Abstract
The cancer care system is increasingly complex, marked by multiple hand-offs between primary care and specialty providers, inadequate communication among providers, and lack of clarity about a “medical home” (the ideal accountable care provider) for cancer patients. Patients and families often cite such difficulties as information deficits, uncoordinated care, and insufficient psychosocial support. This article presents a review of the challenges of delivering well coordinated, patient-centered cancer care in a complex modern healthcare system. An examination is made of the potential role of information technology (IT) advances to help both providers and patients. Using the published literature as background, a review is provided of selected work that is underway to improve communication, coordination, and quality of care. Also discussed are additional challenges and opportunities to advancing understanding of how patient data, provider and patient involvement, and informatics innovations can support high-quality cancer care.
Introduction
Modern cancer care is characterized by three important facets: state-of-the-art clinical medicine, which may include evidence-based and sophisticated therapies targeted to patients’ tumor and biological characteristics. Second, an approach to care that is attentive to the spectrum of patients’ needs (i.e., physical, psychosocial, functional, spiritual). Third, the use of systems solutions, both human and machine, that support organizations in achieving their clinical medicine and patient-centered care delivery goals. Optimizing these delivery features for a disease as complicated and heterogeneous as cancer often entails complex decision making, multiple handoffs between primary and specialty care providers, and coordination among cancer care team members. Although several IOM reports have described these attributes of care delivery for modern health care generally1 and for cancer care delivery specifically,2 few efforts have been made to describe how to marshal IT to effectively measure, monitor, and proactively intervene when necessary across all of these dimensions to continually improve performance and build an effective system of cancer care.
A 2010 presidential commission report on the potential of health information technology (HIT) underscored that IT-enabled health care can reduce fragmentation of information, ensure high-quality, safer care, and aggregate data to enable meaningful use at the point-of-care and population level, leading to a “national health IT ecosystem in which every consumer, doctor, researcher and institution has appropriate access to the information they need…”3 These potential benefits of an IT-enabled system are particularly crucial for cancer care given its complexity.
This article examines attributes of high-performing modern cancer care delivery with special attention to opportunities for IT to help cancer organizations achieve a patient-centered delivery approach. As a relatively new area of research, use is made of published literature and in-progress studies on measuring quality of cancer care to address the following questions: How does IT support modern cancer care? What are the challenges in using IT to support patient-centered cancer care? How are technology and performance measurement currently used to help cancer organizations in these transitions? The conclusion proposes approaches for advancing a research and policy agenda for IT-enhanced cancer care.
Role of Information Technology in Supporting Modern Cancer Care
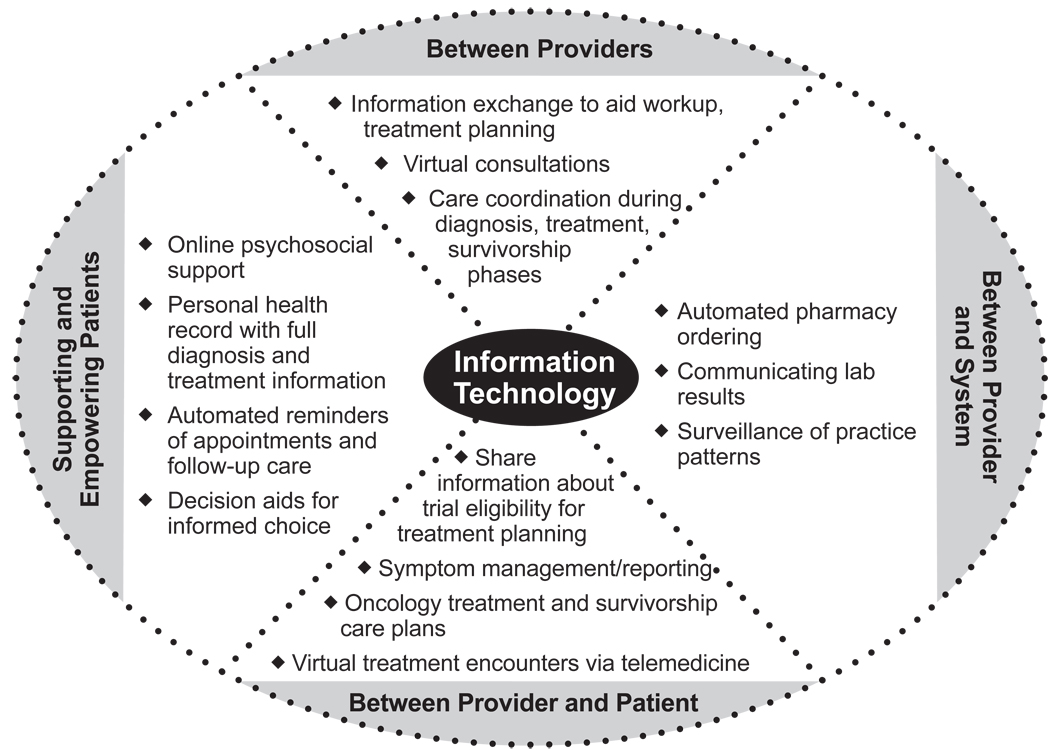
The promise of improved cancer care through IT is eloquently described by Wallace,4 who stated, ”Health IT can transform—in terms of pace, scale, and scope—the process of answering important cancer-related inquires. Its potential to do so lies in its inherent capacity to comprehensively capture rich patient data and to directly support care standardization.” Other recent reports5, 6 have discussed the potential for IT to improve cancer care from both the patient’s vantage and as part of an overall system-improvement strategy. Figure 1 summarizes these complex connections and the potential for IT to facilitate care delivery.
Figure 1.
Patient, provider, and system applications of information technology for cancer care
A 2010 IOM workshop summary on Rapid Learning Health Systems7 for cancer identified several elements that are important for improving care, including electronic registries, a national cancer database, and electronic health record (EHR)–based tools for point-of-care decision support. Although the Office of the National Coordinator for Health Information Technology has formulated a roadmap for an IT-enabled U.S. healthcare system,8 we are years away from overcoming the technical, structural, ethical/legal, and cultural barriers to a national health information infrastructure. Nonetheless, the needs of cancer patients demand that these barriers be addressed, and a growing number of IT resources and tools can help pave the way. Some idealized conceptions of how IT could support patient-centered cancer care are spurred by real examples encountered in the current research and presented in Table 1.
Table 1.
Examples of how IT could support patient-centered cancer care.
| Diagnosis: A patient whose provider suspects cancer orders a diagnostic PET scan. The resulting digital image is captured, annotated, stored, and shared with a provider in a different location for a second opinion, vastly improving the efficiency, effectiveness, and timeliness of care. |
| Treatment Decisions: Any given patient has a range of values, preferences, needs, communication and learning styles, and cultural considerations. For example, a male patient for whom English is a second language, and whose cultural norms encourage passivity, modesty, and deference around physicians, may be unwilling to voice questions about side effects of different prostate cancer treatment options. In this scenario, the ideal IT system could capture and dynamically monitor the patient’s values and preferences, anticipate possible questions and concerns about urological and sexual functioning, and even produce treatment information in another language, or in one of several alternative formats (e.g., print, DVD, podcast). |
| Symptom Management: An optimal IT-enabled system for cancer care could aid providers and patients in handling cancer treatment-related side effects if patients could report problems by accessing a web- or telephone-based symptom reporting system that immediately transfers the symptom data into the patient’s EHR. Depending on intensity and duration of the symptoms, the healthcare team could initiate proactive outreach to the patient by secure email or phone, or at the least, review the symptom trajectory during a subsequent visit. The symptom record would be accessible to all of the patient’s providers (primary care, radiation oncology, medical oncology), irrespective of the provider’s practice setting. |
EHR, electronic health record; IT, information technology
What Can Information Technology Do for Cancer Care Now?
Sittig9 envisioned a cancer care environment in 2015 where technologic innovations from web-enabled mobile devices, integrated patient phenotype and genotype databases for individualized treatment, and real-time decision support, could potentially enhance the clinical, organizational and relational aspects of care. Because many individuals are already within a care delivery practice or system at the time of cancer diagnosis, these tools can be useful across the continuum of cancer care to address prevention, diagnosis, treatment and survivorship.
Recent research focuses on how HIT can empower patients to become more involved in their cancer care. Individuals commonly search the Internet for health information (www.pewinternet.org), and data from a nationally representative survey revealed that nearly half of all Americans have sought cancer-related information on the web.10, 11 Eysenbach et al12–15 describe evidence suggesting that the Internet may have an impact on cancer patients in four areas: communication (e.g., e-mailing doctors), community (e.g., “virtual support groups”), web-based health information, and e-commerce (e.g., purchasing medications). Depending on needs, web sophistication, and familiarity with the specifics of their cancer, the Internet can help or hinder patients and their caregivers in these areas.
Though several studies13–15 note that the Internet has not completely replaced information-seeking from health professionals, family/friends, and print products, it has clearly emerged as an important means of meeting informational needs of cancer patients, particularly for treatment-related information.16 To help ensure the quality and accuracy of cancer information, a patient-focused Association of Online Cancer Resources (www.acor.org) aims to provide credible Internet-based resources and content for cancer patients.
Beyond information seeking, IT provides resources for social and emotional support of cancer patients and their caregivers. Given the distress and uncertainty that inevitably accompanies a cancer diagnosis, virtual social support groups are a way for patients to find coping strategies and share experiences. The ACOR website has hosted cancer-related Internet mailing lists for both patients and caregivers since 1995. Another example is the Comprehensive Health Enhancement Support System (CHESS), developed nearly 2 decades ago.17 CHESS was founded on the principles of “making high-quality information and social support accessible and useful,” and enabling patients to “become…actively involved in their treatment and recovery.” CHESS has been instrumental in shaping understanding of how electronic information can help patients with information and support needs.18–21 Promising approaches to integrating CHESS into routine care delivery,22 and making it available through the NCI’s Cancer Information System are under way.23
Improved cancer management through IT has received considerable research attention in shared decision making, symptom management, and treatment adherence literature. Decision aids guide patients (and providers) toward an informed choice in situations where different treatments entail tradeoffs based on preferences and values. IT-enabled decision aids could be individually tailored, highly interactive, and scalable, whereas many treatment decision aids today are a generic comparison of treatment options (e.g., mastectomy vs lumpectomy). Patient-focused interactive decision aids have been developed for breast cancer surgery24 and are under development for prostate cancer treatment. Other emerging tools such as Adjuvant! Online (www.adjuvantonline.com) and the Cancer Profiler Tool provided by LiveSTRONG and NexCURA (www.nexprofiler.nexcura.com) offer personalized treatment options based on patient characteristics.
Treatment adherence may be disrupted if patients experience distress, bothersome side effects, or adverse events. Comprehensive symptom management lends itself to incorporating IT tools. A recent report of an automated system to identify distress among cancer patients described the ability to auto-notify appropriate professionals (e.g., severe pain triaged to physician, nausea triaged to nurse, depression triaged to psychologist), when patients reported treatment-related symptoms. Such a system keeps all relevant providers aware of patients’ evolving medical and psychosocial needs.25
A small feasibility study26 tested instant delivery of tailored advice about chemotherapy symptoms through handheld computers and reported that patients and providers found this strategy feasible and acceptable. Ruland et al27 evaluated a computerized symptom management system in which patients tracked experiences with a tablet computer, and data were incorporated into planning in-person visits with clinicians, allowing the patient’s primary symptom management needs to be addressed in detail. Basch and colleagues28 developed an online platform for patient-reported outcomes related to chemotherapy based on standard criteria for toxicity monitoring, which was well accepted by patients and providers. Existence of this standardized reporting criteria tool has, itself, led to an interesting IT advance—a related smart phone application.
Although the use of smartphones and web-based personal health record (PHR) tools such as HealthVault, Dossia, or the Google Health™ program to store health information and access it online in partnership with multiple providers is increasing, cancer care seems to lag behind compared with other healthcare applications.29, 30 Project HealthDesign is studying pragmatic and conceptual aspects of incorporating PHRs into patients’ daily lives and healthcare decisions using mobile phones and other online tools, including an exploratory examination of a customized care planning tool for breast cancer patients.31
Challenges and opportunities for patient-focused information technology and cancer care
Despite growing evidence that IT has great potential to improve care, results are mixed. One randomized trial of a mobile phone–based symptom-reporting system reported benefits to patients in the intervention group,32 but another study33 noted that their sample of 477 cancer patients preferred more “traditional” means of symptom reporting (e.g., paper, calling a nurse, in-person visit), compared with secure websites, text-messaging, or interactive voice response. Persistent challenges related to information-seeking include the credibility and trustworthiness of web-based information, and the uneven access to web-based resources among different subpopulations.34–36 Consumers’ and patients’ ability to critically evaluate web-based health information is another understudied area that may be only exacerbated by the rapid proliferation of “Web 2.0” technologies (e.g., social media sites, web blogs) of questionable scientific accuracy.37 Helping vulnerable populations navigate online cancer information also is critical,38 as are tools for older adults and the chronically ill who may be less technologically adept.
Security of personal health information is particularly important for cancer patients, who may feel vulnerable or fear discrimination by insurers or employers. Patients may benefit from a portable PHR on a device (e.g., a flash drive) or website, but interoperability and privacy are key concerns, especially as health information is shared across providers or systems. Patients and providers also may not always share perspectives on the use of portable health records. A recent review article39 noted that as patients turn to the Internet to obtain health information, the patient–provider dynamic may shift in various ways—some providers may feel threatened by highly activated patients; others may welcome the opportunity to collaborate with informed patients.
Information Technology Improvements for Providers and Healthcare Systems
Several reports identify decision support, care coordination, and continuity of care as areas where IT could substantively transform and improve cancer care delivery.40–42
Computerized decision support at the point of care
Galligioni et al.43, 44 have described their experiences developing and using web-based oncology medical records to support shared patient care. These records were carefully designed to integrate the spectrum of cancer care management tasks, from appointment making and information sharing among providers, to chemotherapy sequencing and toxicity monitoring. Their experience exemplifies how wide EHR adoption could embed oncology care innovations into health systems. EpicCare (www.epicsystems.com), an EHR software system deployed for nearly 200 clients (150,000 physicians), including several large integrated delivery systems, has an optional oncology module with comprehensive decision support, chemotherapy dosing schedules, personalized treatment planning, and support for diagnostic staging. Kaiser Permanente is implementing this oncology module, which will provide an unparalleled opportunity for care coordination and shared treatment decision making, given Kaiser’s large enrollee population. The American Society of Clinical Oncology website (www.asco.org) also provides guidance for practitioners around oncology EHRs, describing ideal functionality, and how to select, implement and use EHRs in daily practice.
Do embedded electronic guidelines influence treatment selection, prevent errors, or ensure dosing safety for cancer patients? Such guidelines are used routinely in areas other than cancer, and have been shown to improve both quality and outcomes of cancer screening. This literature is less well-developed in cancer treatment. A study examining whether computerized reminders could ensure appropriate prescribing of erythropoietin for chemotherapy-induced anemia found better prescribing adherence in the intervention group, which received electronic “triggers” when warranted based on patients’ hemoglobin levels.45 Given the numerous decision points throughout a cancer patient’s diagnosis and treatment, opportunities to test and eventually implement other point-of-care decision support strategies appear promising. However, few empirical studies exist specifying optimal design factors to consider when incorporating point-of-care alerts into practice.46 Given the challenging treatment considerations in cancer care, it is important to identify the key features, timing, and other aspects of designing and implementing computerized order entry and related decision support systems, to ensure that tailored clinical solutions do not create new barriers to provider–patient communication.47
The clinical trial enterprise offers several opportunities for IT to improve care.48 Given the well acknowledged problems of inefficient, incomplete, or slow accrual to trials,49–51 a rapid computerized notification system to identify potentially eligible patients is one possible solution. Such a system of embedding in the EHR alerts of clinical trial matches for potentially eligible patients is being tested at Kaiser Permanente. A small study52 exploring benefits and barriers to the use of a PDA to provide clinical trial listings highlighted several challenges, including currency of information and nonstandard taxonomy for categorizing trials (e.g., “stage IV” vs “metastatic”). Absence of a widely adopted technology-driven solution for the trial accrual problem underscores the myriad challenges in this area.
Ensuring coordination and continuity of care
Continuity of care, described as “systematic assurance of uninterrupted, integrated medical and psychosocial care of the [cancer] patient”,42 rooted in the provider–cancer patient partnership, is important in cancer care. Haggerty and colleagues53 noted that the main dimensions of continuity of care are informational, relational, and management. These dimensions are closely tied to care coordination. Transitions in care entail extensive information sharing, timely appointments for work-up, and sometimes reconciliation of different recommendations. Patients often serve as their own care coordinators, arranging appointments, being the nexus for information, and navigating the many steps in their care. Even in settings with established cancer care coordinator functions, breakdowns are possible. Incomplete sharing of information between primary and specialty care providers was cited in a recent study, as well as patients “falling through the cracks” when treatment occurs in one or more settings.54
The multidisciplinary approach to cancer care is certainly essential to determining the right treatment strategy, but as noted by Nouraei et al,55 ensuring that patients receive appropriate care represents a “formidable organizational challenge in coordinating the input of multiple specialties.” This group implemented a centrally accessible database to reduce delays and furnish information expediently to the many providers responsible for caring for patients with head and neck cancer. Although the database was a relatively simple intervention, it was undertaken with careful attention to process workflow planning, coordination among providers and information accessibility.
New regulations on meaningful use of EHRs acknowledge the importance of care coordination and emphasize that HIT infrastructure is a means—not an end. Reflecting these ideas, proposed criteria for ensuring that certified EHRs are used meaningfully require that the underlying technology of the EHR supports disease management and transitions between care settings.56 One notable caution is that in a shared IT environment, an error or mis-statement in one chart may be inadvertently propagated when shared electronically with another provider or system. Still, an IT-enabled system of care could reduce errors and other breakdowns, automating where it makes sense, but not supplanting the relational aspects of cancer care. EHRs and systems that track and share information among providers about the patient’s experience can reinforce a deeper understanding of patients’ values, preferences, and how health events may interrelate. Development and deployment of oncology treatment summaries is probably the best example of how IT solutions may foster care coordination and enhance continuity of care between cancer specialists and patients,57 and between one cancer specialist and other clinicians.58
Measurement Issues in Modern Cancer Care
Successful 21st century cancer care organizations will be learning systems, able to measure patterns of performance that are critical to patient care and organizational survival.1, 7, 59 Organizational learning—which is used here to describe the capability of a practice or system to acquire new information, modify interdependent processes, and ultimately change (improve) how it works—requires more than IT. It requires availability of appropriate content, structured and standardized in ways that are meaningful to patients, practitioners, and administrative staff, and accessible for monitoring, decision support, and quality improvement. Organizational learning is a function of the quality of measurement and the capability of IT to ensure successful acquisition and transmission of this information at the appropriate time and place. Given cancer’s complex presentation in clinical practice, measuring and applying knowledge about optimal care is further considered below.
Improving the knowledge base
High-performing modern cancer care organizations are knowledge-based in that they use scientific evidence to guide decision making. In clinical practice, this means pairing evidence-based medicine with evidence-based management directed to improving clinical effectiveness.60 This issue is relevant in cancer care as studies find both underuse of guideline-based care61, 62 and overuse of services.63
Table 2 describes several ongoing measurement initiatives. All of these can be characterized as passive quality measurement systems, where performance data are collected after care has been delivered. Feedback lags range from several months, in the case of the Quality Oncology Practice Initiative (QOPI), to almost 2 years for measurement systems that rely on cancer registries as the source of data collection and reporting. The Commission on Cancer (CoC) recently launched a pilot program to test near real-time reporting and tracking of breast and colorectal cancer patients as part of a Rapid Quality Reporting System (RQRS) project.7 The RQRS identifies candidate patients soon after surgery and prospectively tracks them throughout their cancer treatment. The system can electronically alert participating facilities to enable them to follow patients and determine whether compliance with guidelines is achieved. This prospective measurement system is still undergoing pilot-testing, but preliminary evidence suggests that test sites improve adherence (M. Johnson, personal communication, 2010).
Table 2.
Selected National Performance Measurement Systems for Cancer Diagnosis and Treatment Indicators, 2010
| Sponsor | Date Program Originated |
Data Sources |
Cancer Clinical Effectiveness Domains |
Source of Guidelines |
Users | Provider Quality Improvement |
National or Regional Benchmarking |
Peer to Peer Comparison |
Public Reporting |
|---|---|---|---|---|---|---|---|---|---|
| ACS/ (CoC) EQUIP | 2007 | Cancer Registries |
|
NCCN, ASCO, ACS | 1460 CoC Accredited Cancer Centers | YES | YES | NO | NO |
| ASCO, Quality Oncology Practice Initiative (QOPI) | 2006 | Medical Records |
|
ASCO, NCCN | 238 Medical Oncologists’ and Hematologists’ Practices | YES | YES | NO | NO |
| NCCN, Outcomes Research Database | 1998 | Cancer Registries, medical Records |
|
NCCN | 21 Comprehensive Cancer Centers | YES | YES | YES | NO |
| ASTRO, PAAROT | 2008 | Medical Records |
|
ASTRO, ACR | 156 Radiation Oncologist Practices | YES | YES | NO | NO |
ACR, ACS, American College of Surgeons; ASCO, American Society of Clinical Oncology; ASTRO, American Society of Therapeutic Radiation Oncology; CoC; Commission on Cancer; EQUIP, NCCN, National Comprehensive Cancer Network; PAAROT, Performance Assessment for the Advancement of Radiation Oncology Treatment
These large-scale initiatives illustrate efforts to develop clinical effectiveness measures in cancer care. Their systems are more prevalent for some cancers (e.g., colorectal and breast) than others, and focus more on initial diagnosis and treatment phase of care, rather than survivorship and end-of-life care. Also, these measures are typically directed at large institutions and cancer specialty physicians, and rarely receive attention in community clinics or primary care settings. Few studies have assessed optimal methods for capturing and reporting the clinical information from medical records necessary to support and sustain these measurement systems in practice-based IT environments.
This knowledge gap is especially relevant for cancer care where many quality measurement systems are still evolving from paper-based chart abstraction to electronic platforms. For example, evidence from the NCI Community Cancer Centers Program (NCCCP) suggests a major barrier to sustained participation in a quality improvement collaborative using QOPI is whether the oncology practice has a functioning EHR.64 Nevertheless, recent efforts to develop and deploy these measures show willingness among cancer organizations to regard quality measurement and improvement as a high priority.
Enhancing patient-centered care
Patient-centered cancer care focuses on the preferences, needs, and overall experience of cancer patients, as defined by patients themselves and their families. Interest has grown in incorporating patient perspectives into measurement systems that evaluate cancer care delivery, either in terms of measuring and interpreting the clinical benefit of therapies or the patient care experience. However, to be useful in cancer care delivery, IT infrastructure is needed to capture these measures throughout the entirety of a patient’s treatment. Thus, a compelling “business case” is essential for persuading IT vendors to build and deploy applications that support: longitudinal data collection on patient experiences, computer adaptive technology for patient and practitioner reporting and feedback, and organizational studies on incorporating these measures in clinical practice.
Broadly defined, patient-reported outcomes (PROs) comprise information from patients that reflect on the health-related quality of life (HRQOL) that patients experience from a disease and its treatment. As described above, cancer diagnosis and treatment are often associated with high distress and toxicity, resulting in burdensome symptoms, like fatigue and pain, that are best measured by asking the patient directly. Considerable evidence shows that these side effects are often deemphasized in cancer diagnosis and treatment,65 and clinicians tend to systematically report fewer symptoms of lower severity compared with patient reports.66 Patients’ symptom reports also have been correlated with adverse outcomes, including functional and emotional disability and rehospitalization.67
Despite decades of research on cancer HRQOL in clinical trials, research on its application in clinical practice is a newer development.68, 69 A recent symposium described promising use of HRQOL instruments in clinical practice, especially for their ability to screen for functional problems, improve clinician–patient interactions, and address quality of care from the patient perspective.70 Yet, considerable barriers remain, including low acceptance of the clinical utility of these measures by physicians; lack of standardized, IT-enabled measurement and data collection that integrate seamlessly into practice; lack of guidelines on incorporating and using these measures in clinical workflow and decision making; and difficulty adapting these measures and their meaning to the increasingly complex cultural, language, and communication preferences of cancer patients.
Cancer organizations, especially cancer centers, have been engaged in patient satisfaction reporting and tracking of global ratings of care for years. However, fewer cancer organizations have focused measurement on the broader construct of patient experience that includes other attributes of the healthcare encounter considered valuable to patients (e.g., access, patient–physician communication, satisfaction with decision making regarding care planning and treatment). Many qualitative and population-based studies document that patient reports on these attributes are considered the gold standard of care assessment.71 Yet, because many measurement systems used by cancer organizations are proprietary, little published research is available that directly assesses the utility of these measurement systems for quality management and improvement in care delivery. Most randomized trials in this area focus on patient–clinician communication and decision quality. Few of these studies use proprietary measures of patient experience widely used in cancer organizations as either primary or secondary end points. Beyond communication and decision quality, only a few nonrandomized studies are available to assess relationships between PRO measures and improved patient-centered cancer care in actual care delivery settings72, 73.
Efforts are underway by federal agencies to expand the availability of cancer-related patient experience measurement systems for research and practice. NCI and AHRQ are sponsoring development of quality indicators of effective patient–clinician communication in cancer care, and are collaborating on a cancer module of the Consumer Assessment of Healthcare Plans Survey. Hopefully, development of actionable patient communication quality indicators and measurement systems like these will accelerate research on their use by diverse cancer care providers across communities and settings.
Enabling systems-minded approaches
Systems-minded cancer care organizations examine the entire care system in a holistic way, intervening—if necessary—to optimize care coordination and continuity. As described earlier, nowhere is that need more evident in modern healthcare than with the increasing use of multispecialty cancer care. Design and assessment of multidisciplinary care centers is emerging. These centers view care coordination as a specialty challenge, enhancing teamwork and communication across cancer surgeons, radiation oncologists, and medical oncologists in treatment planning and execution.74 More work is needed (especially in community settings) to incorporate the primary care physician as part of the definition and to measure care coordination, especially when considering the ubiquitous interfaces between primary care and specialty care throughout the cancer care continuum.75
Measures also are needed that enable patients’ assessments of care coordination. Patients cannot be expected to accurately assess the nature and quality of information exchange within their care team, but they can recognize when care coordination is lacking, be it during the hand-offs between physicians (e.g., lack of familiarity of physicians with prior treatment histories), or in the confusion over next steps in care delivery (either by themselves or by other members of their care team).
Conclusion
The importance of IT in supporting and enhancing patient-centered cancer care delivery is compelling in theory, and evidence of tangible progress is growing. Highly integrated systems like Kaiser Permanente and the Veterans Administration Health System have been recognized as pioneers in developing IT-enabled solutions. Multiple studies have documented increased satisfaction of providers and patients in these closed systems, compared to open systems that accept patients from multiple health plans.76, 77 However, these healthcare systems are the exception, rather than the rule, in cancer care delivery today.
Multiple examples exist of cancer researchers and providers coming together in informal or formal networks to experiment on elements of patient-centered care. Some of the most promising arrangements focus on practice-based research in networks like the Cooperative Trial Groups,78 the National Comprehensive Cancer Network,79 the Cancer Research Network,80 and the NCCCP. These virtual research groups are, albeit slowly, focusing on networkwide research to implement and deliver aspects of patient-centered care that emphasize IT solutions. These networks strive to improve care by raising awareness of their own performance, sharing performance results with network peers and the broader practice community, and disseminating best practices and tools for quality improvement.
These new developments hold promise for accelerating the use of patient-centered care IT tools and enhancing the evidence base for effectively deploying them in diverse cancer delivery settings. Yet the sustainability of these solutions in our current fragmented system is questionable given that benefits of these programs often do not accrue in the same way to the same stakeholders. Leatherman et al81 found that the financial benefit of quality improvement initiatives to reduce unnecessary utilization often did not accrue to the provider in fee-for-service settings even though they were making important changes to implement the intervention. The system simply did not provide the right incentives to make it happen.
Payers and policymakers have been challenged to realign incentives across the healthcare system and have started pilot projects such as the 2006 Medicare “pay for reporting” medical oncology quality demonstration.82 A place to start in realigning incentives toward a patient-centered approach to modern cancer care might be to reward cancer organizations that deploy IT solutions that collect the appropriate data and build the required infrastructure for data collection, reporting, and sharing among clinical teams, patient teams, and payers.
Where do we go from here?
This paper has contended that IT is a foundational element for patient-centered care, but must be thoughtfully linked with other considerations relevant to the cancer care environment. First, we need the right information and the right measures, both of which are responsive to the needs of organizations, clinicians, and patients. This includes robust measurement of clinical effectiveness, care coordination, patient experience, and other PROs—potentially, a “vital sign” to measure patient-centered cancer care, monitored over time. Second, IT must be deployed in a way that that connects providers and patients and facilitates positive communication throughout care systems. Hesse et al. note that IT is not a panacea; user-centered design approaches and attention to the sociotechnical aspects of complex systems are equally critical.5
Finally, IT must do more than just inform patients about their cancer care. It must embrace new technologies, adapt to and enhance the changing roles and relationships between formal care teams and the patient team (patients and families), and recognize the interdependency of patient, providers, systems, and technologies in the care delivery process. Patients cannot effectively diagnose or treat their cancer, and care teams cannot provide highest quality care without meaningful patient involvement. Recognizing these interdependencies will be critical to the effective deployment of IT solutions for patient-centered care.
Acknowledgements
The writing group takes sole responsibility for the content of this article. Content reflects the views of the authors only. This work was supported by the National Cancer Institute (Contract: PO 263-MQ-516309; Grant: CA 79689). We thank Beth Kirlin and Virginia Scobba for assistance with article retrieval, and Anne Rodgers for thoughtful editorial suggestions. Publication of this article was supported by the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.IOM, editor. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2.IOM, Committee on Psychosocial Services to Cancer Patients/Families in a Community Setting, Board on Health Care Services. Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs; Washington, D.C.: The National Academies Press; 2007. Oct 23, [Google Scholar]
- 3.Realizing the Full Potential of Health Information Technology to Improve Healthcare for Americans: The Path Forward Washington, DC. 2010 [Google Scholar]
- 4.Wallace PJ. Reshaping cancer learning through the use of health information technology. Health Aff (Project Hope) 2007;26(2) doi: 10.1377/hlthaff.26.2.w169. [DOI] [PubMed] [Google Scholar]
- 5.Hesse BW, Hanna C, Massett HA, Hesse NK. Outside the Box: Will Information Technology Be a Viable Intervention to Improve the Quality of Cancer Care? Natl Cancer Inst Monogr. 2010;2010(40):81–89. doi: 10.1093/jncimonographs/lgq004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shortliffe EH, Sondik EJ. The public health informatics infrastructure: anticipating its role in cancer. Cancer Causes Control. 2006;17(7):861–869. doi: 10.1007/s10552-006-0028-4. [DOI] [PubMed] [Google Scholar]
- 7.IOM. A Foundation for Evidence-Driven Practice: A Rapid Learning System for Cancer Care: Workshop Summary; Washington DC. 2010. [PubMed] [Google Scholar]
- 8.Nationwide Health Information Exchange Architecture Overview. Nationwide Health Information Network; 2010. Available from: < http://healthit.hhs.gov/portal/server.pt/gateway/PTARGS_0_11113_911643_0_0_18/NHIN_Architecture_Overview_Draft_20100421.pdf>. [Google Scholar]
- 9.Sittig DF. Potential impact of advanced clinical information technology on cancer care in 2015. Cancer Causes Control. 2006;17(6):813–820. doi: 10.1007/s10552-006-0020-z. [DOI] [PubMed] [Google Scholar]
- 10.Rutten LJF, Squiers L, Hesse BW. Cancer-Related Information Seeking: Hints from the 2003 Health Information National Trends Survey (HINTS) Journal of Health Communication: International Perspectives. 2006;11(1 supp 1):147–156. doi: 10.1080/10810730600637574. [DOI] [PubMed] [Google Scholar]
- 11.Hesse BW, Nelson DE, Kreps GL, Croyle RT, Arora NK, Rimer BK, et al. Trust and sources of health information: the impact of the Internet and its implications for health care providers: findings from the first Health Information National Trends Survey. Arch Intern Med. 2005;165(22):2618–2624. doi: 10.1001/archinte.165.22.2618. [DOI] [PubMed] [Google Scholar]
- 12.Eysenbach G. The impact of the Internet on cancer outcomes. CA Cancer J Clin. 2003;53(6):356–371. doi: 10.3322/canjclin.53.6.356. [DOI] [PubMed] [Google Scholar]
- 13.Basch EM, Thaler HT, Shi W, Yakren S, Schrag D. Use of information resources by patients with cancer and their companions. Cancer. 2004;100(11):2476–2483. doi: 10.1002/cncr.20261. [DOI] [PubMed] [Google Scholar]
- 14.Hardyman R, Hardy P, Brodie J, Stephens R. It's good to talk: comparison of a telephone helpline and website for cancer information. Patient Educ Couns. 2005;57(3):315–320. doi: 10.1016/j.pec.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Pereira JL, Koski S, Hanson J, Bruera ED, Mackey JR. Internet usage among women with breast cancer: an exploratory study. Clin Breast Cancer. 2000;1(2):148–153. doi: 10.3816/CBC.2000.n.013. discussion 154–5. [DOI] [PubMed] [Google Scholar]
- 16.Rutten LJ, Arora NK, Bakos AD, Aziz N, Rowland J. Information needs and sources of information among cancer patients: a systematic review of research (1980–2003) Patient Educ Couns. 2005;57(3):250–261. doi: 10.1016/j.pec.2004.06.006. [DOI] [PubMed] [Google Scholar]
- 17.Taylor JO, Gustafson DH, Hawkins R, Pingree S, McTavish F, Wise M, et al. The comprehensive health enhancement support system. Qual Manag Health Care. 1994;2(4):36–43. [PubMed] [Google Scholar]
- 18.Comprehensive Health Enhancement Support System (CHESS) [Google Scholar]
- 19.Gustafson DH, Hawkins R, Boberg E, Pingree S, Serlin RE, Graziano F, et al. Impact of a patient-centered, computer-based health information/support system. Am J Prev Med. 1999;16(1):1–9. doi: 10.1016/s0749-3797(98)00108-1. [DOI] [PubMed] [Google Scholar]
- 20.Gustafson DH, Hawkins RP, Boberg EW, McTavish F, Owens B, Wise M, et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. Int J Med Inform. 2002;65(3):169–177. doi: 10.1016/s1386-5056(02)00048-5. [DOI] [PubMed] [Google Scholar]
- 21.Gustafson DH, McTavish FM, Stengle W, Ballard D, Hawkins R, Shaw BR, et al. Use and impact of ehealth system by low-income women with breast cancer. J Health Commun. 2005;10 Suppl 1:195–218. doi: 10.1080/10810730500263257. [DOI] [PubMed] [Google Scholar]
- 22.The Center for Health Enhancement Systems Study. Available from: < http://chess.wisc.edu/chess/projects/eHealth.aspx>.
- 23.Reynolds S. NCI Cancer Bulletin. 2010. Using e-health tools to improve quality of life for cancer patients; p. 4. [Google Scholar]
- 24.Whelan T, Levine M, Willan A, Gafni A, Sanders K, Mirsky D, et al. Effect of a decision aid on knowledge and treatment decision making for breast cancer surgery: a randomized trial. JAMA. 2004;292(4):435–441. doi: 10.1001/jama.292.4.435. [DOI] [PubMed] [Google Scholar]
- 25.Loscalzo M, Clark K, Dillehunt J, Rinehart R, Strowbridge R, Smith D. SupportScreen: A Model for Improving Patient Outcomes. Journal of the National Comprehensive Cancer Network. 2010;8(4):496–504. [Google Scholar]
- 26.Kearney N, Kidd L, Miller M, Sage M, Khorrami J, McGee M, et al. Utilising handheld computers to monitor and support patients receiving chemotherapy: results of a UK-based feasibility study. Support Care Cancer. 2006 doi: 10.1007/s00520-005-0002-9. [DOI] [PubMed] [Google Scholar]
- 27.Ruland CM, Holte HH, Roislien J, Heaven C, Hamilton GA, Kristiansen J, et al. Effects of a computer-supported interactive tailored patient assessment tool on patient care, symptom distress, and patients' need for symptom management support: a randomized clinical trial. J Am Med Inform Assoc. 2010;17(4):403–410. doi: 10.1136/jamia.2010.005660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Basch E, Jia X, Heller G, Barz A, Sit L, Fruscione M, et al. Adverse Symptom Event Reporting by Patients vs Clinicians: Relationships With Clinical Outcomes. J. Natl. Cancer Inst. 2009;101(23):1624–1632. doi: 10.1093/jnci/djp386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.California Health Care Foundation. How Smartphones Are Changing Health Care for Consumers and Providers. California Health Care Foundation; 2010. [Google Scholar]
- 30.Martin M. Smartphone Use Surges among Physicians. 2010 May 17; [Google Scholar]
- 31.Robert Wood Johnson Foundation. [cited 2010 June 27];Project Health Design. Available from: http://www.projecthealthdesign.org.
- 32.McCann L, Maguire R, Miller M, Kearney N. Patients' perceptions and experiences of using a mobile phone–based advanced symptom management system (ASyMS) to monitor and manage chemotherapy related toxicity. Eur J Cancer Care (Engl) 2009;18(2):156–164. doi: 10.1111/j.1365-2354.2008.00938.x. [DOI] [PubMed] [Google Scholar]
- 33.Kleiboer A, Gowing K, Holm Hansen C, Hibberd C, Hodges L, Walker J, et al. Monitoring symptoms at home: what methods would cancer patients be comfortable using? Qual Life Res. 2010 doi: 10.1007/s11136-010-9662-0. [DOI] [PubMed] [Google Scholar]
- 34.Berland GK, Elliott MN, Morales LS, Algazy JI, Kravitz RL, Broder MS, et al. Health Information on the Internet: Accessibility, Quality, and Readability in English and Spanish. JAMA. 2001;285(20):2612–2621. doi: 10.1001/jama.285.20.2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Helft PR, Eckles RE, Johnson-Calley CS, Daugherty CK. Use of the Internet to obtain cancer information among cancer patients at an urban county hospital. J Clin Oncol. 2005;23(22):4954–4962. doi: 10.1200/JCO.2005.09.621. [DOI] [PubMed] [Google Scholar]
- 36.Shim M. Connecting Internet use with gaps in cancer knowledge. Health Commun. 2008;23(5):448–461. doi: 10.1080/10410230802342143. [DOI] [PubMed] [Google Scholar]
- 37.Eysenbach G, Powell J, Kuss O, Sa ER. Empirical studies assessing the quality of health information for consumers on the world wide web: a systematic review. JAMA. 2002;287:2691–2700. doi: 10.1001/jama.287.20.2691. [DOI] [PubMed] [Google Scholar]
- 38.Neuhauser L, Kreps GL. Online cancer communication: meeting the literacy, cultural and linguistic needs of diverse audiences. Patient Educ Couns. 2008;71(3):365–377. doi: 10.1016/j.pec.2008.02.015. [DOI] [PubMed] [Google Scholar]
- 39.McMullan M. Patients using the Internet to obtain health information: how this affects the patient–health professional relationship. Patient Educ Couns. 2006;63(1–2):24–28. doi: 10.1016/j.pec.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 40.Aiello Bowles EJ, Tuzzio L, Wiese CJ, Kirlin B, Greene SM, Clauser SB, et al. Understanding high-quality cancer care: a summary of expert perspectives. Cancer. 2008;112(4):934–942. doi: 10.1002/cncr.23250. [DOI] [PubMed] [Google Scholar]
- 41.IOM. Ensuring Quality Cancer Care. Washington, D.C.: National Academy Press; 1999. [Google Scholar]
- 42.Lauria MM. Continuity of cancer care. Cancer. 1991;67(6 Suppl):1759–1766. doi: 10.1002/cncr.2820671812. [DOI] [PubMed] [Google Scholar]
- 43.Forti S, Galvagni M, Galligioni E, Eccher C. A real time teleconsultation system for sharing an oncologic web-based electronic medical record. AMIA Annu Symp Proc. 2005:959. [PMC free article] [PubMed] [Google Scholar]
- 44.Galligioni E, Berloffa F, Caffo O, Tonazzolli G, Ambrosini G, Valduga F, et al. Development and daily use of an electronic oncological patient record for the total management of cancer patients: 7 years' experience. Annals of Oncology. 2009;20(2):349–352. doi: 10.1093/annonc/mdn567. [DOI] [PubMed] [Google Scholar]
- 45.Kralj B, Iverson D, Hotz K, Ashbury FD. The impact of computerized clinical reminders on physician prescribing behavior: evidence from community oncology practice. Am J Med Qual. 2003;18(5):197–203. doi: 10.1177/106286060301800504. [DOI] [PubMed] [Google Scholar]
- 46.Schedlbauer A, Prasad V, Mulvaney C, Phansalkar S, Stanton W, Bates DW, et al. What evidence supports the use of computerized alerts and prompts to improve clinicians' prescribing behavior? Am Med Inform Assoc. 2009;16(4):531–538. doi: 10.1197/jamia.M2910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pearce C, Trumble S. Computers can't listen—algorithmic logic meets patient centredness. Aust Fam Physician. 2006;35(6):439–442. [PubMed] [Google Scholar]
- 48.IOM. A National Cancer Clinical Trials System for the 21st Century: Reinvigorating the NCI Cooperative Group Program. Washington DC: 2010. [PubMed] [Google Scholar]
- 49.Dilts DM, Sandler AB. Invisible Barriers to Clinical Trials: The Impact of Structural, Infrastructural, and Procedural Barriers to Opening Oncology Clinical Trials. J Clin Oncol. 2006;24(28):4545–4552. doi: 10.1200/JCO.2005.05.0104. [DOI] [PubMed] [Google Scholar]
- 50.Murthy VH, Krumholz HM, Gross CP. Participation in Cancer Clinical Trials: Race-, Sex-, and Age-Based Disparities. JAMA. 2004;291(22):2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- 51.Sateren WB, Trimble EL, Abrams J, Brawley O, Breen N, Ford L, et al. How Sociodemographics, Presence of Oncology Specialists, and Hospital Cancer Programs Affect Accrual to Cancer Treatment Trials. J Clin Oncol. 2002;20(8):2109–2117. doi: 10.1200/JCO.2002.08.056. [DOI] [PubMed] [Google Scholar]
- 52.Monaco V, Jacobs SA, Arnold AM, Simon MB. Providing PDA-based clinical trial listings to oncologists. AMIA Annu Symp Proc. 2005:1056. [PMC free article] [PubMed] [Google Scholar]
- 53.Haggerty JL, Reid RJ, Freeman GK, Starfield BH, Adair CE, McKendry R. Continuity of care: a multidisciplinary review. BMJ. 2003;327(7425):1219–1221. doi: 10.1136/bmj.327.7425.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Walsh J, Harrison JD, Young JM, Butow PN, Solomon MJ, Masya L. What are the current barriers to effective cancer care coordination? A qualitative study. BMC Health Serv Res. 2010;10:132. doi: 10.1186/1472-6963-10-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nouraei S, Philpott J, Nouraei SM, Maude D, Sandhu GS, Sandison A, et al. Reducing referral-to-treatment waiting times in cancer patients using a multidisciplinary database. Ann Royal College Surgeons England. 2007;89(2):113–117. doi: 10.1308/003588407X155455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.DHHS. Health Information Technology: Initial Set of Standards, Implementation Specifications, and Certification Criteria for Electronic Health Record Technology; Final Rule. In. [PubMed] [Google Scholar]
- 57.IOM, National Research Council of the National Academies. From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, D.C: National Academy Press; 2006. [Google Scholar]
- 58.American Society of Clinical Oncology. Cancer Treatment Plan and Summary. In. [Google Scholar]
- 59.Abernethy AP, Etheredge LM, Ganz PA, Wallace P, German RR, Neti C, et al. Rapid-Learning System for Cancer Care. J Clin Oncol. 2010 doi: 10.1200/JCO.2010.28.5478. JCO.2010.28.5478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Shortell SM, Rundall TG, Hsu J. Improving Patient Care by Linking Evidence-Based Medicine and Evidence-Based Management. JAMA. 2007;298(6):673–676. doi: 10.1001/jama.298.6.673. [DOI] [PubMed] [Google Scholar]
- 61.Harlan LC, Greene AL, Clegg LX, Mooney M, Stevens JL, Brown ML. Insurance status and the use of guideline therapy in the treatment of selected cancers. J Clin Oncol. 2005;23(36):9079–9088. doi: 10.1200/JCO.2004.00.1297. [DOI] [PubMed] [Google Scholar]
- 62.Jessup JM, Stewart A, Greene FL, Minsky BD. Adjuvant Chemotherapy for Stage III Colon Cancer: Implications of Race/Ethnicity, Age, and Differentiation. JAMA. 2005;294(21):2703–2711. doi: 10.1001/jama.294.21.2703. [DOI] [PubMed] [Google Scholar]
- 63.Keating NL, Landrum MB, Guadagnoli E, Winer EP, Ayanian JZ. Surveillance Testing Among Survivors of Early-Stage Breast Cancer. J Clin Oncol. 2007;25(9):1074–1081. doi: 10.1200/JCO.2006.08.6876. [DOI] [PubMed] [Google Scholar]
- 64.Siegel RD, Clauser SB, Lynn JM. National Collaborative to Improve Oncology Practice: The National Cancer Institute Community Cancer Centers Program Quality Oncology Practice Initiative Experience. Journal of Oncology Practice. 2009;5(6):276–281. doi: 10.1200/JOP.091050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lipscomb J, Gotay CC, Snyder CF. Patient-reported outcomes in cancer: a review of recent research and policy initiatives. CA Cancer J Clin. 2007;57(5):278–300. doi: 10.3322/CA.57.5.278. [DOI] [PubMed] [Google Scholar]
- 66.Basch EM, Iasonos A, McDonough T, Barz A, Culkin A, Scher HI, Schrag D. Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: results of a questionnaire-based study. Lancet Oncol. 2006;7(11):903–909. doi: 10.1016/S1470-2045(06)70910-X. [DOI] [PubMed] [Google Scholar]
- 67.Bruner DW. Should Patient-Reported Outcomes Be Mandatory for Toxicity Reporting in Cancer Clinical Trials? J Clin Oncol. 2007;25(34):5345–5347. doi: 10.1200/JCO.2007.13.3330. [DOI] [PubMed] [Google Scholar]
- 68.Frost MH, Bonomi AE, Cappelleri JC, Schünemann HJ, Moynihan TJ, Aaronson NK, et al. Applying Quality-of-Life Data Formally and Systematically Into Clinical Practice. Mayo Clinic Proceedings. 2007;82(10):1214–1228. doi: 10.4065/82.10.1214. [DOI] [PubMed] [Google Scholar]
- 69.Velanovich V. Using quality-of-life measurements in clinical practice. Surgery. 2007;141(2):127–133. doi: 10.1016/j.surg.2006.10.002. [DOI] [PubMed] [Google Scholar]
- 70.Lohr K, Zebrack B. Using patient-reported outcomes in clinical practice: challenges and opportunities. Quality of Life Research. 2009;18(1):99–107. doi: 10.1007/s11136-008-9413-7. [DOI] [PubMed] [Google Scholar]
- 71.Arora N. Importance of patient-centered care in enhancing patient well-being: a cancer survivor’s perspective. Quality of Life Research. 2009;18(1):1–4. doi: 10.1007/s11136-008-9415-5. [DOI] [PubMed] [Google Scholar]
- 72.Moyer A, Sohl SJ, Knapp-Oliver SK, Schneider S. Characteristics and methodological quality of 25 years of research investigating psychosocial interventions for cancer patients. Cancer Treat Rev. 2009;35(5):475–484. doi: 10.1016/j.ctrv.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Cohen D, McDaniel RR, Jr, Crabtree BF, Ruhe MC, Weyer SM, Tallia A, et al. A practice change model for quality improvement in primary care practice. J Healthc Manag. 2004;49(3):155–168. discussion 169–70. [PubMed] [Google Scholar]
- 74.Fennell ML, Prabhu Das I, Clauser S, Petrelli N, Salner A. The Organization of Multidisciplinary Care Teams: Modeling Internal and External Influences on Cancer Care Quality. J Natl Cancer Inst Monogr. 2010;2010(40):72–80. doi: 10.1093/jncimonographs/lgq010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Taplin SH, Clauser S, Rodgers AB, Breslau E, Rayson D. Interfaces Across the Cancer Continuum Offer Opportunities to Improve the Process of Care. J Natl Cancer Inst Monogr. 2010;2010(40):104–110. doi: 10.1093/jncimonographs/lgq012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Mechanic D. Physician Discontent: Challenges and Opportunities. JAMA. 2003;290(7):941–946. doi: 10.1001/jama.290.7.941. [DOI] [PubMed] [Google Scholar]
- 77.Murray A, Montgomery J, Chang H, Rogers W, Inui T, Safran D. Doctor discontent. J General Internal Medicine. 2001;16(7):451–459. doi: 10.1046/j.1525-1497.2001.016007452.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dignam JJ. The role of cancer cooperative groups within the spectrum of cancer care. Cancer Control. 2004;11(1):55–63. doi: 10.1177/107327480401100210. [DOI] [PubMed] [Google Scholar]
- 79.Niland JC. NCCN outcomes research database: data collection via the Internet. Oncology (Williston Park) 2000;14(11A):100–103. [PubMed] [Google Scholar]
- 80.Hornbrook MC, Hart G, Ellis JL, Bachman DJ, Ansell G, Greene SM, et al. Building a virtual cancer research organization. J Natl Cancer Inst Monogr. 2005 35;:12–25. doi: 10.1093/jncimonographs/lgi033. [DOI] [PubMed] [Google Scholar]
- 81.Leatherman S, Ferris TG, Berwick D, Omaswa F, Crisp N. The role of quality improvement in strengthening health systems in developing countries. Int J Qual Health Care. 2010;22(4):237–243. doi: 10.1093/intqhc/mzq028. [DOI] [PubMed] [Google Scholar]
- 82.Doherty J, Tanamor M, Feigert J, Goldberg-Dey J. Oncologists' Experience in Reporting Cancer Staging and Guideline Adherence: Lessons From the 2006 Medicare Oncology Demonstration. Journal of Oncology Practice. 2010;6(2):56–59. doi: 10.1200/JOP.091083. [DOI] [PMC free article] [PubMed] [Google Scholar]