Abstract
The prevalence of obesity, and the cluster of serious metabolic diseases it is associated with, continues to rise globally, and hopes for effective treatment with drugs have been considerably set back. Thus, success with bariatric surgeries to induce sustained body weight loss and effectively cure most of the associated co-morbidities appears almost “miraculous” and systematic investigation of the mechanisms at work has gained momentum. Here, we will discuss the basic organization of gut-brain communication and review clinical and pre-clinical investigations on the potential mechanisms by which gastric bypass surgery leads to its beneficial effects on energy balance and glucose homeostasis. Although a lot has been learned regarding changes in energy intake and expenditure, secretion of gut hormones, and improvement in glucose homeostasis, there has not yet been the “breakthrough observation” of identifying a key signaling component common to the beneficial effects of the surgery. However, given the complexity and redundancy of gut-brain signaling and gut signaling to other relevant organs, it is perhaps more realistic to expect a number of key signaling changes that act in concert to bring about the “miracle”.
Keywords: Bariatric surgery, Roux-en-Y gastric bypass, metabolic syndrome, type-2 diabetes, GLP-1, PYY, ghrelin, insulin, amylin, vagus nerve, energy homeostasis, satiation, glucose homeostasis
1. Introduction
The prevalence of obesity and the metabolic syndrome is rapidly increasing, with the prospect that more than half of the adult population will be overweight or obese in 2015, and every third child born today will develop diabetes later in life [1]. The strong correlation between obesity and development of type 2 diabetes, cardiovascular disease, gall bladder disease, osteoarthritis, sleep and mental disorders make it the major health problem. Current treatment of obesity targets both energy intake and expenditure. It includes dieting and exercise (life style changes), as well as surgery, drugs, plant extracts, and many scientifically undocumented remedies. Most of these treatments are not very effective, with a typical maximal weight loss of less than 10%, and are not able to stop the epidemic. Obesity surgery is presently the most effective treatment with sustained weight loss of up to 50%. It implicates gut-brain signaling by vagal afferent and hormonal mechanisms as an important factor in the development and prevention of obesity. Among the different types of bariatric surgery, Roux-en-Y gastric bypass (RYGB) is the most effective in causing sustained weight loss and normalization of glucose homeostasis and will be the focus of this review.
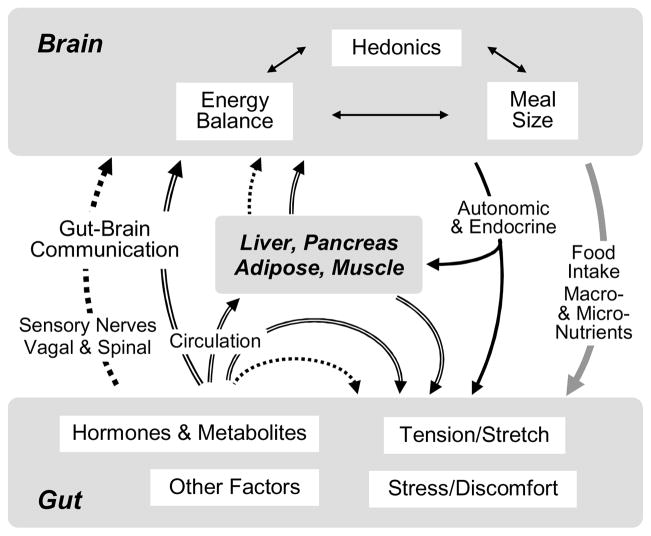
As shown schematically in Fig. 1, the potential mechanisms leading to the beneficial effects of RYGB are likely complex and involve a number of organs and communicating pathways. Not only the gut-brain axis, but also the gut-adipose tissue, gut-liver, gut-pancreas, and gut-muscle axes are involved. At the origin are the immediate surgery-induced changes within the gut itself (see below) that directly or indirectly change hormonal and sensory neural signaling from the gastrointestinal tract to these other organs. The brain is likely a key recipient of humoral and neural signals from the altered gut and is the ultimate orchestrator of changed food intake and preference. Changes in the quantity and composition of food intake, in turn, cause further changes in gut functions and signaling to the brain and other organs. Circulating signals also reach the liver, pancreas, white and brown adipose tissue, and muscle. Functional changes in these organs largely determine substrate utilization and energy expenditure and generate another set of humoral and neural signals to the brain, gut, and to each other. Together with information from the gut, they determine changes in autonomic and endocrine outflow to all relevant organs. Thus, there are up to several loops involved in the information flow from primary surgical effect to the ultimate functional consequence. At a more detailed level there are almost countless potential signaling steps leading to the ultimate functional consequence (Fig. 2). Given this complexity, it is not surprising that the critical change(s) bringing about the beneficial effects of RYGB have not yet been identified. However, the rapidly increasing number of studies in patients and animal models has led to a number of leading candidate mechanisms.
Fig. 1. Schematic diagram showing flow of information potentially involved in the physiological and behavioral consequences of gastric bypass surgery.
Communication by circulating hormones, metabolites, and other factors is depicted by double lined arrows, communication by sensory nerves by dotted lined arrows, and autonomic and endocrine outflow by solid line arrows. Note that the arrangement allows learning to take place, as ingestion of different foods produces different consequences in the altered gut that are in turn sensed by the brain.
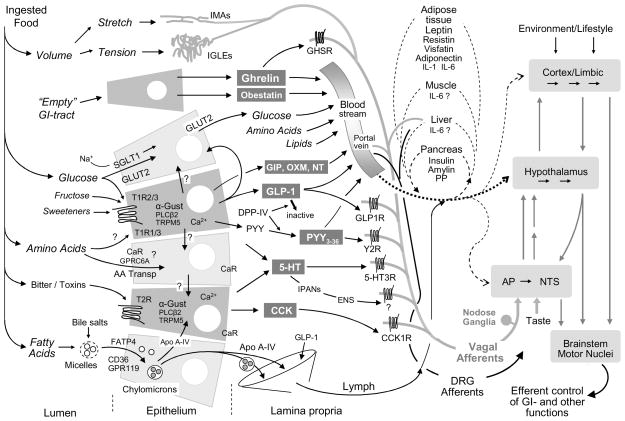
Fig. 2. The sensory limb of gut-brain communication.
Simplified schematic diagram showing the major transduction sites and mechanisms for the detection of ingested food and its macronutrient components. Ordinary enterocytes are shown in light gray and enteroendocrine cells and their hormonal outputs in darker gray. Note that the molecular machinery given for a particular epithelial cell is not completely known and does not, therefore, define specific fixed configurations. In particular, it is not clear to what extent ordinary enterocytes and certain enteroendocrine cells express the different types of G protein-coupled receptors of the T1R and T2R families, the amino acid-sensing calcium receptor and GPCR6, and the fatty acid transporters FATP4, CD36, GPR119, and GPR120. After release of nutrients and hormones into the lamina propria, they are taken up by capillaries and sent to the brain and other organs through the general circulation and/or the lymphatic system. Circulating nutrients and hormones have access to the brain at all levels. Hormones and transmitters in the lamina propria can also interact with relevant receptors on mucosal endings of vagal afferent neurons and enteric neurons as well as dorsal root afferents. Vagal afferent information reaches the brain through the nucleus tractus solitarius and area postrema in the caudal brainstem and is then disseminated to hypothalamus and forebrain as indicated by gray arrows. Note that intestinal epithelial cells can also communicate with each other through paracrine or humoral mechanisms, and with other organs involved in energy balance regulation such as the pancreas, liver, adipose tissue, and muscle, through humoral mechanisms.
We would like to dedicate this review to the pioneering work of Henry S. Koopmans (1944 – 2010). He was one of the first to recognize the potential powerful effects of surgical gut manipulations on the control of food intake and regulation of energy balance and the first to carry out intestinal bypass surgery in rats. In a series of papers published in the late seventies and early eighties [2–6], he laid much of the groundwork for understanding the principal characteristics of modern bariatric surgeries.
2. Effects of RYGB on energy balance
One of the fundamental problems with dieting-induced weight loss is the induction of adaptive responses including hypo-metabolism and increased appetite [7]. This natural biological response to starvation is very strong and occurs even when losing excess weight by obese subjects, in which starvation is perceived rather than real [8–10]. Thus, the substantial weight loss after RYGB could be expected to trigger the same adaptive responses. The following discussion of the available literature demonstrates that the reverse appears to happen after RYGB-induced weight loss - reduced appetite and increased energy expenditure relative to the weight lost. This almost “too good to be true” outcome begs for a mechanistic explanation. Understanding these mechanisms will hopefully lead to the identification of the essential surgical element(s) or even better, “knifeless” approaches with drugs and/or behavioral modifications in the treatment and prevention of obesity and metabolic disease.
2.1. Body weight and body composition
Loss of excess body fat and body weight, reversal of obesity, is the intended outcome of any bariatric surgery, and RYGB is the most effective surgical type for large and sustained body weight loss in obese subjects [11]. Typically, three phases of RYGB-induced weight loss can be distinguished. An initial phase of rapid weight loss is mainly due to severely reduced energy intake, partly caused by nonspecific effects of the surgery (see below). A second phase of much slower weight loss is often seen after food intake has returned to near normal levels. A third phase is characterized either by stable body weight at about 20–40% below the obese level, observed in most rat RYGB models [12,13] (Fig. 3A), or by slow weight regain as observed in many human RYGB patients [14] and in rat gastric sleeve [15] and jejunoileal bypass models[16]. In animal models, sham surgery is followed by a small and transient drop in body weight and, depending on the type of diet, by a return to preoperative levels or by reaching even higher levels. In our “reversal of obesity” model that most closely mimics the humans situation, rats are fed a high-energy diet throughout the experiment, and the difference in body weight between sham-operated and RYGB animals can be as much as 200 g at 5 months after surgery [13] (Fig. 3A).
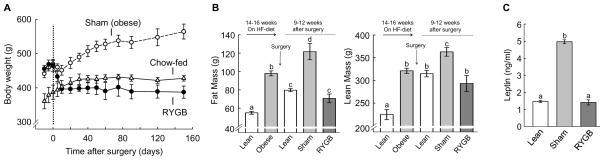
Fig. 3. RYGB induces significant loss of body weight and fat mass with relatively minor effects on lean mass.
A: Body weight of high-fat exposed RYGB (black circles, n = 5) and sham-operated (open circles, n = 6), as well as chow-fed control rats (open triangles, n = 6). B: Body composition as assessed by whole body magnetic resonance relaxometry (NMR), showing fat and lean mass before and after 14 weeks exposure to high-fat diet (left two bars), and for RYGB rats (dark gray bars), sham-operated (obese) rats (light gray bars), and non-operated, age-matched, chow-fed lean rats (white bars). C: Fasting plasma leptin levels at 3 months after surgery. Bars that do not share a common letter are significantly different from each other (P < 0.05; based on ANOVA followed by Fisher’s LSD posthoc test).
Loss of body weight is mainly due to loss of fat mass, with a proportionately smaller loss in lean mass. Nevertheless, in a meta-analysis on a large number of cohorts losing weight by dietary restriction, behavioral modification, and various types of bariatric surgeries showed that relative loss of fat free mass (loss of fat free mass per total weight loss) was positively correlated (R2 = 0.31) to the degree of caloric restriction, and exercise attenuated this relationship [17]. Growth hormone treatment for 6 months after RYGB has also reduced loss of fat free mass [18].
In our rat model, RYGB rats, 3–4 months after surgery, lost about equal absolute amounts of fat mass and fat free mass compared to pre-surgical (obese) levels. However, their fat free mass was not significantly different from chow-fed un-operated control rats of the same age (Fig. 3B). Importantly, the loss of fat mass was accompanied by a complete normalization of plasma leptin levels, indicating loss of all excess fat mass (Fig. 3C).
2.2. Food intake
2.2.1. Energy intake
Available data from animal models and human studies suggest decreased energy intake to be the major cause of the observed weight loss after RYGB, at least during the early post-surgery period. This conclusion is supported by direct measurements of food intake [13,19,20] and by the fact that pair-feeding causes similar initial weight loss [20–23]. However, although not consistently reported, effects on nutrient absorption, feed efficiency, and energy expenditure also need to be considered, particularly after the initial weight loss phase (see below).
There is a substantial reduction in calorie intake during the first few days after RYGB surgery in most human studies and animal models. In animal models, the contribution of non-specific, surgical trauma-related mechanisms to this early hypophagia can be estimated by comparing calorie intake in RYGB and sham-operated animals, but only if true sham surgery is employed. When using a complete liquid diet (Ensure), energy intake in sham-operated rats decreases as much as 50% during the first 3 days and then gradually recovers to normal levels within about 10 days[13]. Full RYGB surgery results in >90% suppression of liquid Ensure intake during the first 3 days and gradual recovery to about 50% of normal daily intake by 10 days. Because different investigators use different feeding strategies after surgery, comparisons are made difficult, but a substantial initial reduction of 20–50% is generally observed [19,20,23,24]. After the initial strong suppression, food intake typically stabilizes at levels 20% below or near the energy intake of sham-operated rats, which often allows discontinuing pair-feeding after 3–4 weeks[23].
2.2.2. Meal patterns
We have studied meal patterns with both liquid and solid foods and consistently found decreased meal sizes and slower eating rates (Fig. 4A,B). Two to three weeks after RYGB surgery, liquid meal size was reduced as much as 60%. Mean meal duration was not different and meal frequency increased, strongly suggesting that the initial hypophagia is due to an inability to consume beyond a threshold volume and speed. These profound changes in liquid meal patterning are likely due to the negative impact of dumping. Under normal conditions, dumping is prevented by feedback control of gastric emptying, but after RYGB, there is no mechanism to retain fluids or solids in the gastric pouch. Ingested food reaching the pouch is rapidly squeezed into the anastomosed mid-jejunum, limited only by the size of the stoma. Human RYGB patients show typical signs of the dumping syndrome by exhibiting severe nausea, light-headedness, flushing, and diarrhea after ingestion of 100 g oral glucose [25]. Although the dumping syndrome is typically observed with sugary foods, aversive effects of fatty foods have also been noted, as almost one third of the RYGB patients consciously avoided fatty foods, mainly due to not feeling good after eating them [26–28]. In support of this interpretation, we have noticed that some RYGB rats consumed very large amounts of Ensure on one day, only to abstain completely from Ensure intake the next day, suggesting negative consequences, and subsequently conditioned avoidance of large meals.
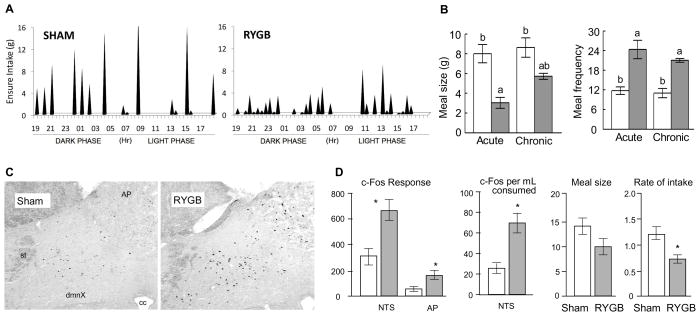
Fig. 4. RYGB-induced decrease of meal size and accompanying exaggerated meal-induced neural activation in the nucleus of the solitary tract.
A: Typical liquid (Ensure) meal pattern, 2–3 weeks after RYGB or sham operation. B: Average meal size and meal frequency during the acute (weeks 2–3) and chronic (weeks 18–20) phases after RYGB (dark bars) or sham-surgery (white bars). Bars that do not share the same letters are significantly different from each other (p<0.05), based on two-way ANOVA). C: Examples of meal-induced c-Fos induction in the dorsal vagal complex of the caudal brainstem, 10 days after RYGB or sham-operation. D: Quantitative analysis of exaggerated c-Fos response in the NTS and area postrema. * p, 0.05 based on t-test.
It is not clear how the signal leading to avoidance is generated and mediated to the brain. Specifically, it is not clear whether it is caused by over-stimulation of physiological satiation mechanisms thought to be mediated mainly by mechano- and chemosensory vagal afferents, or recruitment of pain mechanisms typically mediated by dorsal root afferents and spinal pathways [29,30]. Signaling within both of these neural pathways could be exaggerated through a process of sensitization caused by mechanical and chemical stress via elevated proinflammatory cytokines such as tumor necrosis factor-alpha [31]. High fat diets are known to cause a state of low chronic inflammation in various tissues, including the gastrointestinal tract [32,33].
In a study with RYGB patients, it was found that intraluminal pressure as measured with a sensor lowered into the Roux limb was negatively correlated with meal size, suggesting involvement of vagal or dorsal root mechanosensory afferents [34]. In our rat model, we found exaggerated neural activation in the dorsal vagal complex and paraventricular nucleus of the hypothalamus after ingestion of a given size liquid meal, 10 days after RYGB surgery (Fig. 4C,D). Thus, exaggerated vagal afferent signaling may be at the origin of reduced meal size and may even act beyond individual meals to reduce total food intake.
2.2.3. Macronutrient choice and hedonic eating
RYGB surgery in human subjects has been reported to change food preferences. In one study, RYGB patients showed heightened acuity for sweet taste, with some patients complaining that the food was too sweet [35], but in another study there was increased acuity for bitter and sour tastes and a trend towards reduction in salt and sweet detection [36]. In other human studies, preference for high-carbohydrate foods [37] and high-fat foods [26,37,38] was decreased after RYGB. In addition, RYGB patients were reported to lose the desire or motivation to eat [37].
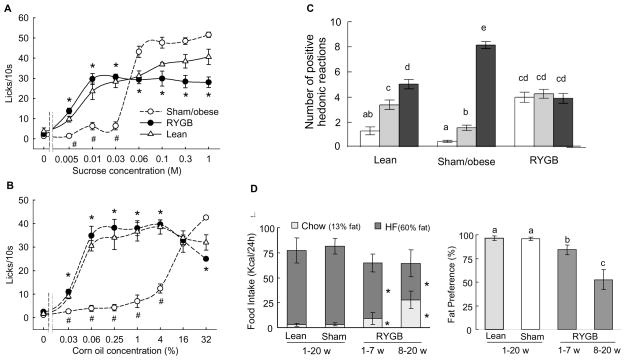
We have observed similar changes in food preference in our rat model. When given a choice of complete diets low or high in fat, RYGB rats showed a gradual shift in preference for the low fat diet (Fig. 5D). In searching for potentially underlying mechanisms for this shift, we have systematically investigated the role of taste-guided hedonic behavior in RYGB, sham-operated, and never obese, age-matched control rats. In the brief access lick test, rats have successive 10 s access to corn oil emulsions of increasing concentrations, minimizing postingestive consequences such as conditioned acceptance. We found that compared to never obese chow-fed control rats, sham-operated obese rats avoided low concentrations of corn oil and strongly preferred the highest concentrations and that this right-shift in the concentration-response curve was completely reversed 3–5 months after RYGB surgery (Fig. 5B,D). These results suggest that the shift in long-term acceptance of diets with different fat content may be due to changes in hedonic processing. This interpretation was supported by similar findings with sucrose, for which we not only demonstrated a right-shift of the concentration-response relationship in the brief access test (Fig. 5A), but also in the taste reactivity test (Fig. 5C), assumed to be a measure of hedonic impact or ‘liking’ [39].
Fig. 5. Roux-en-Y gastric bypass surgery changes hedonic evaluation of food stimuli.
A, B: Lickometer responding for different concentrations of sucrose (A) and corn oil (B). The number of licks/10s was measured in series of ascending concentrations of sucrose solutions and corn oil emulsions. Outbred Sprague-Dawley rats with either Roux-en-Y gastric bypass surgery (RYGB, filled circles; n = 9) or sham surgery (sham, open circles; n = 11), and non-operated, chow-fed, lean controls (lean, open triangles; n = 7). *p < 0.05, RYGB compared with sham/obese and, # p < 0.05, lean compared with sham/obese rats, based on ANOVA and Bonferroni adjusted multiple comparisons. C: Number of positive hedonic reactions (‘liking’) in response to tasting 3 different sucrose concentrations. Bars that do not share the same letter are significantly different from each other (p < 0.05, based on ANOVA and Bonferroni adjusted multiple comparisons). D: Gradual development of high-fat avoidance in RYGB rats. Total calorie intake from chow and high fat diet in two-choice paradigm, showing the gradual increase of chow intake from in RYGB rats is shown in left panel and the corresponding fat preference is shown in the right panel. * p< 0.05 compared with both lean and sham rats.
2.3. Energy digestion efficiency
Not all energy ingested is absorbed - even under normal conditions, a significant percentage of ingested energy is lost in the feces, particularly with high fiber diets [40,41]. As much as 20–25% of ingested energy is lost in the feces when rats eat regular rodent chow. Strategies to reduce absorption of fats and increase fecal energy loss have long been used to treat obesity [42]. Thus, a moderate degree of energy malabsorption not accompanied by clinically significant problems could be seen as a welcome effect of RYGB. Most rat models find increased fecal energy loss after RYGB [23] or jejunoileal bypass [16,43]. In a study using regular chow diet before and after surgery, there was no increase in fecal energy loss, but the loss was already high (~21 kcal/24 h) in sham-operated rats [19]. In another study, fat absorption was quite drastically decreased from 93% to about 70% [24], while in another study, total nutrient absorption was decreased from 95% to 90% [23] at about 3 months after RYGB. We found a significant decrease in total nutrient absorption from 93% in sham-operated rats to 85%, 3–5 months after RYGB, probably reflecting the shorter combined length of the Roux and common limbs (unpublished observations).
There are several factors determining digestion efficiency. The decrease in absorptive capacity due to shortening of the bowel is a major factor, particularly shortening of the common limb, to which bile action is confined. This deficit appears to be maximal early after surgery, before the absorptive surfaces of the Roux and common limbs increase dramatically [16,44], probably due to trophic actions of GLP-2 [45]. Lack of mechanical mixing and breakdown as well as acidification in the stomach can also lead to reduced absorption, including micronutrients such as iron. Another potential factor is a change in the gut microbiome. Changed microbiota composition and weakening of mucosal barrier functions are causally linked to intestinal and adipose tissue inflammation and appear to play major roles in the development of high-fat diet-induced obesity [46–48]. It has also been proposed that the extra energy harvested from high fiber diets by the obesity associated microbiome could contribute to a positive energy balance and lead to obesity [49]. If RYGB reverses the bacterial profile from the obese to the lean state, it would be another welcome mechanism to reduce availability of absorbable energy [50,51].
2.4. Energy expenditure and substrate utilization
As mentioned above, weight loss typically induces a state of increased fuel-efficiency manifested by reduced energy expenditure, even after taking the lower body mass into account. Therefore, the predicted decrease in energy expenditure, which goes beyond simply tracking lean body mass, should be used to estimate the beneficial effects of bariatric surgery. In addition, meaningful calculations of energy expenditure should be carried out during steady state energy balance, not during rapid weight loss or gain. Longitudinal studies conducted in RYGB patients generally support the conclusion that 12–24 months after RYGB, energy expenditure is higher than expected [38,52–58]. In one study, energy expenditure uncorrected for body mass and composition was about 10% higher at 26 months after RYGB compared with age-matched lean control subjects (the difference not reaching statistical significance) [58]. Considering that the RYGB patients had lost about 6 kg body weight, of which as much as 30% could have been fat-free mass [17], the findings suggest inappropriately high energy expenditure in RYGB patients.
In a normal chow-fed Wistar rat model, total 24 h energy expenditure corrected for body weight was significantly increased by 13%, 2 months after RYGB compared to a weight-matched, food restricted, sham-operated group [44]. In an obesity-prone Osborne-Mendel rat model maintained on high fat diet, total energy expenditure corrected by the 0.75 power of body weight, was about 19% higher and resting energy expenditure was 31% higher, ten weeks after RYGB, compared to high-fat restricted, weight-matched control rats, and this increased energy expenditure was accompanied by significantly increased body temperature [23]. Total energy expenditure per body weight to the 0.75 power was also significantly higher by about 7% in RYGB rats compared with sham-operated (obese) rats [23]. In contrast, significantly lower energy expenditure per animal was reported in normal chow-fed Sprague Dawley rats with biliopancreatic diversion and vertical sleeve gastrectomy, compared to both sham-operated and non-operated control rats [16]. This decrease appeared to be maximal at 2 weeks after surgery, and gradually disappeared, so that 6 weeks after surgery, the bypassed rats had similar energy expenditure to the much heavier controls [16].
In our first rat cohort, we found no difference in energy expenditure corrected for body weight or lean mass between RYGB and sham-operated animals, 5 months after surgery. The respiratory exchange rate was significantly increased in RYGB rats, probably reflecting the higher intake of chow [13]. In another cohort (unpublished observations), total and resting energy expenditure corrected for body weight was higher (~ 20%), 3 months after RYGB compared with both sham-operated and pair-fed controls, but the differences were not statistically significant.
Together, these limited observations indicate that RYGB surgery eventually leads to a higher level of energy expenditure than expected on the basis of the much reduced body weight including some lean mass, but that there might also be an initial response in the opposite direction, seen after caloric restriction. Thus RYGB has the ability to somehow ignore or counteract the strong biological signals causing hypo-metabolism and increased hunger during prolonged food restriction as in dieting.
3. Potential role of gut and pancreatic hormones
The first suggestion that a humoral satiety factor is involved came from experiments with jejunoileal bypass in rats. Fasted recipient rats infused intraperitoneally with bypass plasma ate 32% less during the first hour of re-feeding than did recipients of sham-bypass plasma [59]. Since the food suppressive effects of enteroglucagon (specifically its cleavage product, GLP-1) was not known, and PYY had not been discovered at that time, the list of potential candidates included bombesin, cholecystokinin, glucagon, and pancreatic polypeptide [59]. It is only with the ascent of experimental studies on modern gastric bypass surgery that GLP-1, PYY, and ghrelin have risen to be the major hormonal candidates producing reduced food intake and sustained weight loss. The possible mechanisms by which changes in gut hormones lead to weight loss and T2DM remission have been reviewed previously [60–62] and are only briefly reviewed here.
3.1. GLP-1 and PYY
Exaggerated GLP-1 and PYY responses to a mixed meal or oral glucose have been reported in RYGB patients six weeks to 48 months post-surgery [19,58,63–66] (for a review of all types of surgery, see [62]). In one longitudinal study, significantly elevated GLP-1 and PYY responses to a mixed meal were apparent as early as 2 days after RYGB surgery [67].
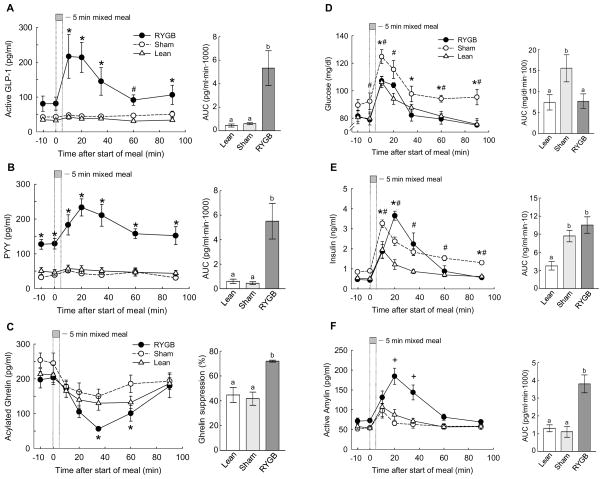
Increased fasting and meal-stimulated plasma levels of GLP-1 have been reported in three animal models [19,21,68], but conclusions were limited by either single blood samples or stressful tail blood sampling and gavaging techniques. We implanted chronic jugular catheters for remote, stress-free, blood sampling in rats trained to consume a mixed meal (Ensure) within a defined time window and a modern multiplex assay was employed. We found significantly elevated meal-stimulated levels of active GLP-1 and total PYY, and increased basal levels of PYY [69] (Fig. 6A,B). GLP-1 and PYY areas under the curve for the 100 min postprandial period were more than 6-fold higher in RYGB rats, compared with either sham-operated (obese) and chow-fed controls, 4–5 months post-surgery.
Fig. 6. Roux-en-Y gastric bypass surgery changes gut hormone secretion and glucose homeostasis.
GLP-1, PYY, ghrelin, glucose, insulin, and amylin responses to a mixed meal in RYGB (black circles), sham-operated, obese rats (open circles), and chow-fed lean controls (open triangles). Overnight food-deprived rats consumed 5 ml (~5 kcal) of Ensure delivered at 1ml/min and jugular vein blood was sampled remotely at the times indicated. * p < 0.05 between sham and RYGB rats; # p < 0.05 between sham and lean rats; + p < 0.05 between RYGB and both other groups. Areas under the curve (AUC) are shown in the bar graphs at the right, with bars that do not share a common letter significantly (p < 0.05) different from each other.
Given the considerable evidence that both peptides suppress food intake [70–74], that GLP-1 strongly stimulates insulin secretion [60], and that PYY-deficient mice have an obese phenotype [75], their robustly increased levels are prime candidates for mediating the beneficial effects of RYGB on body weight and glucose homeostasis. In our rat model, basal and postprandial PYY levels were not different between obese and lean rats but were significantly elevated almost 3-fold 4 months after RYGB. The literature is controversial regarding fasting and meal-stimulated PYY levels in obese subjects. Some studies find that obese children [76] and adults [77] have significantly lower basal and meal-stimulated circulating PYY levels. Children with the lowest fasting levels of PYY where the most likely to succeed in a one year weight loss program, after which PYY levels were restored to higher levels found in lean children [76]. Together with reduced satiety in the obese and the fact that sensitivity to exogenous PYY remained intact [77], these findings suggest that low PYY levels might be a major factor contributing to the development of obesity. However, similar to our results in rats, other clinical studies did not report differences in fasted and meal-stimulated PYY levels between obese and lean subjects [63,78,79]. Some of the discrepant outcomes may be explained by assays detecting either total PYY [76] or selectively PYY(3–36) [63,79]. Nevertheless, our finding of greatly increased fasting and meal-stimulated PYY levels after RYGB agrees with clinical studies and confirms PYY as a major candidate for the beneficial effects of RYGB.
However, a causal relationship between elevated GLP-1 and PYY levels and effectiveness of RYGB has not yet been demonstrated. Once released, GLP-1 is rapidly cleaved by the ubiquitous serine protease dipeptidyl-peptidase IV (DPP-IV), so that the half-life of circulating GLP-1 is only a few minutes. However, there are two mechanisms that protect GLP-1’s potency for remote signaling. First, sensory vagal nerve fibers innervating the gut mucosa and expressing GLP-1 receptors [80] are in close anatomical contact to the base of enteroendocrine cells [81]. Second, GLP-1 entering intestinal lymph appears to be protected from rapid degradation and available for delayed release to the circulation [82]. Furthermore, GLP-1 is produced by a small group of neurons in the nucleus tractus solitarius (NTS) in the caudal brainstem and released as a neuromodulator within the brainstem and hypothalamus [83]. Because these neuronal GLP-1 projections receive input from the gut via vagal afferents [84], likely including GLP-1 sensitive afferents from the intestinal mucosa and the hepato-portal vein [85,86], they might be considered as an additional mechanism for amplification of the rapidly fading peripheral GLP-1 signal.
A peripheral site of action of GLP-1, perhaps on vagal afferents in the mucosa [80,81], is indicated by observations that reduced meal size induced by intraperitoneally administered GLP-1 was abolished in rats with vagal de-afferentation [73]. However, the same group of researchers found that the reduction of meal size by GLP-1 infusion into the hepatic portal vein was not affected by sensory vagotomy, suggesting that intravenous GLP-1 may affect food intake by acting in the brain [73]. Intracerebroventricular administration of GLP-1 or its stable agonist Exendin-4 directly into the brain potently decreases, whereas the GLP-1 receptor antagonist Exendin-9 (Ex9) increases food intake [87]. GLP-1 injected locally into the arcuate nucleus reduces hepatic glucose production but does not affect food intake, whereas injection into the paraventricular nucleus of the hypothalamus suppresses food intake [88]. Using hypothalamic slices from mice that express green fluorescent protein in POMC neurons, it was demonstrated that GLP-1 directly stimulates arcuate nucleus POMC neurons [89]. Furthermore, selective activation of GLP-1 receptors in the caudal brainstem was sufficient to suppress food intake, gastric emptying, and core body temperature in rats [74], likely involving GLP-1 receptors on area postrema neurons projecting to both vagal and sympathetic output systems [90].
In a mouse model of duodeno-jejunal bypass surgery with an intact stomach, peripheral infusion of exendin 9-39 prevented the increased insulin secretion during an oral glucose tolerance test, but not insulin sensitivity, and only minimally rescued surgery-induced hypophagia. These results suggest that increased GLP-1 levels might account for the enhancement of insulin secretion, but play a minor role in hypophagia after the bypass procedure [91]. However, the presence of GLP-1 receptors in peripheral taste pathways [92,93], suggests the possibility of increased modulation of taste functions by the elevated circulating GLP-1levels after RYGB.
In addition to suppressing food intake, PYY may also affect lipid mobilization and energy expenditure. Chronic infusion of PYY(3–36) in high-fat diet-induced obese mice not only reduced food intake, but also prevented the expected (lower body weight) reduction of energy expenditure and lowered the respiratory quotient, indicating increased fat oxidation [94]. Thus, similar to RYGB, PYY(3–36) administration appears to simultaneously affect energy intake and expenditure to achieve an overall catabolic impact.
3.2. Ghrelin
To date, ghrelin is the only orexigenic gut hormone identified, and decreased ghrelin was the first hormonal mechanism implicated in the beneficial weight-loss effects of RYGB. It was initially observed that RYGB patients had substantially reduced plasma ghrelin levels throughout the diurnal cycle despite weight loss, compared with diet-induced increases of ghrelin levels in control subjects [95]. The possibility that decreased ghrelin levels may be partly responsible for reduced hunger after RYGB was confirmed by other clinical studies [96–98] and by the observation that postoperative weight loss is correlated with the magnitude of the decrease in circulating ghrelin levels in a rat model for RYGB [99]. Several other clinical studies did not find significantly decreased fasting ghrelin levels after RYGB compared to untreated obese subjects [58,63,100,101], but in some of these studies, meal-induced suppression of ghrelin was enhanced[58,63]. In a recent prospective study, fasting and postprandial ghrelin did show small decreases at 26 and 52 weeks after RYGB, but these changes were not statistically significant [102]. Thus, although the effects of RYGB on ghrelin are highly variable, a relative ghrelin deficiency compared with the expected rise due to hypophagia and weight loss appears to be a common observation (see also review by Pournaras [103]), keeping ghrelin on the list of major potential candidate mechanisms for the beneficial effects on weight loss after RYGB.
In our RYGB rat model, we did not detect decreases in fasting ghrelin levels compared to both sham-operated obese and lean control rats but the postprandial suppression of plasma ghrelin levels was significantly greater after RYGB (Fig. 6C). Furthermore, the expected counter-regulatory increase of ghrelin levels caused by hypophagia and weight loss after RYGB was not observed.
As suggested by Cummings [61], ghrelin secretion may be decreased after RYGB because of denervation of autonomic input to ghrelin cells in the stomach. The finding that fasting ghrelin levels precipitously decreased only one day after RYGB and then returned to normal levels may be interpreted as the acute effect of removal of a tonic stimulatory neural input [104]. Clearly, the entire gastric remnant containing most ghrelin cells is almost completely vagotomized and sympathectomized (Fig. 7). Preliminary studies showed smaller fasting-induced increases of plasma ghrelin in subdiaphragmatic vagotomized rats, and an acute suppression with atropine treatment in intact rats [105], and ghrelin does not stimulate food intake in patients with vagotomy [106], suggesting that vagal efferents may be involved in the tonic increase of ghrelin in the empty stomach. However, more selective vagotomies, both in terms of vagal branches supplying specific targets and separating afferents from efferents, as well as vagal stimulation studies of the vascularly perfused stomach will be necessary to shed more light on the mechanisms involved. The need for more mechanistic studies is also indicated by disparate findings regarding vagal involvement of prandial ghrelin suppression. While in humans, vagal stimulation by means of modified sham feeding was able to enhance ghrelin suppression by oral fat intake [107], vagotomy was without any effect on basal levels or on re-feeding-induced suppression of ghrelin in rats [105]. In light of the recent finding that electrical stimulation of sympathetic nerves supplying the upper abdominal viscera increases ghrelin concentration in portal blood, it is possible that the sympathetic nervous system may be more involved in the ghrelin spike during meal anticipation than the vagal system[108]. This interpretation is supported by the observation that noradrenalin stimulates ghrelin secretion through β1-adrenergic receptors [109,110] and that fasting-induced rises in circulating ghrelin levels are blocked in mice treated with reserpine to deplete adrenergic transmitters [110]. In addition, there is some evidence for cholinergic modulation of noradrenaline realease from sympathetic terminals in the stomach via nicotinic receptors [111,112]. Because the sympathetic innervation of the stomach is mainly provided via the periarterial plexus of the left gastric artery [113,114] entering the stomach near the cardia, it is eliminated in the bypassed part of the stomach and might explain low ghrelin levels observed by some studies.
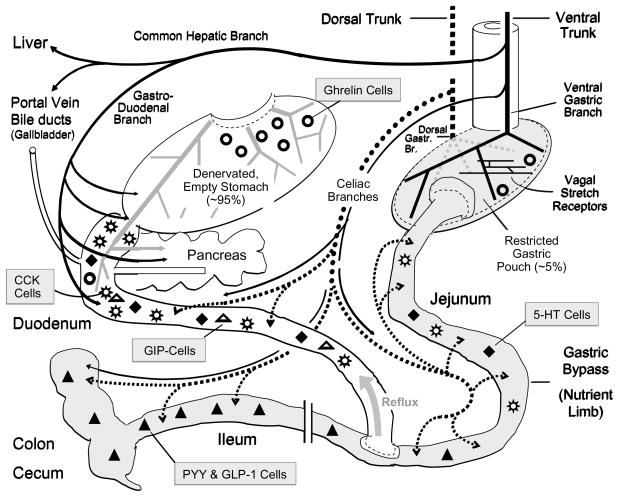
Fig. 7. Roux-en-Y gastric bypass surgery and vagal innervation of the gut and associated organs.
The nutrient limb of the Roux-en-Y gastric bypass consisting of the small gastric pouch and the anastomosed jejunum is shown on the right (shaded). The bilio-pancreatic limb including the large gastric remnant with attached duodenum and proximal jejunum is shown on the left. Note that the stomach remnant is depicted at a much reduced size for clarity. The ventral (anterior) and dorsal (posterior) vagal trunks and their branches are shown as solid and dotted lines, respectively. The relative density and distribution of enteroendocrine cells secreting peptide hormones or transmitters are depicted by different symbols as indicated.
Ghrelin O-acyl transferase (GOAT), the enzyme responsible for ghrelin acylation, has recently gained much attention as an important modulator of ghrelin function and a promising target for anti-obesity drug development [115,116]. It will be interesting to examine changes in GOAT activity in the stomach and other tissues after RYGB.
Together, lack of ghrelin secretion remains an attractive explanation for the success of RYGB in decreasing food intake and deserves further study. At this time it appears more likely that ghrelin suppression is due to interference with neural inputs to ghrelin cells rather than nutrient regulation.
3.3 Other hormones and satiety factors
Increased cholecystokinin signaling at CCK-1 receptors on vagal afferents could plausibly explain the drastically reduced meal size discussed above. However, few attempts have been made to measure meal-stimulated CCK release and plasma levels after RYGB and the findings are inconsistent. There were no changes in plasma CCK levels 6 months after surgery in morbidly obese patients [117] and 3 months after RYGB in high-fat diet-induced obese rats[21]. In contrast, both basal and meal-stimulated levels of CCK were elevated 20 years after jejunoileal bypass in massively obese patients [118]. Because it was recently demonstrated that CCK-58 has greater potency than CCK-8 in suppressing food intake [119], it will be interesting to look for levels of CCK-58 after RYGB.
Apolipoprotein A-IV (ApoA-IV), Oleylethanolamide (OEA), and N-acetylphosphatidylethanolamide (NAPE) are phospholipids secreted by the fed small intestine shown to act as satiety factors [120–122]. Increased secretion of these factors could potentially explain RYGB-induced early satiety and hypophagia. Interestingly, secretion of ApoA-IV was found to be increased several-fold, mainly from the bypassed small intestine, 17 months after RYGB[123]. OEA and NAPE production after RYGB have not yet been looked at. OEA mediates fat-induced satiety by engaging type-alpha peroxisome proliferator-activated receptors (PPAR-alpha), possibly located on vagal afferents, and activation of the brain oxytocin system [124–126]. Interestingly, we found a majority of meal-induced c-Fos positive neurons in the paraventricular nucleus of the hypothalamus in RYGB rats to express oxytocin (unpublished observations). Another fatty acid ethanolamide, anandamide, is best known to be a cannabinoid receptor-1 (CB1R) agonist and as such stimulates food intake[127]. Both OEA and anandamide are degraded by the fatty acid amide hydrolase (FAAH), and FAAH-deficiency promotes energy storage and appetite, suggesting that the accumulation of anandamide and its anabolic effects are dominant over the catabolic effects of OEA [128]. Because anandamide is down-regulated in muscle and liver in rats, reduced peripheral CB1R signaling may be involved in the metabolic improvements after RYGB[20].
Another factor overproduced by the Roux limb might be glucose [91]. In a mouse model of duodeno-jejunal bypass (without any gastric restriction), the two key gluconeogenic enzymes glucose-6-phosphatase and PEPCK were upregulated in the nutrient limb, possibly resulting in augmented glucose release into portal blood and overstimulation of a portal glucose sensor signaling satiety to the brain[129]. Ablation of sensory nerves in the hepatic portal vein in bypassed mice significantly attenuated hypophagia during the first 10 days after surgery [91].
Serum bile acid concentration is also elevated after RYGB [130] and bile acid signaling may be changed. Increased bile acid signaling has been demonstrated to induce energy expenditure via the cyclic-AMP-dependent thyroid hormone activating enzyme type 2 iodothyronine deiodinase [131] and to stimulate the secretion of GLP-1 [132]. Furthermore, circulating GLP-1 and PYY levels were positively, while ghrelin was negatively correlated with levels of bile acids after a mixed test meal in human subjects [133].
Finally, amylin, a hormone co-secreted with insulin from pancreatic beta cells and strongly implicated in the control of food intake, was significantly increased postprandially in our RYGB rats (Fig. 6F). Systemic administration of amylin suppresses food intake and chronic infusion attenuates the development of diet-induced obesity in rodents [134] (and see [135] for a recent review). Furthermore, preclinical and clinical studies suggest that amylin agonism restores leptin responsiveness in diet-induced obesity [136], and enhances the anorexic actions of PYY[3–36] [137]. Thus, amylin could play an important role in RYGB-induced anorexia and weight loss by its own effects on satiation, by synergizing with elevated PYY levels, and by restoring leptin sensitivity in the face of rapidly decreasing circulating leptin levels.
3.4 Glucose homeostasis
One of the hallmarks of RYGB is the rapid resolution of diabetes which appears to be at least partially independent of weight loss [138–140], but the mechanisms involved have been elusive [for an in-depth discussion see [141]]. Rubino and colleagues have demonstrated the usefulness of rat models by providing strong evidence for the involvement of an anti-incretin factor released from the upper intestine upon luminal contact with nutrients [142,143]. The upper intestinal hypothesis suggests that after RYGB less of this hypothetical anti-incretin is released because nutrients are no longer in contact with the upper intestine, resulting in improved insulin secretion. In contrast, the lower intestinal hypothesis suggests that the accelerated delivery of food to the Roux limb leads to exaggerated secretion of GLP-1, which strongly stimulates insulin secretion [144]. It seems clear that the improvement of glycemic control not only depends on increased insulin secretion, but equally on heightened insulin sensitivity. However, the responsible mechanisms are not well understood.
Although our diet-induced obese rats were not diabetic, their fasting glucose levels were slightly but significantly elevated. Postprandial glucose and insulin areas under the curve as well as HOMA-insulin resistance were about 2-fold higher compared with lean rats (Fig. 6D–F). This pre-diabetic state was fully prevented or reversed, 4 months after RYGB [69]. The increased early insulin response to a meal is consistent with a role for elevated GLP-1 after RYGB, but additional experiments with measurements of meal-induced hormone profiles at earlier time points after surgery will be necessary to sort out contributions of weight loss-dependent and independent effects on insulin secretion and insulin sensitivity. Computation of the HOMA index for insulin resistance showed that sham-operated, obese rats were significantly more insulin-resistant than both RYGB and lean controls. HOMA-IR significantly correlated with body weight change and absolute body weight.
4. Potential role of sensory and motor nerves
Besides hormones and other circulating factors, the gut communicates with the brain through primary visceral afferent nerve fibers comprised in the vagus and the dorsal root/spinal cord pathway. In return, the brain can affect gut function through the sympathetic and parasympathetic autonomic nervous systems (Fig. 1). Compared with the sympathetic motor and dorsal root afferent innervation via the spinal cord, the vagal innervation of the gut and associated organs has been studied much more thoroughly and will be the focus of the following discussion.
As shown in Fig. 7, not all three major vagal branches are equally affected by RYGB. The ventral and dorsal gastric branches distributing on the large gastric remnant are clearly cut by the gastrostomy procedure. Because some of these branches, traveling along the lesser curvature, also cross the pyloric sphincter and reach the proximal duodenum and parts of the pancreas [145–149], these areas are also partially vagotomized after RYGB surgery. Both vagal preganglionic efferent and afferent fibers are affected. However, the common hepatic branch originating from the left subdiaphragmatic trunk and innervating parts of the distal antrum, pylorus, proximal duodenum, and pancreas [30,146–150] should remain completely intact after RYGB. Similarly, the two celiac vagal branches traveling with the superior mesenteric artery and its subsidiaries, and supplying most of the small and large intestines from the distal duodenum on downwards should remain intact. Special care must be taken not to damage the dorsal celiac branch when carrying out the gastrostomy, as it exits the dorsal trunk very close to the gastric cardia. In a rat model, it was found that when the dorsal neurovascular bundle (near the division of the dorsal gastric and celiac branches) was intentionally transected, the RYGB procedure produced less suppression of food intake and body weight loss, but did not affect levels of GLP-1 and PYY [151]. However, there was no independent histological or functional verification of exactly which vagal fibers (entire dorsal vagal trunk or selectively the dorsal gastric or dorsal celiac branch) had been cut.
4.1. Sensory nerves
All three abdominal vagal branches (common hepatic, gastric, and celiac) carry satiety signals from various gut regions and the portal vein/liver to the brainstem [91,152–154], and much of this innervation remains intact after RYGB. There is evidence that vagal sensory fibers innervate the hepatic portal vein [155–157] and that glucose and GLP-1 sensors in the hepatic portal vein send a signal through the vagal hepatic branch to the brain [85,86]. It has been suggested that this sensor is responsible for food intake suppression caused by glucose derived from intestinal gluconeogenesis [129], and in a mouse model, capsaicin deafferentation of the hepatic portal vein resulted in rescue of initial hypophagia after RYGB surgery [91]. If increased signaling through such vagal afferents is involved, we expect that RYGB-induced hypophagia is at least partially rescued by specific elimination of afferent fibers in the common hepatic branch. We have recently tested this prediction in high-fat diet-induced obese Sprague Dawley rats that had undergone either RYGB alone, or RYGB in combination with common hepatic vagal branch transection [158]. However, we did not find any difference in body weight and composition, energy intake and expenditure, and food choice over the five months postsurgical observation period [158], suggesting that vagal afferents projecting through the common hepatic branch are not important for RYGB-induced weight loss. Furthermore, if the hepatic portal vein glucose sensor is important for RYGB-induced hypophagia as claimed by Troy et al.[91], its signals to the brain are not mediated by vagal afferents within the common hepatic branch. Because a small portion of vagal hepatic portal vein innervation is mediated by fibers originating from the right subdiaphragmatic trunk by way of the periarterial plexuses along the celiac and hepatic arteries [157], we cannot rule out their possible role. Also, because efferent fibers in the common hepatic vagal branch have been implicated in the control of hepatic glucose production and other liver functions [159,160], it is theoretically possible that their inadvertent transection may have occluded the expected effect of sensory fiber transection. The most parsimonious explanation for the findings of Troy et al. [91] is that the hepatic portal glucose sensor signals to the brain via dorsal root afferents and the spinal cord, but this speculation remains to be demonstrated.
Gut hormones such as CCK, PYY, GLP-1, and ghrelin can affect food intake by acting through vagal afferents [90,161–163]. Particularly GLP-1 and PYY, secreted from the proximal small intestine and colon, are likely acting in a paracrine fashion on mucosal vagal afferent nerve endings supplied by the paired celiac branches [164]. In addition, jejunal lipid infusions in rats also suppress food intake through a vagal-dependent mechanism [165]. Undigested nutrients directly entering the jejunum after RYGB are highly likely to excessively stimulate vagal afferents, sending stronger signals to the brain. In addition to chemical stimuli, mechanical overstimulation of the Roux and/or common limbs may generate exaggerated activation of vagal afferent mechanosensors, as discussed above [34]. This possibility is supported by our preliminary observation of exaggerated meal-induced neural activation in the nucleus of the solitary tract of RYGB rats (Fig. 4). To further test this hypothesis, we are currently combining RYGB surgery with selectively lesions of the sensory fibers in the celiac vagal branches innervating the jejunum, ileum, cecum, and colon.
Finally, it is also possible that over-stimulated vagal tension and stretch sensors in the gastric pouch send stronger signals to the brainstem and are partly responsible for RYGB-induced hypophagia and weight loss. In the rat and mouse, the highest density of intramuscular arrays (IMAs), thought to function as stretch sensors, is found in the gastric fundus [166]. Therefore, selective elimination of afferent fibers in the paired gastric branches could be expected to prevent early meal termination after RYGB surgery, possibly leading to higher total food intake. There are also a few reports suggesting that dorsal root/spinal afferents from the gut and portal vein contribute to the satiation process [167–170].
Vagal deafferentations do produce subtle increases in meal size [152,171,172], but because there is partial compensation by more frequent meals, it does not result in excessive body weight gain. From these observations it would appear that, compared to systems in the hypothalamus, vagal afferents play only a secondary role in the control of long-term food intake and energy balance. However, the methodologies used to manipulate vagal afferents are rudimentary at best, as they do not allow selective ablation or stimulation of functionally specific neurons. For example, given that ghrelin [161] and hyperglycemia [173] can suppress, while gastric distension and CCK [174] can increase firing activity of specific populations of vagal afferents, simply cutting or stimulating both populations should theoretically lead to cancellation of their central effects. By learning more about the functional specificity of vagal afferents and the availability of more selective tools to manipulate them, they can still be a worthwhile target for prevention or treatment of obesity. This view is enforced by emerging evidence that the impressive efficiency of bariatric surgery may, at least in part, be related to changes in gastrointestinal hormones acting on vagal afferents.
4.2. Autonomic (motor) innervation
Although vagal motor outflow does not directly affect food intake and energy expenditure, it can indirectly influence energy balance in several ways. First, the strength of vagal afferent signals from the stomach is a major determinant of satiation and hunger through control of gastric emptying and accommodation [30,146,147,159,160,175–177]. Through its control of intestinal transit time and motility, absorption rate and exposure of enteroendocrine cells to nutrients is determined, ultimately leading to changes in gastrointestinal and pancreatic hormone levels involved in satiation and hunger. Second, vagal motor innervation of the pancreas is in a strong position to indirectly affect energy balance by modulating secretion of islet hormones. Cephalic-vagal stimulation affects mainly the early meal-related release of insulin and is important for normal glucose tolerance [178,179]. Early or acute phase insulin secretion is suppressed in obese subjects and restored after RYGB [180], but vagal mediation has not been investigated under these conditions. The vagal preganglionic neurons projecting to interlobular pancreatic ganglia were identified by tracing [181], and functional studies in the rat demonstrated that they reach the pancreas mainly via the gastric and hepatic-gastroduodenal vagal branches [147,148,182,183]. Thus, damage to the gastric vagal branches as inflicted by RYGB could be expected to have a negative role on glucose homeostasis. Because improvement of glucose homeostasis is one of the hallmarks of RYGB, there must be rapid compensation through vagal input to the pancreas via the gastroduodenal branch or the increased incretin release.
As briefly discussed above, the role of autonomic (motor) innervation in modulating the release of gastrointestinal hormones is not completely understood. That gastrin release is strongly stimulated by vagal stimulation has been known for many years, but the role of the motor vagus in the release of ghrelin, CCK, GIP, GLP-1, PYY, ApoA-IV, and OEA is controversial [105,106,184,185], and the involvement in the beneficial effects of RYGB is unclear.
5. Conclusions and perspectives
Since the pioneering work of Henry S. Koopmans and colleagues thirty years ago, it is only recently that the “power of the gut” in co-determining energy homeostasis has come back into focus. The disappointment with finding effective drugs vis-à-vis the near “miraculous” healing by gastric bypass surgery of a cluster of diseases known as metabolic syndrome has brought back gastrointestinal physiology and gut-to-brain communication into the scientific limelight. Gastroenterologists, endocrinologists, neuroscientists, psychologists and surgeons alike, have come together to find out how the “miracle” works. Although a “smoking gun” has not yet been identified, there has been considerable progress in identifying the myriad of changes induced by bariatric surgeries.
Among the major candidate mechanisms, the lower gut hormones GLP-1 and PYY likely play a critical role, because they have the potential to affect energy balance by acting on both the food intake and energy expenditure side of the equation, and to affect glucose homeostasis by acting on both insulin secretion and insulin sensitivity. However, other gut hormones and factors such as ghrelin, CCK, ApoA-IV, OEA, and NAPE appear to gain interest as well. For all of these mediators of RYGB’s (and other bariatric surgeries’) beneficial effects, scientists feverishly look for answers to the following questions. (1) What mechanism(s) lead to changes in their secretion after surgery? This includes the potential roles of the gut microbiome, immune-signaling, inflammatory responses, autonomic innervation, and accelerated delivery of undigested chime to the lower gut. (2) How do these hormones and factors communicate with other relevant organs such as the brain, liver, muscle, and adipose tissue? This includes direct humoral communication and the role of sensory nerves. (3) What are the functional consequences of these changes in signaling from the gut to other organs? This includes characterization of the neural circuits affected and their behavioral, autonomic, and endocrine outputs. In addition, these mechanisms must be studied at the physiological and behavioral level as a function of time after surgery to capture the adaptive character of the “healing” process.
The potential rewards from this inquiry are huge. It will not only lead to identification of the essential component(s) of successful surgery, but also to the development of novel drugs and behavioral modifications in the fight against the metabolic syndrome.
Acknowledgments
Research supported by the National Institutes of Health, Grant DK047348 and DK 071082.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Li C, Ford ES, McGuire LC, Mokdad AH. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring) 2007;15(1):216–24. doi: 10.1038/oby.2007.505. [DOI] [PubMed] [Google Scholar]
- 2.Koopmans HS. Internal signals cause large changes in food intake in one-way crossed intestines rats. Brain Res Bull. 1985;14(6):595–603. doi: 10.1016/0361-9230(85)90109-1. [DOI] [PubMed] [Google Scholar]
- 3.Koopmans HS. An integrated organismic response to lower gut stimulation. Scand J Gastroenterol Suppl. 1983;82:143–53. [PubMed] [Google Scholar]
- 4.Koopmans HS, Sclafani A. Control of body weight by lower gut signals. Int J Obes. 1981;5(5):491–5. [PubMed] [Google Scholar]
- 5.Koopmans HS, Sclafani A, Fichtner C, Aravich PF. The effects of ileal transposition on food intake and body weight loss in VMH-obese rats. Am J Clin Nutr. 1982;35(2):284–93. doi: 10.1093/ajcn/35.2.284. [DOI] [PubMed] [Google Scholar]
- 6.Sclafani A, Koopmans HS, Vasselli JR, Reichman M. Effects of intestinal bypass surgery on appetite, food intake, and body weight in obese and lean rats. Am J Physiol. 1978;234(4):E389–98. doi: 10.1152/ajpendo.1978.234.4.E389. [DOI] [PubMed] [Google Scholar]
- 7.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med. 1995;332(10):621–8. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 8.Froidevaux F, Schutz Y, Christin L, Jequier E. Energy expenditure in obese women before and during weight loss, after refeeding, and in the weight-relapse period. Am J Clin Nutr. 1993;57(1):35–42. doi: 10.1093/ajcn/57.1.35. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz A, Doucet E. Relative changes in resting energy expenditure during weight loss: a systematic review. Obes Rev. 2010;11(7):531–47. doi: 10.1111/j.1467-789X.2009.00654.x. [DOI] [PubMed] [Google Scholar]
- 10.Redman LM, Heilbronn LK, Martin CK, de Jonge L, Williamson DA, Delany JP, Ravussin E. Metabolic and behavioral compensations in response to caloric restriction: implications for the maintenance of weight loss. PLoS ONE. 2009;4(2):e4377. doi: 10.1371/journal.pone.0004377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Buchwald H, Estok R, Fahrbach K, Banel D, Jensen MD, Pories WJ, Bantle JP, Sledge I. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248–256. e5. doi: 10.1016/j.amjmed.2008.09.041. [DOI] [PubMed] [Google Scholar]
- 12.Meguid MM, Ramos EJ, Suzuki S, Xu Y, George ZM, Das UN, Hughes K, Quinn R, Chen C, Marx W, et al. A surgical rat model of human Roux-en-Y gastric bypass. J Gastrointest Surg. 2004;8(5):621–30. doi: 10.1016/j.gassur.2004.02.003. [DOI] [PubMed] [Google Scholar]
- 13.Zheng H, Shin AC, Lenard NR, Townsend RL, Patterson LM, Sigalet DL, Berthoud HR. Meal patterns, satiety, and food choice in a rat model of Roux-en-Y gastric bypass surgery. Am J Physiol Regul Integr Comp Physiol. 2009;297(5):R1273–82. doi: 10.1152/ajpregu.00343.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sjostrom L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, Dahlgren S, Larsson B, Narbro K, Sjostrom CD, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004;351(26):2683–93. doi: 10.1056/NEJMoa035622. [DOI] [PubMed] [Google Scholar]
- 15.Stefater MA, Perez-Tilve D, Chambers AP, Wilson-Perez HE, Sandoval DA, Berger J, Toure M, Tschop M, Woods SC, Seeley RJ. Sleeve gastrectomy induces loss of weight and fat mass in obese rats, but does not affect leptin sensitivity. Gastroenterology. 2010;138(7):2426–36. 2436, e1–3. doi: 10.1053/j.gastro.2010.02.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nadreau E, Baraboi ED, Samson P, Blouin A, Hould FS, Marceau P, Biron S, Richard D. Effects of the biliopancreatic diversion on energy balance in the rat. Int J Obes (Lond) 2006;30(3):419–29. doi: 10.1038/sj.ijo.0803166. [DOI] [PubMed] [Google Scholar]
- 17.Chaston TB, Dixon JB, O’Brien PE. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes (Lond) 2007;31(5):743–50. doi: 10.1038/sj.ijo.0803483. [DOI] [PubMed] [Google Scholar]
- 18.Savastano S, Di Somma C, Angrisani L, Orio F, Longobardi S, Lombardi G, Colao A. Growth hormone treatment prevents loss of lean mass after bariatric surgery in morbidly obese patients: results of a pilot, open, prospective, randomized, controlled study. J Clin Endocrinol Metab. 2009;94(3):817–26. doi: 10.1210/jc.2008-1476. [DOI] [PubMed] [Google Scholar]
- 19.le Roux CW, Aylwin SJ, Batterham RL, Borg CM, Coyle F, Prasad V, Shurey S, Ghatei MA, Patel AG, Bloom SR. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, and improve metabolic parameters. Ann Surg. 2006;243(1):108–14. doi: 10.1097/01.sla.0000183349.16877.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Guijarro A, Osei-Hyiaman D, Harvey-White J, Kunos G, Suzuki S, Nadtochiy S, Brookes PS, Meguid MM. Sustained weight loss after Roux-en-Y gastric bypass is characterized by down regulation of endocannabinoids and mitochondrial function. Ann Surg. 2008;247(5):779–90. doi: 10.1097/SLA.0b013e318166fd5f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki S, Ramos EJ, Goncalves CG, Chen C, Meguid MM. Changes in GI hormones and their effect on gastric emptying and transit times after Roux-en-Y gastric bypass in rat model. Surgery. 2005;138(2):283–90. doi: 10.1016/j.surg.2005.05.013. [DOI] [PubMed] [Google Scholar]
- 22.Romanova IV, Ramos EJ, Xu Y, Quinn R, Chen C, George ZM, Inui A, Das U, Meguid MM. Neurobiologic changes in the hypothalamus associated with weight loss after gastric bypass. J Am Coll Surg. 2004;199(6):887–95. doi: 10.1016/j.jamcollsurg.2004.07.013. [DOI] [PubMed] [Google Scholar]
- 23.Stylopoulos N, Hoppin AG, Kaplan LM. Roux-en-Y gastric bypass enhances energy expenditure and extends lifespan in diet-induced obese rats. Obesity (Silver Spring) 2009;17(10):1839–47. doi: 10.1038/oby.2009.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guijarro A, Suzuki S, Chen C, Kirchner H, Middleton FA, Nadtochiy S, Brookes PS, Niijima A, Inui A, Meguid MM. Characterization of weight loss and weight regain mechanisms after Roux-en-Y gastric bypass in rats. Am J Physiol Regul Integr Comp Physiol. 2007;293(4):R1474–89. doi: 10.1152/ajpregu.00171.2007. [DOI] [PubMed] [Google Scholar]
- 25.Sugerman HJ, Kellum JM, Engle KM, Wolfe L, Starkey JV, Birkenhauer R, Fletcher P, Sawyer MJ. Gastric bypass for treating severe obesity. Am J Clin Nutr. 1992;55(2 Suppl):560S–566S. doi: 10.1093/ajcn/55.2.560s. [DOI] [PubMed] [Google Scholar]
- 26.Thirlby RC, Bahiraei F, Randall J, Drewnoski A. Effect of Roux-en-Y gastric bypass on satiety and food likes: the role of genetics. J Gastrointest Surg. 2006;10(2):270–7. doi: 10.1016/j.gassur.2005.06.012. [DOI] [PubMed] [Google Scholar]
- 27.Thomas JR, Marcus E. High and low fat food selection with reported frequency intolerance following Roux-en-Y gastric bypass. Obes Surg. 2008;18(3):282–7. doi: 10.1007/s11695-007-9336-3. [DOI] [PubMed] [Google Scholar]
- 28.Tichansky DS, Boughter JD, Jr, Madan AK. Taste change after laparoscopic Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding. Surg Obes Relat Dis. 2006;2(4):440–4. doi: 10.1016/j.soard.2006.02.014. [DOI] [PubMed] [Google Scholar]
- 29.Grundy D. Neuroanatomy of visceral nociception: vagal and splanchnic afferent. Gut. 2002;51 (Suppl 1):i2–5. doi: 10.1136/gut.51.suppl_1.i2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Berthoud HR, Blackshaw LA, Brookes SJ, Grundy D. Neuroanatomy of extrinsic afferents supplying the gastrointestinal tract. Neurogastroenterol Motil. 2004;16 (Suppl 1):28–33. doi: 10.1111/j.1743-3150.2004.00471.x. [DOI] [PubMed] [Google Scholar]
- 31.Whitson BA, Leslie DB, Kellogg TA, Maddaus MA, Buchwald H, Billington CJ, Ikramuddin S. Adipokine response in diabetics and nondiabetics following the Roux-en-Y gastric bypass: a preliminary study. J Surg Res. 2007;142(2):295–300. doi: 10.1016/j.jss.2007.03.036. [DOI] [PubMed] [Google Scholar]
- 32.Ding S, Chi MM, Scull BP, Rigby R, Schwerbrock NM, Magness S, Jobin C, Lund PK. High-fat diet: bacteria interactions promote intestinal inflammation which precedes and correlates with obesity and insulin resistance in mouse. PLoS One. 2010;5(8):e12191. doi: 10.1371/journal.pone.0012191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de La Serre CB, Ellis CL, Lee J, Hartman AL, Rutledge JC, Raybould HE. Propensity to high-fat diet-induced obesity in rats is associated with changes in the gut microbiota and gut inflammation. Am J Physiol Gastrointest Liver Physiol. 2010;299(2):G440–8. doi: 10.1152/ajpgi.00098.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bjorklund P, Laurenius A, Een E, Olbers T, Lonroth H, Fandriks L. Is the roux limb a determinant for meal size after gastric bypass surgery? Obes Surg. 2010;20(10):1408–14. doi: 10.1007/s11695-010-0192-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burge JC, Schaumburg JZ, Choban PS, DiSilvestro RA, Flancbaum L. Changes in patients’ taste acuity after Roux-en-Y gastric bypass for clinically severe obesity. J Am Diet Assoc. 1995;95(6):666–70. doi: 10.1016/S0002-8223(95)00182-4. [DOI] [PubMed] [Google Scholar]
- 36.Scruggs DM, Buffington C, Cowan GS., Jr Taste Acuity of the Morbidly Obese before and after Gastric Bypass Surgery. Obes Surg. 1994;4(1):24–28. doi: 10.1381/096089294765558854. [DOI] [PubMed] [Google Scholar]
- 37.Naslund E, Melin I, Gryback P, Hagg A, Hellstrom PM, Jacobsson H, Theodorsson E, Rossner S, Backman L. Reduced food intake after jejunoileal bypass: a possible association with prolonged gastric emptying and altered gut hormone patterns. Am J Clin Nutr. 1997;66(1):26–32. doi: 10.1093/ajcn/66.1.26. [DOI] [PubMed] [Google Scholar]
- 38.Olbers T, Bjorkman S, Lindroos A, Maleckas A, Lonn L, Sjostrom L, Lonroth H. Body composition, dietary intake, and energy expenditure after laparoscopic Roux-en-Y gastric bypass and laparoscopic vertical banded gastroplasty: a randomized clinical trial. Ann Surg. 2006;244(5):715–22. doi: 10.1097/01.sla.0000218085.25902.f8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berridge KC. Measuring hedonic impact in animals and infants: microstructure of affective taste reactivity patterns. Neurosci Biobehav Rev. 2000;24(2):173–98. doi: 10.1016/s0149-7634(99)00072-x. [DOI] [PubMed] [Google Scholar]
- 40.Bendsen NT, Hother AL, Jensen SK, Lorenzen JK, Astrup A. Effect of dairy calcium on fecal fat excretion: a randomized crossover trial. Int J Obes (Lond) 2008;32(12):1816–24. doi: 10.1038/ijo.2008.173. [DOI] [PubMed] [Google Scholar]
- 41.Coles LT, Moughan PJ, Awati A, Darragh AJ, Zou ML. Predicted apparent digestion of energy-yielding nutrients differs between the upper and lower digestive tracts in rats and humans. J Nutr. 2010;140(3):469–76. doi: 10.3945/jn.109.116293. [DOI] [PubMed] [Google Scholar]
- 42.Hogan S, Fleury A, Hadvary P, Lengsfeld H, Meier MK, Triscari J, Sullivan AC. Studies on the antiobesity activity of tetrahydrolipstatin, a potent and selective inhibitor of pancreatic lipase. Int J Obes. 1987;11 (Suppl 3):35–42. [PubMed] [Google Scholar]
- 43.Warne JP, Padilla BE, Horneman HF, Ginsberg AB, Pecoraro NC, Akana SF, Dallman MF. Metabolic and neuroendocrine consequences of a duodenal-jejunal bypass in rats on a choice diet. Ann Surg. 2009;249(2):269–76. doi: 10.1097/SLA.0b013e3181961d5d. [DOI] [PubMed] [Google Scholar]
- 44.Bueter M, Lowenstein C, Olbers T, Wang M, Cluny NL, Bloom SR, Sharkey KA, Lutz TA, le Roux CW. Gastric bypass increases energy expenditure in rats. Gastroenterology. 2010;138(5):1845–53. doi: 10.1053/j.gastro.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 45.Martin GR, Beck PL, Sigalet DL. Gut hormones, and short bowel syndrome: the enigmatic role of glucagon-like peptide-2 in the regulation of intestinal adaptation. World J Gastroenterol. 2006;12(26):4117–29. doi: 10.3748/wjg.v12.i26.4117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Amar J, Burcelin R, Ruidavets JB, Cani PD, Fauvel J, Alessi MC, Chamontin B, Ferrieres J. Energy intake is associated with endotoxemia in apparently healthy men. Am J Clin Nutr. 2008;87(5):1219–23. doi: 10.1093/ajcn/87.5.1219. [DOI] [PubMed] [Google Scholar]
- 47.Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes. 2008;57(6):1470–81. doi: 10.2337/db07-1403. [DOI] [PubMed] [Google Scholar]
- 48.Cani PD, Delzenne NM. The role of the gut microbiota in energy metabolism and metabolic disease. Curr Pharm Des. 2009;15(13):1546–58. doi: 10.2174/138161209788168164. [DOI] [PubMed] [Google Scholar]
- 49.Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature. 2006;444(7122):1027–31. doi: 10.1038/nature05414. [DOI] [PubMed] [Google Scholar]
- 50.Zhang H, DiBaise JK, Zuccolo A, Kudrna D, Braidotti M, Yu Y, Parameswaran P, Crowell MD, Wing R, Rittmann BE, et al. Human gut microbiota in obesity and after gastric bypass. Proc Natl Acad Sci U S A. 2009;106(7):2365–70. doi: 10.1073/pnas.0812600106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Furet JP, Kong LC, Tap J, Poitou C, Basdevant A, Bouillot JL, Mariat D, Corthier G, Dore J, Henegar C, et al. Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes. 2010;59(12):3049–57. doi: 10.2337/db10-0253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carrasco F, Papapietro K, Csendes A, Salazar G, Echenique C, Lisboa C, Diaz E, Rojas J. Changes in resting energy expenditure and body composition after weight loss following Roux-en-Y gastric bypass. Obes Surg. 2007;17(5):608–16. doi: 10.1007/s11695-007-9117-z. [DOI] [PubMed] [Google Scholar]
- 53.del Genio F, Alfonsi L, Marra M, Finelli C, del Genio G, Rossetti G, del Genio A, Contaldo F, Pasanisi F. Metabolic and nutritional status changes after 10% weight loss in severely obese patients treated with laparoscopic surgery vs integrated medical treatment. Obes Surg. 2007;17(12):1592–8. doi: 10.1007/s11695-007-9286-9. [DOI] [PubMed] [Google Scholar]
- 54.Das SK, Roberts SB, McCrory MA, Hsu LK, Shikora SA, Kehayias JJ, Dallal GE, Saltzman E. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr. 2003;78(1):22–30. doi: 10.1093/ajcn/78.1.22. [DOI] [PubMed] [Google Scholar]
- 55.de Castro Cesar M, de Lima Montebelo MI, Rasera I, Jr, de Oliveira AV, Jr, Gomes Gonelli PR, Aparecida Cardoso G. Effects of Roux-en-Y gastric bypass on resting energy expenditure in women. Obes Surg. 2008;18(11):1376–80. doi: 10.1007/s11695-008-9460-8. [DOI] [PubMed] [Google Scholar]
- 56.Tamboli RA, Hossain HA, Marks PA, Eckhauser AW, Rathmacher JA, Phillips SE, Buchowski MS, Chen KY, Abumrad NN. Body composition and energy metabolism following Roux-en-Y gastric bypass surgery. Obesity (Silver Spring) 2010;18(9):1718–24. doi: 10.1038/oby.2010.89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Flancbaum L, Choban PS, Bradley LR, Burge JC. Changes in measured resting energy expenditure after Roux-en-Y gastric bypass for clinically severe obesity. Surgery. 1997;122(5):943–9. doi: 10.1016/s0039-6060(97)90336-6. [DOI] [PubMed] [Google Scholar]
- 58.Rodieux F, Giusti V, D’Alessio DA, Suter M, Tappy L. Effects of gastric bypass and gastric banding on glucose kinetics and gut hormone release. Obesity (Silver Spring) 2008;16(2):298–305. doi: 10.1038/oby.2007.83. [DOI] [PubMed] [Google Scholar]
- 59.Atkinson RL, Brent EL. Appetite suppressant activity in plasma of rats after intestinal bypass surgery. Am J Physiol. 1982;243(1):R60–4. doi: 10.1152/ajpregu.1982.243.1.R60. [DOI] [PubMed] [Google Scholar]
- 60.Holst JJ. The physiology of glucagon-like peptide 1. Physiol Rev. 2007;87(4):1409–39. doi: 10.1152/physrev.00034.2006. [DOI] [PubMed] [Google Scholar]
- 61.Cummings DE, Overduin J, Foster-Schubert KE. Gastric bypass for obesity: mechanisms of weight loss and diabetes resolution. J Clin Endocrinol Metab. 2004;89(6):2608–15. doi: 10.1210/jc.2004-0433. [DOI] [PubMed] [Google Scholar]
- 62.Bose M, Olivan B, Teixeira J, Pi-Sunyer FX, Laferrere B. Do Incretins play a role in the remission of type 2 diabetes after gastric bypass surgery: What are the evidence? Obes Surg. 2009;19(2):217–29. doi: 10.1007/s11695-008-9696-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Korner J, Inabnet W, Conwell IM, Taveras C, Daud A, Olivero-Rivera L, Restuccia NL, Bessler M. Differential effects of gastric bypass and banding on circulating gut hormone and leptin levels. Obesity (Silver Spring) 2006;14(9):1553–61. doi: 10.1038/oby.2006.179. [DOI] [PubMed] [Google Scholar]
- 64.Morinigo R, Moize V, Musri M, Lacy AM, Navarro S, Marin JL, Delgado S, Casamitjana R, Vidal J. Glucagon-like peptide-1, peptide YY, hunger, and satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab. 2006;91(5):1735–40. doi: 10.1210/jc.2005-0904. [DOI] [PubMed] [Google Scholar]
- 65.Laferrere B, Teixeira J, McGinty J, Tran H, Egger JR, Colarusso A, Kovack B, Bawa B, Koshy N, Lee H, et al. Effect of weight loss by gastric bypass surgery versus hypocaloric diet on glucose and incretin levels in patients with type 2 diabetes. J Clin Endocrinol Metab. 2008;93(7):2479–85. doi: 10.1210/jc.2007-2851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Laferrere B, Heshka S, Wang K, Khan Y, McGinty J, Teixeira J, Hart AB, Olivan B. Incretin levels and effect are markedly enhanced 1 month after Roux-en-Y gastric bypass surgery in obese patients with type 2 diabetes. Diabetes Care. 2007;30(7):1709–16. doi: 10.2337/dc06-1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.le Roux CW, Welbourn R, Werling M, Osborne A, Kokkinos A, Laurenius A, Lonroth H, Fandriks L, Ghatei MA, Bloom SR, et al. Gut hormones as mediators of appetite and weight loss after Roux-en-Y gastric bypass. Ann Surg. 2007;246(5):780–5. doi: 10.1097/SLA.0b013e3180caa3e3. [DOI] [PubMed] [Google Scholar]
- 68.Meirelles K, Ahmed T, Culnan DM, Lynch CJ, Lang CH, Cooney RN. Mechanisms of glucose homeostasis after Roux-en-Y gastric bypass surgery in the obese, insulin-resistant Zucker rat. Ann Surg. 2009;249(2):277–85. doi: 10.1097/SLA.0b013e3181904af0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Shin AC, Zheng H, Townsend RL, Sigalet DL, Berthoud HR. Meal-induced hormone responses in a rat model of Roux-en-Y gastric bypass surgery. Endocrinology. 2010;151(4):1588–97. doi: 10.1210/en.2009-1332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Toft-Nielsen MB, Madsbad S, Holst JJ. Continuous subcutaneous infusion of glucagon-like peptide 1 lowers plasma glucose and reduces appetite in type 2 diabetic patients. Diabetes Care. 1999;22(7):1137–43. doi: 10.2337/diacare.22.7.1137. [DOI] [PubMed] [Google Scholar]
- 71.Chelikani PK, Haver AC, Reidelberger RD. Intravenous infusion of glucagon-like peptide-1 potently inhibits food intake, sham feeding, and gastric emptying in rats. Am J Physiol Regul Integr Comp Physiol. 2005;288(6):R1695–706. doi: 10.1152/ajpregu.00870.2004. [DOI] [PubMed] [Google Scholar]
- 72.Talsania T, Anini Y, Siu S, Drucker DJ, Brubaker PL. Peripheral exendin-4 and peptide YY(3–36) synergistically reduce food intake through different mechanisms in mice. Endocrinology. 2005;146(9):3748–56. doi: 10.1210/en.2005-0473. [DOI] [PubMed] [Google Scholar]
- 73.Ruttimann EB, Arnold M, Hillebrand JJ, Geary N, Langhans W. Intrameal hepatic portal and intraperitoneal infusions of glucagon-like peptide-1 reduce spontaneous meal size in the rat via different mechanisms. Endocrinology. 2009;150(3):1174–81. doi: 10.1210/en.2008-1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hayes MR, Skibicka KP, Grill HJ. Caudal brainstem processing is sufficient for behavioral, sympathetic and parasympathetic responses driven by peripheral and hindbrain glucagon-like-peptide-1 receptor stimulation. Endocrinology. 2008 doi: 10.1210/en.2007-1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Batterham RL, Heffron H, Kapoor S, Chivers JE, Chandarana K, Herzog H, Le Roux CW, Thomas EL, Bell JD, Withers DJ. Critical role for peptide YY in protein-mediated satiation and body-weight regulation. Cell Metab. 2006;4(3):223–33. doi: 10.1016/j.cmet.2006.08.001. [DOI] [PubMed] [Google Scholar]
- 76.Roth CL, Enriori PJ, Harz K, Woelfle J, Cowley MA, Reinehr T. Peptide YY is a regulator of energy homeostasis in obese children before and after weight loss. J Clin Endocrinol Metab. 2005;90(12):6386–91. doi: 10.1210/jc.2005-1357. [DOI] [PubMed] [Google Scholar]
- 77.le Roux CW, Batterham RL, Aylwin SJ, Patterson M, Borg CM, Wynne KJ, Kent A, Vincent RP, Gardiner J, Ghatei MA, et al. Attenuated peptide YY release in obese subjects is associated with reduced satiety. Endocrinology. 2006;147(1):3–8. doi: 10.1210/en.2005-0972. [DOI] [PubMed] [Google Scholar]
- 78.Korner J, Bessler M, Inabnet W, Taveras C, Holst JJ. Exaggerated glucagon-like peptide-1 and blunted glucose-dependent insulinotropic peptide secretion are associated with Roux-en-Y gastric bypass but not adjustable gastric banding. Surg Obes Relat Dis. 2007;3(6):597–601. doi: 10.1016/j.soard.2007.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Holdstock C, Zethelius B, Sundbom M, Karlsson FA, Eden Engstrom B. Postprandial changes in gut regulatory peptides in gastric bypass patients. Int J Obes (Lond) 2008;32(11):1640–6. doi: 10.1038/ijo.2008.157. [DOI] [PubMed] [Google Scholar]
- 80.Nakagawa A, Satake H, Nakabayashi H, Nishizawa M, Furuya K, Nakano S, Kigoshi T, Nakayama K, Uchida K. Receptor gene expression of glucagon-like peptide-1, but not glucose-dependent insulinotropic polypeptide, in rat nodose ganglion cells. Auton Neurosci. 2004;110(1):36–43. doi: 10.1016/j.autneu.2003.11.001. [DOI] [PubMed] [Google Scholar]
- 81.Berthoud HR, Patterson LM. Anatomical relationship between vagal afferent fibers and CCK-immunoreactive entero-endocrine cells in the rat small intestinal mucosa. Acta Anat (Basel) 1996;156(2):123–31. doi: 10.1159/000147837. [DOI] [PubMed] [Google Scholar]
- 82.D’Alessio D, Lu W, Sun W, Zheng S, Yang Q, Seeley R, Woods SC, Tso P. Fasting and postprandial concentrations of GLP-1 in intestinal lymph and portal plasma: evidence for selective release of GLP-1 in the lymph system. Am J Physiol Regul Integr Comp Physiol. 2007;293(6):R2163–9. doi: 10.1152/ajpregu.00911.2006. [DOI] [PubMed] [Google Scholar]
- 83.Tang-Christensen M, Vrang N, Larsen PJ. Glucagon-like peptide containing pathways in the regulation of feeding behaviour. Int J Obes Relat Metab Disord. 2001;25 (Suppl 5):S42–7. doi: 10.1038/sj.ijo.0801912. [DOI] [PubMed] [Google Scholar]
- 84.Vrang N, Phifer CB, Corkern MM, Berthoud HR. Gastric distension induces c-Fos in medullary GLP-1/2-containing neurons. Am J Physiol Regul Integr Comp Physiol. 2003;285(2):R470–8. doi: 10.1152/ajpregu.00732.2002. [DOI] [PubMed] [Google Scholar]
- 85.Vahl TP, Tauchi M, Durler TS, Elfers EE, Fernandes TM, Bitner RD, Ellis KS, Woods SC, Seeley RJ, Herman JP, et al. Glucagon-like peptide-1 (GLP-1) receptors expressed on nerve terminals in the portal vein mediate the effects of endogenous GLP-1 on glucose tolerance in rats. Endocrinology. 2007;148(10):4965–73. doi: 10.1210/en.2006-0153. [DOI] [PubMed] [Google Scholar]
- 86.Nakabayashi H, Nishizawa M, Nakagawa A, Takeda R, Niijima A. Vagal hepatopancreatic reflex effect evoked by intraportal appearance of tGLP-1. Am J Physiol. 1996;271(5 Pt 1):E808–13. doi: 10.1152/ajpendo.1996.271.5.E808. [DOI] [PubMed] [Google Scholar]
- 87.Tang-Christensen M, Larsen PJ, Goke R, Fink-Jensen A, Jessop DS, Moller M, Sheikh SP. Central administration of GLP-1-(7–36) amide inhibits food and water intake in rats. Am J Physiol. 1996;271(4 Pt 2):R848–56. doi: 10.1152/ajpregu.1996.271.4.R848. [DOI] [PubMed] [Google Scholar]
- 88.Sandoval DA, Bagnol D, Woods SC, D’Alessio DA, Seeley RJ. Arcuate GLP-1 receptors regulate glucose homeostasis but not food intake. Diabetes. 2008 doi: 10.2337/db07-1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ma X, Bruning J, Ashcroft FM. Glucagon-like peptide 1 stimulates hypothalamic proopiomelanocortin neurons. J Neurosci. 2007;27(27):7125–9. doi: 10.1523/JNEUROSCI.1025-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 90.Yamamoto H, Kishi T, Lee CE, Choi BJ, Fang H, Hollenberg AN, Drucker DJ, Elmquist JK. Glucagon-like peptide-1-responsive catecholamine neurons in the area postrema link peripheral glucagon-like peptide-1 with central autonomic control sites. J Neurosci. 2003;23(7):2939–46. doi: 10.1523/JNEUROSCI.23-07-02939.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Troy S, Soty M, Ribeiro L, Laval L, Migrenne S, Fioramonti X, Pillot B, Fauveau V, Aubert R, Viollet B, et al. Intestinal gluconeogenesis is a key factor for early metabolic changes after gastric bypass but not after gastric lap-band in mice. Cell Metab. 2008;8(3):201–11. doi: 10.1016/j.cmet.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 92.Shin YK, Martin B, Golden E, Dotson CD, Maudsley S, Kim W, Jang HJ, Mattson MP, Drucker DJ, Egan JM, et al. Modulation of taste sensitivity by GLP-1 signaling. J Neurochem. 2008 doi: 10.1111/j.1471-4159.2008.05397.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Merchenthaler I, Lane M, Shughrue P. Distribution of pre-pro-glucagon and glucagon-like peptide-1 receptor messenger RNAs in the rat central nervous system. J Comp Neurol. 1999;403(2):261–80. doi: 10.1002/(sici)1096-9861(19990111)403:2<261::aid-cne8>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 94.Adams SH, Lei C, Jodka CM, Nikoulina SE, Hoyt JA, Gedulin B, Mack CM, Kendall ES. PYY[3–36] administration decreases the respiratory quotient and reduces adiposity in diet-induced obese mice. J Nutr. 2006;136(1):195–201. doi: 10.1093/jn/136.1.195. [DOI] [PubMed] [Google Scholar]
- 95.Cummings DE, Weigle DS, Frayo RS, Breen PA, Ma MK, Dellinger EP, Purnell JQ. Plasma ghrelin levels after diet-induced weight loss or gastric bypass surgery. N Engl J Med. 2002;346(21):1623–30. doi: 10.1056/NEJMoa012908. [DOI] [PubMed] [Google Scholar]
- 96.Fruhbeck G, Diez Caballero A, Gil MJ. Fundus functionality and ghrelin concentrations after bariatric surgery. N Engl J Med. 2004;350(3):308–9. doi: 10.1056/NEJM200401153500323. [DOI] [PubMed] [Google Scholar]
- 97.Tritos NA, Mun E, Bertkau A, Grayson R, Maratos-Flier E, Goldfine A. Serum ghrelin levels in response to glucose load in obese subjects post-gastric bypass surgery. Obes Res. 2003;11(8):919–24. doi: 10.1038/oby.2003.126. [DOI] [PubMed] [Google Scholar]
- 98.Korner J, Bessler M, Cirilo LJ, Conwell IM, Daud A, Restuccia NL, Wardlaw SL. Effects of Roux-en-Y gastric bypass surgery on fasting and postprandial concentrations of plasma ghrelin, peptide YY, and insulin. J Clin Endocrinol Metab. 2005;90(1):359–65. doi: 10.1210/jc.2004-1076. [DOI] [PubMed] [Google Scholar]
- 99.Stylopoulos N, Davis P, Pettit JD, Rattner DW, Kaplan LM. Changes in serum ghrelin predict weight loss after Roux-en-Y gastric bypass in rats. Surg Endosc. 2005;19(7):942–6. doi: 10.1007/s00464-004-8825-x. [DOI] [PubMed] [Google Scholar]
- 100.Stoeckli R, Chanda R, Langer I, Keller U. Changes of body weight and plasma ghrelin levels after gastric banding and gastric bypass. Obes Res. 2004;12(2):346–50. doi: 10.1038/oby.2004.43. [DOI] [PubMed] [Google Scholar]
- 101.Holdstock C, Engstrom BE, Ohrvall M, Lind L, Sundbom M, Karlsson FA. Ghrelin and adipose tissue regulatory peptides: effect of gastric bypass surgery in obese humans. J Clin Endocrinol Metab. 2003;88(7):3177–83. doi: 10.1210/jc.2002-021734. [DOI] [PubMed] [Google Scholar]
- 102.Korner J, Inabnet W, Febres G, Conwell IM, McMahon DJ, Salas R, Taveras C, Schrope B, Bessler M. Prospective study of gut hormone and metabolic changes after adjustable gastric banding and Roux-en-Y gastric bypass. Int J Obes (Lond) 2009;33(7):786–95. doi: 10.1038/ijo.2009.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Pournaras DJ, le Roux CW. Ghrelin and metabolic surgery. Int J Pept. 2010:2010. doi: 10.1155/2010/217267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Sundbom M, Holdstock C, Engstrom BE, Karlsson FA. Early changes in ghrelin following Roux-en-Y gastric bypass: influence of vagal nerve functionality? Obes Surg. 2007;17(3):304–10. doi: 10.1007/s11695-007-9056-8. [DOI] [PubMed] [Google Scholar]
- 105.Williams DL, Grill HJ, Cummings DE, Kaplan JM. Vagotomy dissociates short- and long-term controls of circulating ghrelin. Endocrinology. 2003;144(12):5184–7. doi: 10.1210/en.2003-1059. [DOI] [PubMed] [Google Scholar]
- 106.le Roux CW, Neary NM, Halsey TJ, Small CJ, Martinez-Isla AM, Ghatei MA, Theodorou NA, Bloom SR. Ghrelin does not stimulate food intake in patients with surgical procedures involving vagotomy. J Clin Endocrinol Metab. 2005;90(8):4521–4. doi: 10.1210/jc.2004-2537. [DOI] [PubMed] [Google Scholar]
- 107.Heath RB, Jones R, Frayn KN, Robertson MD. Vagal stimulation exaggerates the inhibitory ghrelin response to oral fat in humans. J Endocrinol. 2004;180(2):273–81. doi: 10.1677/joe.0.1800273. [DOI] [PubMed] [Google Scholar]
- 108.Mundinger TO, Cummings DE, Taborsky GJ., Jr Direct stimulation of ghrelin secretion by sympathetic nerves. Endocrinology. 2006;147(6):2893–901. doi: 10.1210/en.2005-1182. [DOI] [PubMed] [Google Scholar]
- 109.Hosoda H, Kangawa K. The autonomic nervous system regulates gastric ghrelin secretion in rats. Regul Pept. 2008;146(1–3):12–8. doi: 10.1016/j.regpep.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 110.Zhao TJ, Sakata I, Li RL, Liang G, Richardson JA, Brown MS, Goldstein JL, Zigman JM. Ghrelin secretion stimulated by {beta}1-adrenergic receptors in cultured ghrelinoma cells and in fasted mice. Proc Natl Acad Sci U S A. 2010;107(36):15868–73. doi: 10.1073/pnas.1011116107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Yokotani K, Wang M, Okada S, Murakami Y, Hirata M. Characterization of nicotinic acetylcholine receptor-mediated noradrenaline release from the isolated rat stomach. Eur J Pharmacol. 2000;402(3):223–9. doi: 10.1016/s0014-2999(00)00533-1. [DOI] [PubMed] [Google Scholar]
- 112.Yokotani K, Okada S, Murakami Y, Nakamura K. Nicotinic receptors involved in gastric noradrenaline release evoked by electrical stimulation of the splanchnic nerve in rats. Eur J Pharmacol. 2001;423(2–3):149–55. doi: 10.1016/s0014-2999(01)01114-1. [DOI] [PubMed] [Google Scholar]
- 113.McSwiney BA, Robson JM. The sympathetic innervation of the stomach: II. The effect of stimulation of the peri-arterial nerves on the stomach and small intestine. J Physiol. 1931;71(2):194–200. doi: 10.1113/jphysiol.1931.sp002725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jacobowitz D. Histochemical studies of the autonomic innervation of the gut. J Pharmacol Exp Ther. 1965;149(3):358–64. [PubMed] [Google Scholar]
- 115.Barnett BP, Hwang Y, Taylor MS, Kirchner H, Pfluger PT, Bernard V, Lin YY, Bowers EM, Mukherjee C, Song WJ, et al. Glucose and weight control in mice with a designed ghrelin O-acyltransferase inhibitor. Science. 2010;330(6011):1689–92. doi: 10.1126/science.1196154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Romero A, Kirchner H, Heppner K, Pfluger PT, Tschop MH, Nogueiras R. GOAT: the master switch for the ghrelin system? Eur J Endocrinol. 2010;163(1):1–8. doi: 10.1530/EJE-10-0099. [DOI] [PubMed] [Google Scholar]
- 117.Kellum JM, Kuemmerle JF, O’Dorisio TM, Rayford P, Martin D, Engle K, Wolf L, Sugerman HJ. Gastrointestinal hormone responses to meals before and after gastric bypass and vertical banded gastroplasty. Ann Surg. 1990;211(6):763–70. doi: 10.1097/00000658-199006000-00016. discussion 770–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Naslund E, Gryback P, Hellstrom PM, Jacobsson H, Holst JJ, Theodorsson E, Backman L. Gastrointestinal hormones and gastric emptying 20 years after jejunoileal bypass for massive obesity. Int J Obes Relat Metab Disord. 1997;21(5):387–92. doi: 10.1038/sj.ijo.0800418. [DOI] [PubMed] [Google Scholar]
- 119.Glatzle J, Raybould HE, Kueper MA, Reeve JR, Jr, Zittel TT. Cholecystokinin-58 is more potent in inhibiting food intake than cholecystokinin-8 in rats. Nutr Neurosci. 2008;11(2):69–74. doi: 10.1179/147683008X301432. [DOI] [PubMed] [Google Scholar]
- 120.Rodriguez de Fonseca F, Navarro M, Gomez R, Escuredo L, Nava F, Fu J, Murillo-Rodriguez E, Giuffrida A, LoVerme J, Gaetani S, et al. An anorexic lipid mediator regulated by feeding. Nature. 2001;414(6860):209–12. doi: 10.1038/35102582. [DOI] [PubMed] [Google Scholar]
- 121.Tso P, Liu M, John Kalogeris T, Thomson AB. The role of apolipoprotein a-iv in the regulation of food intake. Annu Rev Nutr. 2001;21:231–54. doi: 10.1146/annurev.nutr.21.1.231. [DOI] [PubMed] [Google Scholar]
- 122.Gillum MP, Zhang D, Zhang XM, Erion DM, Jamison RA, Choi C, Dong J, Shanabrough M, Duenas HR, Frederick DW, et al. N-acylphosphatidylethanolamine, a gut-derived circulating factor induced by fat ingestion, inhibits food intake. Cell. 2008;135(5):813–24. doi: 10.1016/j.cell.2008.10.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Culnan DM, Cooney RN, Stanley B, Lynch CJ. Apolipoprotein A-IV, a putative satiety/antiatherogenic factor, rises after gastric bypass. Obesity (Silver Spring) 2009;17(1):46–52. doi: 10.1038/oby.2008.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Campolongo P, Roozendaal B, Trezza V, Cuomo V, Astarita G, Fu J, McGaugh JL, Piomelli D. Fat-induced satiety factor oleoylethanolamide enhances memory consolidation. Proc Natl Acad Sci U S A. 2009;106(19):8027–31. doi: 10.1073/pnas.0903038106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Gaetani S, Fu J, Cassano T, Dipasquale P, Romano A, Righetti L, Cianci S, Laconca L, Giannini E, Scaccianoce S, et al. The fat-induced satiety factor oleoylethanolamide suppresses feeding through central release of oxytocin. J Neurosci. 2010;30(24):8096–101. doi: 10.1523/JNEUROSCI.0036-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Schwartz GJ, Fu J, Astarita G, Li X, Gaetani S, Campolongo P, Cuomo V, Piomelli D. The lipid messenger OEA links dietary fat intake to satiety. Cell Metab. 2008;8(4):281–8. doi: 10.1016/j.cmet.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Gaetani S, Kaye WH, Cuomo V, Piomelli D. Role of endocannabinoids and their analogues in obesity and eating disorders. Eat Weight Disord. 2008;13(3):e42–8. [PubMed] [Google Scholar]
- 128.Tourino C, Oveisi F, Lockney J, Piomelli D, Maldonado R. FAAH deficiency promotes energy storage and enhances the motivation for food. Int J Obes (Lond) 2010;34(3):557–68. doi: 10.1038/ijo.2009.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mithieux G, Misery P, Magnan C, Pillot B, Gautier-Stein A, Bernard C, Rajas F, Zitoun C. Portal sensing of intestinal gluconeogenesis is a mechanistic link in the diminution of food intake induced by diet protein. Cell Metab. 2005;2(5):321–9. doi: 10.1016/j.cmet.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 130.Patti ME, Houten SM, Bianco AC, Bernier R, Larsen PR, Holst JJ, Badman MK, Maratos-Flier E, Mun EC, Pihlajamaki J, et al. Serum bile acids are higher in humans with prior gastric bypass: potential contribution to improved glucose and lipid metabolism. Obesity (Silver Spring) 2009;17(9):1671–7. doi: 10.1038/oby.2009.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Watanabe M, Houten SM, Mataki C, Christoffolete MA, Kim BW, Sato H, Messaddeq N, Harney JW, Ezaki O, Kodama T, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439(7075):484–9. doi: 10.1038/nature04330. [DOI] [PubMed] [Google Scholar]
- 132.Katsuma S, Hirasawa A, Tsujimoto G. Bile acids promote glucagon-like peptide-1 secretion through TGR5 in a murine enteroendocrine cell line STC-1. Biochem Biophys Res Commun. 2005;329(1):386–90. doi: 10.1016/j.bbrc.2005.01.139. [DOI] [PubMed] [Google Scholar]
- 133.Roberts RE, Glicksman C, Alaghband-Zadeh J, Sherwood RA, Akuji N, le Roux CW. The relationship between postprandial bile acid concentration, GLP-1, PYY and ghrelin. Clin Endocrinol (Oxf) 2010;74(1):67–72. doi: 10.1111/j.1365-2265.2010.03886.x. [DOI] [PubMed] [Google Scholar]
- 134.Mack C, Wilson J, Athanacio J, Reynolds J, Laugero K, Guss S, Vu C, Roth J, Parkes D. Pharmacological actions of the peptide hormone amylin in the long-term regulation of food intake, food preference, and body weight. Am J Physiol Regul Integr Comp Physiol. 2007;293(5):R1855–63. doi: 10.1152/ajpregu.00297.2007. [DOI] [PubMed] [Google Scholar]
- 135.Lutz TA. Control of food intake and energy expenditure by amylin-therapeutic implications. Int J Obes (Lond) 2009;33 (Suppl 1):S24–7. doi: 10.1038/ijo.2009.13. [DOI] [PubMed] [Google Scholar]
- 136.Roth JD, Roland BL, Cole RL, Trevaskis JL, Weyer C, Koda JE, Anderson CM, Parkes DG, Baron AD. Leptin responsiveness restored by amylin agonism in diet-induced obesity: evidence from nonclinical and clinical studies. Proc Natl Acad Sci U S A. 2008;105(20):7257–62. doi: 10.1073/pnas.0706473105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Roth JD, Coffey T, Jodka CM, Maier H, Athanacio JR, Mack CM, Weyer C, Parkes DG. Combination therapy with amylin and peptide YY[3–36] in obese rodents: anorexigenic synergy and weight loss additivity. Endocrinology. 2007;148(12):6054–61. doi: 10.1210/en.2007-0898. [DOI] [PubMed] [Google Scholar]
- 138.Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, Hamad G, Eid GM, Mattar S, Ramanathan R, Barinas-Mitchel E, et al. Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg. 2003;238(4):467–84. doi: 10.1097/01.sla.0000089851.41115.1b. discussion 84–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Wickremesekera K, Miller G, Naotunne TD, Knowles G, Stubbs RS. Loss of insulin resistance after Roux-en-Y gastric bypass surgery: a time course study. Obes Surg. 2005;15(4):474–81. doi: 10.1381/0960892053723402. [DOI] [PubMed] [Google Scholar]
- 140.Ali MR, Fuller WD, Rasmussen J. Detailed description of early response of metabolic syndrome after laparoscopic Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2009;5(3):346–51. doi: 10.1016/j.soard.2008.10.014. [DOI] [PubMed] [Google Scholar]
- 141.Cummings DE. Endocrine mechanisms mediating remission of diabetes after gastric bypass surgery. Int J Obes (Lond) 2009;33 (Suppl 1):S33–40. doi: 10.1038/ijo.2009.15. [DOI] [PubMed] [Google Scholar]
- 142.Moo TA, Rubino F. Gastrointestinal surgery as treatment for type 2 diabetes. Curr Opin Endocrinol Diabetes Obes. 2008;15(2):153–8. doi: 10.1097/MED.0b013e3282f88a0a. [DOI] [PubMed] [Google Scholar]
- 143.Rubino F. Is type 2 diabetes an operable intestinal disease? A provocative yet reasonable hypothesis. Diabetes Care. 2008;31 (Suppl 2):S290–6. doi: 10.2337/dc08-s271. [DOI] [PubMed] [Google Scholar]
- 144.Holst JJ. Glucagonlike peptide 1: a newly discovered gastrointestinal hormone. Gastroenterology. 1994;107(6):1848–55. doi: 10.1016/0016-5085(94)90831-1. [DOI] [PubMed] [Google Scholar]
- 145.Kressel M, Berthoud HR, Neuhuber WL. Vagal innervation of the rat pylorus: an anterograde tracing study using carbocyanine dyes and laser scanning confocal microscopy. Cell Tissue Res. 1994;275(1):109–23. doi: 10.1007/BF00305379. [DOI] [PubMed] [Google Scholar]
- 146.Berthoud HR, Carlson NR, Powley TL. Topography of efferent vagal innervation of the rat gastrointestinal tract. Am J Physiol. 1991;260(1 Pt 2):R200–7. doi: 10.1152/ajpregu.1991.260.1.R200. [DOI] [PubMed] [Google Scholar]
- 147.Berthoud HR, Fox EA, Powley TL. Localization of vagal preganglionics that stimulate insulin and glucagon secretion. Am J Physiol. 1990;258(1 Pt 2):R160–8. doi: 10.1152/ajpregu.1990.258.1.R160. [DOI] [PubMed] [Google Scholar]
- 148.Berthoud HR, Powley TL. Identification of vagal preganglionics that mediate cephalic phase insulin response. Am J Physiol. 1990;258(2 Pt 2):R523–30. doi: 10.1152/ajpregu.1990.258.2.R523. [DOI] [PubMed] [Google Scholar]
- 149.Stavney LS, Kato T, Griffith CA, Nyhus LM, Harkins HN. A Physiologic Study of Motility Changes Following Selective Gastric Vagotomy. J Surg Res. 1963;23:390–4. doi: 10.1016/s0022-4804(63)80064-5. [DOI] [PubMed] [Google Scholar]
- 150.Berthoud HR, Fox EA, Powley TL. Abdominal pathways and central origin of rat vagal fibers that stimulate gastric acid. Gastroenterology. 1991;100(3):627–37. doi: 10.1016/0016-5085(91)80006-u. [DOI] [PubMed] [Google Scholar]
- 151.Bueter M, Lowenstein C, Ashrafian H, Hillebrand J, Bloom SR, Olbers T, Lutz T, le Roux CW. Vagal sparing surgical technique but not stoma size affects body weight loss in rodent model of gastric bypass. Obes Surg. 2010;20(5):616–22. doi: 10.1007/s11695-010-0075-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Schwartz GJ, Salorio CF, Skoglund C, Moran TH. Gut vagal afferent lesions increase meal size but do not block gastric preload-induced feeding suppression. Am J Physiol. 1999;276(6 Pt 2):R1623–9. doi: 10.1152/ajpregu.1999.276.6.R1623. [DOI] [PubMed] [Google Scholar]
- 153.Phillips RJ, Powley TL. Gastric volume detection after selective vagotomies in rats. Am J Physiol. 1998;274(6 Pt 2):R1626–38. doi: 10.1152/ajpregu.1998.274.6.R1626. [DOI] [PubMed] [Google Scholar]
- 154.Berthoud H-R. The caudal brainstem and the control of food intake and energy balance. In: Stricker EM, Woods SC, editors. Handbook of Behavioral Neurobiology. Vol. 14. New York: Plenum; 2004. pp. 195–240. [Google Scholar]
- 155.Berthoud HR, Neuhuber WL. In: Distribution and morphology of vagal afferents supplying the digestive system. Tache Y, Wingate DL, Burks TF, editors. Boca Raton: CRC Press; 1994. pp. 43–66. [Google Scholar]
- 156.Berthoud HR, Neuhuber WL. Functional and chemical anatomy of the afferent vagal system. Auton Neurosci. 2000;85(1–3):1–17. doi: 10.1016/S1566-0702(00)00215-0. [DOI] [PubMed] [Google Scholar]
- 157.Berthoud HR, Kressel M, Neuhuber WL. An anterograde tracing study of the vagal innervation of rat liver, portal vein and biliary system. Anat Embryol (Berl) 1992;186(5):431–42. doi: 10.1007/BF00185458. [DOI] [PubMed] [Google Scholar]
- 158.Shin ACZH, Berthoud HR. Vagal innervation of portal hepatic vein and liver is not necessary for Roux-en-Y gastric bypass surgery-induced hypophagia, weight loss, and hypermetabolism. Ann Surg. 2011 doi: 10.1097/SLA.0b013e31823e71b7. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Wang PY, Caspi L, Lam CK, Chari M, Li X, Light PE, Gutierrez-Juarez R, Ang M, Schwartz GJ, Lam TK. Upper intestinal lipids trigger a gut-brain-liver axis to regulate glucose production. Nature. 2008;452(7190):1012–6. doi: 10.1038/nature06852. [DOI] [PubMed] [Google Scholar]
- 160.German J, Kim F, Schwartz GJ, Havel PJ, Rhodes CJ, Schwartz MW, Morton GJ. Hypothalamic leptin signaling regulates hepatic insulin sensitivity via a neurocircuit involving the vagus nerve. Endocrinology. 2009;150(10):4502–11. doi: 10.1210/en.2009-0445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Date Y, Murakami N, Toshinai K, Matsukura S, Niijima A, Matsuo H, Kangawa K, Nakazato M. The role of the gastric afferent vagal nerve in ghrelin-induced feeding and growth hormone secretion in rats. Gastroenterology. 2002;123(4):1120–8. doi: 10.1053/gast.2002.35954. [DOI] [PubMed] [Google Scholar]
- 162.Koda S, Date Y, Murakami N, Shimbara T, Hanada T, Toshinai K, Niijima A, Furuya M, Inomata N, Osuye K, et al. The role of the vagal nerve in peripheral PYY3–36-induced feeding reduction in rats. Endocrinology. 2005;146(5):2369–75. doi: 10.1210/en.2004-1266. [DOI] [PubMed] [Google Scholar]
- 163.Abbott CR, Monteiro M, Small CJ, Sajedi A, Smith KL, Parkinson JR, Ghatei MA, Bloom SR. The inhibitory effects of peripheral administration of peptide YY(3–36) and glucagon-like peptide-1 on food intake are attenuated by ablation of the vagal-brainstem-hypothalamic pathway. Brain Res. 2005;1044(1):127–31. doi: 10.1016/j.brainres.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 164.Berthoud HR, Kressel M, Raybould HE, Neuhuber WL. Vagal sensors in the rat duodenal mucosa: distribution and structure as revealed by in vivo DiI-tracing. Anat Embryol (Berl) 1995;191(3):203–12. doi: 10.1007/BF00187819. [DOI] [PubMed] [Google Scholar]
- 165.Cox JE, Kelm GR, Meller ST, Spraggins DS, Randich A. Truncal and hepatic vagotomy reduce suppression of feeding by jejunal lipid infusions. Physiol Behav. 2004;81(1):29–36. doi: 10.1016/j.physbeh.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 166.Wang FB, Powley TL. Topographic inventories of vagal afferents in gastrointestinal muscle. J Comp Neurol. 2000;421(3):302–24. [PubMed] [Google Scholar]
- 167.Zittel TT, Lloyd KC, Rothenhofer I, Wong H, Walsh JH, Raybould HE. Calcitonin gene-related peptide and spinal afferents partly mediate postoperative colonic ileus in the rat. Surgery. 1998;123(5):518–27. doi: 10.1067/msy.1998.88090. [DOI] [PubMed] [Google Scholar]
- 168.Sclafani A, Ackroff K, Schwartz GJ. Selective effects of vagal deafferentation and celiac-superior mesenteric ganglionectomy on the reinforcing and satiating action of intestinal nutrients. Physiol Behav. 2003;78(2):285–94. doi: 10.1016/s0031-9384(02)00968-x. [DOI] [PubMed] [Google Scholar]
- 169.Anil MH, Forbes JM. The roles of hepatic nerves in the reduction of food intake as a consequence of intraportal sodium propionate administration in sheep. Q J Exp Physiol. 1988;73(4):539–46. doi: 10.1113/expphysiol.1988.sp003174. [DOI] [PubMed] [Google Scholar]
- 170.Deutsch JA, Jang Ahn S. The splanchnic nerve and food intake regulation. Behav Neural Biol. 1986;45(1):43–7. doi: 10.1016/s0163-1047(86)80004-8. [DOI] [PubMed] [Google Scholar]
- 171.Kelly L, Morales S, Smith BK, Berthoud HR. Capsaicin-treated rats permanently overingest low- but not high-concentration sucrose solutions. Am J Physiol Regul Integr Comp Physiol. 2000;279(5):R1805–12. doi: 10.1152/ajpregu.2000.279.5.R1805. [DOI] [PubMed] [Google Scholar]
- 172.Powley TL, Chi MM, Baronowsky EA, Phillips RJ. Gastrointestinal tract innervation of the mouse: afferent regeneration and meal patterning after vagotomy. Am J Physiol Regul Integr Comp Physiol. 2005;289(2):R563–R574. doi: 10.1152/ajpregu.00167.2005. [DOI] [PubMed] [Google Scholar]
- 173.Niijima A. Glucose-sensitive afferent nerve fibres in the hepatic branch of the vagus nerve in the guinea-pig. J Physiol. 1982;332:315–23. doi: 10.1113/jphysiol.1982.sp014415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Schwartz GJ, McHugh PR, Moran TH. Gastric loads and cholecystokinin synergistically stimulate rat gastric vagal afferents. Am J Physiol. 1993;265(4 Pt 2):R872–6. doi: 10.1152/ajpregu.1993.265.4.R872. [DOI] [PubMed] [Google Scholar]
- 175.van den Hoek AM, van Heijningen C, Schroder-van der Elst JP, Ouwens DM, Havekes LM, Romijn JA, Kalsbeek A, Pijl H. Intracerebroventricular administration of neuropeptide Y induces hepatic insulin resistance via sympathetic innervation. Diabetes. 2008;57(9):2304–10. doi: 10.2337/db07-1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Berthoud HR, Hennig G, Campbell M, Volaufova J, Costa M. Video-based spatio-temporal maps for analysis of gastric motility in vitro: effects of vagal stimulation in guinea-pigs. Neurogastroenterol Motil. 2002;14(6):677–688. doi: 10.1046/j.1365-2982.2002.00369.x. [DOI] [PubMed] [Google Scholar]
- 177.Berthoud HR, Powley TL. Characteristics of gastric and pancreatic responses to vagal stimulation with varied frequencies: evidence for different fiber calibers? J Auton Nerv Syst. 1987;19(1):77–84. doi: 10.1016/0165-1838(87)90147-0. [DOI] [PubMed] [Google Scholar]
- 178.Trimble ER, Berthoud HR, Siegel EG, Jeanrenaud B, Renold AE. Importance of cholinergic innervation of the pancreas for glucose tolerance in the rat. Am J Physiol. 1981;241(5):E337–41. doi: 10.1152/ajpendo.1981.241.5.E337. [DOI] [PubMed] [Google Scholar]
- 179.Siegel EG, Trimble ER, Renold AE, Berthoud HR. Importance of preabsorptive insulin release on oral glucose tolerance: studies in pancreatic islet transplanted rats. Gut. 1980;21(11):1002–9. doi: 10.1136/gut.21.11.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Polyzogopoulou EV, Kalfarentzos F, Vagenakis AG, Alexandrides TK. Restoration of euglycemia and normal acute insulin response to glucose in obese subjects with type 2 diabetes following bariatric surgery. Diabetes. 2003;52(5):1098–103. doi: 10.2337/diabetes.52.5.1098. [DOI] [PubMed] [Google Scholar]
- 181.Berthoud HR, Powley TL. Morphology and distribution of efferent vagal innervation of rat pancreas as revealed with anterograde transport of Dil. Brain Res. 1991;553(2):336–41. doi: 10.1016/0006-8993(91)90846-n. [DOI] [PubMed] [Google Scholar]
- 182.Berthoud HR, Bereiter DA, Trimble ER, Siegel EG, Jeanrenaud B. Cephalic phase, reflex insulin secretion. Neuroanatomical and physiological characterization. Diabetologia. 1981;20 (Suppl):393–401. doi: 10.1007/BF00254508. [DOI] [PubMed] [Google Scholar]
- 183.Wang J, Zheng H, Berthoud HR. Functional vagal input to chemically identified neurons in pancreatic ganglia as revealed by Fos expression. Am J Physiol. 1999;277(5 Pt 1):E958–64. doi: 10.1152/ajpendo.1999.277.5.E958. [DOI] [PubMed] [Google Scholar]
- 184.Berthoud HR, Trimble ER, Moody AJ. Lack of gastric inhibitory polypeptide (GIP) response to vagal stimulation in the rat. Peptides. 1982;3(6):907–12. doi: 10.1016/0196-9781(82)90059-6. [DOI] [PubMed] [Google Scholar]
- 185.Rocca AS, Brubaker PL. Role of the vagus nerve in mediating proximal nutrient-induced glucagon-like peptide-1 secretion. Endocrinology. 1999;140(4):1687–94. doi: 10.1210/endo.140.4.6643. [DOI] [PubMed] [Google Scholar]