Abstract
A growing body of research has implicated disgust as a potential risk factor for the development and maintenance of obsessive–compulsive disorder (OCD). The first aim of the present study was to determine whether related, yet distinct, disgust vulnerabilities are endorsed more strongly by individuals with OCD than by those with another anxiety disorder. The second aim was to examine the unique contributions of changes in disgust to symptom improvement observed with exposure-based treatment for OCD. In study 1, individuals with OCD, generalized anxiety disorder (GAD), and nonclinical controls (NCCs) completed a measure of disgust propensity and disgust sensitivity. Compared to NCCs and individuals with GAD, those with OCD more strongly endorsed disgust propensity. However, individuals with OCD did not significantly differ from individuals with GAD in disgust sensitivity, although both groups reported significantly higher disgust sensitivity levels compared to NCCs. Study 2 comprised mediation analyses of symptom improvement among individuals with OCD and revealed that decreases in disgust propensity over time mediated improvement in OCD symptoms, even after controlling for improvements in negative affect. The implications of these findings for conceptualizing the role of disgust in the nature and treatment of OCD are discussed.
Keywords: Disgust, Obsessive Compulsive Disorder, Vulnerability, Mediation
Obsessive-compulsive disorder (OCD) is characterized by recurrent obsessions or compulsions that cause marked distress and interfere with daily functioning (American Psychiatric Association, 2000). Obsessions are typically defined as intrusive, repetitive thoughts, images, or impulses; and compulsions are purposeful, repetitive overt and covert behaviors or rituals performed in an effort to relieve obsessional distress. Despite recent advances in knowledge on the phenomenology of OCD (Abramowitz, et al., 2008), much remains unknown about the causal mechanisms of OCD. A growing body of research has implicated disgust proneness in the etiology and maintenance of OCD (Olatunji, et al., 2004; Schienle, et al., 2003). For example, recent research has revealed that self-report measures of disgust proneness significantly predict OCD symptoms (Olatunji et al., 2007a; Thorpe, et al., 2003). Furthermore, it has been observed that the neurocircuits involved in disgust processing may be relevant to OCD (Husted, et al., 2006). This growing body of research is in line with the notion that OCD may reflect a false contamination alarm that is mediated by disgust, not only at a basic brain level, but also in terms of the psychosocial aspects of the disorder (Stein, et al., 2001). However, this only explains the contamination obsessions and washing compulsions dimension of OCD. Although much less is known about disgust in other OCD symptom dimensions (symmetry/ordering, checking, pure obsessions), it is plausible that disgust may play a role in other OCD symptom dimensions as a byproduct of a broader emotion regulation deficit (Taylor & Liberzon, 2007).
Several studies have shown that the tendency to experience disgust predicts symptoms of OCD, even after controlling for negative affect (Mancini, et al., 2001; Thorpe et al., 2003). However, a robust association between disgust and OCD has not been consistently observed in the literature. For example, Muris, Merckelbach, Schmidt, and Tierney (1999) found that the association between disgust levels and OCD symptoms among children became nonsignificant when controlling for trait anxiety. A prior study also found that disgust levels among adult OCD patients were not significantly higher than those of patients with social phobia (Woody & Tolin, 2002). However, the psychometric properties of measures of disgust employed in such research have been questioned, and it has been proposed that the discrepant findings may partially be accounted for by differences in how vulnerabilities associated with disgust proneness are operationalized (Olatunji & Cisler, 2009). Although the earliest measures of disgust have been argued to assess ones sensitivity to disgust, such scales appear to be better operationalized as measures of ones proneness to experiencing disgust. Recently,van Overveld, de Jong, Peters, Cavanagh, and Davey (2006) identified disgust propensity and disgust sensitivity as two distinct types of disgust-based vulnerabilities. Disgust propensity is the general tendency (with may be define by both frequency and/or intensity of responding) to respond with disgust in any given situation, whereas disgust sensitivity is the overestimation of the negative consequences of experiencing disgust.
Disgust propensity may reflect a specific aspect of the general tendency to experience negative emotion. Rather than intensely experiencing disgust or experiencing disgust frequently, however, some individuals may appraise cues of disgust and the experience of disgust as threatening, and such disgust sensitivity may confer risk for OCD (Olatunji, 2010). This notion is akin to the role that anxiety sensitivity (i.e., the fear of somatic arousal; Reiss, 1991) plays in the development of panic and related disorders (Schmidt, et al., 1997; Schmidt, et al., 2006). Van Overveld and colleagues (2006) developed the Disgust Propensity and Sensitivity Scale-Revised (DPSS-R) to reliably assess the two types of disgust-based vulnerabilities, and their research has shown that disgust propensity and disgust sensitivity differentially relate to anxiety disorder symptoms. Specifically, disgust propensity was found to be a significant predictor of spider fear, whereas both disgust propensity and disgust sensitivity were significant predictors of blood fear. Disgust sensitivity has also been found to be a stronger predictor of fear of vomiting relative to disgust propensity (van Overveld, et al., 2008). Furthermore, disgust sensitivity has also been shown to demonstrate incremental validity over disgust propensity in predicting fear-relevant phobias (i.e., dog, heights), whereas disgust propensity does not appear to show incremental validity over disgust sensitivity (Fergus & Valentiner, 2009). However, recent work suggests that disgust propensity is more strongly associated with avoidance of sources of contagion than disgust sensitivity (van Overveld, et al., in press).
Although disgust propensity and disgust sensitivity appear to differ in the unique variance accounted for in predicting specific phobias (Olatunji, et al., 2007), it remains unclear how the two vulnerabilities relate to OCD. A recent study did find that whereas disgust sensitivity significantly positively correlated with only hoarding symptoms among patients with OCD, disgust propensity was significantly correlated with hoarding, neutralizing, ordering, and washing symptoms among OCD patients (Olatunji et al, 2010). The association between disgustand hoarding is particularly intriguing (and perhaps counterintuitive) and the authors speculate that this finding may reflect a more general deficit in emotion regulation/tolerance in hoarding. In general, this initial finding does suggest that disgust propensity may be more broadly associated with OCD than disgust sensitivity. The present study builds upon this work by examining the specificity of the relationship between OCD and disgust vulnerability processes. To this end, individuals with OCD were compared to those with generalized anxiety disorder (GAD) and nonclinical controls with respect to their responses on the DPSS-R (Study 1). It was hypothesized that individuals with OCD would report higher levels of disgust propensity and disgust sensitivity than those with GAD and NCCs.
A second aim of this study was to examine the extent to which disgust vulnerability plays a role in OCD symptom improvement observed with treatment. Exposure and response prevention has been shown to reduce disgust responses among those with OCD (McKay, 2006), but it is not clear whether these observed changes account for OCD symptom improvement. Indeed, to the extent that disgust vulnerabilities underlie OCD, one would expect that changes in disgust vulnerabilities during treatment would account for changes in OCD symptoms during treatment. In addressing this mediational hypothesis, we focused on disgust vulnerability processes (e.g., disgust propensity, disgust sensitivity) specific to OCD. That is, as potential mediators, we only selected disgust vulnerability variables that had been shown to be specific to OCD in Study 1. To further test for specificity, we evaluated whether the mediational effect of disgust vulnerability decline would remain significant after controlling for a plausible rival change mechanism, namely improvements in negative affect. To test these hypotheses, we administered measures of disgust vulnerability before and after exposure-based treatment to an independent sample of treatment-seeking adults with OCD.
Study 1: Method & Materials
Sample Characteristics
Participants consisted of 30 adults with a diagnosis of GAD, 30 with OCD, and 30 NCCs with no history of an Axis 1 disorder. OCD participants, who mostly (37%) expressed contamination obsessions and washing compulsions, were recruited mainly from the Obsessive Compulsive Disorder/Tourette Syndrome Program at Vanderbilt University. GAD and NCC participants were recruited from community advertisements or referral from the Vanderbilt Adult Psychiatry Outpatient Clinic. The Structured Clinical Interview for the DSM–IV (SCID-IV; First, et al., 1997) was administered by a trained clinical psychologist to confirm diagnosis for all participants with exclusionary criteria for all groups including a diagnosis of bipolar disorder, substance abuse, ADHD, pervasive developmental disorders, mental retardation, or current or past central nervous system diseases; also, inclusionary criteria for the clinical groups could not overlap (i.e., OCD participants could not have history or current GAD diagnosis). Institutional review board (IRB) approval (Vanderbilt University) was obtained for procedures and all patients gave their written informed consent. Participants were seated at a computer where they completed the self-report questionnaires as part of a larger study on information processing. Table 1 presents demographic information for the participants in each diagnostic group. The groups did not significant differ on age, gender, ethnicity, and education. However, the groups did differ in marital status (χ2 = 10.84, p < .03), with significantly more married participants in the GAD group compared to those with OCD and NCCs.
Table 1.
Demographic characteristics by diagnostic group
| OCD | GAD | NCC | |
|---|---|---|---|
| N | 30 | 30 | 30 |
| Age | 39.23 (11.91) | 38.63 (11.26) | 39.50 (10.29) |
| % female | 50 | 50 | 50 |
| % Caucasian | 96.7 | 86.7 | 73.3 |
| % Married | 30.0 | 65.5 | 30.0 |
| % College Degree | 43.3 | 37.9 | 46.6 |
Note: OCD = Obsessive-compulsive disorder; GAD = Generalized-anxiety disorder; NCC = Non-clinical control.
Measures
The Obsessive-Compulsive Inventory-Revised (OCI-R; Foa et al., 2002) is an 18-item measure of OCD symptoms. Participants rate the degree to which they are bothered or distressed by OCD symptoms in the past month on a 5-point scale from 0 = “Not at all” to 4 = “Extremely”. The OCI-R assesses six types of OCD symptoms: Washing concerns (M = 4.43, SD = 4.03), Checking/Doubting (M = 4.73, SD = 3.36), Obsessing (M = 7.46, SD = 3.33), Mental Neutralizing (M = 3.03, SD = 3.65), Ordering (M = 4.73, SD = 3.99), and Hoarding (M = 4.33, SD = 4.22). The OCI-R had good internal consistency in the present study (α = .92).
The Beck Depression Inventory (BDI, Beck, et al., 1996) is a 21-item self-report measure rated on a 4-point Likert scale that ranges from 0 to 3 with higher scores representing more severe levels of depressive symptoms or dysphoria. The BDI had good internal consistency in the present study (α = .91).
The Disgust Propensity and Sensitivity Scale-Revised (DPSS-R; van Overveld et al., 2006) is a 16-item measure designed to assess the general tendency to respond with the emotion of disgust (Disgust Propensity) and the overestimation of the negative impact of experiencing disgust (Disgust Sensitivity). Subjects rate their agreement with the each item on a scale ranging from 1 (“never”) to 5 (“always”). The DPSS-R had good internal consistency in the present study (α = .88).
Results
Distinction between Diagnostic Groups
As shown in Table 2, a univariate Analysis of Variance (ANOVA) revealed a significant difference among the three groups in OCD symptoms as assessed with the OCI-R [F (2, 86) = 28.62, p < .001]. Follow-up tests showed that patients with OCD and GAD scored significantly higher than did NCCs on the OCI-R (p < .001). Patients with OCD also scored significantly higher than those with GAD on the OCI-R (p < .001). A significant difference among the three groups in depression symptoms, as assessed with the BDI, was also found [F (2, 86) = 19.05, p < .001]. Follow-up tests showed that patients with OCD and GAD scored significantly higher than did NCCs on the BDI (p < .001). However, patients with OCD did not significantly differ from those with GAD in symptoms of depression (p > .05).
Table 2.
Symptom characteristics by diagnostic group
| OCD | GAD | NCC | F | Partial η2 | |
|---|---|---|---|---|---|
| OCI-R | 28.73 (13.55)a | 19.69 (12.51)b | 6.63 (1.39)c | 28.62* | .40 |
| BDI | 16.53 (10.20)a | 15.45 (8.55)a | 4.77 (4.70)b | 19.05* | .31 |
| DPSS-R: Propensity | 15.33 (5.36)a | 12.45 (3.69)b | 11.33 (2.89)b | 7.54* | .15 |
| DPSS-R: Sensitivity | 11.80 (6.57)a | 11.14 (5.77)a | 6.00(3.21)b | 10.44* | .19 |
Note:
p < .001;
OCD = Obsessive Compulsive Disorder; GAD = Generalized Anxiety Disorder; NCC = Nonclinical Control; OCI-R = Obsessive Compulsive Inventory-Revised; BDI = Beck Depression Inventory; DPSS-R = Disgust Propensity and Sensitivity Scale-Revised. Values with difference subscripts are significantly different from each other.
Specificity of Disgust Vulnerability
A 3 (Group; OCD, GAD, NCC) X 2 (DPSS-R subscales) mixed model ANOVA yielded a significant main effect of Group [F (2, 86) = 9.98, p < .001, partial η2 = .18] and DPSS-R subscales [F (1, 86) = 58.07, p < .001, partial η2 = .40]. These main effects were qualified by a significant Group X DPSS-R subscales interaction [F (2, 86) = 6.78, p < .01, partial η2 = .14]. The Group X DPSS-R subscale interaction remained significant when the BDI was entered as a covariate [F (2, 85) = 4.32, p < .02, partial η2 = .09]. Post hoc one-way ANOVAs showed a significant difference among the three groups on both DPSS-R subscales. Bonferroni-corrected follow-up tests showed that patients with OCD (p < .001) and GAD (p < .001) scored significantly higher than did NCCs on Disgust Sensitivity. However, Table 2 shows that patients with OCD did not significantly differ from those with GAD in Disgust Sensitivity (p > .05). In contrast, patients with OCD scored significantly higher than those with GAD on Disgust Propensity (p < .01), yet patients with GAD did not significantly differ from NCCs in Disgust Propensity (p > .05). These findings remained unchanged when controlling for marital status.
Discussion
Contrary to predictions, OCD and GAD patients did not significantly differ from each other in disgust sensitivity, although both patient groups reported significantly higher disgust sensitivity levels compared to NCCs. Furthermore, the effect size for the OCD and GAD comparison in disgust sensitivity was rather small (partial η2 = .003). In contrast, disgust propensity, the general tendency to respond with disgust, was endorsed more strongly by patients with OCD compared to NCCs and those with GAD. This finding suggests that unlike disgust sensitivity, disgust propensity is uniquely associated with OCD relative to GAD. However, it is unclear if disgust propensity is also specifically associated with OCD treatment outcome. Accordingly, Study 2 examines if changes in OCD symptoms during exposure-based treatment is mediated by changes in disgust propensity independent of changes in negative affect.
Study 2: Method & Materials
Sample Characteristics
An independent sample of 40 (21 males) participants with a diagnosis of OCD in an intensive outpatient anxiety disorder treatment program participated in the present study. Diagnoses were based upon the Mini International Neuropsychiatric Interview (MINI; Sheehan et al., 1998). The MINI is a structured clinical interview used to assess 17 Axis I disorders. The MINI was administered by trained and certified master- and doctoral-level clinicians. IRB approval was obtained for procedures and all patients gave their written informed consent. The mean age of the sample was 26.38 (SD = 13.58) and included mostly Caucasians (95%) and individuals who were never married (75%). Income varied with 22.5% (N = 9) reporting less than $40,000 annual income, 17.5% (N = 7) reporting between $40,000 – $65,000 annual income, and 52.5% (N = 21) reporting over $65,000 annual income (N = 1 unreported). Educational attainment also varied with 45% (N = 18) reporting a high school diploma or less, 15% (N = 6) reporting some vocational school or college, 22.5% reporting completion of a vocational degree or a four year college degree, and 7.5% (N = 3) reporting some graduate school or a graduate degree (N = 1 unreported).
Procedures
Participants completed pencil-and-paper questionnaires at the time of their initial assessments (i.e., pre-treatment). They also completed questionnaires at the time of termination (i.e., during or just before the final treatment session; post-treatment). The treatment program took place four days per week, for three-and-a-half hours each day, and the typical length of stay in the program was between two and three weeks. Treatment included some psychoeducation and general cognitive therapy, but the primary activity was exposure and response prevention.
Measures
The OCI-R described in Study 1. Pre-treatment symptom dimensions are as follows: Washing concerns (M = 3.56, SD = 3.88), Checking/Doubting (M = 4.74, SD = 4.20), Obsessing (M = 8.02, SD = 3.64), Mental Neutralizing (M = 3.91, SD = 4.11), Ordering (M = 5.04, SD = 3.70), and Hoarding (M = 3.45, SD = 3.18).
The BDI and DPSS-R described in Study 1. The Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988) assesses 21 common symptoms of clinical anxiety (e.g., sweating, fear of losing control). Respondents indicate the degree to which they have recently been bothered by each symptom during the past week on a 4-point scale from 0 = “Not at all” to 4 = “Severely”. The internal consistency (Alpha) of these scales at pre and post-treatment are presented in Table 3. For the present study, negative affect (NA) was operationalized as a composite of the standardized BAI and BDI scores (see Park et al., 2009).
Table 3.
Pre and post-treatment means, standard deviations, alphas, and correlations of the standardized symptom variables (across time points)
| Measure | BDI | DPSS-R: Propensity | OCI-R | Pre M (SD) | Post M (SD) | Pre Alpha | Post Alpha |
|---|---|---|---|---|---|---|---|
| BAI | .59* | .30* | .43* | 24.99 (14.07) | 12.48 (8.61) | .89 | .85 |
| BDI | - | .40* | .51* | 22.02 (12.39) | 7.84 (5.83) | .90 | .78 |
| DPSS-R: Propensity | - | - | .61* | 12.17 (5.49) | 9.45 (5.09) | .85 | .91 |
| OCI-R | - | - | - | 28.74 (15.62) | 15.12 (13.35) | .90 | .93 |
Note: First three columns represent correlations; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; DPSS-R = Disgust Propensity and Sensitivity Scale-Revised; OCI-R = Obsessive-Compulsive Inventory – Revised;
p < .01
Data Analytic Overview
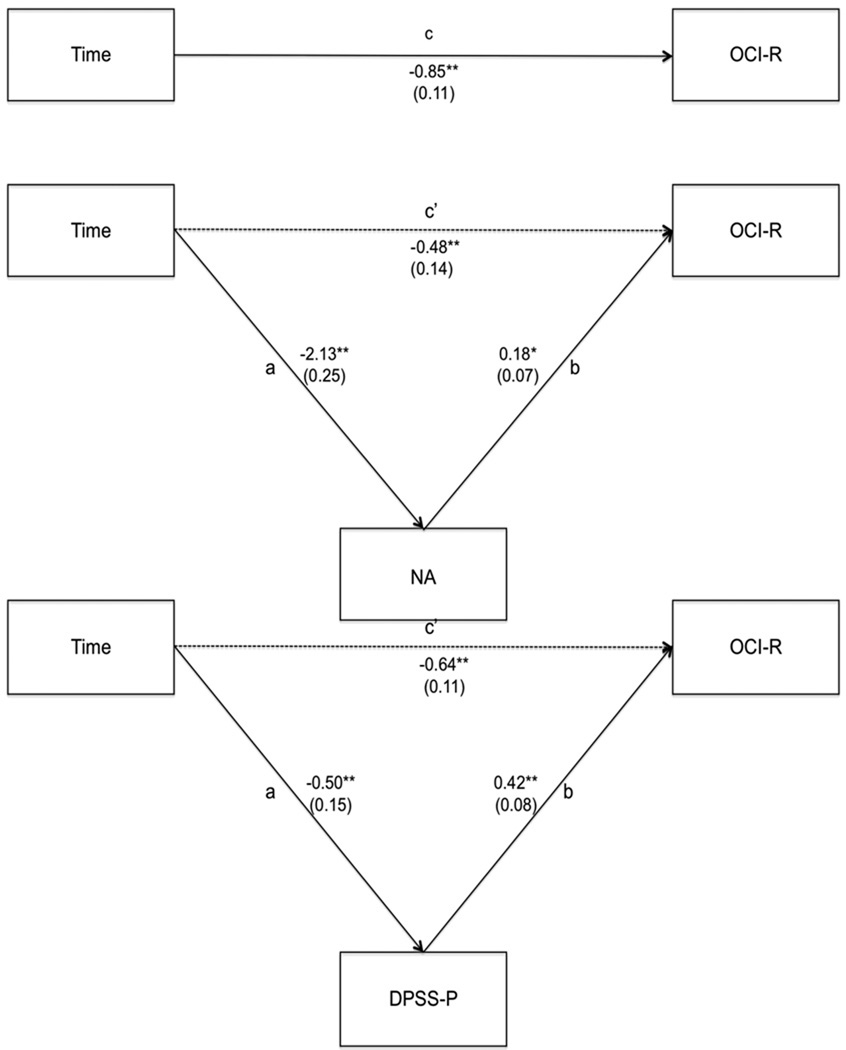
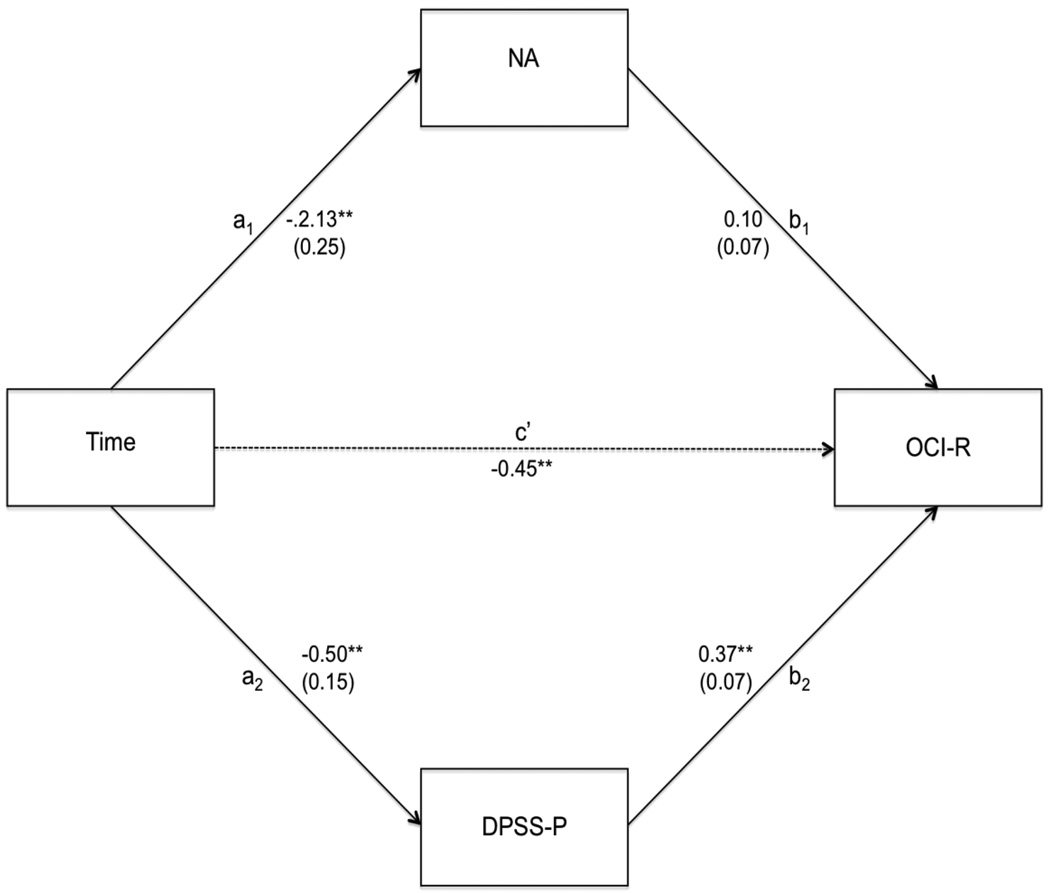
In order to test the study hypotheses, a multilevel mediation framework (MacKinnon, 2008) using version 6 of the software program Hierarchical Linear and Nonlinear Modeling (HLM; Raudenbush, et al., 2004) was employed. HLM is preferred for the analysis of longitudinal data as it permits the examination of relationships over time both within the individual (Level 1) as well as between individuals (Level 2). Here, lower level data (i.e., Level 1 data) were comprised of repeated measures of negative affect (NA), disgust propensity, and OCD symptoms (OCI-R); these were nested within individuals (Level 2). Using this framework, the extent to which reductions over time in the mediators (NA and disgust propensity) accounted for the reductions over time in the outcome variable, OCI-R (see Figures 1 and 2) was examined. The mediators were first tested individually (see Figure 1) and then simultaneously (see Figure 2). As such, the tested models were:
c (total effect) path: Yij (OCI-R) = β0j + β1j (Time) +eij
a (IV predicts mediator) path: Yij (mediator) = β0j + β1j (Time) +eij
b (Mediator predicts DV) & c’ (direct effect) paths (single mediator): Yij (OCI-R) = β0j + β1j (Time) + β2j (mediator 1&2) +eij
b & c’ paths (two mediators): Yij (OCI-R) = β0j + β1j (Time) + β2j (mediator1) + β3j (mediator2) +eij
Figure 1.
Negative affect (NA) and disgust propensity (DPSS-P) as individual mediators of obsessive-compulsive symptom (OCI-R) change over time. Note: *p < .05; **p < .01.
Figure 2.
Negative affect (NA) and disgust propensity (DPSS-P) as simultaneous mediators of obsessive-compulsive symptom (OCI-R) change over time. Note: **p < .01.
In order to facilitate the interpretation of our results, all variables were standardized across time points (z-scores) and Time was centered at pre-treatment (0 = pre-treatment, 1 = post-treatment). To test the significance of the mediated pathways, the distribution of products test (MacKinnon, et al., 2007; MacKinnon, et al., 2002) was employed. The distribution of products test calculates the magnitude of the joint mediated pathway (the a– pathway) by multiplying the regression coefficients of the two segments of the mediated pathway (i.e., a*b) and then calculates the 95% confidence interval (CI) for this product; CI’s that do not include 0 indicate a significant mediated pathway (MacKinnon, et al., 2004). The distribution of products test has demonstrated greater power and more accurate Type I error rates (MacKinnon et al., 2007; MacKinnon et al., 2002) than the causal steps approach (e.g., Baron & Kenny, 1986) and has virtually the same power as bias-corrected bootstrapping with lower Type I error rates (MacKinnon et al., 2004). It also has the advantage of being exactly replicable, which is not the case for bootstrapping (MacKinnon et al., 2004).
Results
Negative Affect and Disgust Propensity as Singular Mediators of OCD Symptom Change
Means, standard deviations, and correlations between the study variables are presented in Table 3. The extent to which changes over time in NA and DPSS-P (disgust propensity) each individually mediated changes in OCI-R was first examined. As can be seen in Figure 1, scores on the OCI-R significantly declined over time (i.e., the c path; b = −0.85, p < .01), as did NA (b = −2.02, p < 0.01) and scores on the DPSS-P (b = − 0.50, p < 0.01; i.e., a paths; see Figure 1). Likewise, changes in NA (b = 0.18, p < 0.05) and scores on the DPSS-P (b = 0.42, p < 0.01) were each associated with changes in OCI-R scores (i.e., b paths; see Figure 1). As indicated by the 95% CI of the a*b products, the joint mediated pathways for NA and OCI-R (a*b = −0.38, 95% CI [−0.70, −0.09], p < 0.05) and DPSS-P and OCI-R (a*b = -0−.21, 95% CI [−0.37, −.08], p < 0.05) were each significant.
Negative Affect and Disgust Propensity as Simultaneous Mediators of OCD Symptom Change
The extent to which both NA and DPSS-P predicted unique variance in OCI-R reductions over and above what was predicted by each mediator was then examined. This was tested by entering both mediators simultaneously into the model. As can be seen in Figure 2, changes in DPSS-P scores were associated with changes in OCI-R scores (b = 0.37, p < 0.01). However, changes in NA were no longer associated with changes in OCI-R scores (b = 0.10, n.s.). These results were reflected in the distribution of products tests; the 95% confidence interval of the joint mediated pathway for DPSS-P and OCI-R symptoms was significant (a*b = −0.18, 95% CI [−0.32, −0.07], p < 0.05), but not significant for NA and OCI-R symptoms (a*b = −0.21, 95% CI [−0.52, 0.08], n.s.).
Discussion
The findings of Study 2 show that changes in disgust propensity and negative affect each account for meaningful changes in symptoms during treatment among patients with OCD. Examination of negative affect and disgust propensity as simultaneous predictors of reductions in OCD symptoms revealed that disgust propensity was associated with symptom changes but changes in negative affect were no longer associated with changes in OCD symptoms. These findings provide some evidence for the specificity in the mediational effects of disgust propensity with respect to OCD symptom improvement during exposure-based treatment.
General Discussion
Several lines of evidence suggest that the tendency to experience disgust may play a role in the development and maintenance of OCD (Cisler, et al., 2009; Olatunji, et al., 2010). However, it is unclear if the disgust vulnerability that may give rise to OCD is best characterized by disgust propensity or disgust sensitivity. Furthermore, before causality can be inferred between disgust and OCD, it is necessary (but certainly not sufficient) to show that OCD patients endorse disgust propensity and/or disgust sensitivity more strongly than do patients with other anxiety disorders (specificity). The findings of Study 1 were partially consistent with this hypothesis. Compared to NCCs and those with GAD, OCD patients more strongly endorsed disgust propensity. However, OCD and GAD patients did not significantly differ from each other in disgust sensitivity, although both patient groups reported significantly higher disgust sensitivity levels compared to NCCs. These findings suggest that disgust propensity may have a more robust relationship with OCD than disgust sensitivity.
The finding that disgust sensitivity did not differentiate OCD patients from those with GAD may indicate that the overestimation of the negative consequences of experiencing disgust is related more to anxiety disorders in general than to OCD. In fact, recent research has shown that disgust sensitivity is more closely associated with anxiety sensitivity (Fergus & Valentiner, 2009), a risk factor for a wide range of a psychological disorders (Olatunji & Wolitzky-Taylor, 2009). Among those with OCD, disgust propensity may be a better diagnostic (and perhaps prognostic) indicator than disgust sensitivity. The finding of the specificity of disgust propensity to OCD also suggests that disgust-related vulnerabilities may be distinct. That is, disgust propensity and disgust sensitivity may have non-overlapping attributes that differentially confer risk for the development of psychopathology. It has been proposed that disgust propensity may be a specific form of negative affect whereas disgust sensitivity represents a more specific form of interoceptive intolerance (Olatunji et al., 2010), though empirical evidence supporting this distinction is currently absent. Future research is clearly needed to delineate how disgust propensity and disgust sensitivity differ from each other and the mechanism(s) that account for their differential association with OCD.
Although the findings from Study 1 support a unique role for disgust propensity in OCD, a stronger relationship between disgust propensity and OCD would be demonstrated if two patterns were observed: first, that change in disgust propensity accounted for meaningful change in OCD symptoms during treatment (mediation); second, that change in disgust propensity accounted for change in OCD symptoms during treatment independent of change in negative affect (specificity). Despite the large body of evidence implicating disgust in OCD (Olatunji et al., 2010), no study to date has examined if individual differences in disgust proneness underlies symptom improvement in OCD. An initial step was taken to address this important gap in the literature in Study 2 by examining a mediational model that assumes that one variable, the independent variable (Time), causes the intervening variable (reduction in disgust propensity), which in turn causes the dependent variable (reduction in OCD symptoms) in a sample of patients with OCD.
The findings of Study 2 revealed significant reductions in OCD symptoms, disgust propensity, and negative affect after exposure-based treatment. Although prior research has shown that trait disgust proneness remains unchanged after exposure-based treatment (de Jong, et al., 1997), these findings suggest that the general tendency to respond with disgust can be effectively reduced with exposure-based treatment for OCD. The findings of Study 2 also revealed that changes in disgust propensity and negative affect during treatment were each associated with changes in OCD symptoms during treatment. Habituation is hypothesized to be necessary for successful outcome during exposure therapy (Foa & Kozak, 1986). Reductions in negative affect may account for change in OCD symptoms by facilitating habituation and increasing motivation for treatment (Abramowitz, et al., 2000). However, prior research has found significant positive associations between negative affect and disgust propensity (Olatunji et al., 2007b). This suggests that changes in disgust propensity may be associated with changes in OCD symptoms as an artifact of its association with changes in negative affect during treatment. Yet, the present study showed that, when examining both negative affect and disgust propensity as mediators, changes in disgust propensity continued to be significantly associated with changes in OCD symptoms.
The findings of Study 2 also showed that the significant association between changes in negative affect and changes in OCD symptoms during treatment was no longer significant when controlling for changes in disgust propensity. One interpretation of these findings is that although change in negative affect accounts for change in OCD symptoms during treatment, this process is accounted for by change in disgust propensity. However, because study 2 did not employ an experimental design and included only two time points, inferences with respect to the direction of the relationship between negative affect and disgust propensity cannot be made. Although much of the literature on disgust in OCD has been aimed at the contamination subtype, these findings also highlight the need to further examine and explain the role of disgust in OCD more broadly. Prior research has shown that the association between disgust and OCD symptoms is more robust for contamination obsessions and washing compulsions (Tolin, Woods, & Abramowitz, 2006). However, research has also found that disgust significantly correlates with OCD symptoms of checking, doubting, ordering, obsessing, and neutralizing (Thorpe et al., 2003). Although the avoidance of disease may account for the role of disgust in the contamination fear (Olatunji et al., 2004), it is unclear why disgust would lead to the development of other OCD subtypes. Disgust may be important in the initial occurrence of symptoms of other OCD subtypes but play a minimal role in the distress associated with the symptom. In contrast, disgust may emerge as an artifact of the distress associated with symptoms of other OCD subtypes but is irrelevant to the initial occurrence of such symptoms.
The present findings suggest that disgust propensity and disgust sensitivity differentially relate to OCD, and the development of the DPSS-R may facilitate future research aimed at describing the mechanisms that define and discriminate the two vulnerabilities. The present study does suggest that disgust propensity, but not disgust sensitivity, is more strongly related to OCD. However, replication and extension of these findings with the DPSS-R among patients with OCD, perhaps with an experimental, or at least a longitudinal research design, may allow for more definitive casual inferences to be made. Replication of this work in larger samples that allows for discrimination of this pattern of findings among patients with different OCD subtypes will also prove to be informative. The present study is also limited by exclusive reliance on self-report measures. Development and implementation of behavioral measures of disgust propensity and disgust sensitivity in future research along these lines is clearly warranted. In addition, this work can be extended by examining whether the specific association between disgust propensity and OCD observed in the present study would be observed in comparison to a broader range of psychopathology.
The specific association between disgust propensity and OCD was also supported when examining treatment changes. Given that causal inferences cannot be made based on this investigation, one interpretation of the present findings is that disgust propensity and OCD symptoms may have a reciprocal relationship during the course of treatment. In this reciprocal process, disgust propensity and OCD symptoms may interact in a manner in which each one influences the experience of the other. Although one conclusion is that OCD symptoms improve during exposure-based treatment because disgust propensity is reduced, research that assesses symptoms at multiple time points during treatment is needed to test for these potential causal and reciprocal effects. Here, we should also note that the observed mediating effects in the present study do not specifically speak to treatment as the cause of change. Without a control condition, the findings may indicate how treatment results in change if treatment is the causative agent; if not, they simply provide an explanation of how changes in disgust propensity (and negative affect) relate to change in OCD symptoms over time. Accordingly, the inclusion of a treatment control condition in future research would help determine whether the change mechanisms are specific to exposure-based treatment. Research along these lines may further clarify the role of disgust in the nature and treatment of OCD.
Acknowledgement
None.
Role of Funding Source
Funding for this study was supported in part by NIMH Grant RO3MH082210-01A1; the NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
All authors declare that they have no conflicts of interest.
Contributors
B. Olatunji designed the study, analyzed data, and wrote first draft of the manuscript.
C. Tart assisted with the design of the study, data analysis, and preparation of the manuscript.
B. Ciesielski assisted with data collect, data analysis, and preparation of the manuscript.
P. McGrath assisted with data management and processing.
J. Smits assisted with the design of the study, data analysis, and preparation of the manuscript.
References
- Abramowitz JS, Franklin ME, Kozak MJ, Street GP, Foa EB. The effects of pretreatment depression on cognitive-behavioral treatment outcome in OCD clinic patients. Behavior Therapy. 2000;31:517–528. [Google Scholar]
- Abramowitz JS, McKay D, Taylor S. Obsessive-compulsive disorder: Subtypes and spectrum conditions. Amsterdam: Elsevier; 2008. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders 4th Edition-Text Revision. Washington DC: Author; 2000. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory. 2nd ed. San Antonio TX: The Psychological Corporation; 1996. [Google Scholar]
- Berle D, Phillips ES. Disgust and obsessive-compulsive disorder: An update. Psychiatry. 2006;69:228–238. doi: 10.1521/psyc.2006.69.3.228. [DOI] [PubMed] [Google Scholar]
- Cisler JM, Olatunji BO, Lohr JM. Disgust fear and the anxiety disorders: a critical review. Clinical Psychology Review. 2009;29:34–46. doi: 10.1016/j.cpr.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong P, Andrea H, Muris P. Spider phobia in children: disgust and fear before and after treatment. Behaviour Research and Therapy. 1997;35:559–562. doi: 10.1016/s0005-7967(97)00002-8. [DOI] [PubMed] [Google Scholar]
- Fergus TA, Valentiner DP. The Disgust Propensity and Sensitivity Scale – Revised: Further examining its factor structure and representational validity. Journal of Anxiety Disorders. 2009;23:703–710. doi: 10.1016/j.janxdis.2009.02.009. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV Axis I disorders. Washington DC: American Psychiatric Association; 1997. [Google Scholar]
- Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, Salkovskis PM. The Obsessive-Compulsive Inventory: Development and Validation of a Short Version. Psychological Assessment. 2002;14:485–496. [PubMed] [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Husted DS, Shapira NA, Goodman WK. The neurocircuitry of obsessive-compulsive disorder and disgust. Progress in NeuroPsychopharmacology and Biological Psychiatry. 2006;30:389–399. doi: 10.1016/j.pnpbp.2005.11.024. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Reviews in Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Williams J. Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research. 2004;39:99–128. doi: 10.1207/s15327906mbr3901_4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mancini F, Gragnani A, D’Olimpio F. The connection between disgust and obsessions and compulsions in a non-clinical sample. Personality and Individual Differences. 2001;31:1173–1180. [Google Scholar]
- McKay D. Treating disgust reactions in contamination-based obsessive-compulsive disorder. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:53–59. doi: 10.1016/j.jbtep.2005.09.005. [DOI] [PubMed] [Google Scholar]
- Muris P, Merckelbach H, Schmidt H, Tierney S. Disgust sensitivity trait anxiety and anxiety disorders symptoms in normal children. Behaviour Research and Therapy. 1999;37:953–961. doi: 10.1016/S0005-7967(99)00045-5. [DOI] [PubMed] [Google Scholar]
- Olatunji BO. Change in disgust corresponds with change in symptoms of contamination-based OCD: A prospective examination of specificity. Journal of Anxiety Disorders. 2010;24:313–317. doi: 10.1016/j.janxdis.2010.01.003. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM. Disgust sensitivity: psychometric overview and operational definition. In: Olatunji BO, McKay D, editors. Disgust and it’s Disorders: Theory Assessment and Treatment. Washington DC: APA; 2009. pp. 31–56. [Google Scholar]
- Olatunji BO, Cisler JM, Deacon B, Connolly K, Lohr JM. The Disgust Propensity and Sensitivity Scale-Revised: Psychometric properties and specificity in relation to anxiety disorder symptoms. Journal of Anxiety Disorders. 2007b;21:918–930. doi: 10.1016/j.janxdis.2006.12.005. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, McKay D, Phillips M. Is disgust associated with psychopathology? Emerging research in the anxiety disorders. Psychiatry Research. 2010;175:1–10. doi: 10.1016/j.psychres.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Moretz M, Wolitzky-Taylor KB, McKay D, McGrath P, Ciesielski B. Disgust vulnerability and symptoms of contamination-based OCD: Descriptive tests of incremental specificity. Behavior Therapy. 2010;41:475–490. doi: 10.1016/j.beth.2009.11.005. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Sawchuk CN, Lohr JM, de Jong PJ. Disgust domains in the prediction of contamination fear. Behaviour Research and Therapy. 2004;42:93–104. doi: 10.1016/s0005-7967(03)00102-5. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Williams N, Lohr JM, Connolly K, Cisler J, Meunier S. Structural differentiation of disgust from negative affectivity in the prediction of specific anxiety disorder symptoms. Behaviour Research and Therapy. 2007a;45:3002–3017. doi: 10.1016/j.brat.2007.08.011. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Williams NL, Lohr JM, Sawchuk CN. The structure of disgust: Domain specificity in relation to contamination ideation and excessive washing. Behaviour Research and Therapy. 2005;43:1069–1086. doi: 10.1016/j.brat.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Wolitzky-Taylor KB. Anxiety sensitivity and the anxiety disorders: A meta-analytic review and synthesis. Psychological Bulletin. 2009;135:974–999. doi: 10.1037/a0017428. [DOI] [PubMed] [Google Scholar]
- Park ER, Chang Y, Quinn V, Regan D, Cohen L, Viguera A, Psaros C, Ross K, Rigotti N. The association of depressive anxiety and stress symptoms and postpartum relapse to smoking: A longitudinal study. Nicotine and Tobacco Research. 2009;11:707–714. doi: 10.1093/ntr/ntp053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Congdon R. HLM 6 for Windows Computer software. Lincolnwood IL: Scientific Software International Inc; 2004. [Google Scholar]
- Reiss S. Expectancy theory of fear anxiety and panic. Clinical Psychology Review. 1991;11:141–153. [Google Scholar]
- Schienle A, Stark R, Walter B, Vaitl D. The connection between disgust sensitivity and blood-related fears faintness symptoms and obsessive-compulsiveness in a non-clinical sample. Anxiety Stress and Coping. 2003;16:185–193. [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatry Research. 2006;40:691–699. doi: 10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T, Baker R, Dunbar GC. The Mini-International Neuropsychiatric Interview MINI: the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–33. [PubMed] [Google Scholar]
- Stein DJ, Liu Y, Shapira NA, Goodman WK. The psychobiology of obsessive-compulsive disorder: How important is disgust? Current Psychiatry. 2001;3:281–287. doi: 10.1007/s11920-001-0020-3. [DOI] [PubMed] [Google Scholar]
- Taylor S, Liberzon I. Neural correlates of emotion regulation in psychopathology. Trends in Cognitive Sciences. 2007;11:413–418. doi: 10.1016/j.tics.2007.08.006. [DOI] [PubMed] [Google Scholar]
- Thorpe SJ, Patel SP, Simonds LM. The relationship between disgust sensitivity anxiety and obsessions. Behaviour Research and Therapy. 2003;41:1397–1409. doi: 10.1016/s0005-7967(03)00058-5. [DOI] [PubMed] [Google Scholar]
- Tolin DF, Woods CM, Abramowitz JS. Disgust sensitivity and obsessive-compulsive symptoms in a nonclinical sample. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:30–40. doi: 10.1016/j.jbtep.2005.09.003. [DOI] [PubMed] [Google Scholar]
- van Overveld M, de Jong PJ, Peters ML, Cavanagh K, Davey GCL. Disgust propensity and disgust sensitivity: Separate constructs that are differentially related to specific fears. Personality and Individual Differences. 2006;41:1241–1252. [Google Scholar]
- van Overveld M, de Jong PJ, Peters ML, Van Hout WJPJ, Bouman TK. An internet-based study on the relation between disgust sensitivity and emetophobia. Journal of Anxiety Disorders. 2008;22:524–532. doi: 10.1016/j.janxdis.2007.04.001. [DOI] [PubMed] [Google Scholar]
- van Overveld M, de Jong PJ, Peters M. The Disgust Propensity and Sensitivity Scale – Revised: Its predictive value for avoidance behavior. Personality and Individual Differences. in press. [Google Scholar]
- Woody SR, Tolin DF. The relationship between disgust sensitivity and avoidant behavior: Studies of clinical and nonclinical samples. Journal of Anxiety Disorders. 2002;16:543–559. doi: 10.1016/s0887-6185(02)00173-1. [DOI] [PubMed] [Google Scholar]
- Zitterl W, Demal U, Aigner M, Lenz G, Urban C, Zapotoczky HG, Zitterl-Eglseer K. Naturalistic course of obsessive compulsive disorder and comorbid depression Longitudinal results of a prospective follow-up study of 74 actively treated patients. Psychopathology. 2000;33:75–80. doi: 10.1159/000029124. [DOI] [PubMed] [Google Scholar]