Abstract
Hematopoietic stem cells (HSCs) differentiate into mature lineage restricted blood cells under the influence of a complex network of hematopoietic cytokines, cytokine-mediated transcriptional regulators, and manifold intercellular signaling pathways. The classical model of hematopoiesis proposes that progenitor cells undergo a dichotomous branching into myelo-erythroid and lymphoid lineages. Nonetheless, erythroid and lymphoid restricted progenitors retain their myeloid potential, supporting the existence of an alternative ‘myeloid-based’ mechanism of hematopoiesis. In this case, abnormal pathology is capable of dysregulating hematopoiesis in favor of myelopoiesis. The accumulation of immature CD11b+Gr-1+ myeloid-derived suppressor cells (MDSCs) has been shown to correlate with the presence of several hematopoietic cytokines, transcription factors and signaling pathways, lending support to this hypothesis. Although the negative role of MDSCs in cancer development is firmly established, it is now understood that MDSCs can exert a paradoxical, positive effect on transplantation, autoimmunity, and sepsis. Our conflicted understanding of MDSC function and the complexity of hematopoietic cytokine signaling underscores the need to elucidate molecular pathways of MDSC expansion for the development of novel MDSC-based therapeutics.
Introduction
Hematopoiesis is the hierarchal differentiation of multipotent progenitors into mature blood cells of various lineages and functions. The bone marrow microenvironment provides a complex network of cytokines, transcription factors, and intercellular signaling pathways, most notably Notch, to tightly regulate the progressive lineage commitment of hematopoietic stem cells (HSCs)(1). HSCs themselves are characterized by a lack of lineage markers and by expression of the receptor tyrosine kinase (RTK) c-kit and the surface protein Sca-1, together termed Lin−Sca-1+c-kt+ (LSK)(2). The expression of Flt3 RTK and CD34 further subdivide the LSK compartment into self-renewing long and short-term HSC populations as well as a multipotent progenitor (MPP) population. This hierarchy descends deeper into lymphoid and myeloid compartments where the progenitors are again subdivided into three distinct populations based upon CD34 and low affinity IgG Fc receptors (FcgRII/RIII). These include CD34+FcgRII/IIIlo Common Myeloid Progenitors (CMP), CD34+FcgRII/IIIhi Granulocyte-Macrophage Progenitors (GMP), and CD34−FcgRII/IIIlo Megakaryocyte-Erythroid Progenitors (MEP) (3).
In the classical dichotomous model of differentiation, MPPs give rise to either lineage restricted common myelo-erythroid progenitors (CMEP) or common lymphoid progenitors (CLPs) (4). This process is dependent upon the expression of three proteins: c-kit, the IL-7 receptor and recombination activation gene 1 (RAG1) (5). The relative expression of these species act as a ‘switch’ that determines the ultimate hematopoietic endpoint. While RAG1 and IL-7R expressing CLPs afford T and B lymphocytes, c-Kit+ CMEPs are observed to generate myeloid and erythroid cells (6, 7). This classical model has been recently challenged by the idea that lineage restriction is not necessarily permanent. Several independent observations indicate that early thymocyte and B cell progenitors retain myeloid potential, leading to an alternative, ‘myeloid-based’ mechanism of hematopoiesis (8, 9). Common myelo-lymphoid progenitors (CMLPs) that are phenotypically indistinguishable from LSKs have been observed, and these cells give rise to either B cells, T cells, or myeloid cells. The myeloid-based mechanism excludes the existence of CLPs, stating that differentiation occurs from these CMLP and CMEP progenitors (10). This suggests that, although committed toward T or B lineage, progenitor cells retain the potential towards myeloid lineage. The existence of progenitor myeloid, B and T (p-MBT) cells which are committed B or T cells, yet retain the ability to revert back to myeloid cells further support this possibility (11, 12). Additionally, the observation of several leukemic disease states containing cells of both myeloid and lymphoid origin indicate that a close relationship exists between p-MTB progenitors (8). This process is heavily influenced microvasculature it terms of the cytokines and signaling pathways it can provide to a developing HSC. Therefore, the cytokine profiles in any given pathologic state can also heavily impact hematopoiesis and thus the subsequent immune response.
In response to physiological insult, such as that generated by a pathogenic organism, the host enters a state of ‘emergency’ hematopoiesis characterized by increased recruitment of myeloid lineage cells such as neutrophils and macrophages (13). However, during chronic inflammatory stimuli such as in cancer progression, severe hematopoietic dysregulation can occur at the CMLP or GMP/CMP stages of differentiation (14). This results in the premature bone marrow (BM) recruitment of a heterogeneous population of mononuclear (CD11b+Gr-1intLy6G− Ly6C+) and polymorphonuclear (CD11b+Gr-1highLy6G+ Ly6C−) cells, known as myeloid-derived suppressor cells (MDSCs) (15). Nonetheless, cancer is not the only pathology known to activate MDSC recruitment; other chronic immune stressors such as the natural aging process, solid organ transplantation, parasitic infections, sepsis, autoimmune response, trauma, and burns have been demonstrated to mobilize the MDSC population (16-19). The phenotypic and functional characteristics of MDSCs strongly underscore their myeloid origin. Common cytokines involved in myeloid development have been implicated in the induction of MDSCs. These factors include macrophage-colony stimulating factor (M-CSF), granulocyte-macrophage colony stimulating factor (GM-CSF), Interleukin-6 (IL-6), vascular endothelia growth factor (VEGF), and granulocyte-colony stimulating factor (G-CSF). Several transcription factors involved in myelopoiesis such as interferon-regulatory factor 8 (IRF-8), CAAT/enhancer binding protein-beta (C/EBP-β), and PU.1 have also been demonstrated to regulate MDSC development (20). In addition to myeloid differentiation antigen Gr-1 and CD11b, MDSCs also express various other markers that are traditionally used to define myeloid cells such as CX3CR1, CCR2, CXCL10, CD206, and IL-1B (21). In fact, CD11b+Gr-1+CCR2+CX3CR1low MDSCs can be considered as inflammatory monocytes and can differentiate into DC and macrophages under appropriate stimuli. The expression of IL-4Rα further supports the differentiation of MDSCs into monocytic (IL-4Rα+) and polymorphonculear cells (IL-4Rα−) with the monocytic fraction expressing a more substantial immunosuppressive character due to its ability to secrete IL-13 and IFN-γ (22, 23).
Recent investigations demonstrate that, at the tumor site, MDSCs bear several classically activated (M1) and alternatively activated (M2) macrophage phenotypic and functional characteristics (24). MDSCs express IL-1B, TNF-a, CXCL10, and inducible nitric oxide synthase (iNOS) that is characteristic to M1 macrophages as well as CD206, and arginase I (Arg I), which are M2 specific. Since MDSC development and proliferation occur in an asynchronous manner along the differentiation of CMPs and GMPs toward mature myeloid cells, it is not surprising that they retain a ‘fluid’ spectrum of myeloid cell characteristics.
Despite the ambiguity surrounding their origin, MDSCs are most prominently recognized for their role in the anti-tumor immune response. MDSCs exert their pro-neoplastic effects through the release of small soluble oxidizers, the impairment of T-cell/antigen recognition, and the depletion of essential amino acids from the local extracellular environment, all ultimately leading to T cell suppression (25-28). Additionally, through overproduction of cytokines and angiogenic factors, MDSCs shift immune regulation to a state favoring both tumor escape and proliferation (29). Although the biological and functional properties of myeloid derived suppressor cells have been well characterized and described elsewhere (15, 30-32), the mechanism(s) of their development remains controversial. This review outlines the role of commonly implicated cytokines and cytokine-mediated transcription factors in MDSC expansion. Furthermore, several controversial mechanisms of MDSC mobilization are discussed, including the recent observation of MDSC expansion induced by Notch-mediated hematopoietic dysregulation.
Cytokine and cytokine-induced transcriptional regulation of MDSC expansion
Interleukin-6
As mentioned earlier, the natural immune response to an infection is the production of myeloid cells, a process termed emergency granulopoiesis. Through differentiation, these myeloid cells afford increased populations of monocytes, granulocytes, neutrophils, and more recently, MDSCs in the circulatory system to serve as regulators of the immune response (33). Inflammatory cytokines play a critical role in this process, particularly interleukin 6 (IL-6). IL-6 is a pleiotropic cytokine secreted by numerous immune and non-immune cells. In a state of emergency granulopoiesis, IL-6 induces the production of acute phase proteins and antibodies, while simultaneously mediating hematopoietic progenitor differentiation (5, 34). One of the multiple biological activities of IL-6 comes from its interaction with the CAAT/enhancer binding protein-beta (C/EBP-β) protein, a transcription factor of the leucine zipper family (35). C/EBP transcription factors regulate granulopoiesis; C/EBP-α is required in steady-state granulopoiesis, while C/EBP-β is exploited as a mediator for emergency granulopoiesis (13). C/EBP-α is itself an activator for several requisite genes in myeloid development, in particular the granulocyte-colony stimulating factor receptor (G-CSFR) (36). In the absence of C/EBP-α, abnormal myeloid differentiation from CMP to GMP has been reported (37). Although C/EBP-β has been observed during myeloid differentiation, its abrogation does not result in abnormal granulopoiesis (38). Nonetheless, C/EBP-β appears to specifically affect MDSC production, as myeloid precursors in C/EBP-β−/− mice are unable to differentiate into MDSCs (13, 39, 40). Additional observations suggest that the role of C/EBP-β extends beyond being requisite for MDSC development; C/EBP-β itself may exert a pro-MDSC effect. In vitro experiments have indicated that C/EBP-β promotes the generation of functionally active MDSCs in the presence of IL-6 and the granulocyte-monocyte colony stimulating factor (GM-CSF) (33). Furthermore, using an in vivo murine model, upregulation of C/EBP-β has been shown to correlate with an increase in the degree of immunosuppression induced by a growing tumor (33, 41). While not directly attributable to MDSC production, this observation is consistent with the immune suppression expected from enhanced MDSC expansion.
In direct support of the myeloid-based model of differentiation, IL-6 acts on lymphoid cells possessing myeloid potential, favoring myelopoiesis (35). IL-6 has also been shown to stimulate uncommitted progenitor cells towards myeloid lineage through expression of the Id1 transcription factor (5). The importance of IL-6 is clearly underscored in transgenic mice containing a deletion of the 5′ inositol phosphatase (SHIP) gene. This modification mimics a state of emergency granulopoiesis with concomitant overproduction of IL-6 (42). As a consequence, these mice phenotypically exhibit severe splenomegaly due to the accumulation of functionally active CD11b+Gr-1+ cells. Like tumor-derived MDSCs, these cells significantly impair priming of allogeneic T cell responses and render the animals less susceptible to Graft versus Host Disease (GVHD) (43, 44).
GM-CSF
The granulocyte-macrophage colony stimulating factor (GM-CSF) is recognized as a critical hematopoietic cytokine, mediating the differentiation of myeloid progenitors into granulocytes, eosinophils, monocytes, megakaryocytes, and erythrocytes(45). Remarkably, depending on the concentration of GM-CSF, this factor can exert either a stimulatory or an inhibitory effect on the immune system. In low concentrations, GM-CSF enhances antigen presentation by dendritic cells (DC) as well as cytotoxic CD8+ and T helper CD4+ T cell responses(46). However, as the concentration of GM-CSF is increased, downregulation of DC differentiation and induction of CD11b+Gr-1+ MDSC accumulation can occur (47). Ultimately, this process results in a state of severe immunosuppression, as observed in most cancers. The accumulation of MDSCs is believed to be a specific consequence of GM-CSF’s ability to skew hematopoiesis towards myeloid development. Several studies have reported GM-CSF induced myelopoiesis that is consistent with the myeloid-based model of hematopoiesis (48-50). Transgenic expression of GM-CSFR in hematopoietic tissue results in a preferential shift towards myeloid progenitors at the CMP, GMP and MEP stages (51). Accordingly, these subpopulations favor myeloid development at the expense of lymphoid committed progenitors, hence preventing subsequent lymphopoiesis (52). This is further supported by the observation of myeloid development from committed CLPs when the IL-2RB receptor is inserted into CLPs to upregulate GM-CSFR(53). Accordingly, it is not unreasonable to believe that excessive GM-CSF production, as seen in conditions leading to MDSC accumulation, can skew CMLP and CMEP lineage commitment towards dysregulated myelopoiesis.
G-CSF
The granulocyte-colony stimulating factor (G-CSF) and its receptor are critical regulators of steady state and emergency granulopoiesis. G-CSF promotes the survival, mobilization, and proliferation of myeloid progenitor cells alongside neutrophil differentiation. G-CSF likewise enhances myriad neutrophil functions including phagocytosis, cytokine production, antibody-dependent cellular cytotoxicity, and bactericidal activity (54, 55). Mice deficient in G-CSF or G-CSFR suffer from neutropenia and succumb to bacterial infections due to the decreased activity of resident neutrophils(55). In vivo and in vitro administration of G-CSF reflects its immunomodulatory effects. In the clinical setting, G-CSF is used to treat neutropenia resulting from congenital pathologies or immunosuppressive therapy. However, a fraction of patients receiving G-CSF have developed myeloproliferative disorders such as acute myeloid leukemia (AML) (56). In addition, G-CSF administration can induce DC tolerance, decrease cytotoxic T cell activity, and promote the induction of IL-10 producing myeloid cells(46).
G-CSF mediated MDSC accumulation has been reported in both tumor models and in vitro studies (18, 29). This process is attributed to the interplay between G-CSF and several cytokines and transcription factors known to induce MDSCs. In this case, the relationship with other mediators is immediately apparent: the transcriptional initiation site of G-CSF itself contains binding sites for both IL-6 and NFκB (57). While the role of IL-6 was clearly outlined earlier, NFκB provides a second pathway by MDSC accumulation may occur. In fact, MDSC accumulation has been observed in pathologies during which NFκB is activated through toll-like receptor (TLR) mediated myeloid differentiation primary response gene 88 (MyD88) signaling, including sepsis, trauma, and particular microbial and viral infections (40, 58). Moreover, other inflammatory mediators implicated in MDSC expansion such as IL-1 and IL-17 also activate G-CSF (19, 59-62). Additionally, the G-CSF responsive genes, PU.1 and C/EBP-β are positively correlated with MDSC upregulation (63, 64).
Nonetheless, the primary consequences of G-CSF mediated myelopoiesis emerge from activation of the G-CSF receptor (G-CSFR) in the BM. Following activation, G-CSFR initiates signaling cascade through the Janus Kinase (Jak) / signal transducer and activator of transcription (STAT) pathway (65). STAT proteins are latent cytoplasmic transcription factors activated by a variety of hematopoietic and immune-mediated cytokine receptors. The critical role STATs in hematopoiesis is illustrated by the close association between lympho-proliferative and myeloproliferative disorders with dysregulated STAT signaling (66). In hematopoietic tissue, G-CSFR is the main activator of Stat3 and, to a lesser degree, Stat1 and 5(65). Phosphorylation of Stat3 is markedly increased in tumor-derived MDSCs, and inhibition of Stat3 phosphorylation in hematopoietic progenitors markedly diminishes MDSC expansion (67). Likewise, the activity of Stat3 in myeloid progenitors prevents differentiation and induces immature myeloid cell expansion (63). The downstream signaling partners of Stat3, in particular S100A8 and S100A9, also modulate behavior in the myeloid compartment. Overexpression of S100A9 results in an enhanced c-kit+ myeloid compartment in the BM (68). S100A9 acts in concert with S100A8 to inhibit DC differentiation and promote MDSC expansion. Further MDSC-mediated immune suppression and survival is mediated through Stat1 and Stat5 pathways(40). Given the wide range of G-CSF activities in the BM, it is not surprising that G-CSF secretion by tumor cells and its in vitro administration can skew hematopoiesis in favor of MDSCs.
M-CSF
The macrophage-colony stimulating factor (M-CSF), also known as CD115, is a critical regulator of monocytic development. M-CSF signals through its corresponding tyrosine kinase receptor, which is widely expressed on the CMP and GMP myeloid compartments(20). M-CSF serves a physiological role in the proliferation and differentiation of monocytes, macrophages, and DCs. In genetically altered murine models, the absence of M-CSF and or its receptor induces a dramatic reduction of peripheral monocyte populations that is only restored upon transgene expression of M-CSF(69).
The M-CSFR promoter contains binding sites for several transcription factors implicated in myeloid development, including PU.1, C/EBP-α, and C/EBP-β (70, 71). Furthermore, dimerization of the M-CSF receptor activates numerous downstream pathways, including Stat1, the Ras/Raf/MEK/ Erk pathway, and the phospholipaseCγ (PLCγ) pathway(72). These systems exert manifold regulatory roles in cell-fate determination. In particular, activation of protein kinase c (PKC) by PLCγ promotes monocyte differentiation, while blockade of ERK signaling in vitro induces subsequent abrogation of monocytic differentiation from FDC-P1 cells(73). Signaling through the ERK pathway is necessary to modulate commitment of lymphoid-myeloid progenitor cells toward CMPs rather than CLPs. Accordingly, hematopoietic cells with myeloid and lymphoid potential exhibit a high sensitivity to M-CSF and undergo differentiation towards myeloid cells at high M-CSF concentrations (74). In fact, high M-CSF concentrations inhibit proper myeloid differentiation and promote the differentiation of DCs into macrophage like cells (75).
Several markers indicate that M-CSF exerts a prominent role in MDSCs-related disease states. In particular, M-CSFR mRNA is induced in several pathological conditions in which MDSCs have been implicated. Once recruited to the site of an immune insult, macrophages initiate an autocrine loop of M-CSF production. This, in turn, alters hematopoiesis and induces the recruitment of MDSCs to the site of insult (76). Once recruited to the site, MDSCs perpetuate the loop by producing additional M-CSF (77). Consequently, it is not surprising the MDSCs have been observed in many infections and pathological conditions in which macrophage response is desirable.
In a second pathway, M-CSF is regulated by the transcription factor MafB to restrict lineage commitment toward myelopoiesis (78). The relationship between MafB and M-CSF is evident in murine models, in which overexpression of MafB limits myeloid differentiation. Conversely, a MafB deficiency in these models has been shown to render myeloid progenitors more sensitive to M-CSF. This is presumably due to increased PU.1 activity shifting hematopoiesis toward myeloid development (79). In addition, MafB is highly expressed in LT-HSCs and becomes downregulated during intermediate stages of HSC differentiation with subsequent upregulation occurring upon lineage commitment (20). Although unclear at this time, one can speculate that in line with myeloid-based model of HSC differentiation, it is plausible that MafB regulates the balance of lineage potential and commitment early in CMLPs and later in p-MBTs.
IFN-γ
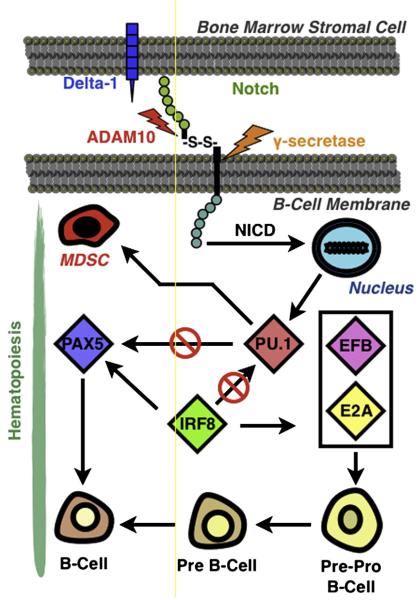
The Th1 cytokine Interferon-gamma (IFNγ) plays a paradoxical role in pathologic states leading to MDSC expansion. IFNγ’s proapoptoic and antiangiogenic effect in innate and adaptive immune responses have made this cytokine an attractive therapy for numerous hematologic malignancies. IFNγ production has been demonstrated to prevent the development of both primary and transplanted tumors. However, it is increasingly recognized that IFNγ may have negative oncological outcomes, specifically with regard to tumor development(80). In particular, IFNγ production by antigen-activated T cells synergizes with MDSC-produced IFNγ to further enhance the suppressive function of MDSCs in a Stat1 dependent and independent manner (81). Conversely, blockade of IFNγ production diminishes MDSC-mediated T cell suppression (22). IFNγ contributes not only to the functional plasticity of MDSCs, but also perhaps to their production through the activity of interferon regulatory factor-8 (IRF-8). Known as the interferon consensus sequence binding protein (ICSBP), IRF-8 is a member of the IRF family of IFN-α and IFN-β dependent transcription factors (82). However, IRF-8 is sensitive to IFNγ and is expressed in hematopoietic myeloid and lymphoid progenitors. Within these cells, IRF-8 serves as a positive modulator of the EBF/E2A transcription system, which regulates B cell development (Figure 1) (83). IRF-8 is also a negative modulator of PU.1, master regulator of myelopoiesis. Inhibition of PU.1 alleviates PAX-5 suppression, which is required for normal B cell development (84). The interplay between PU.1 and B cell development is further supported by the observation in which ectopic expression of PU.1 and C/EBPα induces macrophage cell fate in developing B cells (85). In the absence of IRF-8, PU.1 activity is not inhibited and myeloid differentiation is promoted (86, 87). This is further supported in IRF-8 deficient mice which develop chronic myelogenous-like syndrome subsequent to robust MDSC accumulation(88). Thus, tumor-induced IFNγ dysregulation and IRF-8 reduction would be expected to skew hematopoiesis away from lymphoid development towards myelopoiesis.
Fig. 1.
Putative role of Notch signaling and IRF-8 transcription factor in hematopoietic lineage commitment.Subsequent to ligand engagement and appropriate cleavage by Adam10 and γ-secretase, Notch intracellular domain (NICD) translocates to the nucleus and facilitates transcriptional upregulation of PU.1, mediating differentiation between MDSCs and B cells. IRF-8 serves as a positive EBF/E2A transcription system, which regulates B cell development. IRF-8 also acts as a negative modulator of PU.1, alleviating suppression of the PAX5 transcription factor required for B-cell development. Therefore, the expression of IRF-8 and PU.1 transcription factors as well as Notch signaling regulates MDSC development.
VEGF
Vascular endothelial growth factor (VEGF) is a prototypic growth factor consisting of five family members with tissue specific physiological effects that signal through either of two high affinity tyrosine kinase receptors: VEGFR1, c fms-like tyrosine kinase (Flt1) and VEGFR2, fetal liver kinase-1 (Flk-1)(89, 90). The upregulation and contribution of VEGF to pathogenesis and hematopoietic dysregulation has been well documented in many cancer patients and animal models of neoplasia. Within the BM microenvironment, VEGF is secreted by HSCs to insure cellular survival. In particular, VEGF-deficient HSCs are unable to repopulate in lethally irradiated mice, despite co-administration of WT HSCs. Conversely, stimulation of VEGFR1 rescued their survival of these cells in vivo and in vitro administration of VEGF promoted colony formation. These results indicate that VEGF may regulate hematopoiesis in a cell-autonomous manner by establishing an autocrine loop (91). This assumption is further supported by the autocrine production of VEGF by malignant myeloid precursors in leukemic patients (92), leading to mobilization of immature myeloid progenitors upon stimulation of both VEGFR1 and VEGFR2. VEGF itself binds CD34+ hematopoietic progenitors via VEGFR1, enhancing CD34+ MPP and MEP early progenitor cell production while skewing hematopoiesis in favor of myeloid development (93, 94). This observation supports the myeloid-based model of hematopoiesis, since an increase in VEGF stimulation can induce lineage redistribution of p-MBT cells. In fact, VEGF increased the production of CD34+ progenitor cells with myeloid and lymphoid potential from mouse embryonic stem cells. Furthermore, these cells have been demonstrated to form myeloid colony forming units as well as B220+, CD19+ B lymphocytes when cultured on stromal cells in the presence of IL-2 and IL-7(95).
VEGF differentially regulates hematopoietic alterations contingent upon stimulation of a given VEGFR subpopulation. Signaling through VEGFR1 boosts populations of immature Gr-1+ myeloid and B lymphocytes and ablation of VEGFR1 is associated with decreased HSC survival and differentiation (90, 96). VEGFR1 activation likewise populates the immature myeloid cell compartment by inhibiting NFκB in hematopoietic progenitors. In fact, continous infusion of VEGF abrogates NFκB and downregulates stimulatory FLT3L, thereby reducing DC differentiation and maturation. As a consequence, the immature myeloid compartment is further populated (93, 97). This observation is consistent with observations that alterations in NFκB subunits induce enhanced myelopoiesis and reduced lymphopoiesis (98). The behavior of VEGFR1 is in direct contrast to that mediated by VEGFR2 activation, which promotes CD11b+Gr-1+ MDSCs at the expense of B cells at the pro-B cell state(99). In particular, continuous infusion of VEGF results in decreased lymphoid compartment concomitant with increased myeloid populations, thereby inducing splenomegaly (93). The consequence of increased VEGF signaling in dysregulated hematopoiesis could occur through VEGF/VEGFR modulation of p-MBT cells, redirecting their commitment towards a lymphoid or a myeloid cell.
The controversial role of Notch signaling in MDSC development
The canonical Notch signaling pathway is required for differentiation and cell fate determination during hematopoietic development. The Notch pathway is highly conserved, comprising four families of receptors (Notch1-4) that interact with ligands (Jagged and Delta) expressed by neighboring cells(1). Once engaged with its ligand, the extracellular domain of Notch receptor undergoes cleavage at site 2 (S2) by a disintergrin and metalloproteinase 10 (ADAM10) (100). This results in a subsequent S3 cleavage of the intracellular domain by γ-secretase, releasing the Notch Intracellular Domain (NICD). NICD then translocates into the nucleus to activate various transcription factors such as Hes1, Hes5 and Deltex, and thus exert its effector functions(101). Notch1 mRNA and protein has been found in various stages of cell differentiation including LSKs, CLPs, CMPs, GMPs and MEPs(1). Although the activity of Notch is firmly established in T-cell lineage commitment and maturation, as well as in B-cell marginal zone development, its role in myelopoiesis remains controversial (102, 103).
Several investigators have reported that alterations in Notch signaling have minimal effects on myelopoiesis (104-106). Nonetheless, many convincing investigations conclude the contrary. Enforced expression of NICD or Notch target genes in BM progenitors abrogates B cell development and promotes myeloid differentiation in a non-cell autonomous manner (64, 107). Additionally, undifferentiated myeloid cells have been observed to accumulate in a 32D myeloid progenitor cell line with constitutive Notch-1 expression (108). The importance of Notch in myelopoiesis extends further to in vivo models. Specifically, mice deficient in downstream Notch effectors exhibit defective B cell and myeloid development (109). In light of these observations, it is reasonable to speculate that increased Notch signaling can overcome IRF-8 induced PU.1 inhibition during hematopoiesis, as indicated in a model Figure 1. In fact, enhanced PU.1 expression and myeloid differentiation have been observed in the presence of activated Notch signaling (64).
Taken together, these observations indicate that Notch-mediated alterations in lymphocyte development can impact myelopoiesis. Recent data lend further support to this argument and is consistent with the myeloid based model of hematopoiesis. In particular, two groups have reported that CMLPs are indistinguishable from LSKs and retain the ability to revert back to myeloid cells once committed to lymphoid lineage (8, 109). The exact manner through which these signals integrate into the Notch cascade and subsequent myelopoiesis appears multifaceted; both Notch1 and Notch2 inhibit myeloid differentiation while MDSC accumulation has been observed in mice with diminished γ-secretase activity (110, 111). Furthermore, mice with increased ADAM10 activity also demonstrate altered hematopoiesis in favor of MDSC development as a consequence of perturbed Notch signaling (112).
The retention of myeloid potential and the expression of Notch1 mRNA and protein in various progenitor populations suggest that Notch signaling is indispensable for proper lineage commitment. Furthermore, the conflicting nature of these collective findings indicates that myeloid differentiation is dependent upon the strength and temporal stage of Notch signaling. Further examination of Notch regulators, including ADAM10, may elucidate the role of Notch signaling in lineage differentiation and myeloid development.
Conclusion
Irrespective of their origin, inflammatory stimuli induce emergency granulo-poiesis, in which myelopoiesis is preferred pathway for immune response. Under sustained stimulation, dysregulated hematopoiesis can occur, favoring excessive BM myelopoiesis with the accumulation of immature CD11b+Gr-1+ myeloid precursors in the periphery. The role of Notch signaling in this process is at present controversial. Nonetheless, it is possible that Notch signaling, concomitant with cytokine-induced transcriptional regulation, can influence the differentiation of both myeloid and lymphoid committed cells towards myeloid cells. The overwhelming production of these cells within the limited BM niche would induce their subsequent migration to peripheral organs prior to receipt of appropriate differentiation signals. The phenotypic and functional plasticity of MDSCs indicates that their recruitment may occur at several stages of the myelomonocytic differentiation pathway. Accordingly, it is not surprising that genetically manipulated murine models and in vitro systems have suggested several possible, isolated mechanisms for MDSC expansion. The common denominator in these studies is the dysregulation of hematopoiesis, which is a central tenent of the myeloid based model of hematopoiesis. It is possible that most of the MDSCs generated have their origin in CMLP progenitors rather than CMEP, as other blood cell populations are not dramatically altered in many pathological conditions with MDSC accumulation.
MDSCs comprise a high proportion of wild-type murine BM, however, these cells undergo subsequent differentiation and hence only a small percentage is detected in the periphery. While MDSCs may regulate immune response in a manner promoting tumor development, in other conditions such as GVHD, solid organ transplantation, autoimmunity and sepsis, they exert a beneficial action. Further investigations are necessary to ascertain if MDSC expansion may be exploited as a therapeutic strategy to modulate immune response, and to determine whether these cellular chameleons require a unique cell lineage classification of their own.
References
- 1.Milner LA, Bigas A. Notch as a mediator of cell fate determination in hematopoiesis: evidence and speculation. Blood. 1999;93:2431–2448. [PubMed] [Google Scholar]
- 2.Rosnet O, Schiff C, Pebusque MJ, Marchetto S, Tonnelle C, Toiron Y, Birg F, Birnbaum D. Human FLT3/FLK2 gene: cDNA cloning and expression in hematopoietic cells. Blood. 1993;82:1110–1119. [PubMed] [Google Scholar]
- 3.Pronk CJ, Rossi DJ, Mansson R, Attema JL, Norddahl GL, Chan CK, Sigvardsson M, Weissman IL, Bryder D. Elucidation of the phenotypic, functional, and molecular topography of a myeloerythroid progenitor cell hierarchy. Cell Stem Cell. 2007;1:428–442. doi: 10.1016/j.stem.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Weissman IL, Anderson DJ, Gage F. Stem and progenitor cells: origins, phenotypes, lineage commitments, and transdifferentiations. Annu Rev Cell Dev Biol. 2001;17:387–403. doi: 10.1146/annurev.cellbio.17.1.387. [DOI] [PubMed] [Google Scholar]
- 5.Maeda K, Malykhin A, Teague-Weber BN, Sun XH, Farris AD, Coggeshall KM. Interleukin-6 aborts lymphopoiesis and elevates production of myeloid cells in systemic lupus erythematosus-prone B6.Sle1.Yaa animals. Blood. 2009;113:4534–4540. doi: 10.1182/blood-2008-12-192559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karsunky H, Inlay MA, Serwold T, Bhattacharya D, Weissman IL. Flk2+ common lymphoid progenitors possess equivalent differentiation potential for the B and T lineages. Blood. 2008;111:5562–5570. doi: 10.1182/blood-2007-11-126219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forsberg EC, Bhattacharya D, Weissman IL. Hematopoietic stem cells: expression profiling and beyond. Stem Cell Rev. 2006;2:23–30. doi: 10.1007/s12015-006-0005-z. [DOI] [PubMed] [Google Scholar]
- 8.Kawamoto H, Katsura Y. A new paradigm for hematopoietic cell lineages: revision of the classical concept of the myeloid-lymphoid dichotomy. Trends Immunol. 2009;30:193–200. doi: 10.1016/j.it.2009.03.001. [DOI] [PubMed] [Google Scholar]
- 9.Chi AW, Bell JJ, Zlotoff DA, Bhandoola A. Untangling the T branch of the hematopoiesis tree. Curr Opin Immunol. 2009;21:121–126. doi: 10.1016/j.coi.2009.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kawamoto H, Wada H, Katsura Y. A revised scheme for developmental pathways of hematopoietic cells: the myeloid-based model. Int Immunol. 2010;22:65–70. doi: 10.1093/intimm/dxp125. [DOI] [PubMed] [Google Scholar]
- 11.Kawamoto H, Ohmura K, Katsura Y. Direct evidence for the commitment of hematopoietic stem cells to T, B and myeloid lineages in murine fetal liver. Int Immunol. 1997;9:1011–1019. doi: 10.1093/intimm/9.7.1011. [DOI] [PubMed] [Google Scholar]
- 12.Lu M, Kawamoto H, Katsube Y, Ikawa T, Katsura Y. The common myelolymphoid progenitor: a key intermediate stage in hemopoiesis generating T and B cells. J Immunol. 2002;169:3519–3525. doi: 10.4049/jimmunol.169.7.3519. [DOI] [PubMed] [Google Scholar]
- 13.Hirai H, Zhang P, Dayaram T, Hetherington CJ, Mizuno S, Imanishi J, Akashi K, Tenen DG. C/EBPbeta is required for ‘emergency’ granulopoiesis. Nat Immunol. 2006;7:732–739. doi: 10.1038/ni1354. [DOI] [PubMed] [Google Scholar]
- 14.Sonda N, Chioda M, Zilio S, Simonato F, Bronte V. Transcription factors in myeloid-derived suppressor cell generation. Curr Opin Immunol. 2011 doi: 10.1016/j.coi.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 15.Gabrilovich DI, Nagaraj S. Myeloid-derived suppressor cells as regulators of the immune system. Nat Rev Immunol. 2009;9:162–174. doi: 10.1038/nri2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dilek N, van Rompaey N, Le Moine A, Vanhove B. Myeloid-derived suppressor cells in transplantation. Curr Opin Organ Transplant. 2010 doi: 10.1097/MOT.0b013e3283401742. [DOI] [PubMed] [Google Scholar]
- 17.Gomez CR, Boehmer ED, Kovacs EJ. The aging innate immune system. Curr Opin Immunol. 2005;17:457–462. doi: 10.1016/j.coi.2005.07.013. [DOI] [PubMed] [Google Scholar]
- 18.Highfill SL, Rodriguez PC, Zhou Q, Goetz CA, Koehn BH, Veenstra R, Taylor PA, Panoskaltsis-Mortari A, Serody JS, Munn DH, Tolar J, Ochoa AC, Blazar BR. Bone marrow myeloid-derived suppressor cells (MDSCs) inhibit graft-versus-host disease (GVHD) via an arginase-1-dependent mechanism that is up-regulated by interleukin-13. Blood. 2010;116:5738–5747. doi: 10.1182/blood-2010-06-287839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cuenca AG, Delano MJ, Kelly-Scumpia KM, Moreno C, Scumpia PO, Laface DM, Heyworth PG, Efron PA, Moldawer LL. A Paradoxical Role for Myeloid Derived Suppressor Cells in Sepsis and Trauma. Mol Med. 2010 doi: 10.2119/molmed.2010.00178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Auffray C, Sieweke MH, Geissmann F. Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu Rev Immunol. 2009;27:669–692. doi: 10.1146/annurev.immunol.021908.132557. [DOI] [PubMed] [Google Scholar]
- 21.Steinlin M, Imfeld S, Zulauf P, Boltshauser E, Lovblad KO, Luthy A. Ridolfi, Perrig W, Kaufmann F. Neuropsychological long-term sequelae after posterior fossa tumour resection during childhood. Brain. 2003;126:1998–2008. doi: 10.1093/brain/awg195. [DOI] [PubMed] [Google Scholar]
- 22.Gallina G, Dolcetti L, Serafini P, De Santo C, Marigo I, Colombo MP, Basso G, Brombacher F, Borrello I, Zanovello P, Bicciato S, Bronte V. Tumors induce a subset of inflammatory monocytes with immunosuppressive activity on CD8+ T cells. J Clin Invest. 2006;116:2777–2790. doi: 10.1172/JCI28828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Geissmann F, Jung S, Littman DR. Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity. 2003;19:71–82. doi: 10.1016/s1074-7613(03)00174-2. [DOI] [PubMed] [Google Scholar]
- 24.Umemura N, Saio M, Suwa T, Kitoh Y, Bai J, Nonaka K, Ouyang GF, Okada M, Balazs M, Adany R, Shibata T, Takami T. Tumor-infiltrating myeloid-derived suppressor cells are pleiotropic-inflamed monocytes/macrophages that bear M1- and M2-type characteristics. J Leukoc Biol. 2008;83:1136–1144. doi: 10.1189/jlb.0907611. [DOI] [PubMed] [Google Scholar]
- 25.Talmadge JE. Pathways mediating the expansion and immunosuppressive activity of myeloid-derived suppressor cells and their relevance to cancer therapy. Clin Cancer Res. 2007;13:5243–5248. doi: 10.1158/1078-0432.CCR-07-0182. [DOI] [PubMed] [Google Scholar]
- 26.Viola A, Bronte V. Metabolic mechanisms of cancer-induced inhibition of immune responses. Semin Cancer Biol. 2007;17:309–316. doi: 10.1016/j.semcancer.2007.06.005. [DOI] [PubMed] [Google Scholar]
- 27.Corzo CA, Cotter MJ, Cheng P, Cheng F, Kusmartsev S, Sotomayor E, Padhya T, McCaffrey TV, McCaffrey JC, Gabrilovich DI. Mechanism regulating reactive oxygen species in tumor-induced myeloid-derived suppressor cells. J Immunol. 2009;182:5693–5701. doi: 10.4049/jimmunol.0900092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bunt SK, Yang L, Sinha P, Clements VK, Leips J, Ostrand-Rosenberg S. Reduced inflammation in the tumor microenvironment delays the accumulation of myeloid-derived suppressor cells and limits tumor progression. Cancer Res. 2007;67:10019–10026. doi: 10.1158/0008-5472.CAN-07-2354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mantovani A. The growing diversity and spectrum of action of myeloid-derived suppressor cells. Eur J Immunol. 2010;40:3317–3320. doi: 10.1002/eji.201041170. [DOI] [PubMed] [Google Scholar]
- 30.Youn JI, Gabrilovich DI. The biology of myeloid-derived suppressor cells: the blessing and the curse of morphological and functional heterogeneity. Eur J Immunol. 2010;40:2969–2975. doi: 10.1002/eji.201040895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fujimura T, Mahnke K, Enk AH. Myeloid derived suppressor cells and their role in tolerance induction in cancer. J Dermatol Sci. 2010;59:1–6. doi: 10.1016/j.jdermsci.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Ostrand-Rosenberg S. Myeloid-derived suppressor cells: more mechanisms for inhibiting antitumor immunity. Cancer Immunol Immunother. 2010;59:1593–1600. doi: 10.1007/s00262-010-0855-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marigo I, Bosio E, Solito S, Mesa C, Fernandez A, Dolcetti L, Ugel S, Sonda N, Bicciato S, Falisi E, Calabrese F, Basso G, Zanovello P, Cozzi E, Mandruzzato S, Bronte V. Tumor-induced tolerance and immune suppression depend on the C/EBPbeta transcription factor. Immunity. 2010;32:790–802. doi: 10.1016/j.immuni.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 34.Newburger PE. IL6 to the rescue. Blood. 2008;111:3914–3915. doi: 10.1182/blood-2008-01-133975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Poli V, Mancini FP, Cortese R. IL-6DBP, a nuclear protein involved in interleukin-6 signal transduction, defines a new family of leucine zipper proteins related to C/EBP. Cell. 1990;63:643–653. doi: 10.1016/0092-8674(90)90459-r. [DOI] [PubMed] [Google Scholar]
- 36.Zhang DE, Zhang P, Wang ND, Hetherington CJ, Darlington GJ, Tenen DG. Absence of granulocyte colony-stimulating factor signaling and neutrophil development in CCAAT enhancer binding protein alpha-deficient mice. Proc Natl Acad Sci U S A. 1997;94:569–574. doi: 10.1073/pnas.94.2.569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang P, Iwasaki-Arai J, Iwasaki H, Fenyus ML, Dayaram T, Owens BM, Shigematsu H, Levantini E, Huettner CS, Lekstrom-Himes JA, Akashi K, Tenen DG. Enhancement of hematopoietic stem cell repopulating capacity and self-renewal in the absence of the transcription factor C/EBP alpha. Immunity. 2004;21:853–863. doi: 10.1016/j.immuni.2004.11.006. [DOI] [PubMed] [Google Scholar]
- 38.Screpanti I, Romani L, Musiani P, Modesti A, Fattori E, Lazzaro D, Sellitto C, Scarpa S, Bellavia D, Lattanzio G, et al. Lymphoproliferative disorder and imbalanced T-helper response in C/EBP beta-deficient mice. EMBO J. 1995;14:1932–1941. doi: 10.1002/j.1460-2075.1995.tb07185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang H, Nguyen-Jackson H, Panopoulos AD, Li HS, Murray PJ, Watowich SS. STAT3 controls myeloid progenitor growth during emergency granulopoiesis. Blood. 2010;116:2462–2471. doi: 10.1182/blood-2009-12-259630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Condamine T, Gabrilovich DI. Molecular mechanisms regulating myeloid-derived suppressor cell differentiation and function. Trends Immunol. 2011;32:19–25. doi: 10.1016/j.it.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ng PK, Tsui SK, Lau CP, Wong CH, Wong WH, Huang L, Kumta SM. CCAAT/enhancer binding protein beta is up-regulated in giant cell tumor of bone and regulates RANKL expression. J Cell Biochem. 2010;110:438–446. doi: 10.1002/jcb.22556. [DOI] [PubMed] [Google Scholar]
- 42.Nakamura K, Kouro T, Kincade PW, Malykhin A, Maeda K, Coggeshall KM. Src homology 2-containing 5-inositol phosphatase (SHIP) suppresses an early stage of lymphoid cell development through elevated interleukin-6 production by myeloid cells in bone marrow. J Exp Med. 2004;199:243–254. doi: 10.1084/jem.20031193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paraiso KH, Ghansah T, Costello A, Engelman RW, Kerr WG. Induced SHIP deficiency expands myeloid regulatory cells and abrogates graft-versus-host disease. J Immunol. 2007;178:2893–2900. doi: 10.4049/jimmunol.178.5.2893. [DOI] [PubMed] [Google Scholar]
- 44.Ghansah T, Paraiso KH, Highfill S, Desponts C, May S, McIntosh JK, Wang JW, Ninos J, Brayer J, Cheng F, Sotomayor E, Kerr WG. Expansion of myeloid suppressor cells in SHIP-deficient mice represses allogeneic T cell responses. J Immunol. 2004;173:7324–7330. doi: 10.4049/jimmunol.173.12.7324. [DOI] [PubMed] [Google Scholar]
- 45.Metcalf D. Hematopoietic cytokines. Blood. 2008;111:485–491. doi: 10.1182/blood-2007-03-079681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martins A, Han J, Kim SO. The multifaceted effects of granulocyte colony-stimulating factor in immunomodulation and potential roles in intestinal immune homeostasis. IUBMB Life. 2010;62:611–617. doi: 10.1002/iub.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Serafini P, Carbley R, Noonan KA, Tan G, Bronte V, Borrello I. High-dose granulocyte-macrophage colony-stimulating factor-producing vaccines impair the immune response through the recruitment of myeloid suppressor cells. Cancer Res. 2004;64:6337–6343. doi: 10.1158/0008-5472.CAN-04-0757. [DOI] [PubMed] [Google Scholar]
- 48.Borojevic R, Carvalho MA, Correa-Junior JD, Arcanjo K, Gomes L, Joazeiro PP, Balduino A, Wettreich A, Coelho-Sampaio T. Stroma-mediated granulocyte-macrophage colony-stimulating factor (GM-CSF) control of myelopoiesis: spatial organisation of intercellular interactions. Cell Tissue Res. 2003;313:55–62. doi: 10.1007/s00441-003-0726-0. [DOI] [PubMed] [Google Scholar]
- 49.Iwasaki-Arai J, Iwasaki H, Miyamoto T, Watanabe S, Akashi K. Enforced granulocyte/macrophage colony-stimulating factor signals do not support lymphopoiesis, but instruct lymphoid to myelomonocytic lineage conversion. J Exp Med. 2003;197:1311–1322. doi: 10.1084/jem.20021843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Raskin RE. Myelopoiesis and myeloproliferative disorders. Vet Clin North Am Small Anim Pract. 1996;26:1023–1042. doi: 10.1016/s0195-5616(96)50054-9. [DOI] [PubMed] [Google Scholar]
- 51.Nishijima I, Nakahata T, Watanabe S, Tsuji K, Tanaka I, Hirabayashi Y, Inoue T, Arai K. Hematopoietic and lymphopoietic responses in human granulocyte-macrophage colony-stimulating factor (GM-CSF) receptor transgenic mice injected with human GM-CSF. Blood. 1997;90:1031–1038. [PubMed] [Google Scholar]
- 52.Yasuda Y, Nishijima I, Watanabe S, Arai K, Zlotnik A, Moore TA. Human granulocyte-macrophage colony-stimulating factor (hGM-CSF) induces inhibition of intrathymic T-cell development in hGM-CSF receptor transgenic mice. Blood. 1997;89:1349–1356. [PubMed] [Google Scholar]
- 53.Kondo M, Scherer DC, Miyamoto T, King AG, Akashi K, Sugamura K, Weissman IL. Cell-fate conversion of lymphoid-committed progenitors by instructive actions of cytokines. Nature. 2000;407:383–386. doi: 10.1038/35030112. [DOI] [PubMed] [Google Scholar]
- 54.Jiang D, Schwarz H. Regulation of granulocyte and macrophage populations of murine bone marrow cells by G-CSF and CD137 protein. PLoS One. 2010;5:e15565. doi: 10.1371/journal.pone.0015565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Carulli G. Effects of recombinant human granulocyte colony-stimulating factor administration on neutrophil phenotype and functions. Haematologica. 1997;82:606–616. [PubMed] [Google Scholar]
- 56.Beekman R, Touw IP. G-CSF and its receptor in myeloid malignancy. Blood. 2010;115:5131–5136. doi: 10.1182/blood-2010-01-234120. [DOI] [PubMed] [Google Scholar]
- 57.Dunn SM, Coles LS, Lang RK, Gerondakis S, Vadas MA, Shannon MF. Requirement for nuclear factor (NF)-kappa B p65 and NF-interleukin-6 binding elements in the tumor necrosis factor response region of the granulocyte colony-stimulating factor promoter. Blood. 1994;83:2469–2479. [PubMed] [Google Scholar]
- 58.Delano MJ, Scumpia PO, Weinstein JS, Coco D, Nagaraj S, Kelly-Scumpia KM, O’Malley KA, Wynn JL, Antonenko S, Al-Quran SZ, Swan R, Chung CS, Atkinson MA, Ramphal R, Gabrilovich DI, Reeves WH, Ayala A, Phillips J, Laface D, Heyworth PG, Clare-Salzler M, Moldawer LL. MyD88-dependent expansion of an immature GR-1(+)CD11b(+) population induces T cell suppression and Th2 polarization in sepsis. J Exp Med. 2007;204:1463–1474. doi: 10.1084/jem.20062602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.He RL, Zhou J, Hanson CZ, Chen J, Cheng N, Ye RD. Serum amyloid A induces G-CSF expression and neutrophilia via Toll-like receptor 2. Blood. 2009;113:429–437. doi: 10.1182/blood-2008-03-139923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Cai XY, Gommoll CP, Jr., Justice L, Narula SK, Fine JS. Regulation of granulocyte colony-stimulating factor gene expression by interleukin-17. Immunol Lett. 1998;62:51–58. doi: 10.1016/s0165-2478(98)00027-3. [DOI] [PubMed] [Google Scholar]
- 61.Schwarzenberger P, Huang W, Ye P, Oliver P, Manuel M, Zhang Z, Bagby G, Nelson S, Kolls JK. Requirement of endogenous stem cell factor and granulocyte-colony-stimulating factor for IL-17-mediated granulopoiesis. J Immunol. 2000;164:4783–4789. doi: 10.4049/jimmunol.164.9.4783. [DOI] [PubMed] [Google Scholar]
- 62.He D, Li H, Yusuf N, Elmets CA, Li J, Mountz JD, Xu H. IL-17 promotes tumor development through the induction of tumor promoting microenvironments at tumor sites and myeloid-derived suppressor cells. J Immunol. 2010;184:2281–2288. doi: 10.4049/jimmunol.0902574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.McLemore ML, Grewal S, Liu F, Archambault A, Poursine-Laurent J, Haug J, Link DC. STAT-3 activation is required for normal G-CSF-dependent proliferation and granulocytic differentiation. Immunity. 2001;14:193–204. doi: 10.1016/s1074-7613(01)00101-7. [DOI] [PubMed] [Google Scholar]
- 64.Schroeder T, Kohlhof H, Rieber N, Just U. Notch signaling induces multilineage myeloid differentiation and up-regulates PU.1 expression. J Immunol. 2003;170:5538–5548. doi: 10.4049/jimmunol.170.11.5538. [DOI] [PubMed] [Google Scholar]
- 65.Panopoulos AD, Watowich SS. Granulocyte colony-stimulating factor: molecular mechanisms of action during steady state and ‘emergency’ hematopoiesis. Cytokine. 2008;42:277–288. doi: 10.1016/j.cyto.2008.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ward AC, Touw I, Yoshimura A. The Jak-Stat pathway in normal and perturbed hematopoiesis. Blood. 2000;95:19–29. [PubMed] [Google Scholar]
- 67.Xin H, Zhang C, Herrmann A, Du Y, Figlin R, Yu H. Sunitinib inhibition of Stat3 induces renal cell carcinoma tumor cell apoptosis and reduces immunosuppressive cells. Cancer Res. 2009;69:2506–2513. doi: 10.1158/0008-5472.CAN-08-4323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cheng P, Corzo CA, Luetteke N, Yu B, Nagaraj S, Bui MM, Ortiz M, Nacken W, Sorg C, Vogl T, Roth J, Gabrilovich DI. Inhibition of dendritic cell differentiation and accumulation of myeloid-derived suppressor cells in cancer is regulated by S100A9 protein. J Exp Med. 2008;205:2235–2249. doi: 10.1084/jem.20080132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chitu V, Stanley ER. Colony-stimulating factor-1 in immunity and inflammation. Curr Opin Immunol. 2006;18:39–48. doi: 10.1016/j.coi.2005.11.006. [DOI] [PubMed] [Google Scholar]
- 70.Ross IL, Yue X, Ostrowski MC, Hume DA. Interaction between PU.1 and another Ets family transcription factor promotes macrophage-specific Basal transcription initiation. J Biol Chem. 1998;273:6662–6669. doi: 10.1074/jbc.273.12.6662. [DOI] [PubMed] [Google Scholar]
- 71.Yue X, Favot P, Dunn TL, Cassady AI, Hume DA. Expression of mRNA encoding the macrophage colony-stimulating factor receptor (c-fms) is controlled by a constitutive promoter and tissue-specific transcription elongation. Mol Cell Biol. 1993;13:3191–3201. doi: 10.1128/mcb.13.6.3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Bonifer C, Hume DA. The transcriptional regulation of the Colony-Stimulating Factor 1 Receptor (csf1r) gene during hematopoiesis. Front Biosci. 2008;13:549–560. doi: 10.2741/2700. [DOI] [PubMed] [Google Scholar]
- 73.Filderman AE, Bruckner A, Kacinski BM, Deng N, Remold HG. Macrophage colony-stimulating factor (CSF-1) enhances invasiveness in CSF-1 receptor-positive carcinoma cell lines. Cancer Res. 1992;52:3661–3666. [PubMed] [Google Scholar]
- 74.Himes SR, Tagoh H, Goonetilleke N, Sasmono T, Oceandy D, Clark R, Bonifer C, Hume DA. A highly conserved c-fms gene intronic element controls macrophage-specific and regulated expression. J Leukoc Biol. 2001;70:812–820. [PubMed] [Google Scholar]
- 75.Menetrier-Caux C, Montmain G, Dieu MC, Bain C, Favrot MC, Caux C, Blay JY. Inhibition of the differentiation of dendritic cells from CD34(+) progenitors by tumor cells: role of interleukin-6 and macrophage colony-stimulating factor. Blood. 1998;92:4778–4791. [PubMed] [Google Scholar]
- 76.Irvine KM, Burns CJ, Wilks AF, Su S, Hume DA, Sweet MJ. A CSF-1 receptor kinase inhibitor targets effector functions and inhibits pro-inflammatory cytokine production from murine macrophage populations. FASEB J. 2006;20:1921–1923. doi: 10.1096/fj.06-5848fje. [DOI] [PubMed] [Google Scholar]
- 77.Zhou Z, French DL, Ma G, Eisenstein S, Chen Y, Divino CM, Keller G, Chen SH, Pan PY. Development and function of myeloid-derived suppressor cells generated from mouse embryonic and hematopoietic stem cells. Stem Cells. 2010;28:620–632. doi: 10.1002/stem.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hegde SP, Zhao J, Ashmun RA, Shapiro LH. c-Maf induces monocytic differentiation and apoptosis in bipotent myeloid progenitors. Blood. 1999;94:1578–1589. [PubMed] [Google Scholar]
- 79.Bakri Y, Sarrazin S, Mayer UP, Tillmanns S, Nerlov C, Boned A, Sieweke MH. Balance of MafB and PU.1 specifies alternative macrophage or dendritic cell fate. Blood. 2005;105:2707–2716. doi: 10.1182/blood-2004-04-1448. [DOI] [PubMed] [Google Scholar]
- 80.Trinchieri G. Type I interferon: friend or foe? J Exp Med. 2010;207:2053–2063. doi: 10.1084/jem.20101664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Movahedi K, Guilliams M, Van den Bossche J, Van den Bergh R, Gysemans C, Beschin A, De Baetselier P, Van Ginderachter JA. Identification of discrete tumor-induced myeloid-derived suppressor cell subpopulations with distinct T cell-suppressive activity. Blood. 2008;111:4233–4244. doi: 10.1182/blood-2007-07-099226. [DOI] [PubMed] [Google Scholar]
- 82.Zhao J, Kong HJ, Li H, Huang B, Yang M, Zhu C, Bogunovic M, Zheng F, Mayer L, Ozato K, Unkeless J, Xiong H. IRF-8/interferon (IFN) consensus sequence-binding protein is involved in Toll-like receptor (TLR) signaling and contributes to the cross-talk between TLR and IFN-gamma signaling pathways. J Biol Chem. 2006;281:10073–10080. doi: 10.1074/jbc.M507788200. [DOI] [PubMed] [Google Scholar]
- 83.Wang H, Lee CH, Qi C, Tailor P, Feng J, Abbasi S, Atsumi T, Morse HC., 3rd IRF8 regulates B-cell lineage specification, commitment, and differentiation. Blood. 2008;112:4028–4038. doi: 10.1182/blood-2008-01-129049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tsujimura H, Nagamura-Inoue T, Tamura T, Ozato K. IFN consensus sequence binding protein/IFN regulatory factor-8 guides bone marrow progenitor cells toward the macrophage lineage. J Immunol. 2002;169:1261–1269. doi: 10.4049/jimmunol.169.3.1261. [DOI] [PubMed] [Google Scholar]
- 85.Xie H, Ye M, Feng R, Graf T. Stepwise reprogramming of B cells into macrophages. Cell. 2004;117:663–676. doi: 10.1016/s0092-8674(04)00419-2. [DOI] [PubMed] [Google Scholar]
- 86.Wang H, Morse HC., 3rd IRF8 regulates myeloid and B lymphoid lineage diversification. Immunol Res. 2009;43:109–117. doi: 10.1007/s12026-008-8055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tamura T, Ozato K. ICSBP/IRF-8: its regulatory roles in the development of myeloid cells. J Interferon Cytokine Res. 2002;22:145–152. doi: 10.1089/107999002753452755. [DOI] [PubMed] [Google Scholar]
- 88.Stewart TJ, Greeneltch KM, Reid JE, Liewehr DJ, Steinberg SM, Liu K, Abrams SI. Interferon regulatory factor-8 modulates the development of tumour-induced CD11b+Gr-1+ myeloid cells. J Cell Mol Med. 2009;13:3939–3950. doi: 10.1111/j.1582-4934.2009.00685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Voelkel NF, Vandivier RW, Tuder RM. Vascular endothelial growth factor in the lung. Am J Physiol Lung Cell Mol Physiol. 2006;290:L209–221. doi: 10.1152/ajplung.00185.2005. [DOI] [PubMed] [Google Scholar]
- 90.Huang Y, Chen X, Dikov MM, Novitskiy SV, Mosse CA, Yang L, Carbone DP. Distinct roles of VEGFR-1 and VEGFR-2 in the aberrant hematopoiesis associated with elevated levels of VEGF. Blood. 2007;110:624–631. doi: 10.1182/blood-2007-01-065714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gerber HP, Malik AK, Solar GP, Sherman D, Liang XH, Meng G, Hong K, Marsters JC, Ferrara N. VEGF regulates haematopoietic stem cell survival by an internal autocrine loop mechanism. Nature. 2002;417:954–958. doi: 10.1038/nature00821. [DOI] [PubMed] [Google Scholar]
- 92.Bellamy WT, Richter L, Sirjani D, Roxas C, Glinsmann-Gibson B, Frutiger Y, Grogan TM, List AF. Vascular endothelial cell growth factor is an autocrine promoter of abnormal localized immature myeloid precursors and leukemia progenitor formation in myelodysplastic syndromes. Blood. 2001;97:1427–1434. doi: 10.1182/blood.v97.5.1427. [DOI] [PubMed] [Google Scholar]
- 93.Gabrilovich D, Ishida T, Oyama T, Ran S, Kravtsov V, Nadaf S, Carbone DP. Vascular endothelial growth factor inhibits the development of dendritic cells and dramatically affects the differentiation of multiple hematopoietic lineages in vivo. Blood. 1998;92:4150–4166. [PubMed] [Google Scholar]
- 94.Broxmeyer HE, Cooper S, Li ZH, Lu L, Song HY, Kwon BS, Warren RE, Donner DB. Myeloid progenitor cell regulatory effects of vascular endothelial cell growth factor. Int J Hematol. 1995;62:203–215. doi: 10.1016/0925-5710(95)00412-2. [DOI] [PubMed] [Google Scholar]
- 95.Nakayama N, Fang I, Elliott G. Natural killer and B-lymphoid potential in CD34+ cells derived from embryonic stem cells differentiated in the presence of vascular endothelial growth factor. Blood. 1998;91:2283–2295. [PubMed] [Google Scholar]
- 96.Gerber HP, Ferrara N. The role of VEGF in normal and neoplastic hematopoiesis. J Mol Med. 2003;81:20–31. doi: 10.1007/s00109-002-0397-4. [DOI] [PubMed] [Google Scholar]
- 97.Kusmartsev S, Gabrilovich DI. Effect of tumor-derived cytokines and growth factors on differentiation and immune suppressive features of myeloid cells in cancer. Cancer Metastasis Rev. 2006;25:323–331. doi: 10.1007/s10555-006-9002-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Dikov MM, Oyama T, Cheng P, Takahashi T, Takahashi K, Sepetavec T, Edwards B, Adachi Y, Nadaf S, Daniel T, Gabrilovich DI, Carbone DP. Vascular endothelial growth factor effects on nuclear factor-kappaB activation in hematopoietic progenitor cells. Cancer Res. 2001;61:2015–2021. [PubMed] [Google Scholar]
- 99.Larrivee B, Pollet I, Karsan A. Activation of vascular endothelial growth factor receptor-2 in bone marrow leads to accumulation of myeloid cells: role of granulocyte-macrophage colony-stimulating factor. J Immunol. 2005;175:3015–3024. doi: 10.4049/jimmunol.175.5.3015. [DOI] [PubMed] [Google Scholar]
- 100.van Tetering G, van Diest P, Verlaan I, van der Wall E, Kopan R, Vooijs M. Metalloprotease ADAM10 is required for Notch1 site 2 cleavage. J Biol Chem. 2009;284:31018–31027. doi: 10.1074/jbc.M109.006775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kopan R, Ilagan MX. The canonical Notch signaling pathway: unfolding the activation mechanism. Cell. 2009;137:216–233. doi: 10.1016/j.cell.2009.03.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Gibb DR, El Shikh M, Kang DJ, Rowe WJ, El Sayed R, Cichy J, Yagita H, Tew JG, Dempsey PJ, Crawford HC, Conrad DH. ADAM10 is essential for Notch2-dependent marginal zone B cell development and CD23 cleavage in vivo. J Exp Med. 2010;207:623–635. doi: 10.1084/jem.20091990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Cheng P, Gabrilovich D. Notch signaling in differentiation and function of dendritic cells. Immunol Res. 2008;41:1–14. doi: 10.1007/s12026-007-8011-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Carlesso N, Aster JC, Sklar J, Scadden DT. Notch1-induced delay of human hematopoietic progenitor cell differentiation is associated with altered cell cycle kinetics. Blood. 1999;93:838–848. [PubMed] [Google Scholar]
- 105.Pui JC, Allman D, Xu L, DeRocco S, Karnell FG, Bakkour S, Lee JY, Kadesch T, Hardy RR, Aster JC, Pear WS. Notch1 expression in early lymphopoiesis influences B versus T lineage determination. Immunity. 1999;11:299–308. doi: 10.1016/s1074-7613(00)80105-3. [DOI] [PubMed] [Google Scholar]
- 106.Stier S, Cheng T, Dombkowski D, Carlesso N, Scadden DT. Notch1 activation increases hematopoietic stem cell self-renewal in vivo and favors lymphoid over myeloid lineage outcome. Blood. 2002;99:2369–2378. doi: 10.1182/blood.v99.7.2369. [DOI] [PubMed] [Google Scholar]
- 107.Kawamata S, Du C, Li K, Lavau C. Notch1 perturbation of hemopoiesis involves non-cell- autonomous modifications. J Immunol. 2002;168:1738–1745. doi: 10.4049/jimmunol.168.4.1738. [DOI] [PubMed] [Google Scholar]
- 108.Schroeder T, Just U. Notch signalling via RBP-J promotes myeloid differentiation. EMBO J. 2000;19:2558–2568. doi: 10.1093/emboj/19.11.2558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kawamata S, Du C, Li K, Lavau C. Overexpression of the Notch target genes Hes in vivo induces lymphoid and myeloid alterations. Oncogene. 2002;21:3855–3863. doi: 10.1038/sj.onc.1205487. [DOI] [PubMed] [Google Scholar]
- 110.Bigas A, Martin DI, Milner LA. Notch1 and Notch2 inhibit myeloid differentiation in response to different cytokines. Mol Cell Biol. 1998;18:2324–2333. doi: 10.1128/mcb.18.4.2324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Qyang Y, Chambers SM, Wang P, Xia X, Chen X, Goodell MA, Zheng H. Myeloproliferative disease in mice with reduced presenilin gene dosage: effect of gamma-secretase blockage. Biochemistry. 2004;43:5352–5359. doi: 10.1021/bi049826u. [DOI] [PubMed] [Google Scholar]
- 112.Gibb DR, Saleem SJ, Kang DJ, Subler MA, Conrad DH. ADAM10 Overexpression Shifts Lympho- and Myelopoiesis by Dysregulating Site 2/Site 3 Cleavage Products of Notch. J Immunol. 2011 doi: 10.4049/jimmunol.1003318. [DOI] [PMC free article] [PubMed] [Google Scholar]