening of problematic dissociation (Carlson et al., 1993). Among those who met criteria for PTSD, 17.6%, (n=3) also met criteria for clinically significant dissociation. An examination of specific clusters of dissociative symptoms found that 15.8% (n = 6) of the sample reported experiencing amnestic symptoms, 23.7% (n = 9) reported experiencing symptoms of absorption, and 10.5% (n = 4) reported experiencing symptoms of depersonalization. See Table 2 for descriptive statistics of and correlations between variables of interest to the current study.
Table 2.
Bivariate correlations between adherence, PTSD, dissociative symptoms, and depression, with means (standard deviations) on the diagonal (N = 38).
| 1. | 2. | 3. | 4. | |
|---|---|---|---|---|
| 1. Adherence | 24.18 (13.11) | |||
| 2. Dissociation | −.115 | 20.58 (11.64) | ||
| 3. Impact of Events Scale - Revised: Score | −.342* | .305* | 31.61 (17.10) | |
| 4. CESD Cognitive-Affective scale | −.112 | .387* | .506** | 11.39 (6.58) |
Note:
p < .05,
p < .01
Predicting variance in HIV medication adherence
Given the high correlation between predictor variables (i.e., PTSD symptoms, dissociative symptoms), we centered all continuous predictor variables around their means before entering them into the regression model in order to reduce multicollinearity (Kraemer & Blasey, 2004).
In Block 1 of the logistic regression model, the relationship between depression and medication adherence was non-significant (OR = .98, p > .05) and the overall model was non-significant. In Block 2, the relationship between posttraumatic stress symptoms and medication adherence was significant such that greater PTSD symptoms were significantly associated with lower odds of HIV medication adherence (OR = .92, p < .05), though the overall model remained non-significant. In Block 3, when the interaction term entered the model, dissociative symptoms significantly moderated the effect of PTSD symptoms on medication adherence, resulting in lower odds of HIV medication adherence (OR = .95, p < .05). The overall model including the moderation of PTSD symptoms by dissociation was significant (Nagelkerke R2 = .35, χ2 =11.27, p < .05).
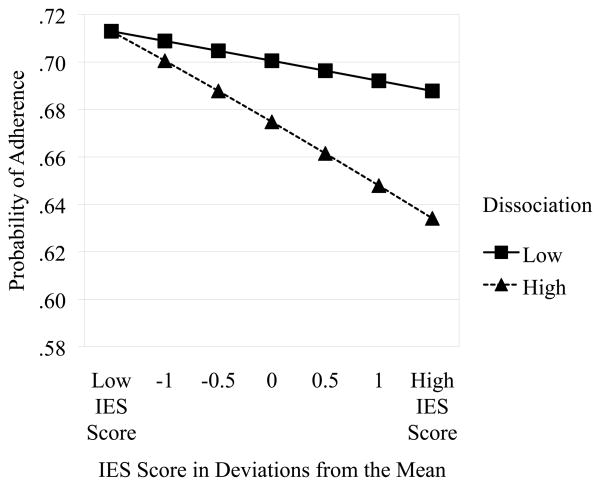
Given the significant moderating relationship found in Block 3, we parsed dissociation symptom scores into high and low categories based on a median split to better characterize the interaction. Posttraumatic stress symptoms were significantly associated with lower odds of medication adherence in individuals reporting high levels of dissociative symptoms (OR = .86, p < .05) but not in those reporting low levels of dissociative symptoms (OR = 1.02, p > .05). See Figure 1 for a graphical depiction of the moderation.
Figure 1.
Graph of Interaction Effect of Dissociation and PTSD Symptoms on Medication Adherence
Discussion
This study represents an initial examination of the relationship between PTSD, dissociative symptoms, and antiretroviral adherence among persons living with HIV/AIDS. The presence of PTSD symptoms was significantly associated with a decreased probability of HIV medication adherence, and this relationship was moderated by dissociative symptoms. Participants with high levels of dissociation showed a significant association between PTSD symptoms and lower odds of HIV medication adherence, whereas those with low levels of dissociation had no association between PTSD symptoms and adherence. To our knowledge, this is the first study to demonstrate that dissociation moderates the relationship between PTSD and adherence. We believe it is also the first study to demonstrate a relationship between dissociation and medication adherence in persons living with HIV/AIDS, or in any other patient population. A subsample of individuals who met criteria for PTSD also screened positive for clinically significant dissociation, which is consistent with the existence of a less common dissociative subtype of PTSD that is thought to involve emotional overmodulation via inhibition of limbic regions of the brain by the medial prefrontal cortex (Lanius et al., 2010). The fact that not all subjects who screened positive for PTSD also met criteria for a dissociative disorder is consistent with findings in a study showing that subjects with PTSD who also met criteria for disorders of extreme stress not otherwise specified (a diagnosis that reflects repeated traumatizations over multiple developmental stages) had greater dissociative symptomatology than subjects with PTSD alone (Zucker, Spinazzola, Blaustein, & van der Kolk, 2006).
Moreover, not all of the participants who screened positive for a dissociative disorder met criteria for PTSD. This is consistent with evidence suggesting that victims of early onset interpersonal violence who had ceased to meet criteria for PTSD still continued to exhibit symptoms of dissociation (van der Kolk et al., 1996). Thus, the experience of greater dissociation later in life, even in the absence of clinically significant PTSD, may be a hallmark of earlier psychological trauma (Bremner, 1999). It has not always been clear in previous studies if comorbid depression was in fact mediating the relationship between PTSD and adherence (Boarts et al., 2006; Delahanty et al., 2004; Sledjeski et al., 2005; Vranceanu et al., 2008). In the current study, PTSD symptoms remained a significant predictor of non-adherence even after controlling for depression.
We found evidence that PLH with depression may not be receiving adequate treatment for their psychiatric symptoms. For instance, half of the participants with clinical depression reported no current treatment with antidepressants. It is also concerning that approximately half of the subjects screening positive for depression are meeting these criteria despite already being on antidepressant therapy: nonadherence to, underdosing of, and resistance or partial responses to antidepressants are all possible explanations for this. Given the compelling evidence that depression is associated with disease progression among PLH (Leserman, 2008), it is critically important for practitioners to assess and treat depressive symptoms. Indeed, adherence to an antidepressant treatment regimen (Horberg et al., 2008) in conjunction with psychotherapy may be an effective way to enhance HIV medication adherence.
Limitations of this study include the use of self-reported medication adherence data, which can involve recall bias and be less accurate than electronic medication monitoring or pill counting strategies; however, ACASI was used to minimize response bias by enhancing reliable self report related to sensitive topics that typically pull for social desirability bias (Gribble, 1999; Tourangeau R, 1996). Moreover, while our study yielded a significant novel finding regarding the relationship of PTSD and dissociation to adherence that is consistent with the existing relevant literature, our sample size may not fully account for the variability observed in the general population of persons living with HIV/AIDS. Subsequent research needs to be conducted to replicate our findings with larger diverse samples and examine demographic and disease-related variables that may be associated with adherence and trauma, such as age, sex, and severity of HIV disease.
It is important to note that the rate of PTSD in our study sample (44.7%, n=17) was predictably higher than the 35%–36% prevalence found among PLH in other studies (Kelly, Otto-Salaj et al. 1998; Kimerling, Armistead, & Forehand, 1999a; Kimerling et al., 1999b). This was because most of our participants were recruited after they had been excluded from a separate study examining the effects of a group intervention to reduce trauma-induced stress and HIV-related risk behaviors. The prevalence for either clinical or subclinical PTSD in the recruitment sample for the group therapy intervention trial is approximately 90%, thus the vast majority of ineligible participants were not excluded from that trial based on a lack of PTSD symptoms, but rather because these individuals were not engaging in HIV-related risk behavior. Although we were targeting HIV-positive individuals with self-reported stress, our sample consists of individuals who are interested in participating in research and thus may not generalize to other HIV/AIDS populations. An additional limitation is that the study design did not allow us to determine whether the participants’ PTSD and dissociative symptoms were because of their HIV diagnosis or related to other traumatic experiences (Boarts, Buckley-Fischer, Armelie, Bogart, & Delahanty, 2009) that may have occurred either before or since the time of HIV diagnosis.
Despite the limitations, our findings have implications for the clinical management of PLH who report trauma-related symptoms, which include PTSD and dissociation. Our findings suggest that there is an important need to conduct screening and assessment of PTSD, dissociation, and depressive symptoms among PLH. Moreover, therapies that reduce trauma symptoms, including dissociative symptoms, are likely to significantly enhance adherence to HIV medications. There is substantial evidence for the effectiveness of cognitive-behavioral strategies in decreasing reactivity to stressful stimuli by increasing emotional regulation and developing adaptive coping behaviors to deal with triggers that result in PTSD or dissociative symptoms (Gore-Felton, 1999a).
Moreover, exposure-based therapy has demonstrated efficacy in the treatment of PTSD (Foa, 1997). This treatment involves repetitive exposure to stimuli associated with the original trauma in order to facilitate emotional reengagement with trauma-related memories, reduce avoidance symptoms, improve affective regulation, and increase cognitive processing of past traumatic experiences, thereby reducing intrusive thoughts and hyperarousal symptoms (Foa & Kozak, 1986; Nemeroff et al., 2006).
When PTSD occurs in conjunction with dissociative symptomatology, exposure therapy may have decreased effectiveness because of the individual’s reduced capacity to engage emotionally with trauma-associated memories (Jaycox, Foa, & Morral, 1998). Among individuals with borderline personality disorder, dissociative states have been shown to inhibit emotional, amygdala-based learning during classical conditioning by alteration of acquisition and extinction processes (Ebner-Priemer et al., 2009), and greater dissociation in this population has been related to poorer psychotherapy outcomes (Ball & Links, 2009). Taken altogether, dissociation often complicates PTSD treatment. Given our finding that dissociation moderates the relationship between PTSD and adherence, phase-based treatment, consisting of initial skills training in affective and interpersonal regulation, with subsequent coping skills to deal with triggers that activate dissociative symptoms, may enhance healthy behaviors for HIV disease management and prove to be the treatment of choice for targeting non-adherence in PLH with histories of trauma.
More research is needed that focuses on the development of effective clinical interventions that assess and target dissociative symptomatology to optimize medication adherence in the context of psychological trauma. Further research into individually-targeted strategies and psychological interventions that maximize adherence is critical for achieving optimal long-term health outcomes among PLH. As individuals with HIV and co-morbid trauma are living longer, medication adherence has important public health implications related to HIV resistance which, in turn, is associated with morbidity and mortality. Indeed, integrating mental health services into the medical management of HIV disease is likely to be an effective strategy in managing the complications of chronic, life-threatening disease.
Table 3.
Hierarchical binary logistic regression predicting variance in medication adherence from depression, PTSD symptoms, and dissociation (N = 38).
| Variable | OR (95% CI) | OR (95% CI) | OR (95% CI) |
|---|---|---|---|
| Block 1: χ2 = .48 | |||
| Depression | .98 (.92 – 1.04) | 1.02 (.94 – 1.11) | 1.04 (.89 – 1.21) |
| Block 2: χ2 = 4.63 | |||
| PTSD | .95* (.89 – .99) | .92* (.85 – .99) | |
| Dissociation | 1.12 (.65 – 1.91) | .88 (.45 – 1.70) | |
| Block 3: χ2 = 6.16* | |||
| PTSD × Dissociation | .95* (.91 – .99) |
Notes. Model χ2 = 11.27, Nagelkerke R2 = .35;
p < .05. Blocks were entered sequentially in the order shown in the table.
Acknowledgments
Role of Funding Sources
This research was supported in part by the Stanford University School of Medicine Medical Scholars Research Program (PI: Alex Keuroghlian, MD; Faculty Research Advisor: Cheryl Gore-Felton, PhD) and the National Institute of Mental Health (NIMH) grant # R01MH072386 (PI: Cheryl Gore-Felton, PhD). Both sources of funding had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
We would like to thank the patients who participated in this study. We thank Susan Sharp for recommendations related to the audio computer-assisted self interview. We also thank Evelyn Nelson, Anna Hinohara and Amy Frohnmayer who kindly assisted with the recruitment and assessment of participants.
Footnotes
Contributors
Alex S. Keuroghlian designed the study, managed the literature searches, wrote the protocol, developed the survey questionnaire, wrote the first draft of the manuscript and oversaw subsequent revisions of the manuscript. Alex S. Keuroghlian, Cheryl Gore-Felton and Charles S. Kamen undertook subsequent revisions of the manuscript. Eric Neri encoded the audio computer assisted self interview survey. Charles S. Kamen, Eric Neri and Alex S. Keuroghlian undertook the statistical analyses. Susanne Lee contributed significantly to the design of the study, developed audio files for the computer-assisted self survey and oversaw logistical aspects of recruitment and assessment of patients. Rhianon Liu contributed significantly to the design of the study. The study was conducted in Cheryl Gore-Felton’s laboratory: she contributed significantly to the design of the study, the statistical analyses, and the writing of the manuscript. All authors contributed to and have approved the final manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- Ammassari A, Antinori A, Aloisi MS, Trotta MP, Murri R, Bartoli L, Monforte AD, Wu AW, Starace F. Depressive symptoms, neurocognitive impairment, and adherence to highly active antiretroviral therapy among HIV-infected persons. Psychosomatics. 2004;45:394–402. doi: 10.1176/appi.psy.45.5.394. [DOI] [PubMed] [Google Scholar]
- Ammassari A, Murri R, Pezzotti P, Trotta MP, Ravasio L, De Longis P, Lo Caputo S, Narciso P, Pauluzzi S, Carosi G, Nappa S, Piano P, Izzo CM, Lichtner M, Rezza G, Monforte A, Ippolito G, d’Arminio Moroni M, Wu AW, Antinori A. Self-reported symptoms and medication side effects influence adherence to highly active antiretroviral therapy in persons with HIV infection. J Acquir Immune Defic Syndr. 2001;28:445–9. doi: 10.1097/00042560-200112150-00006. [DOI] [PubMed] [Google Scholar]
- Ammassari A, Trotta MP, Murri R, Castelli F, Narciso P, Noto P, Vecchiet J, D’Arminio Monforte A, Wu AW, Antinori A. Correlates and predictors of adherence to highly active antiretroviral therapy: overview of published literature. J Acquir Immune Defic Syndr. 2002;31(Suppl 3):S123–7. doi: 10.1097/00126334-200212153-00007. [DOI] [PubMed] [Google Scholar]
- Andrykowski MA, Cordova MJ. Factors associated with PTSD symptoms following treatment for breast cancer: test of the Andersen model. J Trauma Stress. 1998;11:189–203. doi: 10.1023/A:1024490718043. [DOI] [PubMed] [Google Scholar]
- APA. Diagnostic and statistical manual of mental disorders. Revised 4. Washington, DC: Author; 2000. [Google Scholar]
- Ball JS, Links PS. Borderline personality disorder and childhood trauma: evidence for a causal relationship. Curr Psychiatry Rep. 2009;11:63–8. doi: 10.1007/s11920-009-0010-4. [DOI] [PubMed] [Google Scholar]
- Bangsberg DR, Moss AR, Deeks SG. Paradoxes of adherence and drug resistance to HIV antiretroviral therapy. J Antimicrob Chemother. 2004;53:696–9. doi: 10.1093/jac/dkh162. [DOI] [PubMed] [Google Scholar]
- Belzer ME, Fuchs DN, Luftman GS, Tucker DJ. Antiretroviral adherence issues among HIV-positive adolescents and young adults. J Adolesc Health. 1999;25:316–9. doi: 10.1016/s1054-139x(99)00052-x. [DOI] [PubMed] [Google Scholar]
- Berg CJ, Michelson SE, Safren SA. Behavioral aspects of HIV care: adherence, depression, substance use, and HIV-transmission behaviors. Infect Dis Clin North Am. 2007;21:181–200. x. doi: 10.1016/j.idc.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Bernstein EM, Putnam FW. Development, reliability, and validity of a dissociation scale. J Nerv Ment Dis. 1986;174:727–35. doi: 10.1097/00005053-198612000-00004. [DOI] [PubMed] [Google Scholar]
- Boarts JM, Buckley-Fischer BA, Armelie AP, Bogart LM, Delahanty DL. The impact of HIV diagnosis-related vs. non-diagnosis related trauma on PTSD, depression, medication adherence, and HIV disease markers. J Evid Based Soc Work. 2009;6:4–16. doi: 10.1080/15433710802633247. [DOI] [PubMed] [Google Scholar]
- Boarts JM, Sledjeski EM, Bogart LM, Delahanty DL. The differential impact of PTSD and depression on HIV disease markers and adherence to HAART in people living with HIV. AIDS Behav. 2006;10:253–61. doi: 10.1007/s10461-006-9069-7. [DOI] [PubMed] [Google Scholar]
- Bremner JD. Acute and chronic responses to psychological trauma: where do we go from here? Am J Psychiatry. 1999;156:349–51. doi: 10.1176/ajp.156.3.349. [DOI] [PubMed] [Google Scholar]
- Bremner JD, Southwick S, Brett E, Fontana A, Rosenheck R, Charney DS. Dissociation and posttraumatic stress disorder in Vietnam combat veterans. Am J Psychiatry. 1992;149:328–32. doi: 10.1176/ajp.149.3.328. [DOI] [PubMed] [Google Scholar]
- Brief DJ, Bollinger AR, Vielhauer MJ, Berger-Greenstein JA, Morgan EE, Brady SM, Buondonno LM, Keane TM. Understanding the interface of HIV, trauma, post-traumatic stress disorder, and substance use and its implications for health outcomes. AIDS Care. 2004;16(Suppl 1):S97–120. doi: 10.1080/09540120412301315259. [DOI] [PubMed] [Google Scholar]
- Butler LD, Duran RE, Jasiukaitis P, Koopman C, Spiegel D. Hypnotizability and traumatic experience: a diathesis-stress model of dissociative symptomatology. Am J Psychiatry. 1996;153:42–63. doi: 10.1176/ajp.153.8.A42. [DOI] [PubMed] [Google Scholar]
- Carlson E, Putnam FW, Ross CA, Anderson G, Clark P, Torem M, Coons P, Bowman E, Chu JA, Dill D, Lowenstein RJ, Braun BG. Factor analysis of the Dissociative Experiences Scale: A multicenter study. In: Braun BG, Carlson EB, editors. Proceedings of the Eighth International Conference on Multiple Personality and Dissociative States; Chicago: Rush; 1991. [Google Scholar]
- Carlson EB, Putnam FW, Ross CA, Torem M, Coons P, Dill DL, Loewenstein RJ, Braun BG. Validity of the Dissociative Experiences Scale in screening for multiple personality disorder: a multicenter study. Am J Psychiatry. 1993;150:1030–6. doi: 10.1176/ajp.150.7.1030. [DOI] [PubMed] [Google Scholar]
- Carlson EB, Putnam FW. An update on the Dissociative Experiences Scale. Dissociation. 1993;6:16–27. [Google Scholar]
- Center for Disease Control and Prevention. HIV in the United States. 2010 Accessed at: http://www.cdc.gov/hiv/resources/factsheets/us.htm.
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, Wu AW. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12:255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Cohen MA, Alfonso CA, Hoffman RG, Milau V, Carrera G. The impact of PTSD on treatment adherence in persons with HIV infection. Gen Hosp Psychiatry. 2001;23:294–6. doi: 10.1016/s0163-8343(01)00152-9. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale - Revised. Behav Res Ther. 2003;41:1489–96. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Delahanty DL, Bogart LM, Figler JL. Posttraumatic stress disorder symptoms, salivary cortisol, medication adherence, and CD4 levels in HIV-positive individuals. AIDS Care. 2004;16:247–60. doi: 10.1080/09540120410001641084. [DOI] [PubMed] [Google Scholar]
- Deschamps AE, Graeve VD, van Wijngaerden E, De Saar V, Vandamme AM, van Vaerenbergh K, Ceunen H, Bobbaers H, Peetermans WE, de Vleeschouwer PJ, de Geest S. Prevalence and correlates of nonadherence to antiretroviral therapy in a population of HIV patients using Medication Event Monitoring System. AIDS Patient Care STDS. 2004;18:644–57. doi: 10.1089/apc.2004.18.644. [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Mauchnik J, Kleindienst N, Schmahl C, Peper M, Rosenthal MZ, Flor H, Bohus M. Emotional learning during dissociative states in borderline personality disorder. J Psychiatry Neurosci. 2009;34:214–22. [PMC free article] [PubMed] [Google Scholar]
- El-Serag HB, Kunik M, Richardson P, Rabeneck L. Psychiatric Disorders Among Veterans with Hepatitis C Infection. Gastroenterology. 2002;123:476–82. doi: 10.1053/gast.2002.34750. [DOI] [PubMed] [Google Scholar]
- Foa EB. Psychological processes related to recovery from a trauma and an effective treatment for PTSD. Ann N Y Acad Sci. 1997;821:410–24. doi: 10.1111/j.1749-6632.1997.tb48295.x. [DOI] [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: exposure to corrective information. Psychol Bull. 1986;99:20–35. [PubMed] [Google Scholar]
- Gore-Felton C, Gill M, Koopman C, Spiegel D. A review of acute stress reactions among victims of violence:Implications for early intervention. Aggression and Violent Behavior. 1999a;4:293–306. [Google Scholar]
- Gore-Felton C, Gill M, Koopman C, Spiegel D. Acute stress reactions among victims of violence: Implications for early intervention. Aggression and Violent Behavior: A Review Journal. 1999b;36:16–24. [Google Scholar]
- Gore-Felton C, Koopman C. Behavioral mediation of the relationship between psychosocial factors and HIV disease progression. Psychosom Med. 2008;70:569–74. doi: 10.1097/PSY.0b013e318177353e. [DOI] [PubMed] [Google Scholar]
- Gore-Felton C, Koopman C, Bridges E, Thoresen C, Spiegel D. An example of maximizing survey return rates. Methodological issues for health professionals. Eval Health Prof. 2002;25:152–68. doi: 10.1177/01678702025002002. [DOI] [PubMed] [Google Scholar]
- Gribble J, Miller HG, Rogers SM, Turner CF. Interview mode and measurement of sexual behaviors: Methodological issues. Journal of Sex Research. 1999;36:16–24. doi: 10.1080/00224499909551963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer SM, Saag MS, Schechter M, Montaner JS, Schooley RT, Jacobsen DM, Thompson MA, Carpenter CC, Fischl MA, Gazzard BG, Gatell JM, Hirsch MS, Katzenstein DA, Richman DD, Vella S, Yeni PG, Volberding PA. Treatment for adult HIV infection: 2006 recommendations of the International AIDS Society-USA panel. JAMA. 2006;296:827–43. doi: 10.1001/jama.296.7.827. [DOI] [PubMed] [Google Scholar]
- Haynes RB, Sackett DL, Taylor DW. How to detect and manage low patient compliance in chronic illness. Geriatrics. 1980;35:91–3. 96–7. [PubMed] [Google Scholar]
- Horberg MA, Silverberg MJ, Hurley LB, Towner WJ, Klein DB, Bersoff-Matcha S, Weinberg WG, Antoniskis D, Mogyoros M, Dodge WT, Dobrinich R, Quesenberry CP, Kovach DA. Effects of depression and selective serotonin reuptake inhibitor use on adherence to highly active antiretroviral therapy and on clinical outcomes in HIV-infected patients. J Acquir Immune Defic Syndr. 2008;47:384–90. doi: 10.1097/QAI.0b013e318160d53e. [DOI] [PubMed] [Google Scholar]
- Jaycox LH, Foa EB, Morral AR. Influence of emotional engagement and habituation on exposure therapy for PTSD. J Consult Clin Psychol. 1998;66:185–92. doi: 10.1037//0022-006x.66.1.185. [DOI] [PubMed] [Google Scholar]
- Jensen-Fangel S, Pedersen L, Pedersen C, Larsen CS, Tauris P, Moller A, Sorensen HT, Obel N. Low mortality in HIV-infected patients starting highly active antiretroviral therapy: a comparison with the general population. AIDS. 2004;18:89–97. doi: 10.1097/00002030-200401020-00011. [DOI] [PubMed] [Google Scholar]
- Johnson MO, Catz SL, Remien RH, Rotheram-Borus MJ, Morin SF, Charlebois E, Gore-Felton C, Goldsten RB, Wolfe H, Lightfoot M, Chesney MA. Theory-guided, empirically supported avenues for intervention on HIV medication nonadherence: findings from the Healthy Living Project. AIDS Patient Care STDS. 2003;17:645–56. doi: 10.1089/108729103771928708. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M. Distinguishing between overlapping somatic symptoms of depression and HIV disease in people living with HIV-AIDS. J Nerv Ment Dis. 2000;188:662–70. doi: 10.1097/00005053-200010000-00004. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Sikkema KJ, DiFonzo K, Luke W, Austin J. Emotional adjustment in survivors of sexual assault living with HIV-AIDS. J Trauma Stress. 2002;15:289–96. doi: 10.1023/A:1016247727498. [DOI] [PubMed] [Google Scholar]
- Kelly B, Raphael B, Judd F, Perdices M, Kernutt G, Burnett P, Dunne M, Burrows G. Posttraumatic stress disorder in response to HIV infection. Gen Hosp Psychiatry. 1998a;20:345–52. doi: 10.1016/s0163-8343(98)00042-5. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Otto-Salaj LL, Sikkema KJ, Pinkerton SD, Bloom FR. Implications of HIV treatment advances for behavioral research on AIDS: protease inhibitors and new challenges in HIV secondary prevention. Health Psychol. 1998b;17:310–9. doi: 10.1037//0278-6133.17.4.310. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Berglund PA, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Armistead L, Forehand R. Victimization experiences and HIV infection in women: associations with serostatus, psychological symptoms, and health status. J Trauma Stress. 1999a;12:41–58. doi: 10.1023/A:1024790131267. [DOI] [PubMed] [Google Scholar]
- Kimerling R, Calhoun KS, Forehand R, Armistead L, Morse E, Morse P, Clark R, Clark L. Traumatic stress in HIV-infected women. AIDS Educ Prev. 1999b;11:321–30. [PubMed] [Google Scholar]
- Kraemer HC, Blasey CM. Centring in regression analyses: a strategy to prevent errors in statistical inference. Int J Methods Psychiatr Res. 2004;13:141–51. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanius RA, Vermetten E, Loewenstein RJ, Brand B, Schmahl C, Bremner JD, Spiegel D. Emotion modulation in PTSD: Clinical and neurobiological evidence for a dissociative subtype. Am J Psychiatry. 2010;167:640–7. doi: 10.1176/appi.ajp.2009.09081168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehman CL, Cheung RC. Depression, Anxiety, Post-Traumatic Stress, and Alcohol-Related Problems Among Veterans With Chronic Hepatitis C. American Journal of Gastroenterology. 2002;97:2640–6. doi: 10.1111/j.1572-0241.2002.06042.x. [DOI] [PubMed] [Google Scholar]
- Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosom Med. 2008;70:539–45. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Marmar CR, Weiss DS, Schlenger WE, Fairbank JA, Jordan BK, Kulka RA, Hough RL. Peritraumatic dissociation and posttraumatic stress in male Vietnam theater veterans. Am J Psychiatry. 1994;151:902–7. doi: 10.1176/ajp.151.6.902. [DOI] [PubMed] [Google Scholar]
- Morgan CA, 3rd, Hazlett G, Wang S, Richardson EG, Jr, Schnurr P, Southwick SM. Symptoms of dissociation in humans experiencing acute, uncontrollable stress: a prospective investigation. Am J Psychiatry. 2001;158:1239–47. doi: 10.1176/appi.ajp.158.8.1239. [DOI] [PubMed] [Google Scholar]
- Nemeroff CB, Bremner JD, Foa EB, Mayberg HS, North CS, Stein MB. Posttraumatic stress disorder: a state-of-the-science review. J Psychiatr Res. 2006;40:1–21. doi: 10.1016/j.jpsychires.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, Wagener MM, Singh N. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. 2000;133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004. [DOI] [PubMed] [Google Scholar]
- Roca B, Gomez CJ, Arnedo A. Adherence, side effects and efficacy of stavudine plus lamivudine plus nelfinavir in treatment-experienced HIV-infected patients. J Infect. 2000;41:50–4. doi: 10.1053/jinf.2000.0678. [DOI] [PubMed] [Google Scholar]
- Safren SA, Gershuny BS, Hendriksen E. Symptoms of posttraumatic stress and death anxiety in persons with HIV and medication adherence difficulties. AIDS Patient Care STDS. 2003;17:657–64. doi: 10.1089/108729103771928717. [DOI] [PubMed] [Google Scholar]
- Singh N, Squier C, Sivek C, Wagener M, Nguyen MH, Yu VL. Determinants of compliance with antiretroviral therapy in patients with human immunodeficiency virus: prospective assessment with implications for enhancing compliance. AIDS Care. 1996;8:261–9. doi: 10.1080/09540129650125696. [DOI] [PubMed] [Google Scholar]
- Sledjeski EM, Delahanty DL, Bogart LM. Incidence and impact of posttraumatic stress disorder and comorbid depression on adherence to HAART and CD4+ counts in people living with HIV. AIDS Patient Care STDS. 2005;19:728–36. doi: 10.1089/apc.2005.19.728. [DOI] [PubMed] [Google Scholar]
- Spiegel D. Trauma, dissociation, and memory. Ann N Y Acad Sci. 1997;821:225–37. doi: 10.1111/j.1749-6632.1997.tb48282.x. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Cardena E. Disintegrated experience: the dissociative disorders revisited. J Abnorm Psychol. 1991;100:366–78. doi: 10.1037//0021-843x.100.3.366. [DOI] [PubMed] [Google Scholar]
- Spire B, Duran S, Souville M, Leport C, Raffi F, Moatti JP. Adherence to highly active antiretroviral therapies (HAART) in HIV-infected patients: from a predictive to a dynamic approach. Soc Sci Med. 2002;54:1481–96. doi: 10.1016/s0277-9536(01)00125-3. [DOI] [PubMed] [Google Scholar]
- Tourangeau R, ST Asking sensitive questions: The impact of data collection mode, question format, and question context. Public Opinion Quarterly. 1996;60:275–304. [Google Scholar]
- van der Kolk BA, McFarlane AC, Weisaeth L. Traumatic stress: the effects of overwhelming experience on mind, body, and society. New York: Guilford Press; 1996. [Google Scholar]
- van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: the complexity of adaptation of trauma. Am J Psychiatry. 1996;153:83–93. doi: 10.1176/ajp.153.7.83. [DOI] [PubMed] [Google Scholar]
- Vermetten E, Dorahy MJ, Spiegel D. Traumatic dissociation : neurobiology and treatment. 1. Washington, DC: American Psychiatric Pub; 2007. [Google Scholar]
- Vervoort SC, Borleffs JC, Hoepelman AI, Grypdonck MH. Adherence in antiretroviral therapy: a review of qualitative studies. AIDS. 2007;21:271–81. doi: 10.1097/QAD.0b013e328011cb20. [DOI] [PubMed] [Google Scholar]
- Vranceanu AM, Safren SA, Lu M, Coady WM, Skolnik PR, Rogers WH, Wilson IB. The relationship of post-traumatic stress disorder and depression to antiretroviral medication adherence in persons with HIV. AIDS Patient Care STDS. 2008;22:313–21. doi: 10.1089/apc.2007.0069. [DOI] [PubMed] [Google Scholar]
- Wainberg MA, Friedland G. Public health implications of antiretroviral therapy and HIV drug resistance. JAMA. 1998;279:1977–83. doi: 10.1001/jama.279.24.1977. [DOI] [PubMed] [Google Scholar]
- Weiss DS. The Impact of Event Scale: Revised. In: Wilson JP, Tang CS, editors. Cross-cultural assessment of psychological trauma and PTSD. New York: Springer; 2007. pp. 219–238. [Google Scholar]
- Weissman MM, Sholomskas D, Pottenger M, Prusoff BA, Locke BZ. Assessing depressive symptoms in five psychiatric populations: A validation study. American Journal of Epidemiology. 1977;106:203–13. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- Whetten K, Reif S, Whetten R, Murphy-McMillan LK. Trauma, mental health, distrust, and stigma among HIV-positive persons: implications for effective care. Psychosom Med. 2008;70:531–8. doi: 10.1097/PSY.0b013e31817749dc. [DOI] [PubMed] [Google Scholar]
- Yovtcheva SP, Rifai MA, Moles JK, Van Der Linden BJ. Psychiatric Comobidity Among Hepatitis C-Positive Patients. Psychosomatics. 2001;42:411–15. doi: 10.1176/appi.psy.42.5.411. [DOI] [PubMed] [Google Scholar]
- Zucker M, Spinazzola J, Blaustein M, van der Kolk BA. Dissociative symptomatology in posttraumatic stress disorder and disorders of extreme stress. J Trauma Dissociation. 2006;7:19–31. doi: 10.1300/J229v07n01_03. [DOI] [PubMed] [Google Scholar]