Abstract
The direct and interactive effects of neuroticism and stressful life events (chronic and episodic stressors) on the severity and temporal course of depression symptoms were examined in 826 outpatients with mood and anxiety disorders, assessed on three occasions over a one-year period (intake, 6- and 12-month follow-ups). Neuroticism, chronic stress, and episodic stress were uniquely associated with intake depression symptom severity. A significant interaction effect indicated that the strength of the effect of neuroticism on initial depression severity increased as chronic stress increased. Although neuroticism did not have a significant direct effect on the temporal course of depression symptoms, chronic stress significantly moderated this relationship such that neuroticism had an increasingly deleterious effect on depression symptom improvement as the level of chronic stress over follow-up increased. In addition, chronic stress over follow-up (but not episodic stress) was uniquely predictive of less depression symptom improvement. Consistent with a stress generation framework, however, initial depression symptom severity was positively associated with chronic stress during follow-up. The results are discussed in regard to diathesis-stress conceptual models of emotional disorders and the various roles of stressful life events in the onset, severity, and maintenance of depressive psychopathology.
Over the past several decades, sizeable literatures have accrued on the constructs that act as putative risk factors for unipolar depression. Although a number of vulnerability dimensions has been identified, a considerable portion of this research has focused on two constructs: neuroticism and stressful life events. Indeed, there are two largely separate literatures that attest to the empirical and conceptual significance of neuroticism and stressful life events in predicting the onset, severity, and course of depression (for reviews, see Hammen, 2005; Kessler, 1997; Mineka, Watson, & Clark, 1998). However, fewer studies have simultaneously examined the role of neuroticism and stressful life events on depression, and thus the nature of the relationships among these variables is not well understood. Moreover, most studies of life stress and depression have examined episodic stressors, despite recent indications of the relevance of ongoing strains in predicting the severity and course of depression symptoms. Thus, the goal of the present study was to examine the nature of the effects of neuroticism, chronic stress, and episodic stress on the severity and temporal course of depression symptoms in a large sample of outpatients with mood and anxiety disorders.
Neuroticism
Most prominent theories underscore neuroticism as a genetically based core dimension of temperament that is instrumental to the etiology and course of the mood disorders (e.g., Barlow, 2002; Mineka et al., 1998). Indeed, extensive evidence indicates that neuroticism is strongly heritable (e.g., Fanous, Gardner, Prescott, Cancro, & Kendler, 2002; Hettema, Prescott, & Kendler, 2004; Viken, Rose, Kaprio, & Koskenvuo, 1994), temporally stable (e.g., Costa & McCrae, 1988), and plays a key role in accounting for the severity, overlap, and maintenance of depression and anxiety (e.g., Bienvenu et al., 2001, 2004; Brown, 2007; Gershuny & Sher, 1998). Despite the considerable empirical efforts expended on this issue, the specific nature of the relationship between neuroticism and depression has remained elusive. For instance, although leading conceptualizations emphasize the possibility that neuroticism is a vulnerability to emotional disorders (a predispositional explanation; e.g., Barlow, 2002; Clark, 2005), most studies have not been methodologically equipped to address this hypothesis in a compelling fashion (e.g., inability to evaluate directional effects in cross-sectional designs; lack of premorbid assessment of neuroticism in studies using clinical samples). Given that conceptual models also posit that neuroticism predicts a poor prognosis for the treated and untreated course of emotional disorders (e.g., Mineka et al., 1998), longitudinal studies of clinical samples have addressed the nature of the relationship between temperament and psychopathology within a pathoplastic framework (i.e., temperament influences the course and expression of disorders). Several studies of this nature have emanated from treatment outcome research for major depression and dysthymia. These studies are based on the premise that because constructs such as neuroticism are construed as risk factors for depression, these dimensions should predict depression treatment outcome (i.e., high neuroticism is associated with poorer treatment response). However, whereas some studies have found that higher pre-treatment levels of neuroticism predict poorer outcomes for depression (e.g., Bock, Bukh, Vinberg, Gether, & Kessing, 2010; Hayden & Klein, 2001; Quilty et al., 2008), others have failed to support this relationship (e.g., Clark, Vittengl, Kraft, & Jarrett, 2003; Peterson et al., 2002).
Brown (2007) examined the longitudinal course and temporal structural relationships of dimensions of temperament (i.e., a latent variable defined by indicators of neuroticism and behavioral inhibition, N/BI, and a latent variable defined by indicators of behavioral activation and positive affect, BA/P) and selected DSM-IV disorder constructs (depression, social phobia, generalized anxiety disorder) in outpatients with anxiety and unipolar mood disorders (N = 606) who were assessed at intake, and one-year and two-year follow-ups. Most (76%) patients received treatment after intake, and thus the overall rate of anxiety and mood disorders declined over the follow-up period (e.g., 100% to 58% for intake and two-year follow-up, respectively). A series of parallel-process latent growth models indicated that, holding intake levels of the DSM-IV construct constant, initial levels of N/BI were associated with less improvement in social phobia and generalized anxiety disorder. However, neither N/BI or BA/P was predictive of the temporal course of depression. In view of theory and limited evidence that the effects of vulnerability on psychopathology are augmented by stressful life events, Brown (2007) raised the possibility that the influence of N/BI on the course of the DSM-IV disorder constructs was underestimated in this study due to the failure to include measures of life stress.
Indeed, in addition to the aforementioned methodological issues (e.g., over-reliance on cross-sectional designs), most studies to date have focused exclusively on the direct effects of neuroticism on depression. This is despite the fact that current conceptual models assert that dimensions of temperament do not act alone in determining the etiology, course, and complications of emotional disorders (e.g., Barlow, 2002). Specifically, such models espouse a “diathesis-stress” conceptualization such that vulnerable individuals (e.g., those high in neuroticism) are posited to be at higher risk for experiencing psychopathology in the context of triggering stressful events. Moreover, the construct of neuroticism itself has been conceptualized in part as the tendency to experience negative emotions and react adversely to stressors (e.g., Costa & McCrae, 1992). Along these lines, studies using nonclinical samples have found an interaction between neuroticism and daily stress/hassles in predicting negative affect over short-term periods (e.g., Hutchinson & Williams, 2007; Mroczek & Almeida, 2004). In a population-based sample of twins, Kendler, Kuhn, and Prescott (2004) found that individuals with high neuroticism were significantly more likely than individuals with low neuroticism to experience a major depressive episode when exposed to stressful life events.
Life Stress
A large literature has amassed on the role of life stress in the development and maintenance of depression. The consistent finding that stressful life events precede major depressive episodes has led many researchers to underscore the probable existence of a causal effect of stress on the onset of depression in vulnerable individuals (for reviews, see Hammen, 2005; Kessler, 1997; Mazure, 1998; Tennant, 2002). Evidence for a bidirectional relationship between stress and depression has also been obtained; specifically, that in addition to the precipitating effects of life stress on depression, depressed individuals are more likely to experience subsequent stressful events (i.e., stress generation; Hammen, 1991). Furthermore, concurrent stress (i.e., stressors during the study follow-up period) has been associated with poorer depression outcome over various follow-up periods in treatment outcome (e.g., Monroe, Kupfer, & Frank, 1992; Monroe, Roberts, Kupfer, & Frank, 1996; Zlotnick, Shea, Pilkonis, Elkin, & Ryan, 1996) and naturalistic studies (e.g., Lehmann, Fenton, Deutsch, Feldman, & Engelsmann, 1988; Spijker, Bijl, de Graaf, & Nolen, 2001), although some null findings have been reported (Monroe, Bellack, Hersen, & Himmelhoch, 1983; Wildes, Harkness, & Simons, 2002). Less consistent results have been obtained for the influence of antecedent stressors on the course and treatment outcome of depression. For instance, whereas some studies have found that pretreatment stressful events predict poorer response to depression treatment (e.g., Monroe et al., 1992, 1996), others have not (e.g., Monroe et al., 1983; Reno & Halaris, 1990).
Notably, most research on the relationship of life stress and depression has focused on episodic stressors (i.e., discrete life events such as the death of a loved one or automobile accident). In response to concerns that the field had erroneously neglected the potential effects of ongoing stressors (e.g., social isolation, family conflict, work dissatisfaction, financial hardship; Hammen, 2005), a smaller body of research has emerged on the role of chronic stress in predicting the onset and symptom severity of depression (e.g., Hammen, Kim, Eberhart, & Brennan, 2009; Hammen, Shih, & Brennan, 2004; Monroe, Slavich, Torres, & Gotlib, 2007; Muscatell, Slavich, Monroe, & Gotlib, 2009). Some evidence suggests that chronic stressors are more strongly predictive of depression symptom severity than episodic stressors (e.g., McGonagle & Kessler, 1990). Researchers have also raised the possibility that episodic and chronic stressors are differentially related to depression. For instance, many studies have found that episodic stress is more strongly associated with first episodes of depression than with depression recurrences (Hammen, 2005). Chronic stress, however, may be more germane to the maintenance of depressive episodes (Hayden & Klein, 2001; Moerk & Klein, 2000; Riso, Miyatake, & Thase, 2002). Yet, very few studies have examined the influence of chronic stress on the temporal course of depression. In a study of 97 patients with dysthymia, Hayden and Klein (2001) found that chronic stress during the follow-up period was a strong predictor of disorder non-recovery and depression symptom severity at five-year follow-up. This relationship was replicated in another investigation of this sample using a longer follow-up period (7.5 years; Dougherty, Klein, & Davila, 2004). However, these studies did not include measures of episodic stress, thereby precluding evaluation of the differential relevance of chronic and episodic stress in the prediction of the course of depression.
Studies Examining Both Neuroticism and Life Stress
By and large, two separate literatures have developed on the influence of neuroticism and life stress on the emergence and course of depression. However, a smaller set of studies have conducted simultaneous evaluations of these constructs. In addition to direct effects, these studies have often examined conceptually driven indirect and interactive effects of neuroticism and life stress on depression. Mediational models are based on the notion that neuroticism plays a role in stress generation (e.g., Bolger & Zuckerman, 1995; Fergusson & Horwood, 1987; Kendler, Gardner, & Prescott, 2003), and that these stressors subsequently lead to emotional distress (i.e., depression). In a general population sample, for instance, Ormel and Wohlfarth (1991) found that neuroticism exerted an indirect effect on general psychological distress though chronic stress (i.e., long-term difficulties) over an eight-year period. Similar findings have been obtained in briefer prospective studies that examined the relationships among neuroticism (or negative emotionality), episodic stressors (or daily life events), and symptoms of depression in adolescents and undergraduates (Hankin, 2010; Kercher, Rapee, & Schniering, 2009; Lakdawalla & Hankin, 2008; Wetter & Hankin, 2009). However, a study of elderly individuals failed to find that chronic or episodic stressors mediated the effect of neuroticism on depressive episode onset (Ormel, Oldenhinkel, & Brilman, 2001).
In accord with diathesis-stress models of psychopathology (i.e., life stress potentiates the effects of neuroticism), some studies have also evaluated the multiplicative effects of neuroticism, chronic stress, and episodic stress on depression. Evidence for moderating effects of episodic stress on the relationship between neuroticism and depression has been mixed. For example, significant neuroticism-episodic stress interactions have been obtained in the prediction of depression onset (e.g., Kendler et al., 2004; Ormel et al., 2001), but not the severity of depression symptoms (e.g., Hankin, 2010; Wetter & Hankin, 2008). Very few studies have considered the moderating effects of chronic stress on the relationship between neuroticism and depression. In an elderly sample, Ormel et al. (2001) found that individuals with high levels of neuroticism were at increased risk of depression onset if they were also experiencing long-term difficulties. Although Hayden and Klein (2001) found that higher levels of neuroticism and chronic stress were both associated with less improvement in depression among individuals with dysthymia, significant interaction effects were not reported. To our knowledge, no studies to date have simultaneously evaluated the roles of neuroticism, chronic and episodic stress, and their interaction in the prediction of the temporal course of depression in adult clinical samples.
Present Study
Accordingly, the present study examined the direct and interactive effects of neuroticism, chronic stress, and episodic stress on the severity and temporal course of depression symptoms in a large and diagnostically diverse sample of treatment-seeking outpatients who were followed over a one-year period. Based on prevailing research findings, it was predicted that chronic and episodic stress would be positively associated with initial depression severity, and that less improvement in depression would be seen in patients who experienced higher levels of life stress during the follow-up period (perhaps with stronger effects for chronic stress than episodic stress given the potentially greater relevance of chronic stress in depression maintenance; cf. Hayden & Klein, 2001; Moerk & Klein, 2000; Riso et al., 2002; Tennant, 2002). Although neuroticism was expected to have a significant unique association with initial depression severity, any effects of this dimension on the temporal course of depression (cf. Brown, 2007) would be significantly potentiated by the level of life stress experienced during the follow-up period (again, with the possibility that chronic stress would have a stronger moderating effect). Specifically, it was hypothesized that the deleterious effects of neuroticism on the course of depression would significantly increase as the level of exposure to life stress during follow-up increased. In addition to initial depression severity, these relationships were examined controlling for extraversion. Along with neuroticism, the construct of extraversion has been identified in conceptual models and research as a core dimension of temperament with specific relevance to mood disorders, as well as social phobia (e.g., Brown & Barlow, 2009; Mineka et al., 1998). Given the potential role of extraversion in accounting for individual differences in the severity and course of depression symptoms, a measure of this construct was included as an exogenous variable in the cross-sectional and longitudinal analyses (e.g., are direct and interactive effects of neuroticism and life stress on depression holding extraversion constant?).
Method
Participants
The sample consisted of 826 outpatients who presented for assessment or treatment at the Center for Anxiety and Related Disorders (CARD).1 Women constituted the larger portion of the sample (60.4%); average age was 33.62 (SD = 12.52, range = 18 to 79). The sample was predominantly Caucasian (86.3%; African-American = 4%, Asian = 4.8%, Latino/Hispanic = 4.5%). Intake diagnoses (Time 1, T1) were established with the Anxiety Disorders Interview Schedule for DSM-IV: Lifetime version (ADIS-IV-L; Di Nardo, Brown, & Barlow, 1994), a semi-structured interview designed to ascertain reliable diagnosis of the DSM-IV anxiety, mood, somatoform, and substance use disorders, and to screen for the presence of other conditions (e.g., psychotic disorders). Patients were re-evaluated at 6 months (Time 2, T2) and 12 months (Time 3, T3) using the follow-up version of the ADIS-IV which is identical to the ADIS-IV-L except: (a) sections for past diagnoses are omitted; and (b) a section is included to assess treatment follow-up (e.g., nature and extent of treatments received since intake). Both ADIS-IV versions provide dimensional assessment of the key and associated features of disorders (0–8 ratings); such features are dimensionally rated regardless of whether a formal DSM-IV diagnosis is under consideration. A reliability study entailing two independent administrations of the ADIS-IV-L indicated good-to-excellent interrater agreement for current disorders (range of κs = .67 to .86) except dysthymia (κ = .31; Brown, Di Nardo, Lehman, & Campbell, 2001). The rates of current clinical disorders occurring frequently in the sample at intake were: social phobia (47.6%), mood disorders (i.e., major depression, dysthymic disorder, depressive disorder NOS; 39.8%), generalized anxiety disorder (29.4%), panic disorder with or without agoraphobia (24.5%), obsessive-compulsive disorder (16.7%), and specific phobia (15.4%). Of the 329 cases with a current mood disorder, 251 had major depression (160 recurrent, 91 single episode), 64 had dysthymia (45 early onset), and 17 had depressive disorder NOS (total exceeds 329 because three cases were diagnosed with double depression).
Measures
Neuroticism and extraversion
Neuroticism and extraversion were assessed at intake with the NEO-Five Factor Inventory (NFFI; Costa & McCrae, 1992). The NFFI is a 60-item self-report measure of the five-factor model of personality. Items are comprised of self-descriptive statements (e.g., “I am not a worrier,” “I really enjoy talking to people”) rated on a five-point Likert scale (1 = strongly disagree to 5 = strongly agree). The five domain scores (e.g., neuroticism, NFFI-N; extraversion, NFFI-E) are calculated by summing their respective 12 item responses. The latent structure of the NFFI has been supported in clinical samples (Rosellini & Brown, in press) and each domain has been found to possess adequate internal consistency (α = .68 to .86, Costa & McRae, 1992) and temporal stability (e.g., in normal samples, rs = .86 to .90, Robins, Fraley, Roberts, & Trzesniewski, 2001).
Chronic and episodic life stress
Chronic and episodic life stress were assessed at intake and both follow-up evaluations using the UCLA Life Stress Interview (UCLA-LSI; Hammen et al., 1987). The UCLA-LSI is a semi-structured interview that assesses stress occurring over the prior six months in eight domains: social life, romantic relationships, family, work, school, finances, health of self, and health of others. Assessment of chronic stress in multiple domains has been emphasized by depression researchers (e.g., Mazure, 1998). As in prior longitudinal studies examining stress and depression outcomes (e.g., Hayden & Klein, 2001), the UCLA-LSI defines chronic stress as a strain lasting at least six months. Interviewers made a chronic stress rating for each domain on a five-point scale (1 = exceptionally positive circumstances to 5 = extremely adverse circumstances, in increments of .5) using descriptive behavioral anchors. Within the social life domain, for instance, a rating of “2” reflects having a number of friends, weekly socializing (e.g., in person or via telephone), diversity in activities, and good conflict resolution, while a rating of “4” would be used to describe a limited number of friends (e.g., one or two), infrequent social contact, engagement in limited social activities every few months, and poor conflict resolution. Chronic stress at intake (CSI) was a sum composite of the eight stress domain ratings assessed at T1; chronic stress during follow-up (CSF) was a composite of the stress domains collapsing the T2 and T3 assessments.
Episodic stress referred to any acute events that had occurred over the prior six months. Specifically, patients were asked if there had been “any particular event that had occurred” in a specific domain (i.e., social life, romantic relationships, family, etc.). When inquiring about episodic stressors, interviewers provided patients with examples of what would constitute a “particular event.” For example, interviews asked patients if any major arguments or separations had been present when assessing for episodic stress within social, romantic, and family domains. Within health domains (self and others), patients were asked if any acute illnesses, accidents, or injuries had occurred. In addition to assessment of episodic stress within the eight domains mentioned above, acute events regarding migration, bereavement, legal difficulties, crime, and auto accidents were assessed (i.e., 13 episodic stress domains were assessed in total). Information was gathered about the nature of the episodic events (i.e., surrounding circumstances), coping resources, and consequences. Using a five-point scale, interviewers then made ratings of the impact of the particular event (1 = no impact to 5 = severe impact, in increments of .5). Up to three episodic stressors were rated within each domain. Ratings of 0 were assigned if the episodic stress was absent. As with chronic stress, episodic stress at intake (ESI) was a sum composite of the T1 episodic stress ratings, while episodic stress over follow-up (ESF) was a composite of the ratings summing across T2 and T3.
Depression
A latent variable of unipolar depression (DEP) was formed using two questionnaire indicators and an ADIS-IV clinical rating composite (collected at each assessment): (a) Beck Depression Inventory (BDI; Beck & Steer, 1987); (b) Depression scale of the 21-item version of the Depression Anxiety Stress Scales (DASS-D; Lovibond & Lovibond, 1995; cf. Antony, Bieling, Cox, Enns, & Swinson, 1998; Brown, Chorpita, Korotitsch, & Barlow, 1997); and (c) the ADIS-IV dimensional ratings of the 9 symptom criteria of DSM-IV major depression (0 = “none” to 8 = “very severe”; interrater r = .74, Brown et al., 2001). In accord with prior studies (e.g., Brown, 2007; Brown, Chorpita, & Barlow, 1998), the BDI was scored using the 10 items that load on a Cognitive/Affective factor (items 1–9, 13) that are more specific to the unipolar mood disorders. As in Brown (2007), the DASS-D was used as the marker indicator for the DEP latent variable. Observed DASS-D scores were multiplied by two to foster comparability to the unstandardized DEP metric reported in Brown (2007), who used the 42-item version of the DASS (thus, the possible range of DASS-D scores was 0 to 42, with higher scores reflecting more severe depressive symptoms).
Data analysis
The raw data were analyzed using a latent variable software program and maximum-likelihood minimization functions (Mplus 6.0, Muthen & Muthen, 1998–2010). Missing data due to attrition (25% at T2, 40% at T3) were accommodated in all analyses using direct maximum likelihood (cf. Allison, 2003; Raykov, 2005). Goodness of fit of the models was evaluated using the root mean square error of approximation (RMSEA), and its 90% confidence interval and test of close fit (CFit), the Tucker-Lewis index (TLI), the comparative fit index (CFI), and the standardized root mean square residual (SRMR). Acceptable model fit was defined in part by the criteria forwarded by Hu and Bentler (1999): RMSEA values close to .06 or below (90% CI upper limit close to ≥ .06, nonsignificant CFit), CFI and TLI values close to .95 or above, and SRMR values close to .08 or below. In the case of nested models (e.g., evaluation of longitudinal measurement invariance), comparative fit was evaluated with χ2 difference tests (χ2diff). The acceptability of the models was further evaluated by the presence/absence of salient localized areas of strains in the solutions (e.g., modification indices), and the strength and interpretability of the parameter estimates.
Results
Cross-Sectional Analyses
The first set of analyses entailed structural regression models to determine whether chronic stress (CSI) and episodic stress (ESI) over the six months preceding the intake evaluation had significant main effects on T1 depression severity, and whether CSI and ESI moderated the influence of neuroticism on depression severity. As noted previously, depression severity was a latent variable (DEP) defined by three observed measures. Because this measurement model was just-identified (df = 0; cf. Brown, 2006), goodness of fit evaluation was not germane to this set of analyses (completely standardized factor loadings were .90, .89, and .77, for DASS-D, BDI, and ADIS-IV MDD dimensional ratings, respectively; all ps < .001).
Chronic stress
To examine the main effects of neuroticism and chronic stress on depression severity at intake, the DEP latent variable was regressed onto the T1 measures of CSI and neuroticism (N). As seen in Table 1, both main effects were statistically significant (ps < .001) and collectively accounted for 57.6% of the variance in DEP. Next, the CSI × N product term was included as a predictor, which resulted in a significant increase in the model R2 (p < .001, ƭ2 = .02, a small effect per the standards set forth by Cohen, 1988). The regression coefficient for the product term was positive, indicating the strength of the effect of neuroticism on depression increased as chronic stress increased. The nature of this interaction effect is depicted in Figure 1.
Table 1.
Cross-Sectional Structural Regression Models of the Effects of Chronic Stress, Episodic Stress, and Neuroticism on Depression
|
Chronic Stress | ||||
|---|---|---|---|---|
| γ | SEγ | γ* | SEγ* | |
| Main effects (Model R2 = .58): | ||||
| CSI | 0.60*** | 0.08 | .23*** | .03 |
| N | 0.69*** | 0.03 | .65*** | .02 |
| Interaction effect (Model R2 = .59, ƭ2 = .02): | ||||
| N × CSI | 0.03*** | 0.01 | .69*** | .18 |
|
Episodic Stress | ||||
| Main effects (Model R2 = .54): | ||||
| ESI | 0.14** | 0.05 | .08** | .03 |
| N | 0.76*** | 0.03 | .72*** | .02 |
| Interaction effect (Model R2 = .54, ƭ2 = .00): | ||||
| N × ESI | 0.00 | 0.01 | .01 | .11 |
Note. CSI = chronic stress in the 6 months preceding the intake evaluation, N = neuroticism, ESI = episodic stress in the 6 months preceding the intake evaluation, γ = unstandardized path coefficient, γ*= completely standardized path coefficient.
p < .01
p < .001
Figure 1.
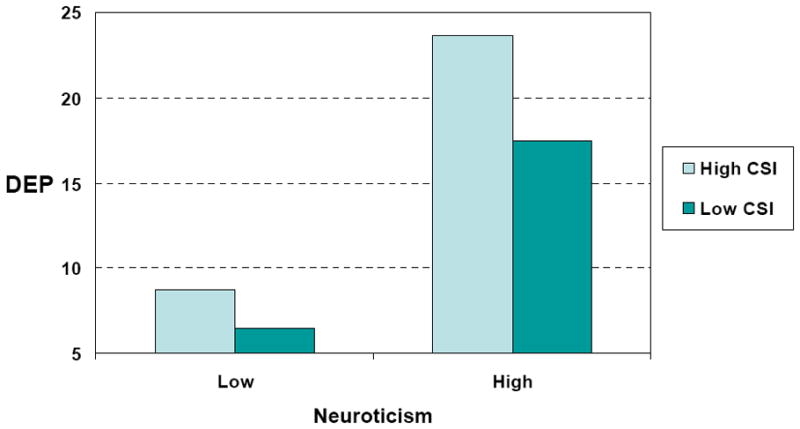
Nature of the Interaction of Neuroticism and Chronic Stress on Depression Symptoms at Intake. DEP = depression, CSI = chronic stress in the 6 months preceding the intake evaluation. The possible range of scores for the unstandardized DEP latent variable is 0 to 42.
These analyses were re-run controlling for extraversion (NFFI-E). As expected, extraversion had a significant direct effect on DEP (unstandardized and completely standardized γs = −0.09 and −.07, respectively; ps = .02). The inclusion of extraversion did not affect the size or statistical significance of the N and CSI main effects, or the N × CSI interaction (e.g., unstandardized γ for product term continued to be 0.03, p < .001).
Episodic stress
As shown in Table 1, ESI had a significant main effect on DEP (p = .003), holding N constant. This direct effect remained statistically significant controlling for extraversion (unstandardized and completely standardized γs for ESI = −0.16 and −.10, respectively; ps < .001). In addition, a model in which ESI and CSI were simultaneously included as predictors (along with the neuroticism and extraversion covariates) indicated that both episodic stress and chronic stress explained significant unique variance in initial depression severity (ps < .03 and .001 for ESI and CSI, respectively). However, the N × ESI product term did not significantly contribute to the prediction of DEP (ƭ2 = 0), indicating that the effect of neuroticism on depression severity did not vary as a function of the level of episodic stress.
Longitudinal Analyses
Diagnostic outcome over follow-up
Nearly three-quarters (74.1%) of the sample received treatment at CARD after the intake assessment. As expected, the overall rate of emotional disorders in the sample declined by 6-month follow-up (i.e., from 100% to 74.8%; McNemar test p < .001), with relatively less additional change at the 12-month assessment (69.4%, p = .04). A similar pattern was found specifically for the DSM-IV mood disorders (i.e., 39.6%, 25.5%, and 20.4% for T1 through T3, respectively); although the T1 to T2 reduction in mood disorders was significant (p < .001), the additional decline at T3 was not (p = .15).
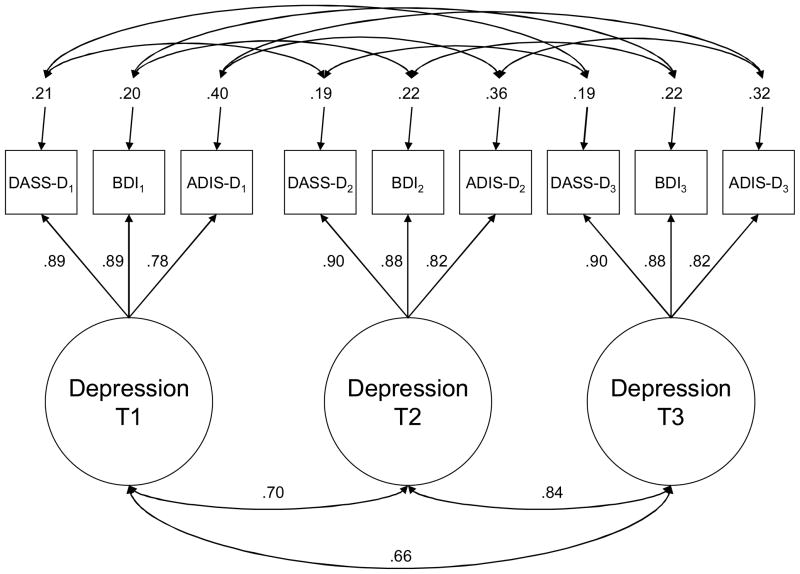
Unconditional longitudinal models
To establish the suitability of the DEP latent variable as an outcome in the subsequent LGMs (i.e., to ensure that temporal change in the DEP latent construct was not confounded by change in its measurement over time), a longitudinal confirmatory factor analytic model was evaluated. As shown in Figure 2, indicators of the same variable assessed at different times (e.g., DASS-D1, DASS-D2, DASS-D3) were specified to have correlated uniquenesses (cf. Brown, 2006). A baseline model, which contained no restrictions on the factor loadings and indicator intercepts, fit the data well, χ2(15) = 42.25, p < .001, SRMR = .02, RMSEA = 0.05 (90% CI = 0.03 to 0.06, CFit =.59), TLI = 0.98, CFI = .99. The next model, which constrained the factor loadings to equality, produced a statistically nonsignificant increase in model χ2, indicating that the loadings were time invariant, χ2diff(4) = 8.54, ns. A final model established the temporal equivalence of the indicator intercepts, χ2diff(4) = 9.01, ns. The completely standardized parameter estimates of this solution are presented in Figure 2 (all factor loading and factor correlation ps < .001).
Figure 2.
Longitudinal Measurement Model of Depressive Symptoms. Completely standardized parameter estimates are provided (all ps < .001). For presentational clarity, correlated error estimates are not presented (range = .19 to .42). T1 = Intake, T2 = 6-month follow-up, T3 = 12-month follow-up; DASS-D = Depression scale of Depression Anxiety Stress Scales; BDI = Beck Depression Inventory; ADIS-D = ADIS-IV dimensional ratings of major depression.
The longitudinal measurement model was re-specified as an unconditional latent growth model (LGM). Because more depression symptom change occurred during the first six months of follow-up (when most patients received treatment), linear growth was untenable. Thus, the Slope factor loadings were specified as follows for T1, T2, and T3, respectively: 0, *, and 1 (* = freely estimated). This specification centers the Intercept factor on T1 (i.e., mean and variance of DEP when Time = 0), and the mean (and variance) of the Slope factor reflects the extent of change (and individual differences in change) in the DEP latent construct over the one-year period. Identification and parsimony of the LGMs was further fostered by fixing the intercepts of the DEP latent variables to zero and holding their residual variances to equality.
The unconditional LGM fit the data well, χ2(25) = 59.84, p < .001, SRMR = .03, RMSEA = 0.04 (90% CI = 0.03 to 0.06, CFit =.86), TLI = 0.99, CFI = .99. As expected, the majority of symptom reduction in the DEP construct occurred in the first six months of follow-up, as reflected by the freely estimated T2 Slope factor loading (λT2 = .87). Estimates for the growth factors are presented in Table 2. The random effects for both the Intercept and Slope were statistically significant (ps < .001), indicating the presence of considerable individual differences in the initial levels (T1) and change in DEP over time. The sign (i.e., negative) and statistical significance (p < .001) of the Slope mean indicated that, on average, patients experienced a significant reduction in DEP over the follow-up period (Cohen’s d = 0.60). The Intercept and Slope were significantly (p < .001) and inversely related (e.g., correlation = −.40); thus, as in Brown (2007), temporal reductions in depression were more pronounced in patients with higher initial levels of depressive symptoms.
Table 2.
Structural Parameter Estimates From the Unconditional Latent Growth Model of Depression
| Intercept | Slope | |
|---|---|---|
| Mean | 14.57 (0.38) | −5.47 (0.36) |
| Variance | 83.57 (5.95) | 36.34 (5.76) |
| Covariance | −22.19 (4.30) | |
| Correlation | −.40 (0.05) | |
Note. Standard errors are in parentheses. All parameter estimates are significant at p < .001.
Chronic stress
Next, a conditional LGM was specified to examine whether T1 neuroticism (N) and the level of chronic stress experienced during the follow-up interval (CSF) predicted individual differences in the extent of change in DEP (holding initial levels of DEP constant). This model provided a good fit to the data, χ2(39) = 102.44, p < .001, SRMR = .03, RMSEA = 0.04 (90% CI = 0.03 to 0.06, CFit =.80), TLI = 0.98, CFI = .99. Collectively, N and CSF accounted for 32.3% of the variance in the DEP Slope (p < .001). However, consistent with the findings of Brown (2007), initial levels of N did not account for significant unique variance in the DEP Slope (unstandardized and completely standardized γs for N = −0.04 and −.06, respectively; ps = .61). The effect of CSF→ DEP Slope was statistically significant (p < .001) and positively signed (unstandardized and completely standardized γs for CSF = 0.47 and .47, respectively). This path reflects a two-way interaction effect; specifically, that the effect of Time on DEP differs across levels of CSF. The positive sign of this path (in tandem with a Slope mean showing an overall reduction in depression over follow-up) indicates that, holding initial levels of depression and neuroticism constant, patients who experienced higher levels of chronic stress during the follow-up period evidenced less symptom improvement in depression.
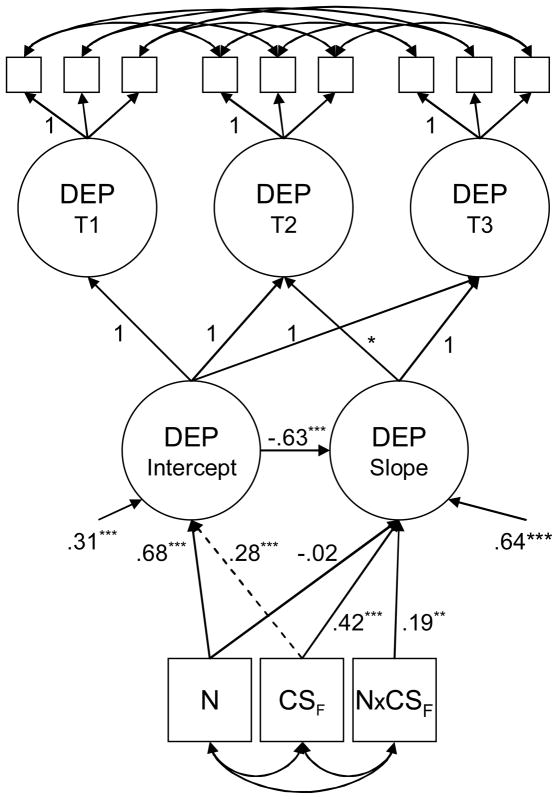
The N × CSF interaction term was then included in the conditional LGM. Prior to forming the product term, N and CSF were mean centered to foster interpretability of the parameter estimates and to eliminate multicollinearity in the predictor set. The parameterization and goodness of fit of this model are shown in Figure 3. The N × CSF→ DEP Slope path was statistically significant (p < .001) and resulted in an R2 change of .03 (ƭ2 = .09, between a small and medium effect per Cohen, 1988). The completely standardized parameter estimates (and two-tailed p levels) of this solution are presented in Figure 3. The significant N × CSF→ DEP Slope path indicates that the strength of the relationship between neuroticism and the trajectory of depression varies as a function of the level of chronic stress experienced during the follow-up period. However, in view of the manner in which Time is parameterized in the LGM, the two-way interaction of these predictors must be probed as a three-way interaction with Time. Thus, the model-implied trajectories of DEP were computed and plotted at low, medium, and high levels of N (−SD, M, +SD, respectively) within high and low levels of CSF (±SD; cf. Curran, Bauer, & Willoughby, 2004).
Figure 3.
Conditional Latent Growth Model of Depressive Symptoms. N = neuroticism, CSF = chronic stress during the follow-up period, N × CSF = neuroticism by chronic stress product term, DEP = Depression, T1 = Intake, T2 = 6-month follow-up, T3 = 12-month follow-up, * = freely estimated parameter. Completely standardized estimates are shown. Overall fit of model: χ2(46) = 126.30, p < .001, SRMR = .03, RMSEA = 0.05 (90% CI = 0.04 to 0.06, CFit = .74), TLI = 0.98, CFI = .98. **p < .01 ***p < .001
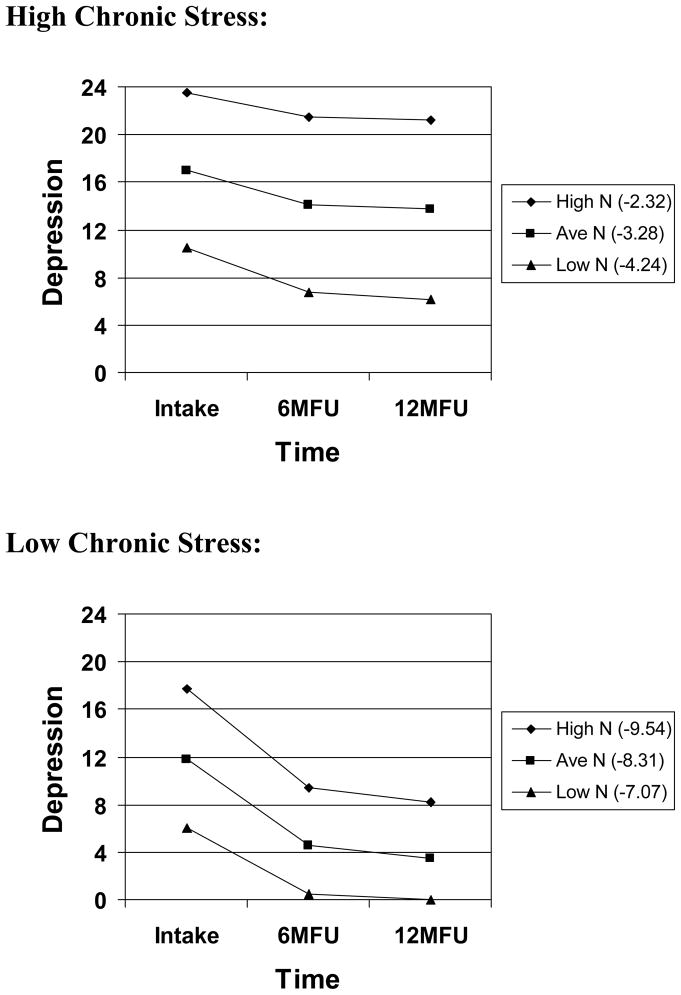
The nature of this three-way interaction is depicted in Figure 4. Each of the six conditional trajectories shown in Figure 4 was statistically significant (largest p = .01). Within low CSF, although the three conditional trajectories are decreasing over time, the magnitude of the reduction in DEP is significantly larger as the initial level of N increases. The opposite pattern occurs when the level of chronic stress is high. Within high CSF, high N is associated with the least amount of DEP symptom reduction. In other words, when chronic stress during follow-up is high, the degree of improvement in DEP is significantly smaller as N increases.
Figure 4.
Model-Implied Trajectories of Depression as a Function of Neuroticism Within High and Low Chronic Stress. The conditional model-implied trajectories are provided in parentheses within the figure legend. N = neuroticism. The possible range of scores for the unstandardized Depression latent variable is 0 to 42.
The previous two conditional LGMs were re-conducted including extraversion (NFFI-E) and CSI. Importantly, the direct effects of CSF and the N × CSF interaction remained statistically significant when controlling for these covariates (e.g., chronic stress reported during the follow-up period continued to predict change in DEP when holding initial levels of chronic stress constant). Interestingly, the direct effect of extraversion on the DEP Slope was statistically significant (unstandardized and completely standardized γs = −0.11 and −.15, respectively; ps < .01). Thus, controlling for other predictors (i.e., initial levels of DEP and neuroticism, and chronic stress), higher levels of T1 extraversion were associated with greater decreases in DEP.
Finally, it should be noted that although the direction of the CSF→ DEP Intercept path shown in Figure 3 is at odds with conceptual reasoning (i.e., chronic stress during follow-up should not have a directional influence on depression severity at intake; see dotted path line in Figure 3), the growth factors in these models were nonetheless regressed onto all background variables because the substantive focus was on the paths relating these predictors to the DEP Slope (i.e., this parameterization allowed the exogenous variables to be freely intercorrelated and accounted for any significant covariance that existed between these variables and the DEP Intercept). In fact, as seen in Figure 3, a significant relationship existed between the DEP Intercept and CSF. Thus, in accord with a stress generation framework, the last conditional LGM was re-specified such that CSF was regressed onto N, extraversion, DEP Intercept, and CSI. The DEP Intercept → CSF path was statistically significant (unstandardized and completely standardized γs = 0.27 and .43, respectively; ps < .001). Therefore, even when these other covariates were held constant, higher levels of depression at intake were associated with higher levels of chronic stress during follow-up.
Episodic stress
The conditional LGMs were repeated replacing CSF with the variable representing the level of episodic stress experienced during the follow-up interval (ESF). Both the main effects and moderation models fit the data well; e.g., goodness of fit for the moderation model: χ2(46) = 86.60, p < .001, SRMR = .02, RMSEA = 0.03 (90% CI = 0.02 to 0.04, CFit = 1.00), TLI = 0.99, CFI = .99. However, neither ESF or the N × ESF product term accounted for significant unique variance in the DEP Slope (ps = .72 and .52, respectively). Moreover, unlike chronic stress, intake depression severity was not significantly associated with episodic stress during follow-up (zero-order r of DEP Intercept and ESF = .04, p = .43). As in the chronic stress LGMs, the N → DEP Slope path was nonsignificant (p = .25). However, higher T1 extraversion was associated with greater decreases in DEP over follow-up, even when controlling for initial levels of DEP and neuroticism, and episodic stress (unstandardized and completely standardized γs = −0.13 and −.18, respectively; ps < .01).
Discussion
As expected (i.e., the majority of the sample received treatment after the intake assessment), results from the unconditional latent growth model indicated that patients experienced a significant reduction in depression symptoms over the follow-up period (Cohen’s d = 0.60). Consistent with a common finding in random effects modeling studies of psychopathological processes (e.g., Brown, 2007), the growth factors were inversely related (Intercept and Slope correlation = −.40). Thus, temporal symptom reductions were more prominent in patients with higher initial levels of depressive symptoms. However, subsequent analyses revealed that several variables moderated this temporal change.
For instance, the collective findings indicate that chronic stress is a salient predictor of the severity and temporal change in depressive symptoms. In the cross-sectional analyses, the level of chronic stress exposure reported during the six months prior to the intake evaluation was uniquely and positively associated with depression symptom severity. A CSF × Time interaction effect was obtained in the longitudinal analyses indicating that patients who reported higher levels of chronic stress during the follow-up period experienced less depression symptom improvement. These results are in accord with previous assertions and some evidence attesting to the relevance of the relatively neglected role of chronic stress in the severity and maintenance of depression (e.g., Hammen et al., 2009; Hayden & Klein, 2001; McGonagle & Kessler, 1990; Tennant, 2002). Moreover, these data are consistent with arguments that chronic stress may have stronger relations with the symptom severity and longitudinal course of depression than episodic stress (Hayden & Klein, 2001; Moerk & Klein, 2000; Tennant, 2002). Indeed, although episodic stress was uniquely predictive of intake symptom severity, nonsignificant effects were obtained in the remaining analyses (i.e., episodic stress did not have a direct effect on depression improvement and was not a significant moderator of the influence of neuroticism on depression symptom severity or temporal course).
These findings may suggest that while exposure to an acute stressor is a stronger precipitant of a depressive episode (as documented by a sizeable literature focused on the role of episodic stress in major depression; cf. Hammen, 2005; Kessler, 1997), ongoing stressors (e.g., poor working conditions, financial difficulties, continuing health problems, conflictual interpersonal relationships) are more germane to the ongoing course of symptoms. Accordingly, chronic strains may work together with a variety of psychological or biological determinants to protract the symptoms of depression (e.g., constant financial or occupational adversities may reinforce feelings of low self-worth; chronic health problems may contribute to a sense of hopelessness). However, it is possible that aspects of the study design fostered the observed differential relationships of chronic and episodic stress. Unlike most previous research, the construct of depression was represented in the analyses as a latent dimension rather than an observed categorical variable (i.e., presence/absence of a DSM-IV mood disorder). Although having many advantages (e.g., increased statistical power, reliability, and validity from using dimensional latent variables defined by multiple indicators; cf. Brown, 2006, 2007; Brown & Barlow, 2009), this approach was concerned with accounting for individual differences in depression symptom severity and did not address the specific timing of the onset of stressors and depressive episodes. For instance, as was the case for chronic stress, the episodic stress variable was a composite rating of acute stressors occurring over a six-month period. Collapsing episodic stressors in this fashion may have weakened the associations that could have been obtained in a finer-grained approach (e.g., linking specific acute stressors to spikes in depression symptom severity if stress and depression were assessed more frequently than every six months). Moreover, several studies have found that acute stressors play a larger role in the onset of the first depressive episode than in subsequent recurrences (e.g., Kendler, Thornton, & Gardner, 2000; Monroe, Slavich, Torres, & Gotlib, 2007; but also see Daley, Hammen, & Rao, 2000). The fact that most study participants with elevated symptoms had recurrent or ongoing depression (e.g., recurrent major depression, early onset dysthymia) may have further attenuated the association seen between episodic stress and depression symptom severity.
The current cross-sectional findings provide further evidence for the strong relationship between neurotic temperament and depression symptom severity (e.g., Brown, 2007). Despite the large effect obtained in the cross-sectional analyses, neuroticism did not significantly predict the longitudinal course of depressive symptoms. Similarly, a null effect was also reported in Brown (2007), in which the variable of neuroticism/behavioral inhibition was associated with less improvement in generalized anxiety disorder and social phobia, but not depression. As noted earlier, studies from the depression treatment outcome literature have produced mixed results with regard to the association between pre-treatment levels of neuroticism and depression treatment response. In Brown (2007), this nonsignificant temporal relationship was discussed in terms of the considerable overlap observed between initial levels of neuroticism/behavioral inhibition and depression (r = .77, resulting in a relatively smaller amount of unique variance in change that could be potentially accounted for by predictors), as well as the possibility that temperament has stronger effects on psychopathology as a predispositional factor than as a pathoplastic influence (i.e., more robust direct effects of temperament on depression may be obtained in community or at-risk samples than in clinical samples). Indeed, the ability to detect temporal relationships between temperament and psychopathology in clinical samples may be complicated by the effects of mood-state distortion; that is, patients’ self-reports of temperament are affected (augmented) by their current clinical state (Brown, 2007; Clark et al., 2003; Widiger & Smith, 2008). For instance, if neuroticism is a temporally stable construct that characterizes everyday functioning (i.e., a trait), its measurement in clinical samples is apt to contain a substantial amount of “state” variance due to general clinical distress. Clark et al. (2003) have argued that the variance due to mood-state distortion may make it difficult to detect the how stable variance in temperament predicts depression outcomes. As in Brown (2007), the present study used the initial depression symptom severity (i.e., the Depression Intercept; cf. Figure 3) as a covariate in the conditional latent growth models in attempt to remove some of the general distress component from neuroticism in the prediction of the temporal course of depression. However, in Brown (2007) and the present study, neuroticism did not exert a significant direct effect on depression symptom change.
A different pattern of results arose when chronic stress was included in the analyses as a moderator of the temporal effects of neuroticism on depression symptoms.2 Consistent with prediction, neuroticism had an increasingly deleterious effect on depression symptom improvement as the levels of concurrent chronic stress increased. Indeed, the least amount of depression symptom reduction was seen in individuals with the highest intake levels of neuroticism who experienced higher levels of chronic stress during the follow-up period (i.e., a model-implied decrease of only 2.32 points on the DASS-D; Figure 4). Importantly, this interaction effect remained statistically significant after controlling for a number of substantively salient covariates (e.g., initial depression symptom severity, extraversion, chronic stress over the six months preceding the follow-up interval). This result is in accord with leading conceptual models of emotional disorders (e.g., Barlow, 2002) which posit that pre-existing biological or psychological vulnerabilities (e.g., genetically based dimensions of temperament, perceptions of low emotional control) must be activated by stressful life events to produce psychopathology. However, in drawing this connection, one must be mindful of the fact that such conceptual models focus primarily on the etiology of disorders (i.e., predisposition) rather than the maintenance of psychopathology (i.e., pathoplasty). Thus, these conceptualizations are more apt to underscore the potentiating role of an acute stressor in the onset of psychopathological states (although the specific nature of the triggering life stressors is not always explicated in these models; e.g., Barlow, 2002). The current findings suggest that this conceptual interplay between temperament and life stress may extend to the maintenance of psychopathology, with chronic stress playing a more important role as a direct and moderating influence than episodic stress. Specifically, although neuroticism may have a key and perhaps stronger role as a predispositional factor, it continues to exert a negative influence on the course of depressive symptoms if the propensity to react adversely to stress is activated by ongoing life strains. Inspection of the model-implied trajectories in Figure 4, however, also indicates that neuroticism had the opposite effect on the course of depressive symptoms in patients who were exposed to lower levels of chronic stress (i.e., in these participants, higher initial levels of neuroticism were associated with larger depression symptom reductions). Thus, if not triggered by life stressors during follow-up, neuroticism appears to have a similar impact on the temporal course of depressive symptoms as does initial depression symptom severity, where the negative correlation between the latent growth factors indicated that higher levels of T1 depression were associated with greater reductions in depressive symptoms over follow-up (i.e., given the strong positive relationship between T1 neuroticism and depression, participants with high neuroticism also had elevated initial levels of depression). However, this inverse relationship was reversed by the moderating effects of chronic stress; that is, if activated by chronic stress, higher initial levels of neuroticism are associated with less, not more, depression symptom improvement.
In addition, our findings were suggestive of a bidirectional relationship between chronic life stress and depressive symptoms. Specifically, although chronic stress had a direct effect on depression severity in the cross-sectional and time-series analyses, results also indicated that initial depression symptom severity was associated with higher levels of chronic stress during the follow-up period. Although measurement issues cannot be dismissed (see next paragraph), this result is consistent with prior evidence of stress generation (e.g., Daley et al., 1997; Hammen, 1991); namely, that the presence of depression is positively associated with the incidence of subsequent stressful life events. Whereas stress generation research has primarily focused on episodic stressors (e.g., Daley et al., 1997), the current results suggest that this effect extends to chronic stressors. Thus, the presence of a persistent depressive disorder may contribute to the emergence or chronicity of ongoing strains (e.g., social withdrawal may contribute to poor interpersonal and occupational relationships; loss of interest/energy may result in underemployment and financial difficulties). Indeed, some research has suggested that depressed individuals are often locked or select themselves into problematic environmental contexts (e.g., Hammen, 2003; Hammen & Brennan, 2002; Kendler, Karkowski, & Prescott, 1999). Yet, this research has also produced evidence that stress generation is not necessarily due entirely to the direct effects of a depressive disorder. For instance, Kendler and colleagues found that exposure to stressful life events is substantially influenced by genetic factors and that the genetic risk factors for stressful life events are positively correlated with the genetic risk factors for major depression (e.g., Kendler & Karkowski-Shuman, 1997; Kendler, Neale, Kessler, Heath, & Eaves, 1993). Along these lines, other evidence from this laboratory indicates that neuroticism is strongly predictive of the occurrence of stressful life events and the quality of interpersonal relationships (Kendler et al., 2003; see also Bolger & Zuckerman, 1995; Fergusson & Horwood, 1987; Gunthert, Cohen, & Armelli, 1999). More research is needed to further explicate the specific role of temperament in the relationship between psychopathology and life stress (e.g., does neuroticism have an indirect effect on life stress, with depression playing an intervening role in this causal pathway?).3
However, the fact that the interview measures of chronic and episodic stress were collected concurrently with measures of depression precludes firm conclusions about the directionality of the relationships among these variables. Moreover, it is possible that the magnitudes of these relationships were unduly augmented by aspects of the assessment approach and the use of a clinical sample. For instance, life stress ratings were based on patients’ retrospective report and thus, like other variables, were susceptible to the effects of mood-state distortion; e.g., depression severity at the time of the evaluation covaried with a tendency to recall negative life events over the preceding six months.
Researchers must also consider the possibility that the associations routinely observed between life stress and depression are spuriously inflated by confounded measurement; i.e., the measurement of life stress may overlap with the measurement of depression. This issue may be particularly germane to the measurement of chronic stress. For example, a higher rating for the UCLA-LSI social domain of chronic stress might be assigned to characterize an individual with impoverished friendships and limited social contacts (see Method). Because clinical depression is often associated with social withdrawal, the chronic social stress rating could be construed as another indicator of depression. As discussed by Hammen (2005), life stress interviews were developed to address this and other potential confounds, and are regarded as the standard of this field (i.e., psychometrically superior to other methods such as life event checklists; cf. Kessler, 1997). Specifically, in addition to the systematic identification of events, these interviews entail the collection of contextual information (e.g., circumstances surrounding the event) used as a basis for rating the “objective” threat of the stressors, independent of an individual’s symptomatology. Indeed, research has indicated that interview methods are less prone to potential measurement confounds and biases (mood-state distortion, cognitive vulnerabilities; e.g., McQuaid, Monroe, Roberts, Kupfer, & Frank, 2000). However, it has been suggested that the contextual information used to bolster the quality of interview ratings may itself be influenced by the risk factors (e.g., neuroticism) that account for the relationship between life stress and depression (Kessler, 1997; Mazure, 1998). Thus, despite the use of an interview method of life stress measurement (UCLA-LSI), these psychometric issues cannot be dismissed.
Nonetheless, aspects of the current results may indicate that measurement confounds were not chiefly responsible for the observed effects. A multivariate approach was undertaken in part to control for the overlap among the various predictors of the longitudinal course of depression symptoms. In these analyses, for instance, chronic stress had a significant direct and moderating effect on the trajectory of depression, even after holding initial levels of depression and neuroticism constant. Moreover, the direction of the effect that chronic stress had on the course of depression symptoms was opposite to that of other predictors (e.g., although the initial level of depression was positively related to chronic stress during follow-up, it was inversely related to depression symptom improvement), a result pattern that may argue against the redundancy of these variables. A more compelling evaluation of the nature of the relationship between chronic stress and depression would require alternative research designs such as studies focused on the impact of stressors that are presumably unrelated to depression and its risk factors (e.g., studies of parents of children with serious medical disorders), or prospective studies of individuals entering stressful life roles (e.g., military service) (Kessler, 1997).
Although mood disorders were well-represented (e.g., n = 329 at intake), it is important to note that this study used a diagnostically diverse sample along with outcome variables that were dimensional latent variables of depression symptoms rather than DSM-IV mood disorder diagnoses. As has been discussed at length elsewhere (e.g., Brown & Barlow, 2005, 2009), this approach has several methodological advantages over the use of DSM diagnoses as units of analysis such as better reliability (further fostered by the use of latent variables that are theoretically free of measurement error), ability to capture individual differences in symptom severity, and increased statistical power. Whereas some previous studies have used research designs similar to the current study (e.g., depression as a continuous variable, Kercher et al., 2009; Wetter & Hankin, 2009), the more common strategy in this literature entails the use of DSM diagnoses as outcomes (e.g., the ability of neuroticism or stress to predict the onset of DSM-defined major depressive episodes, Hammen et al., 2009; Monroe et al., 2007; Ormel et al., 2001). Because this study focused on the severity and longitudinal course of depressive symptoms, it is not clear to what extent these findings would inform the nature of the relationship that neuroticism and life stress have in predicting the onset or recurrence of major depression diagnoses or other DSM-IV mood disorder categories. For instance, the question of whether episodic stressors are more strongly related to first episodes of major depression than to recurrences (e.g., Moerk & Klein, 2000) may be better addressed by studies using DSM disorders as units of analysis than by treating depression as a continuous variable. The dimensional and categorical approaches both have their strengths and place in the stress-vulnerability literature, but care should be taken to the avoid the assumption that findings from one approach will readily generalize to the other.
Interestingly, as well as its association with depression symptom severity at intake, extraversion was found to be significantly and uniquely predictive of the temporal course of depression—i.e., lower initial levels of extraversion were associated with less depression symptom improvement. Because extraversion was included in this study as a covariate (to examine the unique effects of neuroticism and its interaction with life stress controlling for another salient temperamental predictor of depression), this should be regarded as a rather incidental finding. Indeed, previous studies have produced mixed findings with respect to the ability of extraversion and related constructs (e.g., behavioral activation, positive affect) to predict the temporal course and treatment response of depression (e.g., Brown, 2007; Hayden & Klein, 2003; Kasch, Rottenberg, Arnow, & Gotlib, 2002; Quilty et al., 2008). Given the extensive empirical and conceptual basis for the significance of neuroticism in stress-depression research (e.g., as a dimension associated with sensitivity to stressful life events; Hammen, 2005), investigators have not considered the possibility that the effects of extraversion on depression vary as a function of life stress. Although the direct effect of extraversion on depression typically reflects an inverse relationship (i.e., lower levels of extraversion are associated with higher levels of depression), interaction effects involving life stress may be more complex (i.e., the direction of effects vary depending on the facet of extraversion and the type of life stress). Whereas extraversion is not a trait reflecting the propensity to react adversely to stressors (cf. neuroticism), it is defined in part by facets such as sociability and activity that might interact with stressful life events to elicit clinical distress. In line with a congruency model of stress and personality (e.g., Nietzel & Harris, 1990), perhaps depression is apt to arise when the nature of the activating stressor is relevant to the specific facets of extraversion that are characteristic of the individual; e.g., persons scoring high on the excitement-seeking or activity facets may be more prone to depression if exposed to a stressor such as a physically debilitating injury that limits the ability to be active and engaged with their environment (an effect that is opposite to the direction of the typical main effect of extraversion on depression).
Finally, in addition to the aforementioned limitations (e.g., measurement issues, inability to address predispositional relationships), this study focused exclusively on neuroticism as the focal independent variable in the prediction of the severity and course of depressive symptoms. However, current conceptual models assert that dimensions of temperament are not solely responsible for the onset and maintenance of psychopathology. For instance, the triple vulnerability model of emotional disorders (Barlow, 2002) posits that in addition to biologically based temperaments (e.g., neuroticism), a general psychological vulnerability (self-perceptions of low emotional control) and disorder-specific vulnerabilities (e.g., cognitive dimensions such as sociotropy/autonomy and dysfunctional attitudes) act in concert to produce clinical depression. It is possible that these dimensions also influence the temporal course of depression, both directly and if activated by life stress. In addition to studies of predispositional effects (e.g., longitudinal studies using community or at-risk samples), future research should evaluate whether these theoretically relevant dimensions contribute to the maintenance of depressive symptoms, over and beyond the influence of neurotic (and intraverted) temperament.
Acknowledgments
The authors thank Constance Hammen for providing materials and training on the UCLA Life Stress Interview.
Footnotes
There was no overlap between the current sample and the sample reported in Brown (2007).
Although mediational models were not pursued (i.e., Neuroticism → Stress → Depression; e.g., Ormel & Wohlfarth, 1991; Wetter & Hankin, 2009), it is noteworthy that the current results indicated the absence of a direct effect of neuroticism on depression symptom course (no observed relationship between these variables that might be mediated by life stress during the follow-up period).
To evaluate this possibility in the current data set, the final structural model in the Results section was re-specified with the following indirect effect: N → DEPINT→ CSF. In accord with this conceptualization, a significant mediational relationship was obtained; unstandardized and standardized indirect effects = 0.22 and .34, respectively (ps < .001). Thus, holding other covariates constant (e.g., chronic stress during the six months preceding intake), neuroticism was positively associated with higher levels of chronic stress during follow-up (as mediated by initial depression severity).
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/abn
References
- Allison PD. Missing data techniques for structural equation modeling. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales in clinical groups and a community sample. Psychological Assessment. 1998;10:176–181. [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2. New York: Guilford Press; 2002. [Google Scholar]
- Beck AT, Steer RA. Manual for the revised Beck Depression Inventory. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- Bienvenu OJ, Brown C, Samuels JF, Liang KL, Costa PT, Eaton WW, Nestadt G. Normal personality traits and comorbidity among phobic, panic and major depressive disorders. Psychiatry Research. 2001;102:73–85. doi: 10.1016/s0165-1781(01)00228-1. [DOI] [PubMed] [Google Scholar]
- Bienvenu OJ, Samuels JF, Costa PT, Reti IM, Eaton WW, Nestadt G. Anxiety and depressive disorders and the five-factor model of personality: A higher- and lower-order personality trait investigation in a community sample. Depression and Anxiety. 2004;20:92–97. doi: 10.1002/da.20026. [DOI] [PubMed] [Google Scholar]
- Bock C, Bukh JD, Vinberg M, Gether U, Kessing LV. The influence of comorbid personality disorder and neuroticism on treatment outcome in first episode depression. Psychopathology. 2010;43:197–204. doi: 10.1159/000304176. [DOI] [PubMed] [Google Scholar]
- Bolger N, Zuckerman A. A framework for studying personality in the stress process. Journal of Personality and Social Psychology. 1995;69:890–902. doi: 10.1037//0022-3514.69.5.890. [DOI] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. New York: Guilford Press; 2006. [Google Scholar]
- Brown TA. Temporal course and structural relationships among dimensions of temperament and DSM-IV anxiety and mood disorder constructs. Journal of Abnormal Psychology. 2007;116:313–328. doi: 10.1037/0021-843X.116.2.313. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. Categorical vs dimensional classification of mental disorders in DSM-V and beyond. Journal of Abnormal Psychology. 2005;114:551–556. doi: 10.1037/0021-843X.114.4.551. [DOI] [PubMed] [Google Scholar]
- Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: Implications for assessment and treatment. Psychological Assessment. 2009;21:256–271. doi: 10.1037/a0016608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, Barlow DH. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behaviour Research and Therapy. 1997;35:79–89. doi: 10.1016/s0005-7967(96)00068-x. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843x.110.1.49. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114:505–521.05. doi: 10.1037/0021-843X.114.4.505. [DOI] [PubMed] [Google Scholar]
- Clark LA, Vittengl J, Kraft D, Jarrett RB. Separate personality traits from states to predict depression. Journal of Personality Disorders. 2003;17:152–172. doi: 10.1521/pedi.17.2.152.23990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Costa PT, McCrae RR. Personality in adulthood: A six-year longitudinal study of self-reports and spouse ratings on the NEO Personality Inventory. Journal of Personality and Social Psychology. 1988;54:853–863. doi: 10.1037//0022-3514.54.5.853. [DOI] [PubMed] [Google Scholar]
- Costa PT, McCrae RR. NEO PI-R Professional Manual: Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Curran PJ, Bauer DJ, Willoughby MT. Testing main effects and interactions in latent curve analysis. Psychological Methods. 2004;9:220–237. doi: 10.1037/1082-989X.9.2.220. [DOI] [PubMed] [Google Scholar]
- Daley SE, Hammen C, Burge D, Davila J, Paley B, et al. Predictors of the generation of episodic stress: A longitudinal study of late adolescent women. Journal of Abnormal Psychology. 1997;106:251–259. doi: 10.1037//0021-843x.106.2.251. [DOI] [PubMed] [Google Scholar]
- Daley SE, Hammen C, Rao U. Predictors of first onset and recurrence of major depression in young women during the five years following high school graduation. Journal of Abnormal Psychology. 2000;109:525–533. [PubMed] [Google Scholar]
- Di Nardo PA, Brown TA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV: Lifetime Version (ADIS-IV-L) New York: Oxford University Press; 1994. [Google Scholar]
- Dougherty LR, Klein DN, Davila J. A growth curve analysis of the course of dysthymic disorder: The effects of chronic stress and moderation by adverse parent-child relationships and family history. Journal of Consulting and Clinical Psychology. 2004;72:1012–1021. doi: 10.1037/0022-006X.72.6.1012. [DOI] [PubMed] [Google Scholar]
- Fanous A, Gardner CO, Prescott CA, Cancro R, Kendler KS. Neuroticism, major depression, and gender: A population-based twin study. Psychological Medicine. 2002;32:719–728. doi: 10.1017/s003329170200541x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Vulnerability to life events exposure. Psychological Medicine. 1987;17:739–749. doi: 10.1017/s0033291700025976. [DOI] [PubMed] [Google Scholar]
- Gershuny BS, Sher KJ. The relation between personality and anxiety: Findings from a 3-year prospective study. Journal of Abnormal Psychology. 1998;107:252–262. doi: 10.1037//0021-843x.107.2.252. [DOI] [PubMed] [Google Scholar]
- Gunthert KC, Cohen LH, Armelli S. The role of neuroticism in daily stress and coping. Journal of Personality and Social Psychology. 1999;77:1087–1100. doi: 10.1037//0022-3514.77.5.1087. [DOI] [PubMed] [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. Interpersonal stress and depression in women. Journal of Affective Disorders. 2003;74:49–57. doi: 10.1016/s0165-0327(02)00430-5. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress and depression. Annual Reviews of Clinical Psychology. 2005;1:293–319. doi: 10.1146/annurev.clinpsy.1.102803.143938. [DOI] [PubMed] [Google Scholar]
- Hammen C, Adrian C, Gordon D, Burge D, Jaenicke C, Hiroto D. Children of depressed mothers: Maternal strain and symptom predictors of dysfunction. Journal of Abnormal Psychology. 1987;96:190–198. doi: 10.1037//0021-843x.96.3.190. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA. Interpersonal dysfunction in depressed women: Impairments independent of depressive symptoms. Journal of Affective Disorders. 2002;72:145–156. doi: 10.1016/s0165-0327(01)00455-4. [DOI] [PubMed] [Google Scholar]
- Hammen C, Kim EY, Eberhart NK, Brennan PA. Chronic and acute stress in the prediction of major depression in women. Depression and Anxiety. 2009;26:718–723. doi: 10.1002/da.20571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammen C, Shih JH, Brennan PA. Intergenerational transmission of depression: Test of an interpersonal stress model in a community sample. Journal of Consulting and Clinical Psychology. 2004;72:511–522. doi: 10.1037/0022-006X.72.3.511. [DOI] [PubMed] [Google Scholar]
- Hankin BL. Personality and depressive symptoms: Stress generation and cognitive vulnerability to depression in a prospective daily dairy study. Journal of Social and Clinical Psychology. 2010;29:369–401. doi: 10.1521/jscp.2010.29.4.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden EP, Klein DN. Outcome of dysthymic disorder at 5-year follow-up: The effects of familial psychopathology, early adversity, personality, comorbidity, and chronic stress. American Journal of Psychiatry. 2001;158:1864–1870. doi: 10.1176/appi.ajp.158.11.1864. [DOI] [PubMed] [Google Scholar]
- Hettema JM, Prescott CA, Kendler KS. Genetic and environmental sources of covariation between generalized anxiety disorder and neuroticism. American Journal of Psychiatry. 2004;161:1581–1587. doi: 10.1176/appi.ajp.161.9.1581. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Hutchinson JG, Williams PG. Neuroticism, daily hassles, and depressive symptoms: An examination of moderating and mediating effects. Personality and Individual Differences. 2007;42:1367–1378. [Google Scholar]
- Kasch KL, Rottenberg J, Arnow BA, Gotlib IH. Behavioral activation and inhibition systems and the severity and course of depression. Journal of Abnormal Psychology. 2002;111:589–597. doi: 10.1037//0021-843x.111.4.589. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO, Prescott CA. Personality and the experience of environmental adversity. Psychological Medicine. 2003;33:1193–1202. doi: 10.1017/s0033291703008298. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski LM, Prescott CA. Causal relationship between stressful life events and the onset of major depression. American Journal of Psychiatry. 1999;156:837–841. doi: 10.1176/ajp.156.6.837. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Karkowski-Shuman L. Stressful life events and genetic liability to major depression: Genetic control of exposure to the environment? Psychological Medicine. 1997;27:539–547. doi: 10.1017/s0033291797004716. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Kuhn J, Prescott CA. The interrelationship of neuroticism, sex, and stressful life events in the prediction of episodes of major depression. American Journal of Psychiatry. 2004;161:631–636. doi: 10.1176/appi.ajp.161.4.631. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. A twin study of recent life events and difficulties. Archives of General Psychiatry. 1993;50:789–796. doi: 10.1001/archpsyc.1993.01820220041005. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Gardner CO. Stressful life events and previous episodes in the etiology of major depression in women: An evaluation of the “kindling” hypothesis. American Journal of Psychiatry. 2000;157:1243–1251. doi: 10.1176/appi.ajp.157.8.1243. [DOI] [PubMed] [Google Scholar]
- Kercher AJ, Rapee RM, Schniering CA. Neuroticism, life events, and negative thoughts in the development of depression in adolescent girls. Journal of Abnormal Child Psychology. 2009;37:903–915. doi: 10.1007/s10802-009-9325-1. [DOI] [PubMed] [Google Scholar]
- Kessler RC. The effects of stressful life events on depression. Annual Reviews of Psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. [DOI] [PubMed] [Google Scholar]
- Lakdawalla Z, Hankin BL. Personality as a prospective vulnerability to dysphoric symptoms among college students: Proposed mechanisms. Journal of Psychopathology and Behavioral Assessment. 2008;30:121–131. [Google Scholar]
- Lehmann H, Fenton F, Deutsch M, Feldman S, Engelsmann F. An 11-year follow up study of 110 depressed patients. Acta Psychiatrica Scandanavica. 1988;78:57–65. doi: 10.1111/j.1600-0447.1988.tb06301.x. [DOI] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33:335–342. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Mazure CM. Life stressors as risk factors in depression. Clinical Psychology: Science and Practice. 1998;3:291–313. [Google Scholar]
- McGonagle KA, Kessler RC. Chronic stress, acute stress, and depressive symptoms. American Journal of Community Psychology. 1990;18:681–706. doi: 10.1007/BF00931237. [DOI] [PubMed] [Google Scholar]
- McQuaid JR, Monroe SM, Roberts JE, Kupfer DJ, Frank E. A comparison of two life stress assessment approaches: Prospective prediction of treatment outcome in recurrent depression. Journal of Abnormal Psychology. 2000;109:787–791. doi: 10.1037//0021-843x.109.4.787. [DOI] [PubMed] [Google Scholar]
- Mineka S, Watson D, Clark LA. Comorbidity of anxiety and unipolar mood disorders. Annual Review of Psychology. 1998;49:377–412. doi: 10.1146/annurev.psych.49.1.377. [DOI] [PubMed] [Google Scholar]
- Moerk KC, Klein DN. The development of major depressive episodes during the course of dysthymic and episodic major depressive disorders: A retrospective examination of life events. Journal of Affective Disorders. 2000;58:117–123. doi: 10.1016/s0165-0327(99)00102-0. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Bellack AS, Hersen M, Himmelhoch JM. Life events, symptom course, and treatment outcome in unipolar depressed women. Journal of Consulting and Clinical Psychology. 1983;51:604–615. doi: 10.1037//0022-006x.51.4.604. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Kupfer D, Frank E. Life stress and treatment course of recurrent depression: I. Response during index episode. Journal of Consulting and Clinical Psychology. 1992;60:718–724. doi: 10.1037//0022-006x.60.5.718. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Roberts JE, Kupfer DJ, Frank E. Life stress and treatment course of recurrent depression: II. Post-recovery associations with attrition, symptom course, and recurrence over 3 years. Journal of Abnormal Psychology. 1996;105:313–328. doi: 10.1037//0021-843x.105.3.313. [DOI] [PubMed] [Google Scholar]
- Monroe SM, Slavich GM, Torres LD, Gotlib IH. Major life events and major chronic difficulties are differentially associated with history of major depressive episodes. Journal of Abnormal Psychology. 2007;116:116–124. doi: 10.1037/0021-843X.116.1.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mroczek DK, Almeida DM. The effects of daily stress, personality, and age on daily negative affect. Journal of Personality and Social Psychology. 2004;72:355–378. doi: 10.1111/j.0022-3506.2004.00265.x. [DOI] [PubMed] [Google Scholar]
- Muscatell KA, Slavich GM, Monroe SM, Gotlib IH. Stressful life events, chronic difficulties, and the symptoms of clinical depression. Journal of Nervous and Mental Disease. 2009;197:154–160. doi: 10.1097/NMD.0b013e318199f77b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus 6.0 [Computer software] Los Angeles: Author; 1998–2010. [Google Scholar]
- Nietzel MT, Harris MJ. Relationship of dependency and achievement/autonomy to depression. Clinical Psychology Review. 1990;10:279–297. [Google Scholar]
- Ormel J, Oldehinkel AJ, Brilman EI. The interplay and etiological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first, and recurrent depressive episodes in later life. American Journal of Psychiatry. 2001;158:885–891. doi: 10.1176/appi.ajp.158.6.885. [DOI] [PubMed] [Google Scholar]
- Ormel J, Wohlfarth T. How neuroticism, long-term difficulties, and life situation change influence psychological distress: A longitudinal model. Journal of Personality and Social Psychology. 1991;60:744–755. doi: 10.1037//0022-3514.60.5.744. [DOI] [PubMed] [Google Scholar]
- Peterson T, Papakostas GI, Bottonari K, Iacoviello B, Alpert JE, Fava M, Nierenberg AA. NEO-FFI factor scores as predictors to clinical response to fluoxetine in depressed outpatients. Psychiatry Research. 2002;109:9–16. doi: 10.1016/s0165-1781(01)00359-6. [DOI] [PubMed] [Google Scholar]
- Quilty LC, De Fruyt F, Rolland JP, Kennedy SH, Rouillon PF, Bagby RM. Dimensional personality traits and treatment outcome in patients with major depressive disorder. Journal of Affective Disorders. 2008;108:241–250. doi: 10.1016/j.jad.2007.10.022. [DOI] [PubMed] [Google Scholar]
- Raykov T. Analysis of longitudinal studies with missing data using covariance structure modeling with full-information maximum likelihood. Structural Equation Modeling. 2005;12:493–505. [Google Scholar]
- Reno RM, Halaris AE. The relationship between life stress and depression in an endogenous sample. Comprehensive Psychiatry. 1990;31:25–33. doi: 10.1016/0010-440x(90)90051-s. [DOI] [PubMed] [Google Scholar]
- Riso LP, Miyatake RK, Thase ME. The search for determinants of chronic depression: A review of six factors. Journal of Affective Disorders. 2002;70:103–116. doi: 10.1016/s0165-0327(01)00376-7. [DOI] [PubMed] [Google Scholar]
- Robins RW, Fraley RC, Roberts BW, Trzesniewski KH. A longitudinal study of personality change in young adulthood. Journal of Personality. 2001;69:617–640. doi: 10.1111/1467-6494.694157. [DOI] [PubMed] [Google Scholar]
- Rosellini AJ, Brown TA. The NEO-Five Factor Inventory: Latent structure and relationships with dimensions of anxiety and depressive disorders in a large clinical sample. Assessment. doi: 10.1177/1073191110382848. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spijker J, Bijl RV, de Graaf R, Nolen WA. Determinants of poor 1-year outcome of DSM-III-R major depression in the general population: Results of the Netherlands mental health survey and incidence study (NEMESIS) Acta Psychiatrica Scandanavica. 2001;103:122–130. doi: 10.1034/j.1600-0447.2001.103002122.x. [DOI] [PubMed] [Google Scholar]
- Tennant C. Life events, stress and depression: A review of review findings. Australian and New Zealand Journal of Psychiatry. 2002;36:173–182. doi: 10.1046/j.1440-1614.2002.01007.x. [DOI] [PubMed] [Google Scholar]
- Viken RJ, Rose RJ, Kaprio J, Koskenvuo M. A developmental genetic analysis of adult personality: Extraversion and neuroticism from 18 to 59 years of age. Journal of Personality and Social Psychology. 1994;66:722–730. doi: 10.1037//0022-3514.66.4.722. [DOI] [PubMed] [Google Scholar]
- Wetter EK, Hankin BL. Mediational pathways through which positive and negative emotionality contribute to anhedonic symptoms of depression: A prospective study of adolescents. Journal of Abnormal Child Psychology. 2009;37:507–520. doi: 10.1007/s10802-009-9299-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Widiger TA, Smith GT. Personality and psychopathology. In: John OP, Robins RW, Pervin LA, editors. Handbook of personality: Theory and research. 3. New York: Guilford Press; 2008. pp. 743–769. [Google Scholar]
- Wildes JE, Harkness KL, Simons AD. Life events, number of social relationships, and twelve-month naturalistic course of major depression in a community sample of women. Depression and Anxiety. 2002;16:104–113. doi: 10.1002/da.10048. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Shea MT, Pilkonis PA, Elkin I, Ryan C. Gender, type of treatment, dysfunctional attitudes, social support, life events, and depressive symptoms over naturalistic follow-up. American Journal of Psychiatry. 1996;153:1021–1027. doi: 10.1176/ajp.153.8.1021. [DOI] [PubMed] [Google Scholar]