Abstract
This paper assesses how the relationship between health and educational attainment has changed over the last three decades. We examine trends in disease prevalence and self-reporte health using the US National Health Interview Survey for five chronic conditions—arthritis, diabetes, heart disease, hypertension, and lung diseases. The sample is limited to non-Hispanic Whites ages 40–64 to focus on the value of education and not changing representation of minority populations.
We find that health benefits associated with additional schooling rose over time by more than ten percentage points as measured by self-reported health status. This can be attributed to both a growing disparity by education in the probability of having major chronic diseases during middle age, and better health outcomes for those with each disease.
The value of education in achieving better health has increased over the last 25 years; both in protecting against onset of disease and promoting better health outcomes amongst those with a disease. Besides better access to health insurance, the more educated increasingly adapted better health behaviors, particularly not smoking and engaging in vigorous excercise, and reaped the benefits of improving medical technology. Rising health disparities by education are an important social concern which may require targeted interventions.
Keywords: health, education, USA, non-hispanic whites
INTRODUCTION
That richer and better-educated people are healthier is a robust empirical finding in health. Socioeconomic status affects mortality and morbidity in many studies (Marmot, 2000) and—particularly for education—the relationship is quantitatively large (Marmot, 2000; Case, Lubotsky, & Paxson, 2002; Currie & Stabile; Smith, 1999; Pappas, Queen, Hadden, & Fisher, 1993; Preston & Taubman, 1994). Less clear is how this relationship changed over the last three decades as health care has advanced and education levels have risen.
The benefits of more education are rising in other social contexts. The economic returns to education have increased sharply, with rapidly growing income benefits associated with more schooling—particularly college Murphy & Welch, 1992; Card and DiNardo, 2002; Acemoglu, 2003; Lemieux, 2008). It would be unsurprising if there were a parallel trend in other social contexts, with health a prime candidate. Over the last half century, there were enormous improvements in health outcomes (Murphy & Topel, 2006) with the source of many improvements complementary with human skills, partly embodied in education. The introduction of new and highly effective drugs in combating and managing disease is a good example. These drugs require individual action in adoption and effective use, a trait strongly associated with schooling (Goldman & Smith, 2002).
This research documents that health benefits associated with schooling in the USA have expanded sharply. One component rests in growing disparities by education in probabilities of having major chronic diseases during middle age. We also find that rising values of education to better health takes place within major disease group, suggesting that part of rising values of schooling rests partly in improved disease management.
METHODS
We use the US National Health Interview Surveys (NHIS) to document changes in disease prevalence, self-reported health, and availability of health insurance. NHIS is a continuing nationwide in-person survey of approximately 40,000 households, or about 100,000 persons, in the civilian non-institutionalized population (Centers for Disease Control and Prevention, 2008). To focus on our central thesis of changing education value to health, our samples are limited to non-Hispanic whites ages 40–64. The two main minority groups in the U.S.—Latinos and African-Americans—are proportionally more numerous within lower education classes and, at least for Latinos, their relative representation increased significantly over time. We supplement this analysis with samples of African-Americans. Moreover, there are special health issues unique to both populations (Jasso, Massey, Rosenzweig, & Smith, 2004; Kington & Smith, 1997; Palloni & Arias, 2004) that have little to do with our central issue. Restricting samples to the US born is not possible since NHIS contains country of birth indicators beginning in 1989.
Since disease prevalence rises with age, an age group was selected with sufficient sample size neither too young (predating onset of many diseases) or too old (when disease prevalence becomes too widespread and selective mortality confounds the relationship). Education is separated into four groups that can be consistently defined over time in NHIS—0–11, 12, 13–15, and 16 or more years of schooling.
To track changes in behavioral risk factors, NHIS is supplemented by data for the same demographic sub-population from three waves of the National Health and Nutrition Examination Survey: NHANES II (1976–1980), NHANES III (1988–1994), and NHANES IV (1999–2002). While NHIS has the advantage of yearly and consistent measurement of key health outcomes over time, NHANES has the advantage of measuring health behavioral risk factors consistently over time which NHIS does not.
Measures
Disease Prevalence
NHIS changes definitions of diseases periodically, becoming at times more or less expansive with periodic survey redesigns that could impact the changing portrait of American health (Centers for Disease Control and Prevention, 2000; Martin, Schoeni, Freedman, & Andreski, 2007). After reviewing NHIS question wording and prevalence data, we chose five common diseases for study that are very comparably defined over time: arthritis, diabetes, heart disease, hypertension, and diseases of the lung.
We focus on 1978 onward because life-time disease prevalence was not asked each year prior to 1978 (1980 for diabetes), and because health conditions prior to that date were only probed as a reason for physician visits or hospitalizations and the questions typically limit prevalence to having the condition in the last year. In addition, as explained below specific changes in question wording limited the samples to 1978 to 1996 for arthritis and lung disease.
The other major change was between 1986 and 1996 when the NHIS began asking about many health conditions, but these were sub-divided into six condition lists only one of which was given to each respondent. While the condition list by itself does not bias prevalence estimates, it affects precision of the estimates especially within education and disease cells due to smaller samples. While co-morbidity across the full set of diseases cannot be ascertained, that is not our objective.
An important revision after 1996 is that only self-reports about chronic conditions were permitted, with no proxy responses for other family members. Prior to 1996, one family member reported conditions for all members living in the home. Proxy reports for other family members are known to understate disease prevalence (Weir and Smith, 2007). Thus we limit data prior to 1997 to actual respondents only.
For diabetes, hypertension, and heart disease, the post-1996 conditions are based on prior life-time prevalence. (“Has a doctor ever told you…”) This is true pre-1997 for hypertension and heart disease, but not for diabetes which refers to the last year. However, diabetes is a serious disease for which there is no recovery so we do not expect and did not find any real break between pre-1997 and post-1996 data in diabetes prevalence. Pre-1997 prevalence for diseases of the lung and arthritis refer to the previous 12 months.
Besides these general changes affecting all diseases, there were some additional revisions impacting specific diseases. Arthritis is one example. Between 1997 and 2000, each adult was instead asked the symptom question “During the past 12 months, have you had pain, aching, stiffness, or swelling in or around a joint?” This question yields a much higher prevalence so that arthritis can only safely be described comparably for respondents themselves from 1978 to 1996.
Another disease specific change occurred with diseases of the lung. A major revision took place in 1997 and afterwards when individuals were only asked about prevalence of chronic bronchitis during last 12 months and emphysema over their lifetime. Before 1996, they were asked about a longer list of lung related conditions during previous 12 months. There was a sharp drop in prevalence of lung disease between 1996 and 1997 due to this definitional change so we only describe prevalence trends for diseases of the lung from 1978–1996.
Data on hypertension prevalence required one additional adjustment. Because of changes in survey design related to including hypertension embedded within a longer list of heart related problems before 1997 and as a single stand-alone question post-1996, overall hypertension prevalence increased approximately 50% between 1996 and 1997 (from 17.7% to 26.2%). To compensate for this design change, hypertension rates were adjusted between 1997 to 2005 by subtracting an adjustment factor. This constant was computed as 1997 fitted prevalence (using a second order fractional polynomial fitting data from 1997 to 2005) minus 1996 fitted prevalence (using second order fractional polynomial for 1978 to 1996). Adjusted data from 1997 to 2005 are then used to compute fitted models for hypertension over 1978 to 2005. Our findings are not sensitive to that adjustment.
Self-Reported Health
We measure health using self-reported general health status, which is highly predictive of subsequent mortality (Idler and Benyamini, 1997). Since 1982, NHIS used the traditional five point scale: “Would you say your health in general was excellent, very good, good, fair, or poor?” Before 1982, a four point scale of excellent, good, fair, poor was used instead and individuals were asked to compare themselves to others of the same age. Table 1 compares the responses in 1981 and 1982 for the sample used in our analysis. Clearly some respondents who would have said “Very Good” in 1981 allocated themselves to “Excellent” and some allocated themselves to “Good”. Therefore the top three categories are not comparable pre and post 1981. However, the fraction reporting themselves in either fair or poor health was 18.2% in 1981 and 17.1% in 1982 consistent with the gradual secular improvement in health over this period. For this reason, in our analysis heath status is categorized by fractions of respondents reporting themselves in fair or poor health, providing a more consistent treatment of time trends.
Table 1.
NHIS Distribution of Responses in Self-Reported Health in Percents for those 40–64 in 1981 and 1982
| 1981 | 1982 | |
|---|---|---|
| Excellent | 40.7% | 29.5% |
| Very Good | NA | 24.5% |
| Good | 40.7% | 28.4% |
| Fair | 12.9% | 11.4% |
| Poor | 5.3% | 5.7% |
Behavioral Risk Factors
Risk factors from NHANES include currently smoking, obesity (BMI ≥ 30), vigorous exercise, and height in inches. While height is more appropriately viewed as a health outcome than a health risk factor, height is often seen as an excellent summary measure of childhood health especially related to early life nutrition and other health risks in early childhood (Case, Lubotsky, and Paxson, (2002)). Measures of obesity and height are based on physical exams and are free of measurement errors associated with self-reports. The definition of vigorous exercise varies by wave. While these revisions create imprecision in changes over time, the same exercise questions were asked of all education groups in each wave and it is differentials by education that are our primary concern. To supplement this data, we obtained information on availability of any form of health insurance for the NHIS years 1980, 1989, and 2006 to match time periods in the three NHANES. NHANES does not consistently define health insurance over our time period.
Statistical Methods
After stratifying by age, disease and education, sample sizes even in large probability samples like NHIS become small, especially during the time period when NHIS presented separate disease lists to random samples of respondents (1986–1996). For prediction purposes, all level data predictions were based on non linear smoothed predictions using second order fractional polynomial regressions to visually identify non-linear trends with confidence intervals (Royston & Altman, 1997).
Fractional polynomial regression is similar to standard polynomial smoothing, but allows for negative powers and non-integer polynomials. Conventional polynomial smoothing is known to produce artifacts in the tails, especially with higher order polynomials. Our level models give a better fit than polynomials of the same degree and even those of higher degrees. The result is more flexible models with fewer statistical aberrations (waviness or ‘end-point effects’) in higher order fitted curves. It should be noted, however, that standard quadratic methods yield very similar results to those we report here. The raw data are also shown in each figure.
To obtain the best fit for differences between education groups for either disease prevalence or the fractions in poor or fair health, we estimated Ordinary Least Squares (OLS) best linear fit of the differences between education groups.
RESULTS
Overall Trends in General Health by Education
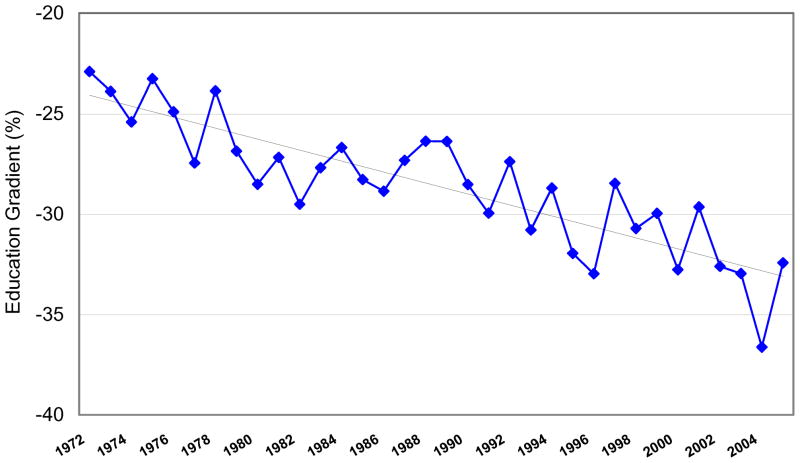
Given well documented large differences in health status by education, our central question is how these health disparities changed secularly. Based on fractions saying their health is either fair or poor, Figure 1 plots differences in these proportions between those with 16 or more years and those with 0–11 years of schooling. Very similar secular patterns exist if we used differences between other education groups.
Figure 1. Education gradient in percentage in fair or poor health, ages 40 to 64.
Note: Figure shows the difference between education groups in the percentage reporting fair or poor health. The difference is computed as the percentage reporting fair or poor health among those with 16 or more years of education less the percentage among those with less than 12 years of education. Over the entire period, the less educated report a higher percentage in fair or poor health, and the differences between the education groups are getting larger over time. The estimated linear coefficient on the solid line is −0.24 with a ‘t’ of 7.48 and a p value < 0.001.
As indicated by the solid line in Figure 1 representing the best linear fit of the data, health disparities by education have risen dramatically. In 1972 percents in fair or poor health among those not graduating from high school exceeded those of college graduates by 23 percentage points. This disparity grew until differences between these two education groups approached 36 percentage points. The estimated linear coefficient on the solid line is −0.24 with a ‘t’ of 7.48 and a p value < 0.001. Health disparities by schooling clearly have become much larger over the last 30 years—perhaps due to increasing differences in disease prevalence or increasing health differences amongst those with disease. We examine these issues below.
Trends in Disease Prevalence by Education
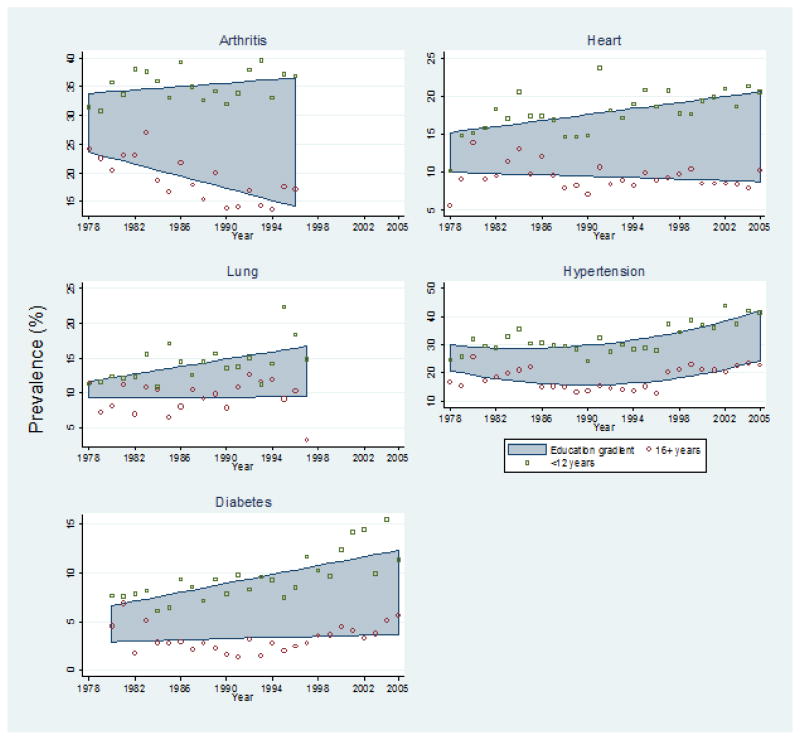
Of key interest is not just the overall trend in disease prevalence, but how it differentially impacted people with different education. Figure 2.A plots trends in predicted disease prevalence for the least and most educated group while the size of the shaded area between indicates differences in predicted prevalence between those with 0–11 years and 16+ years of schooling. For all five chronic conditions, disease prevalence for the least educated is rising and the gap in prevalence between the least and most educated is increasing over time. This growing gap by education is particularly dramatic for arthritis, heart disease, and diabetes (Waidmann, Bound, & Schoenbaum, 1995).
Figure 2.
Figure 2.A Gradient in prevalence of five chronic conditions by education among adults aged 40 to 64, 1978–2005
Note: Figure 2.A shows by year the actual raw data on the prevalence of five major conditions for the least educated (0–11) and the most educated groups (16+ years of schooling) and the nonlinear fitted or ‘smoothed’ predictions of that data for those with 0–11 and those with 16+ years of schooling. The shaded area is the area between these fitted lines. The less educated always has higher disease prevalence for all 5 conditions and these differences are widening over time as indicated by the growing width of the shaded area.
Figure 2.B Linear Trends in differences in prevalence of five chronic conditions between high and low education groups among adults aged 40 to 64, 1978–2005
Figure 2.B contains for each disease the actual raw data for differences between prevalence of disease for the less education minus the most educated group and the best OLS linear fit of those differences. The p-values for the slope being different than zero are: Heart, p<.01; Lung, p=.08; Hypertension, p<.01; Diabetes, p<.01; Arthritis, p<.01
Relying on the same data, Figure 2.B plots differences in prevalence for each of the five chronic conditions between the college educated and those who failed to obtain a high school diploma. The solid line for each disease is the best OLS linear fit of these data on differences in prevalence by education. For all diseases, these estimated lines slope downward indicating growing differences in disease prevalence by education to the disfavor of the less educated. The p-values for the estimated slopes being different than zero are all <0.01 for heart, hypertension, diabetes, and arthritis and is .08 for diseases of the lung. There is little doubt that across these decades the likelihood of having each of these chronic diseases during middle age has increased for the less educated compared to the more educated.
Health Among Those With Disease
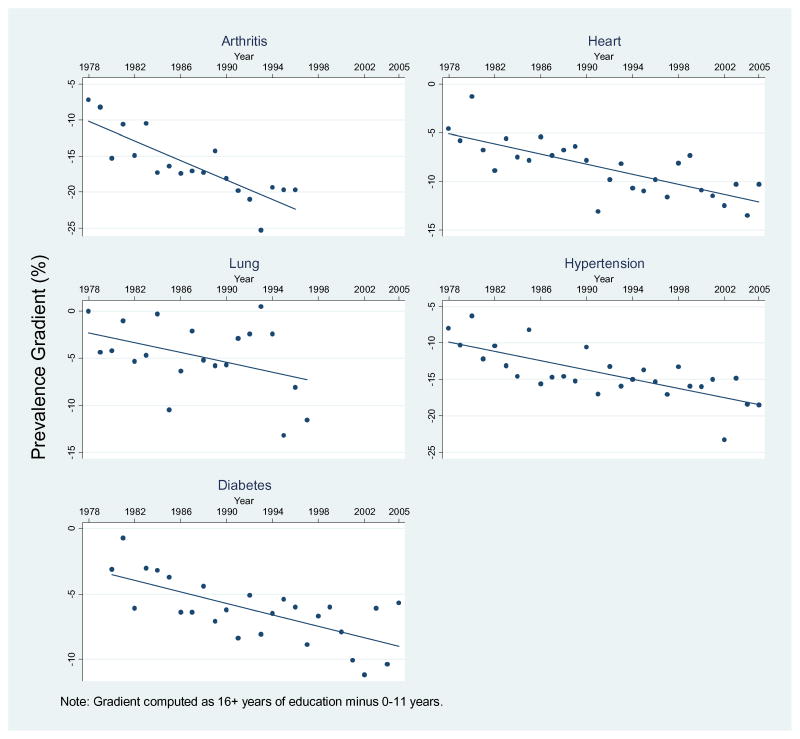
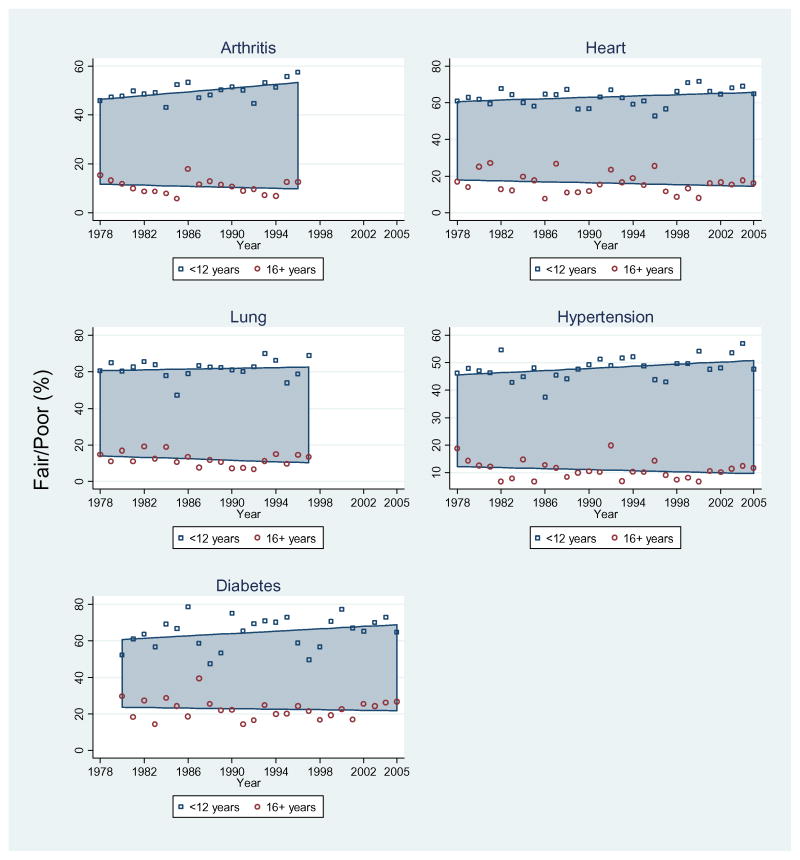
The presence of specific diseases is not the only factor influencing health status. Disease severity and duration, complications of medication, and co-morbidities are also relevant. To assess changing secular trends in the value of health by education within disease, Figure 3.A plots estimated time trends in fractions reporting fair or poor health within five diseases for both education groups. The shaded area between trends lines represents changing differentials in health status by education. Not only have the less educated suffered more from disease onset over the last three decades in that more of them report themselves in fair or poor health, their assessment of their health status within disease deteriorated relative to the more educated.
Figure 3.
Figure 3.A Gradients in percent of population reporting fair or poor health for five chronic conditions among adults aged 40 to 64, 1978–2005
Note: Figure 3.A contains the actual raw data within each disease of the fraction who report themselves in fair or poor health and the nonlinear fitted or ‘smoothed’ predictions of that data for those with 0–11 and those with 16+ years of schooling. The shaded area is the area between these fitted lines. The less educated are always in worse health for all 5 conditions. Most importantly, these differences are widening over time as indicated by the growing width of the shaded area.
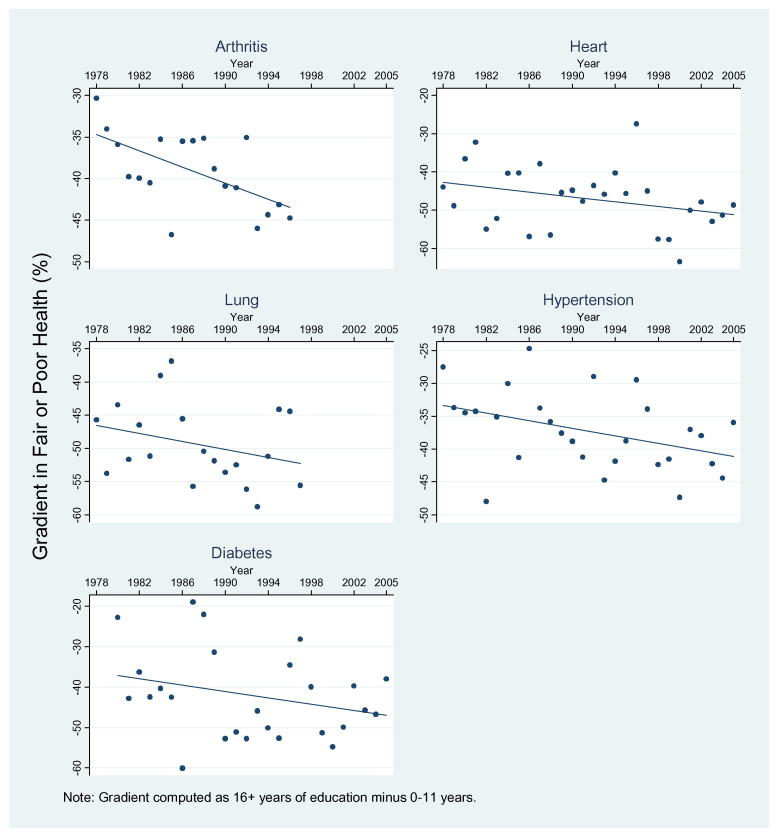
Figure 3.B Differences in % fair or poor health between high and low education groups within disease categories
Figure 3.B contains for each disease the actual raw data for differences between these fractions in fair or poor health for the less education minus the most educated group and the best OLS linear fit of those differences. The p-values for the slope being different than zero are: Heart, p = .10; Lung, p = .19; Hypertension, p = .04; Diabetes, p = .17; Arthritis, p = .01.
Even without controlling for disease, on average there is a 30 percentage point higher fraction in fair or poor health in the low education group compared to the high one. Within disease, differentials in health status are even larger—typically over 40 percentage points indicating that impacts of disease are much more severe on the less educated. This could reflect several factors including more rapid disease progression among less educated due partly to earlier onset and a lower ability to effectively manage disease trajectory.
Figure 3.B contains an alternative way of presenting these trends by plotting for each disease differences in fractions in poor or fair health by these two education classes (Education 16 or more minus Education less than 12). For each disease, the solid line in Figure 3.B shows the best OLS linear fit of the data. The strongest trends in expanding bad health among the less educated are observed for those with heart disease (p=0.10), hypertension (p=0.04) and arthritis (p=0.01) while the p values for diseases of the lung and diabetes are 0.19 and 0.17 respectively.
Trends in Risk Factors by Education Group
To shed light on why these trends occurred, Table 2 lists trends in four health risk behaviors (currently smoking, obesity, exercise, and height in inches) among non-white Hispanics ages 40–64 for three education groups defined consistently over time in NHANES—less than high school, high school graduate, and more than a high school graduate. Under each behavioral risk-factor, the first three rows are fractions with that health behavior—the final row measures within education group change between NHANES IV and NHANES II. We include in this Table the fraction of each sub-population without any type of health insurance as obtained from NHIS. Table 2 also contains test statistics for the existence of a time series trend in each health behavior both for the full sample and within each education group. Finally, we include a test statistic for whether or not the trends are different for the highest education group compared to the lowest education group.
Table 2.
Health Behaviors by Education—Non-Hispanic Whites Ages 40–64 Years
| NHANES Survey | Education Level
|
All | ||
|---|---|---|---|---|
| Low | Middle | High | ||
| Currently smoking (%) | ||||
| 1976–1980 | 41.5 | 36.8 | 32.1 | 37.1 |
| 1988–1994 | 36.6 | 32.0 | 18.6 | 26.6 |
| 1999–2002 | 45.0 | 30.6 | 15.1 | 22.8 |
| Time Series Changea | 3.5 | −6.2*** | −17.0*** | −14.3*** |
| Difference in trend between high and low education of 20.5 has p value <0.001 | ||||
| Body mass index ≥ 30 kg/m2 (%) | ||||
| 1976–1980 | 19.2 | 17.1 | 12.1 | 16.4 |
| 1988–1994 | 33.3 | 30.6 | 19.8 | 26.0 |
| 1999–2002 | 42.2 | 35.9 | 30.4 | 33.3 |
| Time Series Changea | 23.0*** | 18.8*** | 18.3*** | 16.9*** |
| Difference in trend between high and low education of −4.7 has p value of 0.16 | ||||
| Vigorous exercise (%) | ||||
| 1976–1980 | 15.0 | 13.3 | 15.6 | 14.5 |
| 1988–1994 | 11.4 | 16.9 | 41.5 | 27.3 |
| 1999–2002 | 17.4 | 24.7 | 42.8 | 35.1 |
| Time Series Changea | 2.4 | 11.4*** | 27.2*** | 19.6*** |
| Difference in trend between high and low education of 24.8 has p value <0.001 | ||||
| Height (in.) | ||||
| 1976–1980 | 65.9 | 65.9 | 66.9 | 66.2 |
| 1988–1994 | 65.7 | 66.2 | 67.3 | 66.6 |
| 1999–2002 | 65.9 | 66.7 | 67.3 | 67.0 |
| Time Series Changea | 0.0 | 0.8*** | 0.4 | 0.8 |
| Difference in trend between high and low education of 0.4 has p value of 0.43 | ||||
| % Without Health Insuranceb | ||||
| 1980 | 14.1 | 6.7 | 4.4 | 8.5 |
| 1989 | 19.5 | 10.6 | 6.6 | 11.3 |
| 2006 | 25.7 | 16.2 | 7.7 | 11.7 |
| Time Series Changea | 11.6*** | 9.5*** | 3.3*** | 3.2*** |
Difference in trend between high and low education of −7.8 has p value of <0.001
Difference between 1999–2002 and 1976–1980.
Health Insurance data obtained from NHIS
Time series trend is statistically significantly different from zero at the one percent level.
Since there is no strong overall or within education group trend, average height, often used as a simple summary marker for childhood nutrition, is not a plausible reason for growing disparities in disease prevalence or health status by education. Disparities between the highest and lowest education group in all other risk factors by education increased significantly over time and all these growing education disparities are statistically significant. These expanding differences in health behaviors by education are particularly large for smoking, exercise, and the lack of health insurance.
To illustrate, at these ages, current smoking rates increased by 3.5 percentage points (not statistically significant than zero) among the least educated compared to a dramatic fall of 17 percentage points among the most educated (highly statistically different than zero). This statistically significant increase in smoking differentials by education has been shown to contribute to rising differentials by schooling in heart disease and diseases of the lung (Cutler et al, 2007).
Obesity is well established as a strong contributor to the increase in diabetes over time (Smith, 2007a). While obesity rates rose rapidly for all education groups (all trends are statistically significant), rates of increase were somewhat larger among the least educated. The p value for the test in differences in trends for the least and most educated is 0.16. Education differentials in participation in vigorous exercise, protective against heart disease and diabetes, also expanded sharply over time for all groups except the least educated. Not having health insurance is strongly graded by schooling. In 2006 the fraction uninsured is 25.7% among those with less than high school education compared to 7.7% for those beyond high school. While the fraction uninsured rose over time, this problem is growing much faster among the less educated.
Since these set of risk factors are not defined consistently over time in the NHIS, we can only relate these risk factors to disease prevalence with a cross-sectional analysis. We present that analysis in Table 3 for the 2006 NHIS for our sample of Non-Hispanic Whites 40–64 years old. For each of our five diseases we present two prevalence models- (1) the first with only indicators for low education (less than high school) and middle education (high school graduate). In this specification, the coefficient of low education indicator is the difference in prevalence between the low and high education group.
Table 3.
Models of Disease Outcomes and Risk Factors
| Diabetes | Diabetes | Arthritis | Arthritis | Heart disease | Heart Disease | HBP | HBP | Lung Disease | Lung Disease | |
|---|---|---|---|---|---|---|---|---|---|---|
| Ed Low | 0.057*** | 0.031** | 0.095*** | 0.051*** | 0.101*** | 0.074***. | 0.147*** | 0.130*** | 0.118*** | 0.079*** |
| Ed Mid | 0.043*** | 0.033*** | 0.026** | −0.001 | 0.030*** | 0.018* | 0.080*** | 0.051*** | 0.034*** | 0.012 |
| Currently smoke | −0.009 | 0.037*** | 0.031*** | −0.003 | 0.083*** | |||||
| Obese | 0.110*** | 0.135*** | 0058*** | 0.260*** | 0.049*** | |||||
| Vigorous excercise | −0.025*** | −0.020 | −0.030*** | −0.052*** | −0.027*** | |||||
| Height (in inches) | −0.000 | −0.005*** | 0.001 | 0.004** | −0.004*** | |||||
| Constant | 0.061*** | 0.051*** | 0.264*** | 0.577*** | 0.101*** | 0.005* | 0.284*** | −0.029 | 0.278*** |
Statistically significant at the one percent level;
statistically significant at the five percent level:
statistically significant at the ten percent level
In these prevalence models, we initially also included an indicator variable for not-having health insurance which was significantly negative for all five diseases. While at first blush this may seem puzzling, there are two reasons why this could occur. Since these diseases are self-reported in NHIS. this may reflect lack of contact with physicians. More importantly, this may reflect selection effects in that those who choose not to purchase health insurance are actually healthier (so insurance is worth less to them) than those who do have insurance. In either case, this estimate clearly does not represent any health improving impact of being insured. For this reason we confined our analysis in Table 3 to the other risk behaviors.
These risk factors combine to explain a significant part but not all of the education gradient in disease. Comparing the two models for each disease, about half of the education difference between the low and high education groups is explained for diabetes and arthritis, about a third for heart and lung disease and about a fifth for hypertension.
DISCUSSION
Education is a powerful social force, but much of the focus is on how it affects income as earnings differentials by schooling have widened rapidly. We find precisely the same thing happened with health—clear evidence of a rising value of education to health outcomes equivalent to one-quarter of a percentage point per year in self-reported health. Compared to 30 years ago, the probability of having major chronic conditions increased sharply for the least educated compared to the more educated. While improved detection was less rapid among the least educated, studies using biomarkers also show that real disease prevalence increased more rapidly for the less educated (Smith, 2007a). Within disease group, health of the less educated deteriorated compared to the more educated. Using a very different health outcome indicator than the one used here, over this same time period all recent gains in life expectancy in the US were enjoyed by the more educated (Cutler et al 2007).
Our estimates in Table 3 indicate that lifestyle contributes to these growing disparities, and smoking, obesity, and exercise all apparently played roles in prevention of disease. Our analysis documents a pronounced secular deterioration of these health behaviors of the less compared to the more educated. For a risk factor to play an important role, it must be significantly related to disease outcomes, be differentially prevalent across education groups, and have changed over time differentially by education. The last of those criteria eliminates height as a likely explanation (and therefore childhood conditions if height is an adequate summary). Although height is statistically significant in prevalence models for arthritis, hypertension, and lung disease, Table 2 shows that height did not change much over time across education groups.
Smoking is a strong predictor of arthritis, heart and lung disease and exhibits a large growing disparity over time by education. Similarly obesity positively predicts all five diseases with a growing gap between the least and most educated. Engaging in vigorous exercise statistically lowers the probability of all diseases except arthritis and also has differentially changed across the last three decades by education. Thus, all three of these factors combined to contribute to the widening health gap between the education groups.
The growing problem of non-access to health insurance was also increasingly concentrated among the less educated. However, due to strong health selection effects between the insured and non-insured, it is difficult to access the impact of the growing prevalence of non-insurance on these health differentials. Even with near universal insurance the quality of care provided may not only be inferior for the less educated but this gap may be growing over time. However, a recent study investigated differences in quality received by those who had made at least one visit to a health care provider during the previous two years by education groups and found no differences by education (Asch et al, 2006). For this to matter for differential secular trends, the quality of care for the less educated must have been higher than that of more educated groups in the past, a highly implausible result.
What other factors may contribute to growing health disparities by education? One possibility centers on the sharply rising levels of income inequality over the last thirty years in the United States (Card and Di Nardo, 2002 and Lemieux, 2008). The NHIS itself can not be used to examine the effect of rising income inequality on health since family income is placed into income intervals which vary in width especially at the top. For example in the 1996 NHIS the top code is $50,000 or more which includes almost half the sample. Characterizing the 80th percentile of the income distribution and how it changes over time is simply not possible using the NHIS. However, the main characteristics of the changing structure of income in the United States has been well described in several studies, and we can see if those patterns are consistent with our documented changes in the structure of health outcomes.
One of the most comprehensive recent studies is that of Lemieux (2008). In a detailed description consistent with those of other studies, Lemieux documents the following salient trends in changing income inequality in the last three decades; (1) changes are quite large- in 1974 men at the 90th percentile of the wage distribution earned 27% more than those at the 10th percentile- by 2004 that gap had more than doubled to 56%; (2) these trends are highly nonlinear over time with almost three-quarters of the change concentrated in the fifteen years prior to 1989 compared to the subsequent fifteen years; (3) changes in the structure of wages is largely a product of wages changes among the most educated-college graduates and particularly those with post college education. For example among men, compared to high school graduates wages of those with 0–11 years of schooling fell by only 3% between 1974 and 2004 and has actually risen slightly since 1989. In contrast, once again compared to high school graduates, wages of those with post-college degrees were 77% higher than high school graduates in 2004 compared to 37% in 1974.
These wage patterns are not consistent with changes in health by education described in this paper. First in contrast to the highly non-linear trends in the structure of wages, Figure 1 demonstrates that the trend in the deterioration of health of the least education compared to the most educated was quite linear. In addition, in spite of the relatively constant wage differences between high school dropouts and high school graduates with only a three percent decline in relative wages of high school dropouts since 1974, the health gap between these two groups rose steadily and rapidly over these thirty years. Compared to high school graduates, the percent in fair or poor health was 18% higher among high school dropouts in 1974- by 2004 that gap had risen to 27%.
Moreover, these arguments are also based on a presumption that incomes especially of those above the median have significant effects on health outcomes. However, the emerging empirical evidence in the last decade strongly indicates that within the age span of interest education continues to predict new onset of disease and in particular diseases that are our focus in this paper. In sharp contrast, this same evidence consistently shows that income does not predict the future onset of disease even when we allow for non-linear effects of income that distinguish between the top and bottom of the income distribution (Smith, 2004, Smith, 2007b).
Instead of absolute wage changes, another potential hypothesized mechanism is through rising income inequality itself (Wilkinson, 1996). The rationale has many variants, but a common theme is that inequality in relative rank raises levels of psycho-social stress which negatively affects health outcomes. Once again, empirical studies have documented that the timing and patterns of changing income inequality in the United States cannot not explain the timing and patterns of these health outcomes (Deaton and Paxson, 2004, Lynch et al, 2004)
Economists have argued that technological innovations favoring the college-educated—such as the personal computer—contributed to increasing wage gaps. Similarly, protective effects of education may be tied to improving medical technology. One example is the development of home glucose monitoring devices, which help diabetes patients titrate medications and adjust their behavior to achieve better glycemic control. Doing so effectively requires skill that may either be learned through education, or are just complementary with other factors that explain why people have more education. Either way, the result is an association between education and better outcomes for diabetics. Improvements in treatment of heart disease with better drugs and surgical treatments were a major source of extension of life among the middle age and these improvements were larger among the more educated (Cutler et al.2007).
There are also interactions between lifestyle and technology. Arthritis is associated with much pain, and its management requires significant personal involvement including use of medication and exercise. There were substantial improvements in medication and surgical treatments for arthritis over the last 20 years.
Another concern is reverse causation—that poor health in childhood reduces educational attainment producing associations observed in adulthood. However, these effects are relatively small—about half a year, apparently because parents are able compensate for childhood health problems to insure relatively equal outcomes for their children (Marmot, 2000; Case et al. 2002, Smith, 2009). Another possibility concerns changing education composition over time which in fact motivated limiting our sample to non-Hispanic Whites. Among those who did not graduate from high school, the fraction who were either African-American or Hispanic was about a quarter in 1980 compared to about half 20 years later. Given the well-known health problems in these important minority groups especially African-Americans, we did not want changing racial and ethnic mix to confound our analysis of education’s effect.
We probed this issue further. Data from National Assessment of Educational Progress (NAEP) (Campbell, Hombo, & Masseo, 2000), the best indicator of changing American student ability, contains reading and math scores (at ages 13 and 17) of those in the lowest quartile (most likely to be high school dropouts) and those in highest quartile (most likely to be college graduates). While the bottom quartile scores are much lower than the highest quartile, score improvements since 1975 are slightly higher in the lowest quartile, suggesting that changing composition may not be a major factor in explaining these trends when we confine the analysis to our sample. In spite of this data, one would want to have more comprehensive and direct evidence about the changing composition of these education groups over time. Until such evidence is available, the potential role of changing composition can not be dismissed.
One strategy would be to examine changes in the wage distribution over time. However, wages are the product of the price per unit of skill times the amount of skill people have. While our interest centers on the changing distributions in the amount of skill, research by labor economists has demonstrated that the principal force in changing the wage distribution in the last two decades has been an increase in the price of skill (Murphy and Welch, 1992, Lemieux, 2008).
Our restriction to non-Hispanic Whites raises legitimate questions of whether our findings can be replicated in other groups. Table 4 compares changing values of education to health for African-Americans to our sample of non-Hispanic Whites. In either year displayed, there is a larger value to education for African-Americans. Given higher disease prevalence amongst African-Americans, education may play more of a role in improving health for them. There is an equally large secular increase in the value of education for African-American compared to Non-Hispanic Whites.. While additional replication is required for other subgroups, our results appear to apply to other key sub-groups in American society. Table 4 also demonstrates that successfully eliminating racial disparities in health outcomes—a worthy societal goal—would leave the vast majority of health disparities in place.
Table 4.
Percent in Fair or Poor Health by Education and Race
| 0–11 | 16+ | 0–11 - 16+ | |
|---|---|---|---|
| Non-Hispanic Whites | |||
| 1975 | 31.7 | 8.5 | 23.2 |
| 2005 | 37.2 | 4.8 | 32.4 |
|
| |||
| African Americans | |||
| 1975 | 40.4 | 9.6 | 30.8 |
| 2005 | 48.3 | 8.8 | 40.2 |
Data obtained from NHIS for each race ages 40–64 in years indicated.
Several recent studies have shown that among SES markers it is education and not income that is related to onset of disease (Smith, 1999; Campbell et al., 2000). The benefits of education to health can be illustrated with diabetes. Diabetes prevalence has been on an accelerating upward trajectory, which reflects a real increase in prevalence largely associated with the rise in obesity alongside a significant trend toward improved detection (Smith, 2007a). Both factors benefited the more educated compared to the less educated. In the 1970s, half of diabetes cases were undiagnosed and there was no education gradient; today the fraction is about one in five and a significant education gradient in undiagnosis has emerged. The principal factor operating to reduce increases in diabetes prevalence was increases in education which by itself predicted a significant decline in diabetes prevalence points (Smith, 2007a).
With the exception of the rise in obesity, many changes in behavioral risk factors over the last twenty years were health improving as were advances in medical knowledge, treatment, and availability of effective drugs. It was easier for the more educated to reap the benefits of these advances either through the adoption of good personal health behaviors like exercise or the avoidance of unhealthy behaviors like smoking, or a greater ability to adhere to beneficial but difficult drug regimens (Goldman & Smith, 2002). We need a better understanding of what the barriers are that make it more difficult for the less educated to invest in their health and benefit equally from the health enhancing improvements. Without waiting for that understanding, we need to find remedies that compensate for deteriorating relative health outcomes of the most disadvantaged.
Research highlights.
We model changes in changes in health by education over the last three decades in the USA.
We find growing differences in disease prevalence by education.
We find expanding differences by education in health status within disease over time.
The more educated have adopted better health behaviors including not smoking and better exercise.
The more educated have benefited more from improving medical technology
Acknowledgments
This paper was written with the support of grant RO1AG023363 from the National Institute on Aging. The expert programming assistance of David Rumpel is gratefully acknowledged.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dana Goldman, RAND Corporation.
James P. Smith, RAND Corporation, Santa Monica, California UNITED STATES
References
- Acemoglu D. Patterns of Skill Premia. The Review of Economic Studies. 2003 Apr;70(2):199–230. [Google Scholar]
- Asch SM, Kerr EA, Keesey J, Adams JL, Setodji CM, Malik S, et al. Who is at greatest risk for receiving poor-quality health care? New England Journal of Medicine. 2006;354:1147–1156. doi: 10.1056/NEJMsa044464. [DOI] [PubMed] [Google Scholar]
- Campbell JR, Hombo CM, Masseo J. Trends in academic progress: Three decades of student performance NAEP 1999. Washington, DC: U.S. Department of Education, Office of Educational Research and Improvement, National Center for Education Statistics, NCES; 2000. pp. 2000–469. [Google Scholar]
- Card D, DiNardo J. Skill-Biased Technological Change and Rising Wage Inequality: Some Problems and Puzzles. Journal of Labor Economics. 2002 Oct;20(4):733–783. [Google Scholar]
- Case A, Lubotsky D, Paxson C. Economic status and health in childhood: the origins of the gradient. American Economic Review. 2002;92:1308–1334. doi: 10.1257/000282802762024520. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. [Accessed November 3, 2008]; http://www.cdc.gov/nchs/nhis.htm.)
- Centers for Disease Control and Prevention. 1998 National Health Interview Survey-NHIS Survey Description. 2000. [Google Scholar]
- Currie J, Stabile M. Socioeconomic status and child health: why is the relationship stronger for older children? American Economic Review. 2003;93:1813–1823. doi: 10.1257/000282803322655563. [DOI] [PubMed] [Google Scholar]
- Cutler DM, Long G, Berndt ER, Royer J, Fournier A, Sasser A, et al. The value of antihypertensive drugs: a perspective on medical innovation. Health Affairs. 2007;26:97–110. doi: 10.1377/hlthaff.26.1.97. [DOI] [PubMed] [Google Scholar]
- Deaton A, Paxson C. Mortality, Income, and Income Inequality over Time in Britain and in the United States. In: Wise D, editor. Perspectives on the Economics of Aging. University of Chicago Press; 2004. [Google Scholar]
- Goldman D, Smith JP. Can patient self-management help explain the SES health gradient? PNAS. 2002;99:10929–10934. doi: 10.1073/pnas.162086599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Jasso G, Massey D, Rosenzweig M, Smith JP. Immigrant health: selectivity and acculturation. In: Anderson NB, Bulatao RA, Cohen B, editors. Critical Perspectives on Racial and Ethnic Differences in Health in Late Life. Washington, DC: National Academies Press; 2004. pp. 227–266. [PubMed] [Google Scholar]
- Lemieux T. The Changing Nature of Wage Inequality. Journal of Population Economics. 2008 Jan;21(1):21–48. [Google Scholar]
- Lynch J, Smith GD, Harper S, Hillemeier M. Is Income Inequality a Determinant of Population Health? Part 2. U.S. National and Regional Trends in Income Inequality and Age- and Cause Specific Mortality. The Milband Quartely. 2004;82(2):355–400. doi: 10.1111/j.0887-378X.2004.00312.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marmot M. In: Social Epidemiology. Berkman L, Kawachi I, editors. Oxford University Press; New York: 2000. pp. 349–367. [Google Scholar]
- Martin LG, Schoeni RF, Freedman VA, Andreski P. Feeling better? Trends in general health status. J Gerontol B Psychol Sci Soc Sci. 2007;62:S11–S21. doi: 10.1093/geronb/62.1.s11. [DOI] [PubMed] [Google Scholar]
- Murphy K, Topel R. The value of health and longevity. J Polit Econ. 2006;114:871–904. [Google Scholar]
- Murphy K, Welch F. The structure of wages. Q J of Econ. 1992;107:285–326. [Google Scholar]
- Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. New Engl J Med. 1993;329:103–109. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- Preston SH, Taubman P. In: Social Epidemiology. Martin LG, Preston SH, editors. National Academy Press; Washington DC: 1994. pp. 279–318. [Google Scholar]
- Royston P, Altman DG. Approximating statistical functions by using fractional polynomial regression. J Roy Stat Soc (Series D): The Statistician. 1997;46:411–422. [Google Scholar]
- Smith JP. Healthy bodies and thick wallets: The dual relation between health and economic status. J Econ Perspectives. 1999;13:145–167. [PMC free article] [PubMed] [Google Scholar]
- Smith JP. Unraveling the SES-Health Connection. Population & Development Review. 2004;30:108–132. [Google Scholar]
- Smith JP. Nature and causes of trends in male diabetes prevalence, undiagnosed diabetes, and the socioeconomic status health gradient. PNAS. 2007a;104:13225–13231. doi: 10.1073/pnas.0611234104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JP. The Impact of Socioeconomic Status on Health over the Life-Course. Journal of Human Resources. 2007b Fall42(4):739–764. [Google Scholar]
- Smith JP, Kington R. Race, socioeconomic status, and health in late life. In: Martin LG, Soldo BJ, editors. Racial and Ethnic Differences in the Health of Older Americans. Washington, DC: National Academies Press; 1997. pp. 106–162. [PubMed] [Google Scholar]
- Smith JP. The Impact of Childhood Health on Adult Labor Market Outcomes. Review of Economics and Statistics. 2009 August;91(3):478–489. doi: 10.1162/rest.91.3.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waidmann T, Bound J, Schoenbaum M. The illusion of failure: trends in the self-reported health of the U.S. elderly. Milbank Quarterly. 1995;73:253–287. [PubMed] [Google Scholar]
- Weir D, Smith JP. Do Panel Surveys Really Make People Sick? U.S. Arthritis Trends in the Health and Retirement Study. Social Science and Medicine. 2007 September;65(6):2263–2267. [Google Scholar]
- Wilkinson RG. Unhealthy Societies: The Afflictions of Inequality. London: Routledge; 1996. [Google Scholar]