Abstract
Tarsal coalition is a congenital disturbance of hindfoot development. Talonavicular coalition is among the rarest forms of aberrant bony union of the tarsus. It frequently occurs bilaterally and in association with a number of skeletal deformities. Some patients are asymptomatic and the anomaly is discovered incidentally on plain radiographs. For others, a troublesome bony prominence will be the principle complaint and in a small proportion of patients marked foot and ankle pain with activity will prove debilitating. The authors describe the case of a 54-year-old male with bilateral foot pain spanning for nearly two decades. Symptom onset was insidious and at the time of presentation, he was limited to 10–15 min of mobilisation on flat ground.
Background
The incidence of tarsal coalition is 1–2%.1 2 Talonavicular coalitions are among the most uncommon and least documented of all coalitions of the tarsus.3 There is a strong genetic predisposition with talonavicular coalition inherited in an autosomal dominant pattern with high penetrance.4 It frequently occurs bilaterally and has been associated with a number of skeletal deformities including the great toe being shorter than the second, ball-and-socket ankle joint, carpal synostoses, peroneal spastic flat foot, symphalangisim and clinodactyly.5–8 Loss of the medial longitudinal arch places additional stress upon surrounding tendinous and soft-tissue structures and increases the load borne by adjacent bony articulations. The irregular bony configuration may precipitate inflammatory and degenerative changes within the foot and ankle leading to compensatory changes in joints proximal to the coalition. This case illustrates many of the unique features characteristic of talonavicular coalition including familial inheritance, associated skeletal abnormalities and degenerative bony changes both in the foot and at proximal articulations. The patient in question endured decades of discomfort before he was finally referred for specialist consultation. Had this process occurred sooner, measures could have been instituted to reduce his distress and promote an existence of pain-free mobility.
Case presentation
A 54-year-old gentleman presented to the orthopaedic outpatient clinic with insidious onset of a dull aching pain in both ankles and feet for nearly 20 years. He had been managed for these symptoms conservatively by his general practitioner with analgesics and physiotherapy. He continued to suffer constant pain despite these measures and struggled to mobilise – at the time of presentation he struggled to walk on uneven ground and walking on the flat was limited to 10–15 min. The pain was non-radiating and he denied any neurological symptoms.
The patient was born with bilateral symphalangism of the hands and feet requiring operative intervention. He had a lengthy orthopaedic history including patellectomies as a teenager following troublesome chondromalacia. He developed osteoarthritis of both hips and knees as an adult and at the time of presentation he was awaiting a left total knee replacement. He had also undergone bilateral arthroscopic shoulder decompression and surgical management for ingrowing toenails. His medical history included insulin-dependent diabetes mellitus, triple vessel coronary artery disease (optimised medically), epilepsy, recurrent epididymo-orchitis and previous orchidectomy for testicular cancer, peptic ulcer disease, possible pancreatic insufficiency and obesity. He reported a family history of tarsal coalition – his brother had surgery in the US for talonavicular coalition.
On examination, he was noted to have a stiff leg gait with mild pes planus of both feet. He was tender over the anteromedial and anterolateral aspects of both ankles with discomfort over the sinus tarsi and peronei of both feet. Range of motion in the ankle was limited with no dorsiflexion beyond neutral and 30° plantar flexion on both sides. Stiffness was noted in both subtalar joints with motion occurring instead at the midfoot bilaterally. There was no evidence of any tendon dysfunction and full power was seen in all myotomes of the lower limbs.
Investigations
Plain radiographs demonstrated bilateral complete talonavicular coalition with symphalangism of the phalanges (figure 1). There was a small accessory navicular on the left and evidence of a fused accessory navicular on the right (figures 2 and 3). CT of both feet confirmed the diagnosis of bilateral complete bony coalition of the talus and navicular.
Figure 1.

Anteroposterior radiograph demonstrating bilateral talonavicular coalition with accessory navicular on the left and fused accessory navicular on the right.
Figure 2.
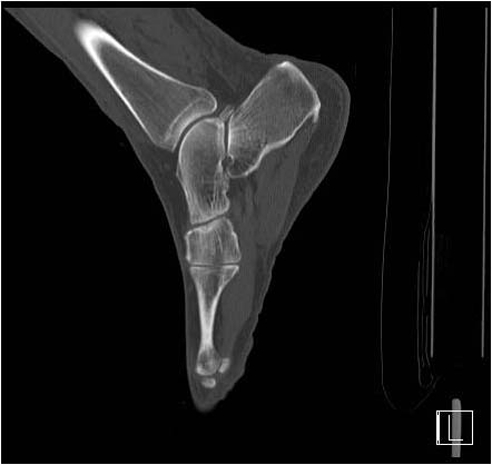
CT (sagittal view) right foot. Evidence of coalesced talus and navicular articulating with medial cuneiform.
Figure 3.

CT (sagittal view) of left foot. Evidence of coalesced talus and navicular articulating with medial cuneiform.
Outcome and follow-up
The patient was referred for orthotic assessment. Unfortunately, his health deteriorated in the interim and to date he has been unable to attend his scheduled appointment with the orthotist.
Discussion
First described by R J Anderson in 1879,9 talonavicular coalition is a congenital fusion of the talus and navicular with fibrous, cartilaginous or osseous tissue uniting the two bones. For many years it was widely accepted that tarsal coalition resulted from the incorporation of accessory ossicles into the neighbouring major tarsal bones.6 Proposed by Pfitzner in 1876, this theory held sway until 1955 when Harris identified coalitions in developing fetuses. Her discovery provided unequivocal support for the increasingly popular idea that a failure of differentiation of primitive mesenchyme lay behind the aberrant bony development.7
Around this time in the mid-1900s, evidence was mounting in the argument for hereditary transmission of tarsal coalitions. In 1935, Rothberg et al described a case of bilateral talonavicular coalition with presumed hereditary influence in a young female.9 Subsequent studies during the 1940s and 50s confirmed such findings but the most convincing evidence for genetic predisposition was provided in 1974 when Leonard identified tarsal coalitions in just under half of the 98 first degree relatives of 31 patients treated for peroneal spastic flat foot associated with tarsal coalition.7 His work revealed an autosomal dominant pattern of inheritance with high penetrance.4
The incidence of talonavicular coalition is unknown. The overall incidence of tarsal coalition has been estimated at 1–2%,1 2 with calcaneonavicular (53%) and talocalcaneal coalition (37%) the most common types10 – thus, talonavicular coalition represents 10% or less of this 1–2%. In 1984, there had been fewer than 35 cases of talonavicular coalition reported in the world literature6 and by 1998, this number had risen only slightly to 46.3
The symptoms of talonavicular coalition cover a broad spectrum. Some patients will be asymptomatic5 and the anomaly discovered incidentally on plain radiographs performed following minor trauma such as a sprain of the ankle. For others, a troublesome bony prominence will be the principle complaint3 and for a small proportion of patients, including our own patient, marked foot and ankle pain with activity will prove debilitating.
Characteristic radiographic changes seen with talonavicular coalition include absence of a well-circumscribed navicular or a decrease in talonavicular joint space, rounding of the naviculocuneiform joint and beaking of the navicular.3 While plain radiographs will often prove sufficient to make the diagnosis, further investigations may include CT to delineate the anatomy of the foot and plantar pressure or dynamic pressure studies to assess the biomechanics and guide management.
In the majority of patients, the mainstay of treatment will include conservative measures such as footwear modification and functional foot orthoses. In some cases, localised infiltration of steroid injections may provide relief but in patients for whom surgical intervention is required, excision of troublesome bony protuberances or limited foot arthrodesis may be undertaken. In extreme cases, pan-talar or ankle arthrodesis may be considered.
Learning points.
-
▶
Tarsal coalition occurs in up to 1 in 50 people
-
▶
Talonavicular coalition may be associated with other skeletal defects. These include abnormalities associated with imperfect mesenchymal septation such as symphalangism
-
▶
Talonavicular coalition is one of the rarest forms of tarsal coalition. Calcaneonavicular and talocalcaneal are the most common
-
▶
Talonavicular is a cause of chronic painful flat foot which may be amenable to surgery if conservative treatment with functional foot orthoses fails.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Resnik CS, Aiken MW, Kenzora JE. Case report 780. Fracture of talar beaks in tarsal coalition. Skeletal Radiol 1993;22:214–17 [DOI] [PubMed] [Google Scholar]
- 2.Yeates HA. Talonavicular synostosis. Ulster Med J 1980;49:165–8 [PMC free article] [PubMed] [Google Scholar]
- 3.David DR, Clark NE, Bier JA. Congenital talonavicular coalition. Review of the literature, case report, and orthotic management. J Am Podiatr Med Assoc 1998;88:223–7 [DOI] [PubMed] [Google Scholar]
- 4.Vincent KA. Tarsal coalition and painful flatfoot. J Am Acad Orthop Surg 1998;6:274–81 [DOI] [PubMed] [Google Scholar]
- 5.Doyle SM, Kumar SJ. Symptomatic talonavicular coalition. J Pediatr Orthop 1999;19:508–10 [DOI] [PubMed] [Google Scholar]
- 6.Mosier KM, Asher M. Tarsal coalitions and peroneal spastic flat foot. A review. J Bone Joint Surg Am 1984;66:976–84 [PubMed] [Google Scholar]
- 7.Leonard MA. The inheritance of tarsal coalition and its relationship to spastic flat foot. J Bone Joint Surg Br 1974;56B:520–6 [PubMed] [Google Scholar]
- 8.Migues A, Slullitel GA, Suárez E, et al. Case reports: symptomatic bilateral talonavicular coalition. Clin Orthop Relat Res 2009;467:288–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Challis J. Hereditary transmission of talonavicular coalition in association with anomaly of the little finger. J Bone Joint Surg Am 1974;56:1273–6 [PubMed] [Google Scholar]
- 10.Stormont DM, Peterson HA. The relative incidence of tarsal coalition. Clin Orthop Relat Res 1983;181:28–36 [PubMed] [Google Scholar]


