Abstract
The increasing complexities of health care that dental graduates must be equipped to handle require schools to develop new models of education in order to address these intricacies. To meet these challenges, it is the school’s responsibility to provide an environment that fosters discovery and scholarly activity, embraces evidence-based philosophies, encourages partnerships with other units on campus and the community, including the global community, and recognizes the richness of diversity in both our human resources and our thinking. Beyond new curriculum initiatives within our school, we recognized the need to build strong partnerships outside our four walls in order to respond to the challenges confronting us. Four such notable recent initiatives at the University of Washington School of Dentistry discussed in this article are Regional Initiatives in Dental Education, the Center for Pediatric Dentistry: Program in Early Childhood Oral Health, Northwest PRECEDENT (Practice-based REsearch Collaborative in Evidence-based DENTistry), and Alaska Native Dental Health Aide Therapist Program. These partnerships focus on new models to improve access to care and to enhance the impact of research on evidence-based practice. These are examples of the many opportunities for us to act collectively in creating new models that ensure our graduates have the knowledge, attitudes, and skills to be competent oral health care professionals.
Keywords: dental education, evidence-based dentistry, practice-based research, access to health care, partnerships, regional programs/research, dental health aide therapist, children’s oral health
Within the last decade, substantial changes have been made in dental education in response to four major issues: 1) existing disparities in oral health and access to care among underserved groups in the United States; 2) rapid advancements in scientific knowledge and information impacting oral health, most visibly in the areas of genetics and links between oral and systemic health; 3) faculty shortages in critical educational, clinical, and research areas at academic dental institutions; and 4) the isolation of dentistry (including dental education) from other health professions, with consequences for policy, practice, and patient outcomes. To meet these challenges, it is a dental school’s responsibility to provide an environment that fosters discovery and scholarly activity, embraces evidence-based philosophies, encourages partnerships with other units on campus and the community, including the global community, and recognizes the richness of diversity in both our human resources and our thinking. The school must also model and educate its students to a level of professionalism that includes social responsibility and ethical practices in all clinical, educational, and research endeavors. We aspire to graduate students eager to take on new challenges, committed to evidence-based practices and lifelong learning, and ready to address access issues and contribute to the education of the next generation of dentists. Beyond educating students who are capable of serving the oral health care needs of the nation, our graduates should be equipped with the knowledge and skills to serve as primary health care resources for screening/risk assessment of a wide variety of diseases that may be detectable within the oral-dental craniofacial region. They should be able to collaborate with their colleagues in medicine and the other health professions to create more seamless health care for patients and to ensure oral health knowledge reaches beyond the walls of the dental community.
Some of the ways dental educators in the United States are responding to these challenges were presented at the 2nd and 3rd Hiroshima Conferences on Education and Science in Dentistry, in 2007 and 2009.1,2 Our presentations at those conferences and this resulting publication focus on curriculum innovation, an area in which the American Dental Education Association’s Commission on Change and Innovation in Dental Education continues to take a leadership role in defining the basic principles and curriculum changes required to create a dental education environment that matches society’s complex needs.3 Within our school, we have begun to modify curricula in order to provide more interdisciplinary-focused opportunities, including having students review and critique scientific literature as well as develop solutions to problems on a scientific topic with the help of faculty mentors. For example, we have developed a highly successful problem-based freshman course in social issues designed to enable our students to become rigorous thinkers. Groups of students and faculty members address community oral health needs and develop strategies to solve existing challenges around access to care. Each team presents its solution to a given problem to the entire class as a final project for the course.
In addition, we continue to explore, develop, and implement innovative partnerships that have resulted in new opportunities for community members, faculty members, students, and staff to participate in programs to improve oral health and, as a result, the total health and quality of life of the communities we serve. Four such notable recent initiatives at the University of Washington School of Dentistry (UWSOD) that involve partnerships outside our four walls are the following: Regional Initiatives in Dental Education; the Center for Pediatric Dentistry: Program in Early Childhood Oral Health; Northwest PRECEDENT (Practice-based REsearch Collaborative in Evidence-based DENTistry); and the Alaska Native Dental Health Aide Therapist Program. Each of these initiatives supports the School of Dentistry’s vision:
The University of Washington School of Dentistry educates a diverse student body through a challenging learning environment informed by cutting-edge scholarship. We fully embrace the social responsibility and public trust of our role as an international leader in education, research, and clinical services. As part of a public university, we will educate a progressive workforce, develop community collaborations, and bring advances in science to address the pressing oral health needs of our state, the nation, and the world. In order to accomplish our vision, we will promote diversity in thinking and human resources, support creative breakthroughs, and commit to ethical and responsible leadership in patient care, scholarship, and research.
Early on, we recognized the need to develop and cultivate strong partnerships outside of the school and also outside of dentistry to have the breadth of knowledge as well as resources to achieve our goals. Each of these four initiatives highlights the importance of these partnerships in addressing the challenges of access to care and the need to translate research findings to the public more efficiently than in the past.
The RIDE Program
The Regional Initiatives in Dental Education (RIDE) Program (www.dental.washington.edu/ride) is a strategic expansion of the school that focuses on the selection and training of an additional cohort of dental students to address workforce and access issues in the eastern (and more rural and underserved) part of our state. RIDE includes innovative, interprofessional educational experiences for dental students to help overcome the traditional isolation of dental education and encourage a team approach to health care. The program includes extensive community-based experiences with diverse populations to foster cultural competence, social responsibility, and professionalism in students. To accomplish these goals, the school has created partnerships with other universities and schools, with private and public dental practices, and with the larger community. The RIDE program is intended to distribute the oral health workforce to communities needing dentists to improve access to care and reduce oral health disparities while fostering dissemination of new knowledge.
The RIDE program is a partnership involving the UW Schools of Dentistry and Medicine, Eastern Washington University (EWU), and Washington State University (WSU), funded by the state of Washington. Under planning since 2003, the program received funding in 2007 and has now enrolled three cohorts of eight students and has selected a fourth. RIDE students take their first year of dental school at the Riverpoint campus in Spokane, the shared health science campus of EWU and WSU, where first-year UW medical students are also educated. Dental students spend their second and third years at the Seattle campus of the UWSOD. Students have extended community-based clinical experiences in eastern Washington in their fourth year and have shorter community experiences in the summers after their first and second years.
The RIDE program utilizes faculty from EWU’s School of Dental Hygiene and from the EWU and WSU basic science departments. The latter support foundational first-year courses in anatomy and embryology, histology, microbiology, physiology, and pathology. The RIDE program makes extensive use of distance learning technologies to deliver curricula where local faculty resources are not available (such as to teach dental materials or provide detailed education in oral histology and embryology). The distance learning technologies also support frequent communication between the two campuses and careful implementation of administrative procedures to ensure that educational equivalency and other accreditation requirements are met.
RIDE also takes advantage of the UW School of Medicine (SOM)’s long-standing regional education program. The UWSOM has a total of seven regional medical training sites in the states of Washington, Wyoming, Alaska, Montana, and Idaho (WWAMI) and more than three decades of successful regional medical education.4 The UWSOM is currently the nation’s number-one ranked program in both primary care and rural health. The Spokane campus is the UWSOM’s newest regional site, providing the first year of medical school to a cohort of twenty medical students. RIDE has profited by the UWSOM’s considerable institutional experience with regional education, including the policies and processes needed to ensure the success of such programs.
As a result of the partnerships with EWU’s School of Dental Hygiene and the UWSOM, a number of curriculum innovations have been possible. For example, dental students take such courses with dental hygiene students as “Introduction to Clinical Dentistry” and “Periodontology.” Dental students in the RIDE program work more closely with dental hygiene students than is currently possible at the UWSOD Seattle campus. They also take an early elective in dental injections. We were encouraged in our efforts to expand our partnership with the dental hygiene program and the dental professional community in Spokane as a result of our students’ high rating of “The Dental Team Experience.” Under this earlier outreach program model, UW dental students, EWU dental hygiene students, and Spokane Community College dental assisting students close to graduation could work together to deliver dental services in clinics caring for underserved patients, at the same time improving team-building skills and clinical efficiency.
Our collaboration with the UWSOM allows RIDE students to participate in small groups with medical students in “Introduction to Clinical Medicine,” a course that includes interviewing hospitalized patients and topics such as ethics and professionalism and communication skills needed for working with diverse populations. Dental students also get an additional course in Spokane with medical students, “Medical Information for Decision Making,” that enhances their ability to evaluate evidence in the biomedical literature early in their educational experience. Similar to what occurs in Seattle, dental and medical students also take gross anatomy, embryology, and histology with medical students. Other innovations under exploration are an oral health elective for medical students at the Riverpoint campus, a course that has been successfully offered in the past in Seattle. Further, in 2010 a behavioral dental course was implemented for students in the RIDE program.5,6 We are also evaluating the possibility of enhanced research partnerships with these regional universities.
Our close relationship with the dental professional community in Spokane has enabled us to develop the extended community-based experiences and calibrated preceptors needed for RIDE students’ fourth-year clinical rotations. Extended community rotations were given a jumpstart by the Robert Wood Johnson Foundation’s Pipeline, Profession, and Practice: Community-Based Dental Education grant—created to improve recruitment and retention of minority dental students and address disparities through community-based education.7
With the RIDE program, we have been able to develop strategies to improve access to care and eliminate disparities in our region, while enhancing interprofessional collaboration and students’ exposure to diverse populations in underserved communities. Through the creative partnerships with the SOM, regional universities, and the dental professional community, we have been able to take advantage of existing educational resources—a critical step with today’s economic constraints and mounting faculty shortages.8 The RIDE program is also testing curriculum innovations that can lead to new educational approaches in the school as a whole, including more partnerships with other professional schools and the use of more community-based experiences.
Center for Pediatric Dentistry
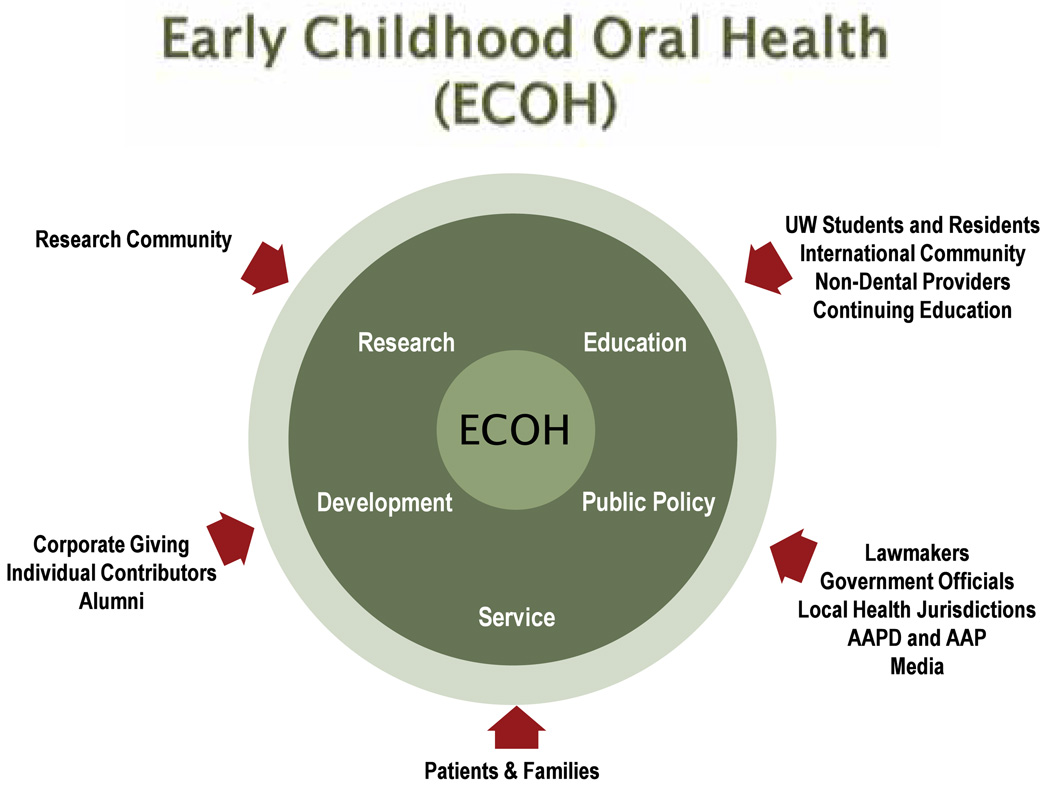
The Early Childhood Oral Health Program in the Center for Pediatric Dentistry has been established to provide a focused direction for addressing the growing crisis of childhood dental disease. Importantly, this is a joint effort between the UWSOD and Seattle Children’s Hospital that includes the development of a new pediatric dental facility, the Washington Dental Service Building for Early Childhood Oral Health. The mission of this effort is to improve the oral health of infants and toddlers through research, education, service delivery, and public policy (Figure 1).
Figure 1.
Focus areas of paramount importance to the Early Childhood Oral Health program within the Center for Pediatric Dentistry: education, research, public policy, service, and development
For each area of interest there are various groups that serve and contribute to the center. In terms of research, the research community conducts innovative research encompassing basic health, social health, behavioral health, public health, health care delivery systems, and database management that can be used to benefit the center. Students and residents, along with non-dental providers and the international community, gather and disseminate the evidence-based information and outcomes collected from research amongst themselves, other health care providers, families, and the community.
Further development of the center depends on the individual contributors, corporate giving, and alumni who provide monetary support and allow the program to grow. Public policy is influenced by lawmakers, government officials, local health jurisdictions, the media, and pediatric health organizations like the American Academy of Pediatric Dentistry and the American Academy of Pediatrics. These individuals work together to support legislation that will ultimately provide assistance for the center and similar early childhood oral health efforts. All this allows us to provide care to the community of patients and families and offer improved access for those with special needs and those requiring urgent care.
The center serves the children most at risk in several ways within four areas:
Research: conduct innovative research encompassing basic health, social health, behavioral health, public health, health care delivery systems, and database management.
Teaching: gather and disseminate evidence-based information and outcomes to predental students, dental students, pediatric dental residents, pediatric/medical faculty and residents, general and pediatric dentists, family health care providers, families, and the community.
Health care delivery systems: apply the latest evidence-based science and clinical practices, coupled with the highest quality oral health care, to prevent and treat children’s oral health problems at an early age when disease can be prevented9 and offer improved access for special and urgent needs patients.
Public policy: affect children’s dentistry by lever-aging faculty expertise in oral health; advocate on behalf of very young children; increase access and decrease barriers; and collaborate with other oral health initiatives of paramount importance.10
Unique in the nation, the center deploys a multidisciplinary health care team—including pediatricians, psychologists, social workers, and public health practitioners—to create an environment conducive for quality education and oral health care delivery to infants and toddlers and their families, especially those in the underserved populations.11 The program will serve the combined dental needs of the UWSOD’s Department of Pediatric Dentistry and Seattle Children’s Department of Dentistry, an estimated 30,000 annual visits in the first year of operation (September 2010) and 40,000 at capacity. All children with oral-craniofacial needs will be served, with emphasis on children with special needs from western Washington and across the state. The age range consists of children from birth to age twenty-one, with programmatic emphasis on early childhood (birth to age three).12
A key for success of many of our programs is the generous support of our stakeholders in the community as well as federal and industry-supported research. Implementation of this program required a major fundraising effort. A $5 million gift from the Washington Dental Service and the Washington Dental Service Foundation allows the center to grow exponentially and effectively double the number of pediatric dental visits between the two institutions, UWSOD’s Department of Pediatric Dentistry and Seattle Children’s Department of Dentistry. The Center for Pediatric Dentistry, Washington Dental Service Building also provides a central location for dental cases performed under general anesthesia and opportunities for students and faculty members to develop improved models of pediatric oral health care for delivery domestically and abroad.
The facility housing the program includes twenty-six dental chairs and three infant rooms for a total of twenty-nine chairs and three operating rooms and a total square footage, including nonclinical usage, of 28,000 square feet. The center faculty and staff are at the forefront of public involvement, education, and community outreach in the facilitation of partnerships with community-based organizations, parents, providers, and others about early childhood oral health.13
Practice-Based Research in Evidence-Based Dentistry
One of the principles increasingly accepted in the dental profession in the United States is that what is done in practice should be based on research-based evidence of what is most effective. The notion that best practices should be based on objective evidence has been gathering momentum in the medical profession for fifteen to twenty years, but the concept has become noteworthy in dentistry only in the past five or so years. However, it is clear that private insurers as well as government agencies that pay for dental care will in the future insist on the presence of evidence to support the effectiveness of procedures for which they pay. This movement stresses the need for well-prepared dental graduates of the future to understand and participate in two concepts: the practice of evidence-based dentistry and the development of practice-based research as evidence.
To understand how to practice evidence-based dentistry, one must be able to evaluate evidence as presented in published literature. This requires skills in searching the published literature, which we introduce in a first-year course that utilizes problem-based learning to raise awareness of social issues such as disparities in oral health and access to care. In the third year, we introduce students to principles involved in evaluating evidence in the literature and in interpreting the results from published studies. A new elective for third- and fourth-year students is the result of a curriculum grant from the National Institute of Dental and Craniofacial Research (NIDCR) (R25DE018436) intended to introduce more research into the dental school curriculum. This grant paid for the development and presentation of a faculty development course on the principles and practice of systematic reviews and meta-analyses. It also provides small grants to faculty members who wish to lead dental students in elective courses in which the two conduct systematic reviews of the published evidence on contemporary topics that are clinically relevant and of interest to the students.
When compiling and assessing the published literature on a clinically relevant topic, the opportunity to change clinical practice as a result of a systematic assessment of the evidence often depends on how convincing the published studies are. In the past, the publication of clinical research findings from studies done in academic institutions often had little impact on the actual practice of dentistry. That was because the studies were conducted under conditions that were felt to be artificially controlled and not at all like the conditions faced by practicing dentists. As a result, the results were often ignored. In an effort to make clinical research more relevant and hopefully have more of an impact on the practice of dentistry, in 2005 the NIDCR funded three practice-based research networks in the United States.14 These networks are charged with developing infrastructures of at least 100 practitioners who are engaged in research in their practices on topics identified by them to be relevant to the contemporary practice of dentistry.
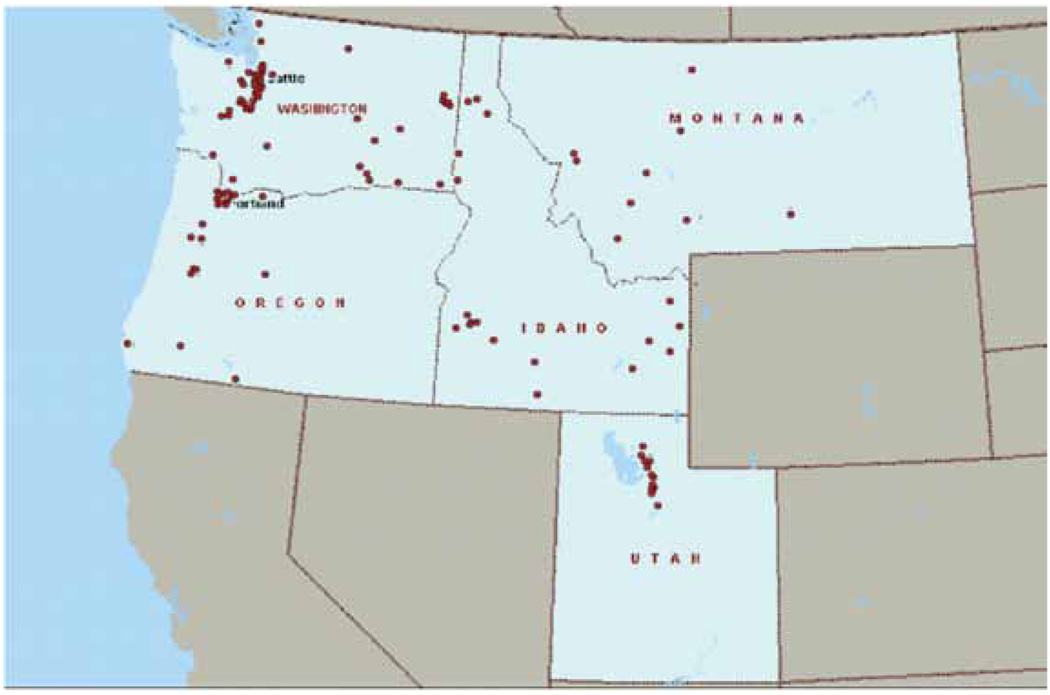
Since the development of practice-based research was consistent with our vision and mission of emphasizing evidence-based dentistry, we successfully pursued one of the three networks funded by NIDCR for Northwest PRECEDENT, which enrolls practicing dentists from the five Pacific Northwest states of Washington, Oregon, Idaho, Montana, and Utah.15 (See Figure 2.) Northwest PRECEDENT is funded by two grants: one a Network Chair grant (U01DE016750) jointly administered by dental schools at the University of Washington and Oregon Health & Science University, and the second a Data Coordinating Center grant (U01DE016752) at the University of Washington. The Northwest PRECEDENT network has developed more than a dozen clinical research projects that are completed or under way. The research projects were developed in consultation with the member practitioners, keeping some basic principles of practice-based research in mind: identify topics of interest to practitioners and relevant to the practice of dentistry; design studies that are straightforward, with simple clinical endpoints; carry out studies requiring minimal interference with everyday practice; and evaluate clinical effectiveness of approved techniques/materials. Following these principles, Northwest PRECEDENT has embarked on such clinically relevant studies as the following: The Use of Salivary Markers in Caries Risk Assessment; Case Control Study of Osteonecrosis of the Jaw; Computer-Assisted Relaxation Learning (CARL) for Needle-Phobic Patients; An Assessment of Oral Health Conditions in a Random Sample of Patients; Assessing the Outcomes of Cracked Teeth; A Clinical Comparison of MTA and Calcium Hydroxide as Direct Pulp Capping Agents for Permanent Teeth; Dentin Hypersensitivity: Treatments in General Dental Practices; Dentin Hypersensitivity: Prevalence in Patients; Third Molar Extraction: Indications and Outcomes; Temporary Anchorage Devices in Orthodontic Practice: Attitudes Toward Use and Clinical Outcomes (Orthodontists); and Primary Care Management for TMJD Pain.
Figure 2.
Geographical distribution of Northwest PRECEDENT practices, with dots representing offices involved in PRECEDENT in Washington, Oregon, Idaho, Montana, and Utah
This network and projects are currently being conducted among practicing dentists as a collaborative effort between dental schools at the University of Washington and Oregon Health & Science University, and there is potential to make these collaborations multiinstitutional and international. While Northwest PRECEDENT has developed a continuing dental education course to prepare dentists already in practice to participate in practice-based research,15 as our graduates complete their training, we should do more to prepare them to accept responsibility for helping create the evidence for future evidence-based practice of dentistry through participation in practice-based research. It should not be viewed as something to be imposed upon them, but as an opportunity to help create the evidence base for what represents best practices.
Dental Health Aide Therapists: Rethinking the Role of Supervision
In 2007, the first dental health aide therapist (DHAT) students to be trained in the United States entered a controversial new program in Anchorage, Alaska. While originally intended by Alaska tribal organizations to be a solution to their unique remote village oral health problems, the program became a lightning rod for U.S. dental health workforce controversies relating to patient safety, the cost of dental training, and even the profitability of individual dental practices.16 Promotion of the project through presentations, publications, news coverage of a lawsuit brought by the American Dental Association, and the successful graduation of the first DHAT class in December 2008 generated broad public interest. Members of disadvantaged and underserved communities saw dental therapists as a solution to their oral health access issues. Dental educators and innovators saw the introduction of a new oral health professional as an opportunity to reconsider the makeup of the dental workforce and introduce new training and practice methodologies.
Overall, the concept of dental health therapy is that individuals with shorter but more focused training can provide less complex procedures, thereby increasing cost-effective health care access. Dental therapy practice also includes the application of public health and prevention strategies to eliminate dental caries. A narrow scope of practice with dental supervision is a hallmark of the career. Dental therapy programs typically include one year of didactic training and one year of full-time clinical training followed by a preceptorship with an employing dentist. Students for dental therapy programs are recruited from local communities and specific population groups to ensure culturally competent care.
The Alaska DHAT program is based on the original New Zealand dental therapy model, introduced in 1921 and developed to provide dental care to all children in local schools.17 The two-year curriculum has been designed to meet the needs of remote Alaska villages where dentists and dental hygienists have historically provided only limited itinerant care. The first year of didactic training takes place in Anchorage, with the second year of full-time clinical experience occurring in Bethel, Alaska. Students are tribal members committed to returning to their village communities to practice as dental therapists. Dental therapists practice in remote sites under supervision by dentists. The curriculum features a redefinition of “supervision” as it is used in dental practice to a three-part structured supervision model typically used with physician assistants. The intent is to provide oversight for clinical practice that will increase the comfort of dentists in providing better-understood supervision of clinical procedures.
The dental health therapist program (also called DENTEX—for Dental Extender) is a partnership of the Alaska Native Tribal Health Corporation (ANTHC), a consortium of Alaska tribal organizations with common health goals; the University of Washington MEDEX (Physician Assistant) Program; and Yuut Elitnaurviat People’s Learning Center in Bethel, Alaska. Faculty at the University of Washington School of Dentistry currently provide instruction during the didactic year. Major funding for this program came from the W.K. Kellogg Foundation, Rasmuson Foundation, M.J. Murdock Charitable Trust, Paul G. Allen Foundation, The Denali Commission, and Bethel Community Services. A summary of the DENTEX curriculum is provided in Table 1.
Table 1.
DENTEX curriculum summary
| Year One | Year Two |
|---|---|
| Anatomy & Physiology, an online course | 39 weeks of clinical instruction (1,600 hrs) |
| Basic dental clinical environment skills | Working with a supervising dentist |
| Development of a high level of practical clinical skills | Community dentistry and prevention |
| Simulation | Village practice rotations |
| Direct patient contact | Fly into rural bush location |
| General health sciences | 200–400 people |
| Oral health sciences | Telemedicine communication training |
| Community dentistry and behavioral management techniques | Special topics:
|
Prior to development of the Alaska training program, tribal organizations through their representative, ANTHC, had sponsored twelve students for training at the University of Otago in Dunedin, New Zealand. Since their return to the United States, the Alaska dental health aide therapists’ practice has been controlled by federal regulations governing the practice of community health aides. These clinicians have provided primary care—with supervision—in Alaska villages since the development of tuberculosis medications in the 1950s. The existence of community health aide regulations creates a unique practice opportunity for DHATs that does not exist in the other forty-nine states.
In the past, a number of dental educators had sought to promote dental therapist training, but encountered strong resistance from organized dentistry. This opposition was in sharp contrast to organized medicine during creation of the physician assistant profession since, after initial resistance, medicine embraced the new profession in the late 1960s and 1970s. Based on the U.S. experience with physician assistants (PAs) and nurse practitioners (NPs), the creation of a new health profession provides the opportunity for innovation in education and practice. Problem-based learning, now integrated at least in part into most U.S. dental and medical schools, was developed for use in PA and NP programs. Similarly, new admissions processes and standardized physical assessment teaching were major innovations in health professions education first developed and implemented in PA and NP programs. At the practice level, an important development of the PA movement was a new and more structured view of supervision—since PAs, like dental therapists, function only with physician supervision.
Traditionally, dentists have provided care in solo or small group practice settings with on-site supervision of clinical staff characterized by “sign-offs” of delegated responsibilities. Currently absent in dentistry is a culture of supervision like that in medicine, in which movement up through the hierarchy of medical education (medical student to resident to chief resident to fellow to attending) brings with it increasing responsibility for supervision and development of supervisory skills.
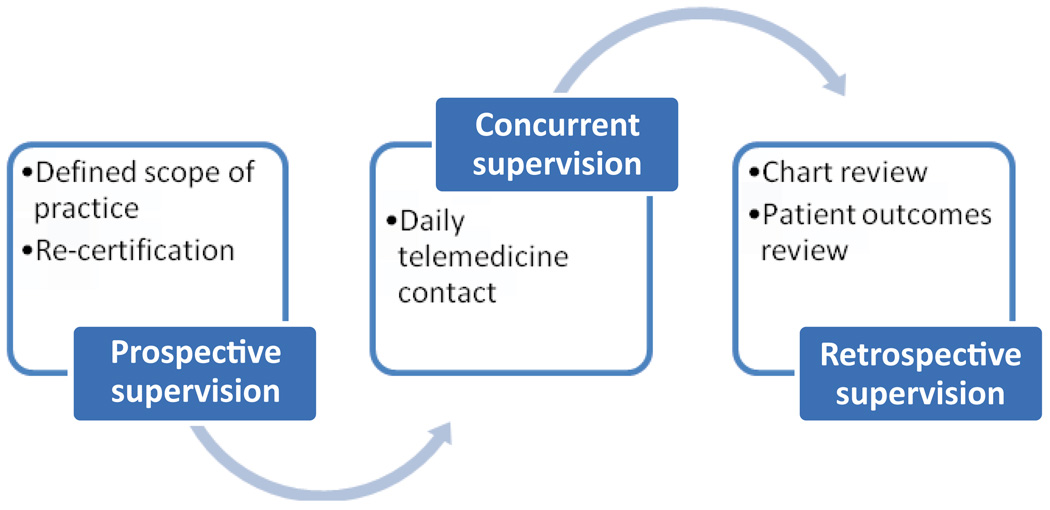
The physician assistant supervision model as it applies to DHAT practice has three components: prospective, concurrent, and retrospective (Figure 3). These terms are descriptive of the functions that make up supervision. “Prospective” refers to an agreedupon scope of practice and role definition. This may vary depending on the PA’s (or DHAT’s) training and experience. It also should include plans for future learning activities and development of additional clinical skills. “Concurrent” refers to activities while the doctor/dentist and PA/DHAT practice simultaneously (this could include electronic communication). “Retrospective” includes quality assessment activities such as post-visit case presentations/discussions, chart review, and assessment of outcomes. Originally, physicians supervising PAs received training in these supervision strategies, which dentists might obtain through continuing dental education.
Figure 3.
Model of supervision for the PA/DHAT
Note: This model emphasizes a defined scope of practice based on individual competencies, as well as a need to focus on concurrent and retrospective supervision with clearly defined expectations for success of the PA/DHAT.
The Alaska dental health aide therapist program is helping to establish a new mid-level dental profession in the United States designed to address the needs of underserved populations and the shortage of private dentists to serve them.18 As the dental therapist model moves forward, its success will be measured by increased oral health access and reduced dental disease.19 A secondary gain might be a reconsideration of the role that a new culture of supervision can play in the dental education and practice environment.
Conclusion
Beyond these four formal partnerships, we have more informal efforts ongoing in professionalism and ethics and curriculum innovation. The former has resulted in a rich conversation within the school and with our larger community about shared values and how to best implement these to enhance the culture of our school, reinforcing messages about social responsibility and ethical practices in clinical care. The task force on curriculum has just begun, charged with creating a more flexible curriculum to better achieve the many goals outlined above. We look forward to sharing these results with the larger community as well.
And so we will continue, along with our dental partners—the American Dental Education Association, American Dental Association, and International Association for Dental Research/American Association for Dental Research, as well as other national and international dental groups—to examine the best ways to move away from a densely packed, memory-based, test-driven, inflexible curriculum to one that promotes exploration and professional values while remaining solid in the knowledge, attitudes, and skills of competent oral health professionals. There are many opportunities for us to act collectively to create new models for the future. By addressing issues effectively, including advances in research and technologies, disparities in oral health, and the economic and policy environments of schools and communities, we will ensure that our profession does not become marginalized or reduced to producing technicians trained at trade schools, but instead stands at the forefront of the future of dental education.
Acknowledgments
This study was funded by the Robert Wood Johnson Foundation’s Pipeline, Profession, and Practice: Community-Based Dental Education program grant, an American Dental Association Foundation Innovation in Education grant, the National Institute of Dental and Craniofacial Research (R25DE018436), the Network Chair (U01DE016750) jointly administered by dental schools at the University of Washington and Oregon Health & Science University, and the Data Coordinating Center (U01DE016752) at the University of Washington. We wish to thank the University of Washington and our partners for their contributions and success of these programs and Jada Stewart for assistance in preparing this article.
Footnotes
The results were first presented at the 3rd Hiroshima Conference on Education and Science in Dentistry, October 2009.
Contributor Information
Ruth Ballweg, MEDEX Northwest, Division of Physician Assistant Studies, School of Medicine, University of Washington.
Joel Berg, Department of Pediatric Dentistry, School of Dentistry, University of Washington.
Tim DeRouen, Department of Biostatistics, School of Public Health and Community Medicine, University of Washington.
Louis Fiset, MEDEX Northwest, School of Medicine, University of Washington.
Wendy Mouradian, Regional Initiatives in Dental Education, School of Dentistry, University of Washington.
Martha J. Somerman, Department of Periodontics, School of Dentistry, University of Washington.
REFERENCES
- 1.Somerman MJ, Mouradian WE. Dental education in the United States: responding to challenges; Presentation at the 2nd Hiroshima Conference on Education and Science in Dentistry; 2007. Oct, [Google Scholar]
- 2.Ballweg R, Berg J, DeRouen T, Fiset L, Mouradian WE, Somerman MJ. Dental education in the United States: beyond the four walls; Presentation at the 3rd Hiroshima Conference on Education and Science in Dentistry; 2009. Nov, [Google Scholar]
- 3.Beyond the crossroads: change and innovation in dental education. Washington, DC: American Dental Education Association; 2009. American Dental Education Association Commission on Change and Innovation in Dental Education. [Google Scholar]
- 4.Ramsey PG, Coombs JB, Hunt D, Marshall SG, Wenrich MD. From concept to culture: the WWAMI program at the University of Washington School of Medicine. Acad Med. 2001;76(8):765–775. doi: 10.1097/00001888-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Mouradian W, Reeves A, Kim S, Lewis C, Keerbs A, Slayton R, et al. New oral health elective for medical students at the University of Washington. Teach Learn Med. 2006;18:336–347. doi: 10.1207/s15328015tlm1804_11. [DOI] [PubMed] [Google Scholar]
- 6.Mouradian W, Reeves A, Kim S, Evans R, Schaad D, Marshall S, Slayton R. An oral health curriculum for medical students at the University of Washington. Acad Med. 2005;80(5):434–442. doi: 10.1097/00001888-200505000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Formicola A, Bailit H, D’Abreu K, Stavisky J, Bau I, Zamora G, et al. The dental pipeline program’s impact on access disparities and student diversity. J Am Dent Assoc. 2009;140:346–353. doi: 10.14219/jada.archive.2009.0166. [DOI] [PubMed] [Google Scholar]
- 8.Chmar JE, Weaver RG, Valachovic RW. Dental school vacant budgeted faculty positions, academic years 2005–06 and 2006–07. J Dent Educ. 2008;72(3):370–385. [PubMed] [Google Scholar]
- 9.Berg JH. Fluoride varnish application prevents caries in preschool children. J Evid Based Dent Pract. 2007;7(1):23–24. doi: 10.1016/j.jebdp.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 10.Berg JH, Slayton R, editors. Early childhood oral health. Ames, IA: Wiley-Blackwell; 2009. [Google Scholar]
- 11.Berg JH, Domoto PK. The “age-one” dental visit: preventing early childhood caries. Inside Dentistry. 2007 March;:2–10. [Google Scholar]
- 12.Berg JH. Minimal intervention: motivating patients through caries risk assessment. Compendium. 2007;28(3):162–164. [PubMed] [Google Scholar]
- 13.Berg JH. ECOH forms to impact the childhood caries epidemic. Doctor Dent. 2007;3:9. [Google Scholar]
- 14.Kuska B. News release. Rockville, MD: National Institute of Dental and Craniofacial Research, National Institutes of Health; 2005. NIDCR awards grants for new practice-based initiative. [Google Scholar]
- 15.DeRouen TA, Hujoel P, Leroux B, Mancl L, Sherman J, Hilton T, et al. for the Northwest Practice-based REsearch Collaborative in Evidence-based DENTistry (PRECEDENT). Preparing practicing dentists to engage in practice- based research. J Am Dent Assoc. 2008;139:339–345. doi: 10.14219/jada.archive.2008.0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McKinnon M, Luke G, Bresch J, Moss M, Valachovic RW. Emerging allied dental workforce models: considerations for academic dental institutions. J Dent Educ. 2007;71(11):1476–1491. [PubMed] [Google Scholar]
- 17.Coates D, Kardos T, Moffat S, Kardos R. Dental therapists and dental hygienists educated for the New Zealand environment. J Dent Educ. 2008;73(8):1001–1008. [PubMed] [Google Scholar]
- 18.Bolin KA. Assessment of treatment provided by dental health aide therapists in Alaska: a pilot study. J Am Dent Assoc. 2008;139:1530–1535. doi: 10.14219/jada.archive.2008.0080. [DOI] [PubMed] [Google Scholar]
- 19.Nash D, Ruotoistenmäki J, Argentieri A, Barna S, Behbehani J, Berthold P, et al. Profile of the oral health care team in countries with emerging economies. Eur J Dent Educ. 2008;1:111–119. doi: 10.1111/j.1600-0579.2007.00493.x. [DOI] [PubMed] [Google Scholar]