Description
A 31-year-old Caucasian office worker who had received a liver transplanted 1 year earlier consulted for a painful ulcer located on the medial face of the right elbow (figure 1). Four months before, he fell while skiing (without direct cutaneous exposure) and developed a haematoma on the right elbow that never healed but fistulised and ulcerated. The lesion was solitary and there were no clinical signs of dissemination. White blood cell count and C reactive protein were within normal levels. Cryptococcal capsular antigen (CCA) was undetectable in serum. Microscopic examination of a skin biopsy specimen showed numerous encapsulated yeast forms amidst a dense dermal inflammatory infiltrate (figure 1). Cultures yielded C. neoformans var. neoformans (serotype D, identified using a monoclonal antibody specific for capsular polysaccharide).
Figure 1.
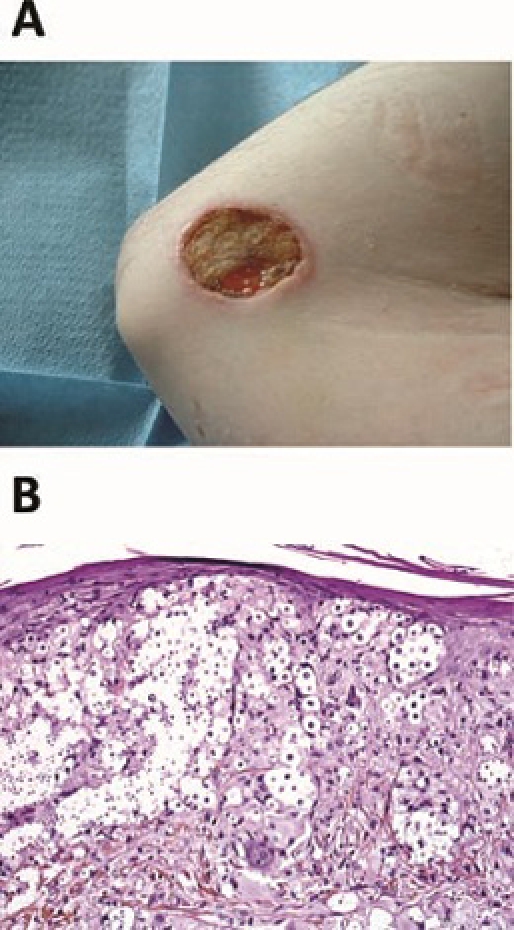
(A) 3.5×2.6 cm umbilicated, ulcerated lesion is seen on the right medial face of the elbow. (B) Microscopic examination shows multiple cryptococcal organisms within the dermis (haematoxylin-eosin-saffron staining, original magnification, ×400).
The patient was given fluconazole (6 mg/kg/d following a single loading dose of 12 mg/kg) and surgical debridement was performed. Tacrolimus dose was reduced by 50% because of drug interactions. The QTc-interval remained <420 ms and no hepatotoxicity occurred during treatment. Complete healing of the lesion was achieved within four months of treatment.
Primary cutaneous cryptococcosis (PCC) in transplant recipients is usually a localised disease, without evidence for dissemination based on undetectable CCA in serum and negative blood, urine and CSF cultures. PCC is characterised by a solitary lesion, predominantly developing on the upper limbs following a pre-existing skin traumatism due to outdoor hobbies/activities.1 2 Unlike disseminated cryptococcosis, most PCC cases are due to Cryptococcus neoformans var. neoformans.1 Treatment consists of systemic antifungal therapy with fluconazole, with or without surgical resection. Interactions with immunosuppressive drugs (mainly tacrolimus and ciclosporin) need to be considered.3 This treatment is usually effective, provided it is administered for 4 weeks to 4 months.1 2
Acknowledgments
The authors acknowledge Institut Pasteur, Unité de Mycologie Moléculaire, Centre National de Référence Mycologie et Antifongiques, Paris, France for serotyping.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Neuville S, Dromer F, Morin O, et al. Primary cutaneous cryptococcosis: a distinct clinical entity. Clin Infect Dis 2003;36:337–47 [DOI] [PubMed] [Google Scholar]
- 2.Sun HY, Alexander BD, Lortholary O, et al. Cutaneous cryptococcosis in solid organ transplant recipients. Med Mycol 2010;48:785–91 [DOI] [PubMed] [Google Scholar]
- 3.Mahnke CB, Sutton RM, Venkataramanan R, et al. Tacrolimus dosage requirements after initiation of azole antifungal therapy in pediatric thoracic organ transplantation. Pediatr Transplant 2003;7:474–8 [DOI] [PubMed] [Google Scholar]


