Abstract
A 46-year-old gentleman, being investigated for symptoms of generalised weakness, low-grade fever and weight loss, was found to have a large, infiltrative mass of the liver on CT scan. The radiological impression was that of advanced hepatic malignancy with involvement of lesser curve of the stomach and regional lymph nodes. Multiple biopsy attempts failed to yield an adequate tissue sample for histopathological diagnosis. Surgery was planned for left hemihepatectomy with resection of the hepatogastric ligament and partial gastrectomy. Frozen section of a peroperative tissue sample confirmed the diagnosis of hepatic tuberculosis (TB). The granulomatous area was debrided and anti-TB treatment was started postoperatively. Recovery was unremarkable and the patient is currently asymptomatic.
Background
While tuberculosis (TB) itself is a common disease, isolated TB of the liver is a rare entity. The presented case demonstrates the difficulty of diagnosing this condition in spite of a complete investigation, due to its non-specific clinical and radiological appearances.
Case presentation
A 46-year-old Information Technology analyst first presented with 3 months complaints of low-grade fever, night sweats and mild exertional breathlessness. The symptoms worsened over time and were accompanied by fatigue and loss of weight of approximately 3 kg. There were no specific clinical findings. Haematology, coagulation profile, liver and renal functions were within normal limits.
At this stage the differential diagnosis of lymphoma with B symptoms was considered and a CT scan was requested. Viral hepatitis was ruled out by serological testing (ELISA), and although possibility of other parasitic and helminthic infestations was considered, it was a lower priority at this stage due to absence of a significant contributory history of exposure.
Investigations
Plain CT scan of the abdomen showed an 8 cm solid, poorly enhancing mass in segment II and IV of the liver, which extended into the liver capsule. The mass was contiguous with a 30 mm × 37 mm lymph node mass in the gastrohepatic ligament which encased the left gastric artery. The adjacent wall of the lesser curve of the stomach was markedly thickened and showed low attenuation change in keeping with necrosis (figure 1). The features were thought to suggest an advanced malignancy of hepatic or gastric origin. There was no evidence of malignant disease elsewhere in the peritoneal cavity or viscera. An ultrasound-guided biopsy of this mass was recommended. However, the mass was found to be inaccessible for safe percutaneous biopsy and this was not attempted.
Figure 1.

Coronal reformat contrast enhanced CT of abdomen.
Upper gastrointestinal endoscopy was attempted as an alternative method to obtain tissue for histological diagnosis. It showed the gastric cardia to be situated at 40 cm from the incisor teeth, with mildly thickened and inflamed mucosa at 45 cm. Biopsies were taken from this area but histopathological examination of these was inconclusive.
Finally, a diagnostic laparoscopy was performed to visualise the liver mass, and multiple percutaneous core biopsies were obtained under direct visualisation. These also failed to yield a definite diagnosis.
MRI of the mass was done to further characterise the lesion (figure 2), and the case was reviewed by the hepato-pancreato-biliary multi-disciplinary team.
Figure 2.
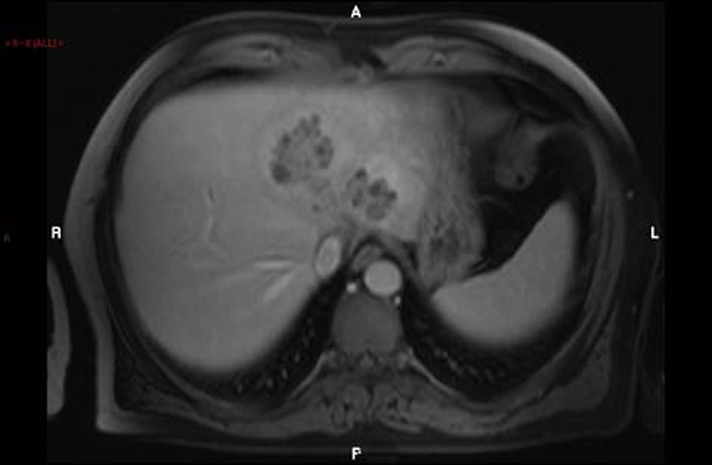
T1-weighted postcontrast MRI.
Differential diagnosis
The provisional diagnosis on the basis of initial history and clinical examination was lymphoma with B symptoms. Although a differential diagnoses of bacterial, viral or parasitic infections was considered, it was kept at a low priority due to the lack of significant history suggesting exposure or foreign travel.
The findings of an abdominal mass on radiology made malignancy the primary diagnosis. The differential diagnoses now being considered included hepatic tumours (hepatocellular carcinoma), gastric adenocarcinoma or lymphoma. There was no evidence of disease elsewhere in the body and therefore the possibility this mass being metastatic was kept at a lower priority. Multiple attempts at obtaining histological diagnosis failed to yield a definite result.
Infectious causes were once again considered less likely because of the well-localised disease pattern with complete absence of effects in the respiratory or gastrointestinal tracts. For this reason, the biopsy specimens were not tested or cultured for infectious organisms.
Outcome and follow-up
In view of the young age of the patient and absence of comorbid conditions, a radical surgical excision of the mass by performing a left hemihepatectomy with partial gastrectomy and excision of hepaticogastric ligament was planned. During surgery, a small tissue sample was sent for frozen section examination and the report confirmed caseating granulation suggestive of TB (figure 3). The plan for radical surgery was altered and the liver was debulked of the granulomatous mass (figure 4).
Figure 3.
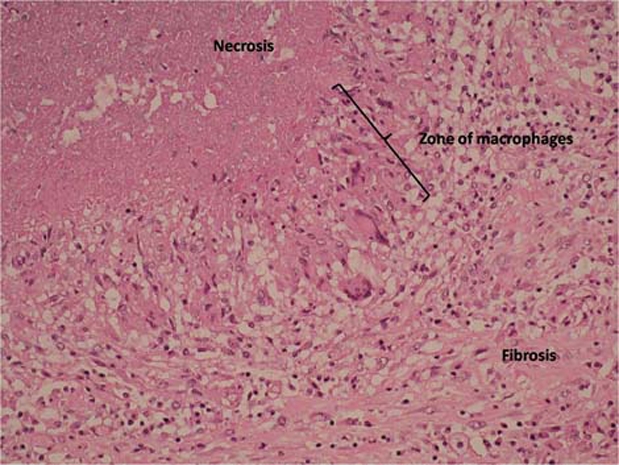
Microscopy of lesion showing a typical granuloma with surrounding fibrosis.
Figure 4.
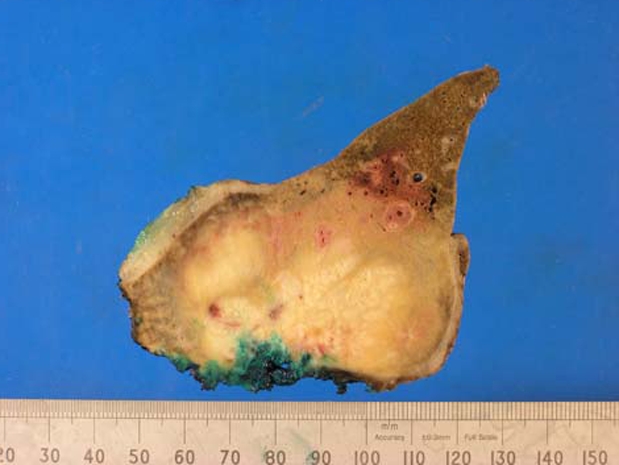
Resected specimen – stained for histopathology.
Anti-TB medication was commenced postoperatively under the advice of the Infectious Diseases Unit. Postoperative recovery was unremarkable. The patient is currently receiving anti-TB therapy and is asymptomatic.
Discussion
Infection with Mycobacterium tuberculosis is common, with almost one-third of the world’s population being affected at any given time.1 In 2006, approximately 9.2 million new TB cases were diagnosed worldwide, of which Africa and Southeast Asia accounted for about 3 million. An estimated 1.5 million deaths result from TB worldwide annually. There has been a global resurgence of TB since the AIDS epidemic of 1981 and development of multidrug-resistant TB strains.2 The United States has seen a 10-fold decline in TB incidence since 1953, and most of the new cases diagnosed are among the population born outside the USA. The UK demonstrates similar epidemiological trends, with the Health Protection Agency reporting 9153 new cases in a provisional report in 2009 (14.9 per 100 000 population).3
Researchers describe three morphological types of hepatic TB: (1) miliary TB associated with generalised miliary TB, (2) primary TB of the liver without involvement of other organs and (3) primary pyogenic lesion in the liver. The second and third varieties are the rarest,4 with only approximately 20 cases being reported in literature.
The clinical presentation of isolated liver TB is vague and without specific symptoms. Radiological appearances may mimic any of the common hepatic lesions such as tumours, haemangiomata,5 abcesses6 or cirrhosis.7 There is an association with immunodeficiency.8 M tuberculosis is not routinely looked for when cultures are requested on pus aspirated from hepatic abscesses, and the yield of Ziehl–Neilson stain in such cases is anyway low at best (0–45% positive only).9 The accepted criteria for the diagnosis of hepatic TB include (1) acid-fast bacillus in liver tissue, (2) tubercle bacilli elsewhere, plus hepatic granuloma with or without Langhans-type giant cells, and/or caseation, (3) typical macroscopic appearance on laparotomy or peritoneoscopy and (4) response to antituberculous therapy.10
Isolated liver TB does not usually merit a priority on the list of differential diagnoses for liver lesions since the pulmonary, miliary and even spinal TB are much more common forms of presentation. The fact that isolated liver TB does not produce characteristic symptoms, clinical signs or radiological appearances makes diagnosis more difficult. Finally, the necrosis produced by TB leads to inconclusive histopathological findings on small-sized tissue samples such as core biopsies and fine needle aspiration for cytology.
Learning points.
-
▶
Isolated hepatic TB is a rare but definite entity. Clinical signs, symptoms and radiological findings may often be unhelpful, while the finding of typical caseating granulomas on histopathology is only strongly suggestive of but not entirely specific for TB. A high index of suspicion is required before the diagnosis of TB can be considered in these circumstances.
-
▶
Even with the specific diagnosis of TB being considered, it is important to consider that the specific tests like the tuberculin skin test and T-SPOT.TB test can be falsely negative; cultures can take 4–6 weeks to produce results and the nucleic acid amplification tests (eg, PCR) require a minimum bacterial load, are complicated and expensive to run. All these issues make the diagnosis of TB a difficult one.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.The Merck Manuals Online Medical Library. Tuberculosis (TB), 2009. http://www.merck.com/mmpe/sec14/ch179/ch179b.html (accessed 10 March 2011).
- 2.Purl AS, Nayyar AK, Vij JC. Hepatic tuberculosis. Ind J Tub 1994;41:131–4 [Google Scholar]
- 3.Health Protection Agency Tuberculosis Update. UK: Health Protection Agency, 2010 [Google Scholar]
- 4.Spiegel CT, Tuazon CU. Tuberculous liver abscess. Tubercle 1984;65:127–31 [DOI] [PubMed] [Google Scholar]
- 5.Singh D, Singh S, Raut SB, et al. Isolated liver tuberculosis: a case report. Pediatr Surg Int 2004;20:727–8 [DOI] [PubMed] [Google Scholar]
- 6.Bangroo AK, Malhotra AS. Isolated hepatic tuberculosis. J Indian Assoc Pediatr Surg 2005;10:105–7 [Google Scholar]
- 7.Tai WC, Kuo CM, Lee CH, et al. Liver tuberculosis in Southern Taiwan: 15-years clinical experience. J Intern Med Taiwan 2008; 19:410–17 [Google Scholar]
- 8.Hassani KI, Ousadden A, Ankouz A, et al. Isolated liver tuberculosis abscess in a patient without immunodeficiency: A case report. World J Hepatol 2010;2:354–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen HC, Chao YC, Shyu RY, et al. Isolated tuberculous liver abscesses with multiple hyperechoic masses on ultrasound: a case report and review of the literature. Liver Int 2003;23:346–50 [DOI] [PubMed] [Google Scholar]
- 10.Maharaj B, Leary WP, Pudifin DJ. A prospective study of hepatic tuberculosis in 41 black patients. Q J Med 1987;63:517–22 [PubMed] [Google Scholar]


