Abstract
Objectives
To provide a long-term look at suicide risk from adolescence to young adulthood for former participants in Promoting CARE, an indicated suicide prevention program.
Methods
Five hundred ninety-three suicide-vulnerable high school youth were involved in a long-term follow-up study. Latent class growth models identify patterns of change in suicide risk over this period.
Results
Three distinct trajectories are determined, all showing a maintenance of decreased suicide risk from postintervention in adolescence into young adulthood for direct suicide-risk behaviors, depression and anger. Intervention conditions as well as key risk/protective factors are identified that predict to the long-term trajectories.
Conclusion
Early intervention is successful in promoting and maintaining lower-risk status from adolescence to young adulthood, with the caveat that some high-risk behaviors may indicate a need for additional intervention to establish earlier effects.
Keywords: suicide-risk behaviors, suicide prevention, long-term behavior change, adolescence, transition to adulthood
The prevalence and persistence of adolescent and young adult suicide and suicide-related behaviors represent a significant health problem. Recent results from a large nationwide survey of 9th -through 12th -grade high school students indicated that 15% of students had seriously considered attempting suicide, 11% had made a specific plan to attempt suicide, and 7% had attempted suicide during the 12 months preceding the survey.1 These findings are consistent with other research reports involving high school samples2–6 and document the importance of attending to youth suicide-risk behaviors during the high school years. Suicide risk, however, is not limited to the high school years: rates for suicide risk, particularly death by suicide, is actually higher in young adulthood,7 as opposed to other adolescent risk behaviors (such as drug use), which often level off or reduce during this period.8 These suicide-risk patterns indicate a lengthier period of vulnerability than previously thought and pose an additional task – attending to the course of suicide risk beyond youth and into young adulthood – for the prevention scientists, policy makers, and practitioners concerned about youth suicide. The study reported in this paper explores the long-term effects of an indicated school- and home-based suicide prevention program for adolescents. By relying on data on adolescents and young adults from a randomized control intervention study, this paper offers an analysis of postintervention suicide-risk trajectories and, therefore, assesses the maintenance of long-term behavioral change.
Risk and Protective Factors for Suicide
Research has shown that there are identifiable behavioral characteristics that are key to both accessing and assessing suicide risk. These suicide-risk factors provide an early signal of risk as well as an avenue for preventive interventions designed to reduce risk. In addition, these discernible characteristics are an important alternative means of tracking risk when one is dealing with low-base rate behaviors such as suicide attempts and deaths. Identified behavioral risk factors for adolescent suicide include not only direct suicide behaviors such as thoughts or attempts but also depression, anger, anxiety, and substance use.9–11 In addition, school problems, as well as family distress and lack of support, may increase risk.2,12–14 Overall, risk factors for suicide are likely to co-occur and mutually exacerbate their influence on youth behaviors.9,15 Anger and depression in particular are linked to known causes or precursors of adolescent suicidal behavior such as impulsivity, conflicts with parents or peers, and hopelessness related to poor coping skills and lack of a longer-term future-orientation.9,16,17
The Transition to Young Adulthood
Many of the identified adolescent risk factors, particularly direct suicide risk behaviors, depression, and anger/aggression, have shown a tendency to persist beyond adolescence and into adulthood.4,15,18–21 The research on emerging adulthood indicates that the period from adolescence to young adulthood entails significant challenges to well-being, involving more transitions, often with less support, than any other life period.22,23 While the introduction of the new roles, responsibilities, and contexts can pose considerable adjustment difficulty for many young adults, initial risk in adolescence may exacerbate the effects of young adult stress and set the stage for poor adaptation (ie, increased or continued distress). Thus, higher suicide rates in young adulthood result from a combination of continued risks and new risks.
Suicide-vulnerable adolescents are at risk of carrying earlier difficulties forward, for both externalizing and internalizing problems, and in both clinical and nonclinical samples.4,18–21,24,25 Research reveals that a history of adolescent emotional distress can have broad effects on a young adult’s current adaptation (such as social life and day-to-day function), when compared to other young adults who appear to have similar levels of emotional distress but less problematic histories.18,19 Youth at risk for suicide presumably carry vulnerability forward within a constellation of risk behaviors as past direct suicide behavior appears to be one of many factors that influence later suicidal behavior.9,15,16,26 Within those constellations, risk factors may interact to increase risk (such as depression and anger with suicide ideation) or to predispose one to mal-adaptive coping responses to subsequent stress and life difficulties.15,27 Over time, suicidal behaviors may become less related to the present external stressors and more likely to be spontaneously activated as coping responses to stress in general.26,28–30 The co-occurrence of adolescent risk factors, the underlying stresses and restructuring of lives associated with emerging adulthood, and the links between the 2 periods point to a need to understand the longitudinal patterns of suicide risk through this time period and assess the value of early prevention efforts on long-term behavior change.
The Promoting CARE Study
Central to this paper is the extent to which positive behavior change, in this case postintervention reduced suicide-risk behaviors, is maintained from youth to young adulthood and whether some individuals appear to maintain or achieve positive behavior change more successfully than others do. The basis for the long-term follow-up study is the Promoting CARE indicated suicide prevention program that explicitly targeted suicide-vulnerable high school youth, and provided a school- and home-based program to enhance important personal and social resources. To our knowledge, Promoting CARE is the only systematically evaluated comprehensive suicide prevention program delivered to youth who were assessed initially as at risk of suicide. The program integrates principles of behavior change maintenance, in particular using elements to enhance skills acquisition, social support, motivation, and self-efficacy.31–38 Promoting CARE’s content and procedures are based upon prevention science theory and empirical findings showing that interventions that attend to and increase motivation to change, social support access, and self-efficacy (ie, the confidence that one can effectively meet life challenges and access learned skills) increase the likelihood that skills will be learned, behavior will change, and change will be maintained.32,35,38,39 Skills acquisition and accessibility, in particular skills related to stress management, emotion control, and social support, are integral to the successful maintenance of a positive developmental course postintervention.32,33 Long-term change will depend on how well skills acquired during adolescence carry over to meet the challenges of young adulthood. This paper analyzes longitudinal data from this comprehensive prevention program that was presented to 615 high school youth and their parents, depicting the postintervention risk trajectories and focusing on the long-term maintenance of achieved short-term changes.
The Original Intervention Design
The Promoting CARE program was delivered successfully to over 600 suicide-vulnerable high school youth and their families in the Pacific Northwest. It addressed youth suicide risk by intervening to improve youth skills in managing emotion and coping with stress, as well as to increase success in support-seeking and receiving. By increasing personal and social resource skills we aimed to reduce negative behaviors such as suicide risk and depression. Of 615 youth, (a) 155 were assigned to a brief parent intervention (Parents CARE, P-CARE); (b) 153, to a brief youth intervention (Counselors CARE, C-CARE); (c) 164, to a combination of both youth and parent (P&C-CARE); and (d) 143, to a minimal-intervention comparison group (MI) that by necessity and institutional review board (IRB) protocol contains help elements and resource contact in forms similar to C-CARE but with less specificity and dose. (Specific details of the Promoting CARE prevention program are available from the authors.)
The central aim of the high school intervention was to evaluate the efficacy of the 3 brief suicide prevention protocols—in particular, the combined P&C-CARE compared to each component alone and each intervention group compared to the minimal-intervention comparison group — at reducing suicide-risk behaviors and the related risk factors of depression and anger. The expectation was that the combined P&C-CARE intervention would result in more marked and pervasive changes in outcomes than the other interventions would and that the 3 intervention components would be more effective than the minimal-intervention.
METHODS
Participants
Original participants
Participants were in grades 9–12 in one of 20 high schools representing 8 Pacific Northwest urban and suburban school districts. Over 2000 youth were screened to identify 615 youth who were at risk for suicide; a 25–30% case identification is consistent with the prevalence of such behaviors cited in the literature. The mean age of youth was 15.9 and 61% were female and 67% white.
Original procedures
All procedures for original and long-term follow-up studies were IRB approved. Teens in each of the high schools were recruited to a survey and possible selection into a brief intervention study. Oral and written informed assent was obtained from students, and oral and written informed consent was obtained from at least one parent/guardian via approved human subjects protocol. Participating students completed a comprehensive survey, the High School Questionnaire: Profile of Experiences (HSQ),40 which tapped key study variables and included a screen for suicide risk. Indicators included suicidal behaviors (thoughts, threats, attempts), depression, and drug involvement. Tests of the suicide-risk screen (SRS), embedded in the HSQ, document the reliability as well as the construct and predictive validity of this case-finding model.41,42 Youths identified as not currently at risk for suicide exited the study at this point.
Teens screening in as at risk were randomly assigned to participate in either the CARE or the MI (minimal intervention) protocols. Teens assigned to C-CARE completed a 1.5- to 2-hour assessment interview followed by a brief counseling protocol and the facilitation of social connections with parents and school personnel (1.5.–2 hour). A booster consisting of the C-CARE follow-up interview, a brief counseling protocol and a repeat of the social connection, was completed at 2.5 months post baseline. Teens assigned to MI participated in a brief (15- to 30-minute) assessment interview using the 22-item Screen for Youth Suicide Risk (SYSR), followed by a risk feedback and mobilization of support resources at home and at school. This comparison condition is designed to simulate usual intervention that would be provided by school personnel once a student is identified as being at potential suicide risk.
Upon completion of the teen protocol (either C-CARE or MI), parents assigned to the P-CARE intervention completed two 2-hour home visits designed to engage parents in a partnership in which parents learn suicide prevention “first aid” and are coached in the delivery of skills training and targeted support to their teen. A parent booster session (follow-up telephone call to parent) in which the teen’s suicide-risk status is reviewed and specific support strategies are reinforced was initiated 2.5 months post baseline. In the intervention study, 87% of youth were retained over the first 5 assessments. Completion was not significantly related to condition in the study.
Current long-term follow-up procedures
All Promoting CARE participants who did not specifically withdraw from participation in the originally funded evaluation were considered eligible (N=530) to participate in the young adult follow-up study, which involved one-hour assessment interviews administered by telephone. As part of the long-term follow-up study, there were one or 2 study contacts attempted during young adulthood (some had completed the first long-term follow-up questionnaire in the original study). Time from baseline, from 2.5 to 8 years, was tracked for all follow-up interviews and incorporated in the analysis.
Long-term retention of the participants was acceptable. Eighty-six percent (86%) of youth (530) of the original 615 participants were eligible for invitation to the long-term young adult follow-up study; 14% had left the original study prior to the start of the long-term follow-up. All requests to discontinue were regarding continued contact, and none refused use of previously collected data. Every effort was made to locate and invite these former 530 participants to the young adult study. Four hundred participated in a young adult telephone interview, and an additional 48 had completed a young adult follow-up in the original study. There were no baseline differences on outcome measures or across basic demographic variables between those who did and did not participate as young adults. Some differences arise in that youth who had more school moves during adolescence and those who resided in nonparental households (ie, with nonparent custodians such as grandparents or family friends) were less likely to be found and re-interviewed.
Measures
Measures of the study variables came from the High School Questionnaire (HSQ), administered in-person at the high schools, and the Young Adult Questionnaire, administered by telephone during young adulthood. The High School Questionnaire: Profile of Experiences40 measured suicide-risk behaviors and related-risk and protective factors. All measures were derived from standard measures or constructed specifically for the Reconnecting Youth (RY) Prevention Research Program. The Young Adult Questionnaire is a direct extension of the High School Questionnaire with items changed/added for the broader social context and events common in young adulthood (eg, employment, marriage). Key dimensions measured in the Young Adult Questionnaire are essentially identical to the High School Questionnaire scales. Analyses in prior work have shown the scales to have good reliability, construct, and predictive validity across multiple independent samples.38,40–45 Table 1 depicts the mean and standard deviations across the key outcome and other variables at baseline; appropriate reliability coefficients for the current sample are reported below.
Table 1.
Descriptives of Key Variables
| Baseline Variable/Scalea | Mean | Std. Dev. |
|---|---|---|
| Outcomes (N=615) | ||
| Suicide risk behaviors | 0.88 | 0.94 |
| Depression | 3.13 | 1.19 |
| Anger | 2.66 | 1.37 |
| Demographics | ||
| Sex(female=1) | .60 | .48 |
| Age at initial contact | 15.95 | 1.08 |
| Race (white=1) | .67 | .47 |
| Parents of origin | .43 | .49 |
| Stepparent | .23 | .42 |
| Single parent | .24 | .43 |
| Nonparent household (ref) | .10 | .29 |
| Personal/Social Resources | ||
| Self-efficacy | 3.23 | 1.20 |
| Family/parent support | 2.47 | 1.51 |
| Additional (antecedent) Risks | ||
| Elevated suicide risk (1=elevated) | .56 | .49 |
| Alcohol use (in past 30 days) | 1.86 | 2.33 |
| Other drug use (in past 30 days) | .81 | 2.10 |
| School problems | 2.77 | 1.01 |
Notes.
All outcomes, Self-efficacy, Family/parent support are measured on a 0 to 6 Likert scale.
Alcohol use and Other drug use are sums of items scaled from 0 to 6 (no use to daily) across types of substances.
School problems is based on a 0 to 6 scale.
Study Variables
Outcome measures in the analysis were direct suicide-risk behaviors and 2 distress factors: depression and anger. Direct suicide-risk behaviors were measured using 7 indicators (based on 0–6 point Likert scales indicating frequency) that included suicidal thoughts, notes, threats, and attempts (α=.89).46 The depression scale is derived from the CES-D47 using 6 items (α=.88), eg, “I feel depressed” and “I feel lonely.” Anger control problems,48 a 4-item scale (α=.77), measured “feeling out of control when angry” and “irritability or getting easily angered.” In young adulthood, identical measures were available for suicide-risk behaviors, depression and anger (α=.74, .88, and .77 respectively).
We included key demographic variables for the adolescent at baseline. Sex (60% female), age at baseline (nearly 16 years), race (white vs nonwhite) and household parent structure were input into the models as controls. The household-parent variables compare specific structures that contain at least one biological parent to nonparent households (10% of cases) such as living with other relatives or friends.
Protective factors measured at baseline were sense of self-efficacy/coping and family support. Self-efficacy, described as coping with problems and influencing positive outcomes (eg, “ability to make good things happen” or “ability to learn to adjust/cope with problems”), was measured by a 5-item 0–6 scale (α=.76).49 Family support,50 a 5-item measure of support satisfaction (α=.90), reflected the degree of satisfaction with family (eg, satisfied with how “share problems,” “can talk to,” and “time spent together”).
We included as additional controls risk factors capturing baseline characteristics of the youth. Elevated suicide risk comes from the overall suicide-risk screen and is operationalized as a dummy variable that indicates an individual had greater than 1 prior self-reported suicide attempts and/or an elevated depression score of 4 or greater on the maximum 6 scale. Alcohol use frequency is a continuous measure of use “in the last 30 days” based upon both reported beer/wine and hard liquor consumption.51 Other illicit drug use is also a continuous measure of the frequency of illicit drug use summed over 7 substances (cocaine, opiates, depressants, tranquilizers, hallucinogens, inhalants, stimulants). The variable school problems is a sum of 3 items on a 0–6 scale capturing self-report of performance, absenteeism, and likelihood of dropping out of high school.
Analysis Plan
We used latent class growth models (LCGM) to determine patterns of change from Time 2 (postintervention) to long-term follow-up52–55 for depression, anger, and suicide-risk behaviors. We focused on this period to explore the long-term maintenance of the initial declines due to intervention; all youth received some level of intervention that has been shown to reduce distress significantly from baseline. Furthermore, the CARE youth interventions and similar work by our research team have demonstrated significant short-term decreases relative to a minimal intervention control.56,57 Once distinctive postintervention patterns are discerned, we relate initial baseline characteristics of the youth to class/group membership in the patterns of long-term change. For the longitudinal analysis we use all individuals who remained in the study at the second interview and contributed at least one more additional assessment (N=593). Overall we fitted a model in which the outcome Y is a quadratic function of time (yit = b0 (c) + b1(c) T + b2(c) T2), where i represents individuals and t captures time; the equation has different sets of parameters for each underlying class, represented by the superscript c; we use Mplus 5.3 to estimate the models.54 We then modeled the class membership of individuals as a multinomial logistic regression (STATA 10.0) in order to explore what predicts the most probable class to which an individual belongs.
The nature of the follow-up study introduces 2 problems. First, individuals were at different distances away from baseline at their young adult assessments. We handled this by capturing 4 separate periods/distances from baseline for the 2 young adult assessments such that some individuals have a sixth and seventh assessment whereas others have a seventh and eighth, though in both cases, only 2 assessments were given. This allows a continuous-like time formulation and allows estimates of the trajectories that account for the differences in the length of time from baseline to the young adult follow-up measures. The second problem involves missing data at any time point over the entire period. We considered the data to be missing at random for the analyses and we incorporated the missing data by using a maximum likelihood approach in our estimation, which takes advantage of all information present in fitting the underlying model.58,59 This is a reasonable assumption given that there were not strong differences on baseline measures for those observed over time versus those missing in the long-term follow-up. Also, we used a selection model approach 59,60 to assess nonrandom selection into follow-up; we specified the growth models and included a variable capturing the likelihood of being in the follow-up and showed no difference in the underlying classes found.
Prior to fitting the various models, we explored the univariate distributions for outliers and distribution of the data. In general there were no extreme outliers for any of the 3 outcome variables over the period of study, but in all variables there is some skew to the data and is more pronounced, as would be expected, for the suicide-risk-behaviors indicator compared to either depression or anger. The LCGM is based on an underlying assumption of conditional multivariate normality, and some simulation work has shown that under distributional violations, classes may emerge that are simply related to the nonnormal structure rather than had substantive meaning.61 To insure the stability of our results, we also ran analyses using transformed data (both a square root and natural log transformation) to attempt to reduce the skew in the variables and conform more to the underlying distributional assumptions. In general, results with the transformed data are consistent in terms of number of classes and patterns of trajectories, and the general results of the intervention conditions and key variables were consistent with what is reported below.
Fit of the LCGM models was evaluated for all outcomes based on BIC and the Lo-Mendell-Rubin LRT; we also evaluated the accuracy or overlap of the estimated classes using an entropy measure and posterior probabilities of being in a given class. In addition, we also evaluated the general value or interpretability of the estimated class structure. For the 3 outcomes all models suggested that a 3 class growth model was the preferred; the quadratic models in general fit better than simple linear models.53,62
RESULTS
Before we report on the maintenance of behavior change effects from the Promoting CARE study, we present an overview of the short-term behavior change from baseline to immediately postintervention, for the study. Promoting CARE was effective at reducing risk and increasing protective factors for suicide. All study options showed immediate and significant results in reducing suicide ideation and threats, depression, hopelessness, anxiety, and anger. The protective factors of coping, self-efficacy, and family support also increased. Additionally, these significant differences were sustained through follow-up at 9 months (7 months postintervention) for all groups. While all intervention approaches were beneficial, in general, the intensive P&C-CARE component showed greater reductions in negative behavior and greater improvement in positive factors than did the other components. P-CARE on its own was often not significantly different from the MI comparison.
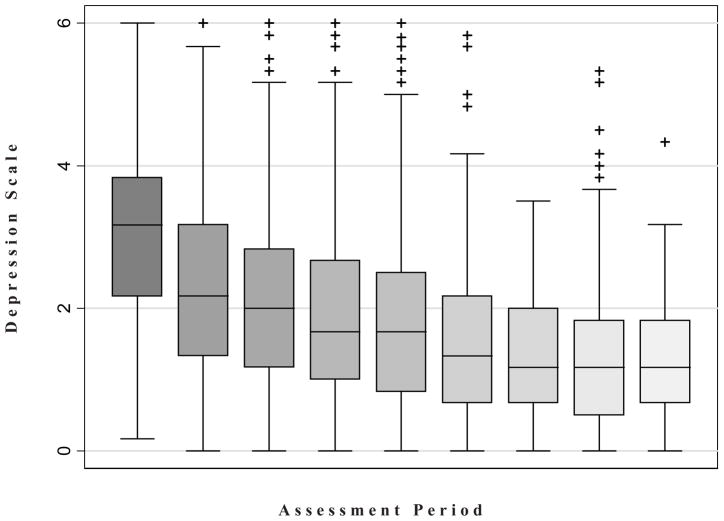
Next we turn to our main focus on long-term patterns and trajectories from postintervention in adolescence into young adulthood and the question of whether initial decline in risk behaviors was maintained into young adulthood. The first stage of the analyses determined similar patterns of change from postintervention to long-term follow-up (approximately 6 years post baseline) for the 3 risk behaviors, depression, anger, and suicide behaviors. This pattern also held for measures of hopelessness and anxiety as well as disaggregated suicide behaviors such as suicide ideation (not shown). Figure 1, showing box-plots of depressed affect over the period of study, is illustrative of the general pattern of change observed across time. From baseline to immediate postintervention there was a drop, and from Time 2 forward, there continued to be a decline at a decreasing rate. Although this demonstrates the general aggregate pattern, it is possible to have heterogeneous patterns within the data. Here the value of applying the latent class growth models is evident as it allowed us to explore whether there are distinctive subsets of individuals following a different growth regime within the data.
Figure 1.
Plot of Depressed Affect Scale Over Assessments
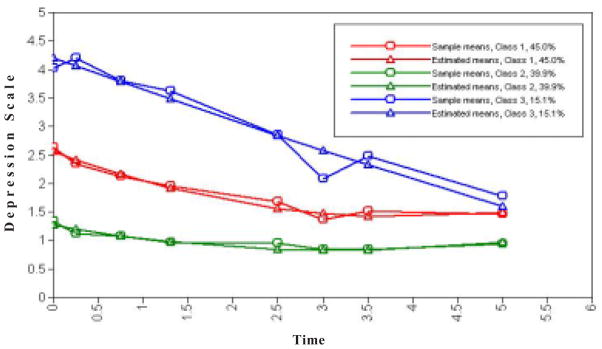
Figure 2 shows the estimated and actual means for depressed affect. As indicated, the patterns that emerged were (a) low-risk maintenance group (40% of cases), (b) a moderate-risk early-reducing group (45%), and (c) a higher-risk, continued-declining group (15%).
Figure 2.
Estimated and Actual Means for the 3 Latent Class Trajectories of Depression
Resulting trajectories described patterns of change over a 5- to 6-year period, from average age of 16 in high school to an average young adult age of 21. Across all outcomes the patterns, including the suicide behavior scale and anger, there were 3 distinct common patterns or classes of decline. Table 2 shows the resulting equations for each class of the 3 key outcomes presented and the percentage membership in each class. The intercepts for each equation capture the level of the outcome for each class at the immediate postassessment whereas the coefficients for time capture the decline (generally at a decreasing rate of decline given the squared term is positive). The equations show that for Class 3 the intercept, or postintervention starting point, was higher relative to the other 2 classes; and for all classes the slopes indicating initial decline differed significantly from zero. None of the equations indicated a sizeable upswing or relapse in the general pattern of long-term change.
Table 2.
Class Trajectory Equations (s.e.) and Class Allocation
| Outcome | Class 1 (low) | Class 2 (moderate) | Class 3 (high) |
|---|---|---|---|
| Depression | 1.26 (.08) + −.275(T) (.06) + .043 (T2) (.01) 40% N=236 |
2.55 (.09) + −.585(T) (.08) + .074 (T2) (.02) 45% N=268 |
4.20 (.13) + −.572(T) (.16) + .010 (T2) (.04) 15% N=89 |
| Anger | 1.21 (.07) + −.208(T) (.05) + .021 (T2) (.01) 44% N=258 |
2.47 (.11) + −.446(T) (.08) + .057 (T2) (.02) 40% N=268 |
4.18 (.14) + −.663(T) (.22) + .031 (T2) (.04) 16% N=89 |
| Suicide Risk Behaviors | .19 (.01) + −.063(T) (.02) + .009 (T2) (.004) 85% N=504 |
1.22 (.06) + −.500(T) (.07) + .059 (T2) (.02) 13% N=77 |
2.93 (.22) + −1.508(T) (.27) + .200 (T2) (.06) 2% N=12 |
The next stage of the analysis related key baseline predictors to membership in the classes distinguished above. We used a multinomial logistic regression and compared the moderate and high categories to the low-risk maintenance group; given the small sample size in the high declining direct suicide-risk category (Class 3) the analysis for direct suicide-risk behaviors collapsed classes 2 and 3 and compared them to the low-risk maintenance group.
Key predictors include the Promoting CARE intervention group assignment, basic demographic variables, personal/family resources, and individual antecedent risk factors (Table 3). The results of modeling showed a reasonably consistent pattern of effects for the program intervention. Across nearly all outcomes, the interventions showed a consistent negative relation to being in the higher patterns relative to the low group net of the covariates. Both C-CARE and P&C-CARE showed greater, and usually significant, effects related to trajectory membership, with the combination of C-CARE and P-CARE (ie, P&C-CARE) tending to greater effects. For example, the effects relative to MI for C-CARE and P&C-CARE for depression were, respectively, −.609 and −.784 (log odds) for comparing the moderate to low group, and −1.161 and −1.072 for comparing the high- to the low-risk group. These are significant effects whereas P-CARE shows no difference from MI. In almost all cases, P-CARE administered alone showed the weakest (nonsignificant difference) compared to the minimal intervention control; this suggests that the parental intervention on its own is relatively weak compared to the more direct and extensive intervention with the youth, and this difference is even more apparent when youth intervention is combined with parent. Overall, in our earlier short-term evaluation results, C-CARE combined with the P-CARE parent intervention showed the greatest and most persistent immediate effects across risk behaviors, compared to MI, from the intervention (Time 1 to Time 2), and it continued to predict membership in the more salubrious trajectory that includes young adulthood.
Table 3.
Multinomial Logit Model of Predictors on Membership in Trajectoriesa
| Baseline Predictorb | Depression low vs moderate | Depression low vs high | Anger low vs moderate | Anger low vs high | Suicide Risk low vs moderate/high |
|---|---|---|---|---|---|
| Program | |||||
| C-CARE | −.609* | −1.161*** | −.119 | −.033 | −.342 |
| P-CARE | .028 | − .650 | −.280 | −.775* | −.445 |
| PC-CARE | −.784** | −1.072*** | −.901** | −.799* | −.679^ |
| Demographics | |||||
| Gender(Female) | .250 | −.086 | .196 | −.142 | .454^ |
| Age | .207* | .071 | .083 | −.105 | .044 |
| Ethnic(White) | −.022 | .098 | −.479* | −.574* | .131 |
| Parents of origin | .158 | −.409 | −.442 | −1.042* | −.324 |
| Stepparents | .531 | .079 | .334 | .203 | −.068 |
| Single parent | .238 | −.167 | −.184 | −.162 | −.379 |
| Personal Resources | |||||
| Personal efficacy | −.412*** | −.784*** | − .199* | −.203^ | − .284** |
| Family support | −.053 | .029 | −.002 | −.194* | .011 |
| Risks | |||||
| Elevated suicide risk (baseline) | .851*** | 2.332*** | .379^ | .648* | 1.096*** |
| Alcohol use | .029 | .001 | .038 | .108^ | .009 |
| Hard drug use | .061 | .069 | .101^ | .145 * | .123* |
| School deviance | −.035 | .242^ | .106 | .261* | −.056 |
| Constant | −2.144 | −1.138 | − .687 | 1.606 | −2.085 |
| Model L2 | 159.93 (30df P<.001) | 91.76 (30df P<.001) | 41.89 (15df P<.001) | ||
Notes
P<.10;
P<.05;
P<.01;
P<.001
Given the number of youth in the high decline class for suicide risk behaviors (N=12) we collapse group 2 and 3 for this analysis.
Referent category was always membership in the low maintenance group
Across the demographic factors there appeared to be no strong consistent effects of any given variable except that, relative to nonwhites, white adolescents are likely to be in the lower class of anger. Being in a dual-parent biological family also lowers the odds of being in higher categories of anger. Regarding resources, initial perceived levels of self-efficacy were significantly related to suicide-risk behaviors, depression, and anger. Higher levels of self-efficacy placed the individual in the low maintenance group relative to either of the other 2 groups. Family support is related only to trajectories for anger and only for being in the highest versus lowest group (log odds coefficient = −.194). The same is true for school problems such as failure to attend or progress. The antecedent risk factor of elevated suicide behaviors at baseline tended to increase the odds of remaining in a higher-risk category over the postintervention period (ie, more likely to be in a relatively moderate-risk or in the higher-risk class) for the 3 outcomes. Using drugs other than alcohol and marijuana (ie, “hard drugs”) played a role in suicide behaviors but did not in depression or anger (at least not directly at the .05 level). Alcohol use did not play a substantial role across outcomes.
DISCUSSION
This study is a unique opportunity to consider the long-term course of suicide risk and suicide prevention outcomes. We examined outcomes of a successful and comprehensive community-based suicide prevention program targeting suicide-vulnerable high school youth and their families. Thorough risk-factor assessments were obtained across multiple time points in a longitudinal follow-up of a randomized control study. Finally, and importantly, we examined suicide risk across a challenging life transition, when rates for suicide in general are higher, for a vulnerable population.
The fact that all observed risk trajectories indicate a continued pattern of decreasing risk over the transition to young adulthood is an important testimony to the long-term effectiveness and maintenance of behavior resulting from the Promoting CARE preventive intervention and, more broadly, the general value of suicide-risk case identification coupled with short-term intervention. Reported young adult rates for suicide and suicide attempts and the stresses associated with the life course transition from adolescence to young adulthood create an expectation of increasing risk, or minimally continued risk, especially for those individuals evidencing such behaviors early in their life course.4,15,27,63 In spite of the new challenges in young adulthood, participants in this study who were showing signs of suicide risk in adolescence and who received an intervention did not show signs of relapse but continued their downward trend to a reduced level of risk.
Across the 3 behavior outcomes, we observed 3 distinct trajectories (2 are combined for suicide behaviors). The separate trajectories are distinguished from each other primarily by their level of the risk behavior at immediate postintervention (high, medium, and low) and, to a lesser extent, by the subsequent time taken to achieve the relatively low levels of risk behavior apparent for all by early adulthood. Those in the lower trajectories benefit from an earlier, and a longer, period of lowered risk. Importantly, even those who remained at slightly elevated risk postintervention continued to reduce their risk behaviors well after the intervention ended. Although some individuals may have experienced fluctuation in their distress, the trajectories show in general that declines in risk initially experienced after the intervention continued to occur over this period from adolescence to young adulthood without any significant indication of a relapse subgroup. This pattern of continued decline is noteworthy as it is not necessarily typical of the postintervention outcomes for either health behavior or behavior change interventions (eg, smoking cessation, weight loss, or lifestyle improvement). Intervention researchers often expect to see and address relapse after seeing initial declines in risk behaviors.
A number of factors intrinsic to the interventions and to the study design may help us understand the observed pattern of continued decrease or lack of relapse for all study participants. First of all, all youth were identified (via a case-finding screening process) as vulnerable from an indicated prevention perspective by using early signs of risk; all were intervened with; and, to some extent all were monitored in early follow-up assessments in adolescence. Thus the risk patterns we see are descriptive of a timely and successful short intervention strategy directed at early signs of risk; the effects appear strong and consistent across risk behaviors. The intervention conditions, while distinguishably different in generating immediate decline, are less distinctive in their long-term maintenance of the decline. Secondly, the theory and the posited change agents that underlie the more intensive intervention components, C-CARE and P-CARE, also guide the briefer minimal intervention approach: youth are presumed to benefit from a response that involves increasing their help seeking, support activation, and problem awareness. In other words, all study options offer intervention components guided by those principles, although options differ in the degree and variety of ways they seek to accomplish those goals. All the interventions included a check-in, problem acknowledgement, and linkage to home and school support resources. In addition, study participants were checked with if any follow-up assessments showed evidence of elevated distress, consistent with both human subjects protocol and study design. Hence, all participating study youth are provided with a booster on an intervention-as-necessary basis, with the intention of boosting their resources and awareness of their suicide risk during the initial adolescent intervention and follow-up.
In particular, youth help-seeking behavior and access to social support were targeted in all intervention options. Youth who experience thoughts of suicide, or depression, are known to be less likely to engage in help-seeking behaviors on their own.64,65 Increased help-seeking is directly addressed in the intervention by discussing suicide risk in a direct and supportive way, while investigating and selecting support resources and actively introducing youth to potential support persons. The selected support resource persons, both at home and at school, were coached by study staff to understand youth bids for support and to respond appropriately. In sum, it is likely that when young people learn to seek help when thoughts of suicide occur instead of acting on those thoughts, suicide risk is lowered. Moreover, their help-seeking willingness and skills are reinforced if their environment is “activated,” or prepared to respond appropriately; and once learned, the skill of support seeking may be carried forward to new contexts and periods.
A distinguishing feature and difference between the 3 trajectories for each outcome are their starting points, which are a function of short-term intervention outcomes. Key to differences is the extent to which youth enjoy a longer protective period of lowered risk; although all participants in general reduce risk, the higher- and moderate-risk pattern do not drop immediately, but drop gradually across the late adolescent period. The focus of this paper is long-term postintervention effects, but we must acknowledge that short-term effects for this intervention study play an important role. Although the current analysis does not support a strong statement regarding the significance of intervention components specific to long-term change maintenance, membership in the lower-risk groups, characterized by accelerated change and a longer period of low risk, is predicted by intervention condition. By virtue of initial decline, individuals in the C-CARE and P&C-CARE group experienced less depression and anger over the transition period from adolescence to young adulthood. It is primarily the intensive youth intervention, C-CARE, and its combination with P-CARE that were related to the earlier risk-reduction patterns for depression and anger; the parent condition alone, P-CARE, did not distinguish itself as different from MI. It is not surprising that, among the intervention options, the parent intervention on its own appears less related to early declines as a parent intervention is less likely to be a primary source of youth behavior change by mid-adolescence. However, in the long-term maintenance of change, the parent-only condition is not relevant, nor are the other conditions except to the extent MI and P-CARE, while experiencing a steady decline, are likely to experience a longer period of relatively higher risk compared to a lower-risk trajectory group (more likely to be CARE or P&C-CARE).
In addition to intervention conditions, individual features measured at baseline, both risk and protective, predict membership in a lower-risk trajectory group and do so for all of the 3 risk behavior outcomes. In particular, the predictors are initial presence of higher levels of self-efficacy and less severe level of suicide behaviors. These measured effects, for conditions and/or risk and protective factors, are over and above the effects of each other, including all entered demographic characteristics.
Self-efficacy is an important individual protective characteristic, promoting both commitment and confidence related to undertaking positive efforts. It is also, because of its critical role in maintaining and continuing positive change, a target of the C-CARE and P-CARE interventions.31,66 Self-efficacy affects both willingness to learn skills and willingness to use them. Skills acquisition enhances self-efficacy because adolescents feel more confident and capable of altering behavior as they acquire the necessary skills. Increased social support, another target of the study, also leads to greater self-efficacy,66 as well as being an important factor in long-term behavior change that aids the movement from one stage of change to another.67 Indeed, in this analysis, preintervention self-efficacy was a consistent predictor for all risk behavior outcomes. We see in this postintervention analysis that over and above the effects of intervention, initial self-efficacy reduces risk and maintains well-being – reiterating the importance of targeting this resource in behavior change intervention.
An important question in prevention research is whether individuals with particular antecedent risk behaviors or demographic features respond less positively to intervention, indicating their need for greater or different intervention to meet outcome goals. In this study, a consistent antecedent risk predictor, net of intervention condition and other factors, of the higher-risk trajectories for all 3 risk-behavior outcomes was the initial severity of an adolescent’s suicide involvement. Those who were experiencing more severe levels of suicidal involvement (attempts, numbers of suicide behaviors, higher depression) were less likely to be in the lower-risk trajectories. Nonetheless, while severity predicted a slower decline in risk, and a subsequent longer period of vulnerability, eventually their young adult risk was comparable to others.
We might ask why the initial drop in the 3 risk behaviors was less for those showing more severe suicidal involvement. One reason is that direct suicide-risk behaviors are known to be part of a cluster of co-occurring risks that not only impact initial risk status but also may complicate, and thus inhibit or slow the reduction of risk.9,12,16 In addition to the measures of risks controlled in the study analysis, we must acknowledge that difficulties in reducing risk might be maintained by other correlates of suicide risk such as childhood abuse, nonviolent adversity and emerging psychopathology that are not specifically controlled in the study. Maltreatment, abuse, and social disadvantage are consistent predictors of suicide risk, often but not always mediated by individual mental health, social difficulties, and subsequent stress exposures. Considered, from a life course perspective, they are part of a causal chain process where past events render one increasingly vulnerable to current stressors and likely to engage in suicide behavior.4,63,68,69 Furthermore, even if initially linked causally to antecedent risk factors, the suicide behaviors themselves may become entrenched, making them more difficult to change.29 Our short- and long-term findings suggest a tiered intervention approach might be helpful, where additional intensive and tailored intervention is offered to some individuals, informed by a comprehensive assessment of the related factors that make it more difficult for some to reduce suicide-risk behaviors.
On a similar note is the potential role of drug use when predicting the course of direct suicide behaviors. Those who report using hard drugs were also less likely to have achieved the low-risk trajectory postintervention for suicide behavior, indicating a need to attend to evidence of problematic substance use in suicide prevention. Those who report advanced drug use, in the sense of drug use progression,70 may require additional intervention or prevention focus to insure an initial postprogram decrease in use. Hard drug use, which is less normative in adolescence or adulthood, predicts greater, more distinct, and longer-term difficulties in adulthood (eg, economic marginalization, criminal involvement.)71,72 Overall, substance abuse can interact with anger and depression to increase emotional lability and the likelihood of experiencing more extreme emotional states, impulsivity, and disinhibition, making it more likely one would not only experience negative emotions that increase risk, but also that one would act on them.5,12,68,73
There was a surprising lack of effects related to demographic factors: family composition, age, sex, and race were for the most part noncontributors to better or worse long-term outcomes. Effects for the anger trajectories were an exception; anger was the only behavior for which there were relatively poorer outcomes for those who were nonwhite or not living with their natural parents. In addition, those who were initially experiencing more school problems and lower family support also showed greater likelihood of being in worse anger trajectories. It is interesting that by postintervention, the only risk-behavior connection to school and family problems was around anger, a reminder of the links between family conflict, school performance, and adolescent suicide behavior.2,12,16,74
Limitations
There are potential problems that may affect the results and our interpretation. First, missing assessments may be a source of bias in the analysis. We incorporated all available information in the longitudinal analysis when estimating the trajectories based on an assumption of missing at random. We believe this is reasonable given the lack of strong differences in those lost to follow-up and baseline information. In addition, our efforts to check the results by incorporating a selection mechanism showed no differences in the emerging patterns. Second, we have no control group to represent a “natural” course of risk development over this time period. Protocol requires some intervention upon discovery of suicide risk, and although we ideally would like to have a natural progression of risk, such a comparison group is not feasible. Given this, we cannot rule out completely that it is possible that all youth, simply left alone, would progress to lower levels of risk as identified in our trajectories. However, we point to the general patterns in the population that show increasing risk for this age-group and the fact we observe differentials related to the experimental conditions, to suggest the declines observed in this study are not simply a natural progression.
Summary
A detailed postintervention examination of a brief preventive intervention administered to suicide-vulnerable adolescents shows remarkably long-term results, with positive changes to suicide behavior, depression, and anger, sustained across the transition to young adulthood, a period typically defined as volatile and potentially difficult. Three trajectories for each of these risk behaviors were determined, all describing reductions in risk and maintenance of reduced risk across the period of follow-up. Even the higher-risk group does not abandon the positive direction of behavior change that began years before in a high school preventive intervention. Key antecedent risk and protective factors were identified that are implicated in the initial response to the interventions, in particular initial self-efficacy and the severity of suicide behavior involvement, and hence in long-term change. Also those who report using hard drugs were less likely to have achieved the low-risk trajectory postintervention for suicide behavior, over and above all other risks and conditions, indicating a need to attend to evidence of problematic substance use in suicide prevention. At the same time these baseline factors do not appear related to any pattern suggesting a failure to maintain initial or continued declines in distress. These additional risks may place an individual at slightly elevated risk for a longer period, but these factors are not halting the observed decline among youth exposed to some form of intervention. Results suggest that those who participated in the more intensive youth interventions, C-CARE and P&C-CARE, were most likely to achieve low-risk status early and maintain that status, but in the end all interventions lead to a common state of reduced risk in young adulthood. Study results also suggest that future prevention research might extend these findings for a brief intervention by examining a tailored approach to suicide intervention, including additional or more intensive intervention for those who evidence higher levels of distress or greater involvement in drug use.
Acknowledgments
This research was supported by NR 008823-01 and NR 04933-01 from the National Institute on Nursing Research. We are indebted to the Health Maintenance Consortium for supporting our work with young adults and to the young adults who, with their participation, enriched our understanding of this period. We are grateful for the support and collaboration of our research group colleagues.
References
- 1.Centers for Disease Control. Trends in the prevalence of suicide-related behaviors. [Accessed September 30, 2009];National YRBS 1991–2007 (on-line) Available at: https://www.cdc.gov/HealthYouth/yrbs07/USSuicideRelatedBehaviors.pdf.
- 2.Resnick MD, Bearman PS, Blum R, et al. Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA. 1997;278(10):823–832. doi: 10.1001/jama.278.10.823. [DOI] [PubMed] [Google Scholar]
- 3.Allison S, Pearce C, Martin G, et al. Parental influence, pessimism and adolescent suicidality. Arch Suicide Res. 1995;1(4):229–242. [Google Scholar]
- 4.Fergusson DM, Woodward LJ, Horwood LJ. Risk factors and life processes associated with the onset of suicidal behaviour during adolescence and early adulthood. Psychol Med. 2000;30(1):23–39. doi: 10.1017/s003329179900135x. [DOI] [PubMed] [Google Scholar]
- 5.Garrison CZ, McKeown RE, Valois RF, Vincent ML. Aggression, substance use, and suicidal behaviors in high school students. Am J Public Health. 1993;83(2):179–184. doi: 10.2105/ajph.83.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wichstrøm L. Predictors of adolescent suicide attempts: a nationally representative longitudinal study of Norwegian adolescents. J Am Acad Child Adolesc Psychiatry. 2000;39(5):603–610. doi: 10.1097/00004583-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 7.National Center for Injury Prevention and Control. [Accessed November 15, 2009];Web-based Injury Statistics Query and Reporting System (WISQARS) (on-line) Available at: http://cdc.gov/nicp/wisqars/
- 8.Gerhardt CA, Britto MT, Mills L, et al. Stability and predictors of health-related quality of life inner-city girls. J Dev Behar Pediatr. 2003;24(3):189–194. doi: 10.1097/00004703-200306000-00010. [DOI] [PubMed] [Google Scholar]
- 9.King RA, Schwab-Stone M, Flisher AJ, et al. Psychosocial and risk behavior correlates of youth suicide attempts and suicide ideation. J Am Acad Child Adolesc Psychiatry. 2001;40(7):837–846. doi: 10.1097/00004583-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Davis LL, Frazier E, Husain MM, et al. Substance use disorder comorbidity in major depressive disorder: a confirmatory analysis of the STAR*D cohort. Am J Addict. 2006;15(4):278–285. doi: 10.1080/10550490600754317. [DOI] [PubMed] [Google Scholar]
- 11.Chassin L, Pitts SC, DeLucia C. The relation of adolescent substance use to young adult autonomy, positive activity involvement, and perceived competence. Dev Psychopathol. 1999;11(4):915–932. doi: 10.1017/s0954579499002382. [DOI] [PubMed] [Google Scholar]
- 12.Kandel D, Raveis VH. Suicidal ideation in adolescence: depression, substance use and other risk factors. J Youth Adolesc. 1991;20(2):289–307. doi: 10.1007/BF01537613. [DOI] [PubMed] [Google Scholar]
- 13.Lewinsohn PM, Hops H, Roberts RE, et al. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM III-R disorders in high school students. J Abnorm Psychol. 1993;102(1):133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- 14.Resnick MD, Borowsky IW, Ireland M. Adolescent violence perpetration: what predicts? what protects? J Adolesc Health. 1999;24:128–142. doi: 10.1016/j.jadohealth.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 15.Lewinsohn PM, Rohde P, Seeley JR, Baldwin CL. Gender differences in suicide attempts from adolescence to young adulthood. J Am Acad Child Adolesc Psychiatry. 2001;40(4):427–434. doi: 10.1097/00004583-200104000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Walsh E. Dissertation. Seattle, WA: University of Washington; 1999. Suicide-risk Behaviors and Drug Involvement among Potential High School Dropouts. UMI No. 9944193. [Google Scholar]
- 17.Daniel SS, Goldston DB. Interventions for suicidal youth: a review of the literature and developmental considerations. Suicide Life Threat Behav. 2009;39(3):252–268. doi: 10.1521/suli.2009.39.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hofstra MB, Van Der Ende J, Verhulst FC. Adolescents’ self-reported problems as predictors of psychopathology in adulthood: a 10-year follow-up study. Br J Psychiatry. 2001;179:203–209. doi: 10.1192/bjp.179.3.203. [DOI] [PubMed] [Google Scholar]
- 19.Hofstra MB, Van Der Ende J, Verhulst FC. Pathways of self-reported problem behaviors from adolescence into adulthood. Am J Psychiatry. 2002;159(3):401–407. doi: 10.1176/appi.ajp.159.3.401. [DOI] [PubMed] [Google Scholar]
- 20.Achenbach TM, Howell CT, McConaughy SH, Stanger C. Six year predictors of problems in a national sample: III. Transitions to young adult syndromes. J Am Acad Child Adolesc Psychiatry. 1995;34(5):658–669. doi: 10.1097/00004583-199505000-00018. [DOI] [PubMed] [Google Scholar]
- 21.Achenbach TM, Howell CT, McConaughy SH, Stanger C. Six-year predictors of problems in a national sample: IV. Young adult signs of disturbance. J Am Acad Child Adolesc Psychiatry. 1998;37(7):718–727. doi: 10.1097/00004583-199807000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Schulenberg JE, Bryant AL, O’Malley PM. Taking hold of some kind of life: how developmental tasks relate to trajectories of well-being during the transition to adulthood. Dev Psychopathol. 2004;16(4):1119–1140. doi: 10.1017/s0954579404040167. [DOI] [PubMed] [Google Scholar]
- 23.Schulenberg JE, Maggs JL, O’Malley PM. How and why the understanding of developmental continuity and discontinuity is important. In: Mortimer JT, Shanahan MJ, editors. Handbook of the Life Course. NY: Plenum Press; 2003. pp. 413–436. [Google Scholar]
- 24.Harrington R, Fudge H, Rutter M, et al. Adult outcomes of childhood and adolescent depression: I. Psychiatric status. Arch Gen Psychiatry. 1990;27:465–473. doi: 10.1001/archpsyc.1990.01810170065010. [DOI] [PubMed] [Google Scholar]
- 25.Schulenberg JE, Zarrett NR. Mental health during emerging adulthood: Continuity and discontinuity in courses, causes, and functions. In: Arnett JJ, Tanner JL, editors. Emerging Adults in America: Coming of Age in the 21st Century. Washington, DC: APA; 2006. pp. 135–172. [Google Scholar]
- 26.Joiner TE, Fitzpatrick KK, Berlim MT, et al. Four studies on how past and current suicidality relate even when “everything but the kitchen sink” is covaried. J Abnorm Psychol. 2005;114(2):291–303. doi: 10.1037/0021-843X.114.2.291. [DOI] [PubMed] [Google Scholar]
- 27.Fergusson DM, Horwood LJ, Ridder EM, Beautrais A. Suicidal behaviour in adolescence and subsequent mental health outcomes in young adulthood. Psychol Med. 2005;35(7):983–993. doi: 10.1017/s0033291704004167. [DOI] [PubMed] [Google Scholar]
- 28.Beautrais AL. National strategies for the reduction and prevention of suicide. Crisis. 2005;26(1):1–3. doi: 10.1027/0227-5910.26.1.1. [DOI] [PubMed] [Google Scholar]
- 29.Joiner TE, Rudd MD. Intensity and duration of suicidal crises vary as a function of previous suicide attempts and negative life events. J Consult Clin Psychol. 2000;68(5):909–916. doi: 10.1037/0022-006X.68.5.909. [DOI] [PubMed] [Google Scholar]
- 30.Linehan MM. Behavioral treatments of suicidal behaviors: definitional obfuscation and treatment of outcomes. Ann NY Acad Sci. 1997;836:302–328. doi: 10.1111/j.1749-6632.1997.tb52367.x. [DOI] [PubMed] [Google Scholar]
- 31.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 32.Baer JS, Kivlanhan DR, Donovan DM. Integrating skills training and motivational therapies. J Subst Abuse Treat. 1999;17(1–2):15–23. doi: 10.1016/s0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- 33.Marlatt GA. Cognitive factors in the relapse process. In: Marlatt GA, Gordon JR, editors. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: Guilford; 1985. pp. 128–200. [Google Scholar]
- 34.Lin N, Dean A, Ensel W. Social Support, Life Events, and Depression. Orlando: Academic Press; 1986. [Google Scholar]
- 35.Prochaska JO, Redding CA, Evers KE. The transtheoretical model and stages of change. In: Glanz K, Lewis FM, Rimer BK, editors. Health Behavior and Health Education: Theory, Research and Practice. San Francisco: Jossey-Bass; 1997. [Google Scholar]
- 36.Goldstein AP, Martens BK. Lasting Change: Methods for Enhancing Generalization of Gain. Champaign, IL: Research Press; 2000. [Google Scholar]
- 37.Litt MD, Kleppinger A, Judge JO. Initiation and maintenance of exercise behavior in older women: predictors from the social learning model. J Beh Med. 2002;25(1):83–97. doi: 10.1023/a:1013593819121. [DOI] [PubMed] [Google Scholar]
- 38.Thompson EA, Eggert LL, Herting JR. Mediating effects of an indicated prevention program for reducing youth depression and suicide risk behaviors. Suicide Life Threat Behav. 2000;30(3):252–271. [PubMed] [Google Scholar]
- 39.Miller W, Rollnick S. Motivational Interviewing: Preparing People for Change. New York: Guilford Press; 2002. [Google Scholar]
- 40.Eggert LL, Herting JR, Thompson EA. The High School Questionnaire: Profile of Experiences. Seattle, WA: Reconnecting Youth Prevention Research Program, University of Washington School of Nursing; 1995. [Google Scholar]
- 41.Thompson EA, Eggert LL. Using the suicide risk screen to identify suicidal adolescents among potential high school dropouts. J Am Acad Child Adolesc Psychiatry. 1999;38(12):1506–1514. doi: 10.1097/00004583-199912000-00011. [DOI] [PubMed] [Google Scholar]
- 42.Eggert LL, Thompson EA, Herting JR. A measure of adolescent potential for suicide: development and preliminary findings. Suicide Life Threat Behav. 1994;24(4):359–381. [PubMed] [Google Scholar]
- 43.Thompson EA, Moody KA, Eggert LL. Discriminating suicide ideation among high-risk youth. J Sch Health. 1994;64(9):361–367. doi: 10.1111/j.1746-1561.1994.tb06205.x. [DOI] [PubMed] [Google Scholar]
- 44.Thompson EA, Horn M, Herting JR, Eggert LL. Enhancing outcomes in an indicated drug prevention program for high-risk youth. J Drug Educ. 1997;27(1):19–41. doi: 10.2190/G6XY-U2CQ-GFQF-PNEV. [DOI] [PubMed] [Google Scholar]
- 45.Thompson EA, Mazza JJ, Herting JR, Eggert LL. The mediating roles of anxiety, depression, and hopelessness on adolescent suicidal behaviors. Suicide Life Threat Behav. 2005;35(1):14–34. doi: 10.1521/suli.35.1.14.59266. [DOI] [PubMed] [Google Scholar]
- 46.Thompson EA, Eggert LL, Herting JR. Mediating effects of an indicated prevention program for reducing youth depression and suicide risk behavior. Suicide Life Threat Behav. 2000;30(3):252–271. [PubMed] [Google Scholar]
- 47.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. J Appl Psychol Meas. 1997;1(3):385–401. [Google Scholar]
- 48.Spielberger CD, Jacobs G, Russel S, Crane RS. Assessment of anger. In: Butcher JN, Spielberger CD, editors. Advances in Personality Measurement Assessment. Vol. 2. Hillsdale, NJ: Lawrence Erlbaum; 1983. pp. 159–187. [Google Scholar]
- 49.Coppel DB. Dissertation. Seattle, WA: University of Washington; 1981. The Relationship of Perceived Social Support and Self-Efficacy to Major and Minor Stress. [Google Scholar]
- 50.Smilkstein G, Ashworth C, Montano D. Validity and reliability of the family APGAR as a test of family function. J Fam Pract. 1982;15(2):303–311. [PubMed] [Google Scholar]
- 51.Eggert LL, Herting JR, Thompson EA. The drug involvement scale for adolescents (DISA) J Drug Educ. 1996;26(2):101–130. doi: 10.2190/EQ6J-D4GH-K4YD-XRJB. [DOI] [PubMed] [Google Scholar]
- 52.Singer JD, Willett JB. Applied Longitudinal Data Analysis. NY: Oxford University Press; 2003. [Google Scholar]
- 53.Jung T, Wickrama KAS. An introduction to latent class growth analysis and growth mixture modeling. Soc Personal Psychol Compass. 2008;2(1):302–317. [Google Scholar]
- 54.Muthen LK, Muthen BO. Mplus User’s Guide. Los Angeles: Muthen&Muthen; 2004. [Google Scholar]
- 55.Audrain-McGovern J, Rodriguez D, Tercyak KP, et al. Identifying and characterizing adolescent smoking trajectories. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2023–2034. [PubMed] [Google Scholar]
- 56.Randell BP, Eggert LL, Pike KC. Immediate post intervention effects of 2 brief youth suicide prevention interventions. Suicide Life Threat Behav. 2001;31(1):41–60. doi: 10.1521/suli.31.1.41.21308. [DOI] [PubMed] [Google Scholar]
- 57.Thompson EA, Eggert LL, Randell BP, Pike KC. Evaluation of indicated suicide risk prevention approaches for potential high school dropouts. Am J Pub Health. 2001;91(5):742–752. doi: 10.2105/ajph.91.5.742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Little RJA, Rubin DB. Statistical Analysis with Missing Data. New York: Wiley & Sons; 1987. [Google Scholar]
- 59.Allison P. Missing Data. Thousand Oaks, CA: Sage University Press; 2002. [Google Scholar]
- 60.Heckman JJ. The common structure of statistical models of truncated, sample selection and limited dependent variables, and a simple estimator of such models. Ann of Econ Soc Meas. 1976;5(4):475–492. [Google Scholar]
- 61.Bollen KA, Curan PJ. Latent Curve Models: A Structural Equation Perspective. Hoboken, NJ: Wiley; 2006. [Google Scholar]
- 62.Nulund KL, Asparouhov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carol simulation study. Struct Equ Model. 2007;14:535–569. [Google Scholar]
- 63.Fergusson DM, Beautrais AL, Horwood LL. Vulnerability and resiliency to suicidal behaviours in young people. Psychol Med. 2003;33(1):61–73. doi: 10.1017/s0033291702006748. [DOI] [PubMed] [Google Scholar]
- 64.Carlton P, Deane FP. Impact of attitudes and suicidal ideation on adolescents’ intentions to seek professional psychological help. J Adolesc. 2000;23(1):35–45. doi: 10.1006/jado.1999.0299. [DOI] [PubMed] [Google Scholar]
- 65.Garland AF, Zigler EF. Psychological correlates of help-seeking attitudes among children and adolescents. Am J Orthopsychiatry. 1994;64(4):586–593. doi: 10.1037/h0079573. [DOI] [PubMed] [Google Scholar]
- 66.McAuley E. Self-efficacy and the maintenance of exercise participation in older adults. J Behav Med. 1993;16(1):103–113. doi: 10.1007/BF00844757. [DOI] [PubMed] [Google Scholar]
- 67.Marcus BH, Rakowski W, Rossi JS. Assessing motivational readiness and decision making for exercise. Health Psychol. 1992;11:257–261. doi: 10.1037//0278-6133.11.4.257. [DOI] [PubMed] [Google Scholar]
- 68.Gould M, Greenberg T, Velting DM, et al. Youth suicide risk and preventive interventions: a review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42(4):386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 69.Johnson JG, Cohen P, Gould MS, et al. Childhood adversities, interpersonal difficulties, and risk for suicide attempts during late adolescence and early adulthood. Arch Gen Psychiatry. 2002;59(8):741–749. doi: 10.1001/archpsyc.59.8.741. [DOI] [PubMed] [Google Scholar]
- 70.Kandel D, Yamaguchi K. From beer to crack: developmental patterns of drug involvement. Am J Pub Health. 1993;83(6):861–855. doi: 10.2105/ajph.83.6.851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Newcomb MD, Bentler PM. Consequences of Adolescent Drug Use: Impact on the Lives of Young Adults. Newbury Park, CA: Sage; 1988. [Google Scholar]
- 72.Bogart LL, Collins RL, Ellickson PL, et al. Are adolescent substance users less satisfied with life as young adults and if so, why? Soc Indic Res. 2007;81(1):149–169. [Google Scholar]
- 73.Kandel DB. Substance use, depressive mood, and suicidal ideation in adolescence and young adulthood. In: Stiffman AR, Feldman FA, editors. Advancement in Adolescent Mental Health. Greenwich, CT: JAI Press; 1988. pp. 127–152. [Google Scholar]
- 74.Kidd S, Henrich CC, Brookmeyer KA, et al. The social context of adolescent suicide attempts: interactive effects of parent, peer, and school social relations. Suicide Life Threat Behav. 2006;36(4):386–395. doi: 10.1521/suli.2006.36.4.386. [DOI] [PubMed] [Google Scholar]