Abstract
Objective
Little is known about the effect of social context and gender on ADHD persistence in children of early and middle school years. The study compares persistence of DSM-IV attention-deficit/hyperactivity disorder (ADHD) and ADHD not otherwise specified (NOS) over two years, in two groups of Puerto Rican children.
Method
A three wave study obtained data on Puerto Rican children aged 5 through 13 years at baseline. Samples were drawn in the south Bronx in New York (N = 1,138) and two metropolitan areas in Puerto Rico (N = 1,353). The Diagnostic Interview Schedule for Children-IV was used to diagnose ADHD and ADHD-NOS.
Results
ADHD or ADHD-NOS diagnosis at wave 1 strongly predicted disorder at waves 2 and 3. ADHD has a significantly stronger predictive effect than ADHD-NOS consistently across site and gender. There is a significant interaction with baseline age. For those younger at baseline the strength of the prediction of ADHD-NOS is relatively weak; for older children the presence of ADHD-NOS at baseline predicts risk of subsequent ADHD or ADHD-NOS.
Conclusions
Persistence of ADHD in children of similar ethnicity does not manifest differently across context and gender. Results suggest that age-specific symptom criteria and modification of age of onset criteria should be considered for the diagnosis.
Keywords: ADHD, persistence, ADHD-NOS, gender, context
Attention-deficit hyperactivity disorder (ADHD) can affect individuals across the life span.1 The Fourth Edition of DSM (DSM-IV)1 vaguely defines a subthreshold condition, ADHD not otherwise specified (ADHD-NOS), as “disorders characterized with prominent symptoms of inattention or hyperactivity-impulsivity that do not meet criteria” for ADHD. The number of symptoms required for “prominence” or the degree of impairment necessary for the diagnosis are not provided. Discussions about how to deal with these aspects of ADHD continue as the proposed edition (DSM-V) is being prepared. In the methods section we provide the operational definition of ADHD-NOS that is used in this study.
ADHD is considered to be a persistent disorder. Persistence has been studied using different diagnostic criteria and assessment procedures. Most existing studies were carried out using clinical samples without strictly applying DSM-IV criteria at baseline and/or follow-up assessments.2 In a meta analysis of over thirty studies, Faraone, Biederman and Mick3 reported that persistence rates varied from less than 5% to more than 85%, a variability partly due to methodological issues such as how diagnosis was made (whether ADHD involved only a full threshold diagnosis or included subthreshold ADHD), the interval between measurements and the age at initial assessment. In general, studies of older children found less persistence than those of younger children. Greater persistence was found when the follow-up criterion included subthreshold as well as full diagnosis.
Most studies in the meta-analysis3 involved treated cases, and emphasized persistence from childhood to adulthood. Whether subjects are treatment referred or randomly drawn from the community is of critical importance, as both prevalence and persistence are found to be lower in community samples. Clinic-referred subjects have more symptomatology and impairment.4 Other characteristics of referred samples have been associated with persistence of ADHD, including psychiatric comorbidity, psychosocial adversity, and early childhood hyperactivity.5–7 Presumably clinical treatment affects the presence or absence of subsequent symptoms and could confound the results when persistence is studied in clinic-referred samples. Even in community studies, a proportion of children with the diagnosis will be receiving treatment, as was true in our sample.8
Symptoms of ADHD decline with age,6,9,10 and lower rates of persistence during adolescence and adulthood may not reflect a true decline of the disorder. The decline may be an artifact of DSM-IV symptom criteria in that characteristics typical of older adolescent or adult ADHD are not specified in the manual. Current criteria require 6 of 9 symptoms of inattention or 6 of 9 symptoms of hyperactivityimpulsivity. Older individuals may cope better with the disorder and report fewer symptoms. Some adolescents and adults may seemingly have remitted because established symptom thresholds are insufficiently sensitive to detect the disorder at older ages, because a different symptom typology in older age groups involves symptoms that are not elicited,3,11 or possibly because of a different age of onset. Such issues have forwarded a discussion of whether DSM-V should lower symptom thresholds for older adolescents and adults or whether they require a different operationalization of the disorder. The discussion, nevertheless, highlights the importance of considering both a lower threshold and an older age of onset in the definition of ADHD.12
Presence and persistence of symptoms may manifest differently across context and gender due to sociocultural variations in what is considered normative behavior.13 Persistence may be greater in contexts where chronic stress from discrimination or economic disadvantage exists. Despite the fact that ADHD is viewed as a neurobiological disorder, its persistence, comorbidity, and the degree of associated impairment may be influenced by contextual factors, such as psychosocial adversity.5,7 To our knowledge no studies have systematically studied the effects of psychosocial variables on the persistence of ADHD. Gender may further moderate the influence of contextual factors over time. Little is known about gender differences in the trajectory of ADHD or subthreshold ADHD. Existing evidence does not support gender differences in persistence over time.14,15
There are important gaps in the current literature on persistence of ADHD among children. Only three studies reviewed employed DSM-IV diagnostic assessments both at baseline and follow-up,9,16,17 with only one carried out on a non-clinical sample.17 The latter was a twin study to test stability of ADHD subtypes, with a sample not representative of children in the community. The literature does not contain information about the persistence of ADHD among school age children who may or may not have been assigned to treatment.
In this report we address this gap using existing data from the Boricua Youth Study (BYS).18–20 These data provide an exceptional opportunity to study how context can influence the presence and persistence of ADHD symptoms across development over a three-year period. The assessments at three time points, one year apart, can shed light on the timing of changes in the frequency of ADHD diagnosis. This is the first study to evaluate the persistence of ADHD and ADHD-NOS in a community sample using DSM-IV diagnostic assessments at both baseline and follow-up. The study considers the influence of context, baseline age, and gender on the persistence of the disorder.
Method
Previous reports provide the parent study's methodology and findings.8,18–20 In brief, the longitudinal study was designed to assess prevalence, associated comorbidities and risk factors of disruptive behavior disorders among Puerto Rican children in two contexts: The South Bronx (SB) in New York City (N=1,138) and the Standard Metropolitan Areas in San Juan and Caguas, Puerto Rico (PR) (N=1,353). Children aged 5 to 13 years at baseline were followed over three waves one year apart (mean 349.6 days; SD 54.6). Each sample is a multistage probability sample of households of the target populations, and each can be weighted to represent the populations of Puerto Rican children in the SB and PR. A household was eligible if: (1) there was at least one child residing in the household aged 5 through 13 years identified as being of Puerto Rican background and (2) at least one of the child's parents or primary caretakers also self-identified as being of Puerto Rican background. Up to three eligible children per household were selected at random to participate.
Children and caretakers were interviewed in English or Spanish, using the Diagnostic Interview Schedule for Children (DISC-IV)21,22 and other measures previously described by Bird et al.18 The DISC was not administered to children under 10 years because the reliability of younger informants' responses to the DISC is questionable.23,24 In order to have the same information base for all subjects aged 5 through 13 years, cases of ADHD were defined using only data obtained from the adult informant on the DISC-IV.
Test-retest reliability of parent reports for ADHD diagnosis is acceptable (K=0.49 for the Spanish DISC-IV and K=0.60 for the English DISC-IV), representing fair to good agreement.21,22 For the ADHD schedule, agreement between lay interviewer and clinician administered DISC-IV as well as agreement with clinical judgment has fluctuated from fair to good.24,25
Procedures
Adult informed consent and youth assent used forms and procedures approved by the New York State Psychiatric Institute and the University of Puerto Rico Medical School Institutional Review Boards. Characteristics of the interviews have been previously reported.18,19 Data collection for the three-wave study spanned a period of almost four years averaging approximately one year between waves for each respondent. Attrition was low with subject retention over three waves approximately 90%.20 Because all study data were computerized, interviewers were blind to any results from previous waves of the study.
Diagnostic Status
We constructed three categories of diagnostic status: (1) neither current ADHD nor ADHD-NOS, (2) current ADHD and (3) current ADHD-NOS. The ADHD-NOS category was operationalized assigning the diagnosis of “ADHD-NOS” both to those that meet ADHD symptom and impairment criteria but do not meet the onset before age 7 criterion (n=56) and those who are symptomatically subthreshold (defined below) for the ADHD diagnosis and have associated impairment (n=176). To assess impairment, parents of children who either meet symptom criteria or who are subthreshold are asked a standard series of six, two-part questions about impairment in six domains: relationship with parents/caretakers, participation in family activities, participation in peer activities, relationship with teachers (boss), academic (occupational) functioning, and distress. Each domain utilizes a stem/contingent structure, where the stem determines if there is any “impairment” and the contingent measures frequency or severity. Including impairment in the operationalization of ADHD-NOS was considered important in order to maintain false positives at a minimum and to be faithful to DSM-IV requirements for clinical significance. The subthreshold grouping does not consider age of onset but follows the suggestions of the DISC developers (P. Fisher, Personal communication). More specifically, the subject does not meet full criteria for ADHD but needs to have at least half (3 to 5) of the symptoms present in either ADHD dimension (inattentive or hyperactive/impulsive), needs to manifest the symptoms in at least two settings (ADHD Criterion C) and has either a moderate rating of impairment in at least two of the six domains measured, or a severe rating in at least one domain (Criterion D). This definition qualifies for the vague definition of ADHD-NOS provided in DSM-IV and fits well with the examples provided in DSM-IV Revised text (2000).26
Statistical Analyses
We adjusted for differences in the probability of selection due to sample design and differences from the 2000 census in the age/gender distribution. For estimates of means, rates and correlations among variables, we used SUDAAN software (release 8)27 to compute weighted estimates and to adjust standard errors for intraclass correlations induced by multi-stage sampling, with children nested within households and households nested within primary sampling units.
Because youth in the two sites might have differed in multiple ways besides living in different locations, we carried out a propensity score adjustment in the analysis. This method creates groups of PR and SB youth that appear to be comparable on a number of factors, including a combination of maternal age, maternal education and family income. Using logistic regression, we created a model that predicted who would be expected to be from PR on the basis of youth and family characteristics. This allowed us to identify SB youth who had characteristics similar to PR youth (i.e. would be predicted to have been in the PR sample rather than their true SB sample), and also the opposite, PR youth who had characteristics similar to SB youth. Following conventions five propensity score strata were defined that contained youth who were relatively similar with regard to their mother's age, education and family income.28 We included variables that represented these strata in the analysis to adjust for site differences
Analytic strategy for overall persistence
The goal is to determine the degree to which ADHD and ADHD-NOS predict those disorders in subsequent years. The outcome is whether a youth showed either ADHD or ADHD-NOS at the second and/or third waves. The independent variable is baseline diagnoses of ADHD, defined as mutually exclusive categories of ADHD, ADHD-NOS, or neither. Because the outcome is a binary repeated measure, we use logistic regression with generalized estimating equations.29 Adjustments are made for site through propensity score groups based on site, gender, and age at baseline. Our analytic model emphasizes persistence from the baseline (wave1) assessment to later assessments (wave 2 or 3),We include an indicator of whether the outcome is observed at wave 2 or 3 to determine if the degree of persistence decreases as the length of follow-up increases.
Analytic strategy to assess the influence of context, gender and age
Two variations of the logistic model were considered. In the first, we focused on the main effects of ADHD diagnosis after adjusting for the propensity score variables, demographics and time of outcome. In the second we included interactions of ADHD diagnosis with site, gender and age to determine whether the predictive utility of diagnosis varied by site, gender or age. For both sets of analyses we used the GENMOD procedure of SAS with adjustments made for the complex survey design.
Results
Rates of ADHD Disorders over Time
In Table 1 we report the rates of ADHD and ADHD plus ADHD-NOS (which we call ADHD+) at follow-up for groups of children defined on the basis of their diagnostic status at wave 1. For those who were diagnosed with ADHD or ADHD-NOS at wave 1 the rates that appear in the Table indicate the rate of persistence. Overall the persistence of either baseline ADHD or ADHD-NOS is higher when the outcome is ADHD+. Among those with wave 1 ADHD (only) there is a median persistence rate of 50% when the outcome is ADHD+ (Wave 1 ADHD to Wave 2 or 3 ADHD+). When the outcome is restricted to ADHD (Wave 1 ADHD to Wave 2 or 3 ADHD) the median persistence rate is 37%. Persistence of those with wave 1 ADHD-NOS is lower: the median rate is 30% when the outcome is ADHD+ (Wave 1 ADHD-NOS to Wave 2 or 3 ADHD+) and is 8% if the outcome is defined as ADHD (Wave 1ADHDNOS to Wave 2 or 3ADHD). Among those with neither ADHD nor ADHD-NOS at wave1, the median rate of ADHD at either follow-up was 2% and 5% for the broader outcome (ADHD+).
Table 1.
Persistence of attention-deficit hyperactivity disorder (ADHD) and ADHD not otherwise specified across site and gender
| Percent Positive (95% CI) |
||||||
|---|---|---|---|---|---|---|
| ADHD (Wave 2) | ADHD (Wave 3) | ADHD+NOS (Wave 2) | ADHD+NOS (Wave 3) | |||
| Status at Wave 1 | Unweighted N | |||||
| South Bronx | ||||||
| Males | ADHD | 44 | 41.7 (27.1,57.8) | 36.4 (24.2, 50.5) | 63.6 (45.7, 76.9) | 47.7 (33.7, 62.0) |
| ADHD NOS | 50 | 12.3 (5.5, 25.2) | 16.0 (8.0, 29.2) | 39.1 (26.6, 53.3 | 38.8 (25.2, 54.4) | |
| No ADHD | 416 | 4.7 (3.0, 7.2) | 4.3 (2.5, 7.2) | 11.9 (9.1, 15.3) | 8.8 (6.3, 12.3) | |
| Females | ADHD | 23 | 29.4 (13.2, 53.3) | 13.3 (4.5, 33.3) | 57.4 (36.5, 75.9) | 26.8 (13.9, 45.4) |
| ADHD NOS | 40 | 6.9 (2.2, 19.9) | 2.2 (.03, 14.1) | 23.3 (12.7, 38.8) | 26.4 (14.6, 43.1) | |
| No ADHD | 420 | 2.6 (1.4, 4.9) | 1.0 (.4, 2.6) | 6.7 (4.4, 10.0) | 4.3 (2.7, 6.9) | |
| Metro San Juan | ||||||
| Males | ADHD | 58 | 30.6 (18.8, 45.7) | 37.3 (24.3, 52.6) | 65.7 (52.4, 76.8) | 54.7 (40.0, 68.6) |
| ADHDNOS | 84 | 7.7 (3.6, 16.0) | 9.3 (4.0, 19.9) | 35.9 (24.1, 49.7) | 31.2 (21.7, 42.7) | |
| No ADHD | 506 | 3.2 (1.7, 5.7) | 1.8 (0.9, 3.8) | 7.5 (5.2, 10.5) | 5.7 (4.0, 8.0) | |
| Females | ADHD | 21 | 37.1 (15.0, 66.2) | 31.1 (11.0, 62.7) | 42.1 (17.9, 70.7) | 32.7 (12.0, 63.3) |
| ADHD NOS | 37 | 3.5 (0.8, 14.1) | 7.1 (1.7, 25.3) | 19.2 (18.8, 36.9) | 25.1 (12.4, 44.2) | |
| No ADHD | 560 | 1.5 (0.7, 3.2) | 1.0 (0.4, 2.8) | 5.3 (3.6, 7.8) | 3.5 (2.2, 5.5) | |
Note: ADHD= attention-deficit hyperactivity disorder; NOS= not otherwise specified
Persistence among males is generally higher than among females. For ADHD the level of persistence diminished from wave 2 to 3, but for ADHD-NOS the level of persistence remains generally constant over time. The comparison of rates across sites shows no simple pattern.
Multivariate analyses
To further investigate the patterns of persistence over Waves 2 and 3, we carried out logistic regression analyses predicting overall ADHD+. These analyses showed the degree to which rates of persistence noted in Table 1 were statistically stable after adjustment for other variables. We included ADHD-NOS in the outcome to fully consider symptomatic persistence and to have a comprehensive understanding of the progression and outcomes of the disorder.
Table 2 shows the results of the model predicting persistence of ADHD as a function of site, gender, age, and ADHD status at baseline. The results of the main effect model are shown on the left hand column. Even after adjusting for baseline diagnosis of ADHD or ADHD-NOS, girls were about half as likely to be diagnosed with either ADHD or ADHD-NOS (ADHD+) than boys (β (SE) = ~0.589 (0.135), odds ratio [OR] = 0.55). There was also a trend for youth in Puerto Rico to have slightly less ADHD+ at follow-up after adjusting for disorder at baseline (β (SE) = ~0.24 (0.136), p =0.070, OR = 0.78). Finally, there was an indication that the risk of ADHD+ decreased from wave 2 to wave 3 (β (SE)= ~0.334 (0.086), p<. 0001). The rate of disorder at wave 3 is on average, 72% of what it was in wave 2.
Table 2.
Estimates from logistic regression predicting persistence of attention-deficit hyperactivity disorder (ADHD) as measured by presence of ADHD or ADHD not otherwise specified at waves 2 and 3 as a function of wave 1 clinical status, site, gender, age and interactions.
| Predictor | ADHD Model 1 | ADHD Model 2 | ||||
|---|---|---|---|---|---|---|
| Estimate (SE) | p Value | Odds Ratio | Estimate (SE) | p Value | Odds Ratio | |
| Intercept | −2.15 (.17) | <.0001 | 0.12 | −2.13 (.19) | <.0001 | 0.12 |
| Site | ||||||
| Puerto Rico (Ref. South Bronx) | −0.24 (.14) | 0.073 | 0.78 | −0.43 (.21) | 0.04 | 0.65 |
| Gender | ||||||
| Female (Ref. Male) | −0.59 (.14) | <.0001 | 0.55 | −0.60 (.20) | 0.003 | 0.55 |
| Age (10) | 0.001 (.02) | 0.966 | 1.00 | −0.04 (.04) | 0.24 | 0.96 |
| ADHD | 2.67 (.18) | <.0001 | 14.50 | 2.52 (.28) | <.0001 | 12.45 |
| ADHD NOS | 1.80 (.16) | <.0001 | 6.03 | 1.74 (.26) | <.0001 | 5.74 |
| Wave 2 to 3 stability | −0.33 (.08) | <.0001 | 0.72 | −0.34 (.09) | <.0001 | 0.71 |
| ADHD × Site | -- | -- | -- | 0.47 (.37) | 0.198 | 1.60 |
| ADHD NOS × Site | -- | -- | -- | 0.24 (.32) | 0.461 | 1.27 |
| ADHD × Gender | -- | -- | -- | −0.15 (.39) | 0.690 | 0.86 |
| ADHD NOS × Gender | -- | -- | -- | 0.001 (.34) | 0.997 | 1.00 |
| ADHD × Age (10) | -- | -- | -- | 0.03 (.07) | 0.698 | 1.03 |
| ADHD NOS × Age (10) | -- | -- | -- | 0.19 (.06) | 0.003 | 1.21 |
| Age (10) × Site | -- | -- | -- | −0.01 (.05) | 0.837 | 0.99 |
| Gender × Site | -- | -- | -- | 0.11 (.27) | 0.685 | 1.12 |
Note: General estimating equations parameter estimates and standard errors. Propensity scores were adjusted in the models. ADHD= attention-deficit hyperactivity disorder; NOS= not otherwise specified
Persistence involves the relation of wave 1 diagnosis with disorder at follow-up. There is significant persistence at waves 2 and 3. Those who had a diagnosis of ADHD at wave 1 were over 14 times more likely to have a diagnosis of ADHD or ADHD-NOS than those with no disorder at Wave 1(β (SE) = 2.674 (0.179), p <. 0001), whereas those who had a diagnosis of ADHD-NOS were about 6 times more likely to have the ADHD+ diagnosis at waves 2 or 3. Although both baseline diagnoses were related to persistence, the full ADHD diagnosis had a significantly stronger effect (χ2 (1) = 17.78, < p 0.001) than ADHD-NOS.
To test whether persistence was consistent across site, gender and age we included interactions of wave 1 diagnosis in the model (Model 2). There was no evidence of interactions for site and gender, but there was a significant interaction for baseline age (χ2 (2)=8.6, p <. 015). For those younger at baseline the strength of the prediction of ADHD-NOS was relatively weak, but for older children the presence of ADHD-NOS at baseline predicted risk of subsequent ADHD or ADHD-NOS that was similar to the prediction strength of ADHD itself (Table 2).
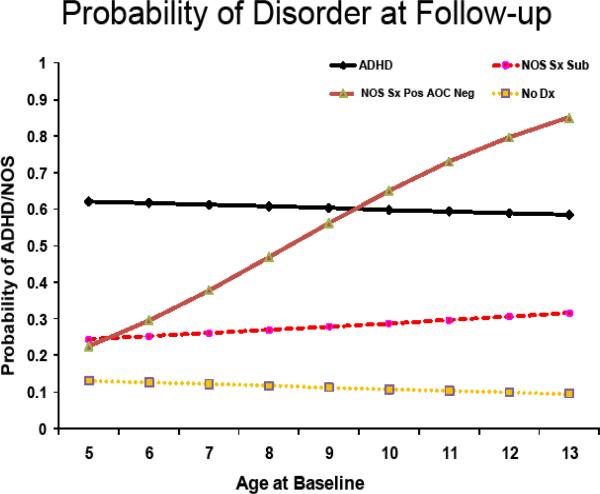
To clarify the nature of the age and NOS interaction we divided the NOS group into those who did not meet the necessary symptom criteria (Sx Sub; n=176) and those who met symptom criteria but not the age of onset criterion (Sx Pos, AOC Neg; n=56). We then re-estimated the interaction model presented in Table 2. Again there were no statistically significant interactions between the ADHD diagnostic groups and site and gender. The only statistically significant interaction was between age and the Sx Pos, AOC Neg group (β (SE) =0.42(0.14), OR = 1.52, p < .01). The interaction in Table 2 can be attributed to the group who did not meet criteria for ADHD due to the age on onset criteria (Figure1). We also explored psychopharmacological treatment effects. In this model both stimulants (β (SE) =1.74 (0.24), OR = 5.67, p < .0001) and other medications (β (SE) =1.12 (0.43), OR = 3.05, p < .01) were associated with higher persistence at follow up. The mean age of the 56 Sx Pos, AOC Neg cases (10.87; SE=0.31) was significantly higher than the mean age of the Sx Sub cases in the NOS group (9.38; SE=0.23) (t=3.44; < p .001). These two groups did not differ significantly by gender (66.6% vs. 56.8%). About half (48.6%) of the Sx Pos, AOC Neg cases were inattentive type, 36.9% were hyperactive-impulsive type, and 14.5% were combined type. There were a significantly higher proportion of inattentive cases than combined cases (p < .05). No significant differences were found in the proportion of hyperactive-impulsive and combined cases (p >.05).
Figure 1.
Relation of baseline age to probability of broadened ADHD+ (ADHD plus ADHD NOS) at follow-up broken down by ADHD; NOS symptom subthreshold (NOS Sx Sub); NOS symptom positive, negative age of onset criterion (NOS Sx Pos, AOC negative); and No diagnosis (No Dx) at baseline
Finally, we checked if the associations in Table 2 were influenced by the definition of the outcome as ADHD+. When the analyses were repeated using ADHD alone as outcome (excluding ADHD-NOS), we obtained similar findings, although the overall level of persistence was reduced (results from authors by request).
Discussion
Persistence of ADHD can be defined in several ways. In our assessment, we use a definition that includes not only the full diagnosis as per DSM-IV, but also those with ADHD-NOS. There is controversy in the field as to whether ADHD should be defined categorically or on a continuum. In the authors' opinion, both approaches are equally important and each one contributes to the conceptualization of the disorder. We recommend that clinicians, educators and parents attend to children with a history of ADHD who continue to have attention and impulse control problems, even when they fall short of a diagnosis. We found that fewer than half of the youth with baseline DSM-IV ADHD continued to have the full disorder one year later, but a majority of these youth had persistent disorder with a more inclusive decision rule that combines ADHD and ADHD NOS. ADHD defined more stringently at Time 1 was the strongest predictor of persistence, regardless of how persistence was defined. Furthermore, the combination of ADHD and ADHD-NOS diagnosis at wave 1 was strongly predictive of persistence at waves 2 and 3. Although full ADHD diagnosis was the strongest predictor, baseline ADHD-NOS was also a strong predictor that added information even after adjusting for full ADHD. ADHD-NOS children were 6 times more likely to have ADHD or ADHD-NOS diagnoses at follow-up. These findings are consistent with Faraone et al.'s3 conclusion, on a meta analysis of mostly clinical studies, that persistence of ADHD is greater when cases identified as presenting impairing symptoms such as ADHD in partial remission (a concept akin to ADHD-NOS) are included in the follow-up. These findings argue for considering the continuum of ADHD symptoms, even when categorical definitions are employed.
While ADHD is considered a chronic condition that theoretically should persist once diagnosed, the persistence rates obtained are lower than anticipated. To our knowledge, no other studies exist addressing this issue systematically in community samples, using DSM-IV diagnostic instruments, so comparison with similar studies is not possible. In general rates of persistence of ADHD in community samples tend to be considerably lower17,30–32 than those in clinical samples.3 Conceivably this finding is related to disorders in community samples being generally less severe (fewer symptoms and less impairment) than among subjects who seek clinical services; therefore the diagnosis of both ADHD and ADHD-NOS in community subjects is probably less stable and subject to minor fluctuations in both symptom levels or impairment. Community subjects that persist are in all likelihood those requiring services, but our previous report8 showed that few subjects with the diagnosis receive services, and among those, even fewer receive psychotropic medication which is an important component in the treatment of ADHD. Receiving medication was not an explanation for lower persistence. Paradoxically children receiving medication appear as more persistent in waves 2 and 3, implying not so much that medication was not working but that possibly that the more severe cases received treatment.
The significant interaction between ADHD-NOS and age at wave 1 suggests that persistence of ADHD-NOS is greater among older than younger children. It is possible that a subset of the older NOS cases are not diagnosed as full ADHD because DSM-IV symptom threshold or content are not appropriate to the child's age or developmental level.3 In our analyses this age interaction was better explained by cases with 6 or more inattention or hyperactivity-impulsivity symptoms with a later age of onset. It has been argued that the age of onset criterion should be revised and raised to at least 14 to 16 years.12 Presently the DSM 5 ADHD Workgroup considers changing this criterion to onset on or before 12 years. Other authors question the clinical utility and validity of the age of onset criterion.12,33 As was true in our findings, other research suggests that a sizeable proportion of those that meet symptom criteria but are classified as ADHD-NOS because their onset is after age 7, involve children with ADHD inattentive type. However, finding that 37 % of children that did not meet AOC were ADHD Hyperactive-Impulsive was unexpected given previous findings and lacks a clear explanation at present.34,35 In brief, although both research and clinical experience indicate that a lower symptom cut-off may be appropriate for older adolescents and adults, our findings lend even greater support to the argument made by clinicians and researchers alike that the onset criterion be raised to an older age regardless of the threshold.
As noted, differences in sampling, diagnostic criteria and ascertainment procedures make it difficult to compare findings across published studies. From the literature reviewed, it could not be determined whether other studies have considered context, site, or gender. Our study is the first to examine these issues and the results indicate that persistence of ADHD in children of similar ethnicity does not manifest differently across context and gender.
Psychosocial risk factors have been associated with ADHD persistence over time.5 Children in the South Bronx are exposed to more psychosocial risk factors than in Puerto Rico.18,19 However, contrary to our expectation, we did not find greater persistence of ADHD and ADHD-NOS among Puerto Rican children in the South Bronx than those in P.R.
At any time point girls were about half as likely to be diagnosed with ADHD or ADHD-NOS, however the pattern of persistence was the same for both genders. This finding is consistent with a previous community study indicating that males and females present similar risk factors and clinical profiles, including comorbidty,36 and that gender does not moderate the course of ADHD.15 Nevertheless, it is important to study the variables that may influence the likelihood of persistence or may be masking absence of gender differences in persistence.
A limitation of our study is that it can only address short-term persistence in relatively young children. The study bears replication with other populations over a longer time span. Also, direct teacher reports were not available. Our findings about school behaviors came from parents who may not have been fully cognizant of their child's behavior at school. The reliability for ADHD DISC diagnoses, as with similar diagnostic instruments, represents only fair to good agreement, and this reliability level may influence persistence findings.
Our findings however, have important implications. Persistence can be underestimated in longitudinal studies that measure and report only the full syndrome of ADHD. A subgroup of adolescents or adults that are true clinical cases but with a diagnosis of ADHD NOS may not be identified as persistent.3,37 While the diagnosis of ADHD NOS identifies cases that do not have full ADHD status, symptomatic persistence, that is, maintenance of subthreshold symptoms with impairment, is important to fully understand the progression and the outcomes of the disorder.3 Clinicians need to consider that impaired ADHD-NOS cases also need early identification and possibly treatment, given their persistence over time and potentially disabling consequences.
The DSM-IV ADHD-NOS category needs to be further studied and better operationalized in light of the current revisions considered for DSM 5 and other classification systems. Our criteria for ADHD-NOS not only qualify for the vague definition in DSM-IV, but highlight the need for more precise requirements (number of symptoms in the two dimensions and degree of impairment in two settings) that can be used to operationalize an NOS syndrome with greater specificity. Our results indicate that ADHD-NOS predict both ADHD and ADHD-NOS at follow up. This finding argues in favor of better operationalization of NOS syndromes in DSM 5, not only for ADHD but for other disorders as well.
ACKNOWLEDGMENTS
Drs. Bauermeister, Chavez, Ramirez, and Canino are with the Behavioral Sciences Research Institute, University of Puerto Rico, San Juan, PR; Dr. Bird is with the Department of Psychiatry, Columbia University; Dr. Shrout is with the Department of Psychology at New York University.
The primary study was supported by the National Institute of Mental Health through grants RO-1 MH56401 (Dr. Bird, principal investigator). Dr. Canino is supported by grant P60MD002261-01 from the National Center for Minority Health Disparities (Dr. Canino, principal investigator). Statistical expert: Patrick E. Shrout
References
- 1.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- 2.Spencer TJ, Biederman J, Mick E. Attention-deficit/hyperactivity disorder: diagnosis, lifespan, comorbidities, and neurobiology. Ambul Pediatr. 2007;7:73–81. doi: 10.1016/j.ambp.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 3.Faraone SV, Biederman J, Mick E. The age-dependent decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 2006;36:159–165. doi: 10.1017/S003329170500471X. [DOI] [PubMed] [Google Scholar]
- 4.Goodman SH, Hoven CW, Narrow WE, et al. Measurement of risk for mental disorders and competence in a psychiatric epidemiologic community survey: the National Institute of Mental Health Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) Study. Soc Psychiatry Psychiatr Epidemiol. 1998;33:162–173. doi: 10.1007/s001270050039. [DOI] [PubMed] [Google Scholar]
- 5.Biederman J, Faraone S, Milberger S, et al. A prospective 4-year follow-up study of attention-deficit hyperactivity and related disorders. Arch Gen Psychiatry. 1996;53:437–446. doi: 10.1001/archpsyc.1996.01830050073012. [DOI] [PubMed] [Google Scholar]
- 6.Hart EL, Lahey BB, Loeber R, Frick PJ. Developmental change in attention-deficit hyperactivity disorder in boys: a four-year longitudinal study. J Abnorm Child Psychol. 1995;23:729–749. doi: 10.1007/BF01447474. [DOI] [PubMed] [Google Scholar]
- 7.Taylor E, Sandberg S, Thorley G, Giles S. The epidemiology of childhood hyperactivity. Oxford University Press; London: 1991. [Google Scholar]
- 8.Bird HR, Shrout PE, Duarte CS, Shen S, Bauermeister JJ, Canino G. Longitudinal mental health service and medication use for ADHD among Puerto Rican youth in two contexts. J Am Acad Child Adolesc Psychiatry. 2008;47:879–889. doi: 10.1097/CHI.0b013e318179963c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hinshaw SP, Owens EB, Sami N, Fargeon S. Prospective follow-up of girls with attention-deficit/hyperactivity disorder into adolescence: Evidence for continuing cross-domain impairment. J Consult Clin Psychol. 2006;74:489–499. doi: 10.1037/0022-006X.74.3.489. [DOI] [PubMed] [Google Scholar]
- 10.Ramtekkar UP, Reiersen AM, Todorov AA, Todd RD. Sex and age differences in attention-deficit/hyperactivity disorder symptoms and diagnoses: implications for DSM-V and ICD-11. J Am Acad Child Adolesc Psychiatry. 2010;49:217–228. e211–213. [PMC free article] [PubMed] [Google Scholar]
- 11.Barkley RA, Fischer M, Smallish L, Fletcher K. The persistence of attention-deficit/hyperactivity disorder into young adulthood as a function of reporting source and definition of disorder. J Abnorm Psychol. 2002;111:279–289. [PubMed] [Google Scholar]
- 12.Barkley RA, Biederman J. Toward a broader definition of the age-of-onset criterion for attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 1997;36:1204–1210. doi: 10.1097/00004583-199709000-00012. [DOI] [PubMed] [Google Scholar]
- 13.Canino G, Alegria M. Psychiatric diagnosis - is it universal or relative to culture? J Child Psychol Psychiatry. 2008;49:237–250. doi: 10.1111/j.1469-7610.2007.01854.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lahey BB, Hartung CM, Loney J, Pelham WE, Chronis AM, Lee SS. Are there sex differences in the predictive validity of DSM-IV ADHD among younger children? J Clin Child Adolesc Psychol. 2007;36:113–126. doi: 10.1080/15374410701274066. [DOI] [PubMed] [Google Scholar]
- 15.Monuteaux MC, Mick E, Faraone SV, Biederman J. The influence of sex on the course and psychiatric correlates of ADHD from childhood to adolescence: a longitudinal study. J Child Psychol Psychiatry. 2010;51:233–241. doi: 10.1111/j.1469-7610.2009.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lahey BB, Pelham WE, Loney J, Kipp H, Ehrhardt A, Lee SS. Three-year predictive validity of DSM-IV attention deficit hyperactivity disorder in children diagnosed at 4–6 years of age. Am J Psychiatry. 2004;161:2014–2020. doi: 10.1176/appi.ajp.161.11.2014. [DOI] [PubMed] [Google Scholar]
- 17.Todd RD, Huang H, Todorov AA, et al. Predictors of stability of attention-deficit/hyperactivity disorder subtypes from childhood to young adulthood. J Am Acad Child Adolesc Psychiatry. 2008;47:76–85. doi: 10.1097/chi.0b013e31815a6aca. [DOI] [PubMed] [Google Scholar]
- 18.Bird HR, Canino GJ, Davies M, et al. A study of disruptive behavior disorders in Puerto Rican youth: I. Background, design, and survey methods. J Am Acad Child Adolesc Psychiatry. 2006a;45:1032–1041. doi: 10.1097/01.chi.0000227878.58027.3d. [DOI] [PubMed] [Google Scholar]
- 19.Bird HR, Davies M, Duarte CS, Shen S, Loeber R, Canino GJ. A study of disruptive behavior disorders in Puerto Rican youth: II. Baseline prevalence, comorbidity, and correlates in two sites. J Am Acad Child Adolesc Psychiatry. 2006b;45:1042–1053. doi: 10.1097/01.chi.0000227879.65651.cf. [DOI] [PubMed] [Google Scholar]
- 20.Bird HR, Shrout PE, Davies M, et al. Longitudinal development of antisocial behaviors in young and early adolescent Puerto Rican children at two sites. J Am Acad Child Adolesc Psychiatry. 2007;46:5–14. doi: 10.1097/01.chi.0000242243.23044.ac. [DOI] [PubMed] [Google Scholar]
- 21.Bravo M, Ribera J, Rubio-Stipec M, et al. Test-retest reliability of the Spanish version of the Diagnostic Interview Schedule for Children (DISC-IV) J Abnorm Child Psychol. 2001;29:433–444. doi: 10.1023/a:1010499520090. [DOI] [PubMed] [Google Scholar]
- 22.Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- 23.Jensen PS, Rubio-Stipec M, Canino G, et al. Parent and child contributions to diagnosis of mental disorder: are both informants always necessary? J Am Acad Child Adolesc Psychiatry. 1999;38:1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- 24.Schwab-Stone M, Fallon T, Briggs M, Crowther B. Reliability of diagnostic reporting for children aged 6–11 years: a test-retest study of the Diagnostic Interview Schedule for Children-Revised. Am J Psychiatry. 1994;151:1048–1054. doi: 10.1176/ajp.151.7.1048. [DOI] [PubMed] [Google Scholar]
- 25.Ribera JC, Canino G, Rubio-Stipec M, et al. The Diagnostic Interview Schedule for Children (DISC-2.1) in Spanish: reliability in a Hispanic population. J Child Psychol Psychiatry. 1996;37:195–204. doi: 10.1111/j.1469-7610.1996.tb01391.x. [DOI] [PubMed] [Google Scholar]
- 26.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed., text rev American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- 27.Research Triangle Institute . SUDAAN User's Manual. version 8.0 Research Triangle Park; NC: 2001. [Google Scholar]
- 28.Shadish WR, Steiner PM. A primer on propensity score analysis. Newborn Inf Nurs Rev. 2010;10:19–26. 2010. [Google Scholar]
- 29.Diggle PJ, Heagerty PJ, Liang KY, Zeger SL. Analysis of Longitudinal Data. Oxford University Press; New York, NY: 2002. [Google Scholar]
- 30.McGee R, Partridge F, Williams S, Silva PA. A twelve-year follow-up of preschool hyperactive children. J Am Acad Child Adolesc Psychiatry. 1991;30:224–232. doi: 10.1097/00004583-199103000-00010. [DOI] [PubMed] [Google Scholar]
- 31.Offord DR, Boyle MH, Racine YA, et al. Outcome, prognosis, and risk in a longitudinal follow-up study. J Am Acad Child Adolesc Psychiatry. 1992;31:916–923. doi: 10.1097/00004583-199209000-00021. [DOI] [PubMed] [Google Scholar]
- 32.Taylor E, Chadwick O, Heptinstall E, Danckaerts M. Hyperactivity and conduct problems as risk factors for adolescent development. J Am Acad Child Adolesc Psychiatry. 1996;35:1213–1226. doi: 10.1097/00004583-199609000-00019. [DOI] [PubMed] [Google Scholar]
- 33.Polanczyk G, Caspi A, Houts R, Kollins SH, Rohde LA, Moffitt TE. Implications of extending the ADHD age-of-onset criterion to age 12: results from a prospectively studied birth cohort. J Am Acad Child Adolesc Psychiatry. 2010;49:210–216. [PubMed] [Google Scholar]
- 34.Applegate B, Lahey BB, Hart EL, Biederman J, Hynd GW, Barkley RA. Validity of the age-of-onset criterion for ADHD: A report from the DSM-IV field trials. J Am Acad Child Adolesc Psychiatry. 1997;36:1211–1221. [PubMed] [Google Scholar]
- 35.Willoughby MT, Curran PJ, Costello EJ, Angold A. Implications of early versus late onset of attention-deficit/hyperactivity disorder symptoms. J Am Acad Child Adolesc Psychiatry. 2000;39:1512–1519. doi: 10.1097/00004583-200012000-00013. [DOI] [PubMed] [Google Scholar]
- 36.Bauermeister JJ, Shrout PE, Chavez L, et al. ADHD and gender: are risks and sequela of ADHD the same for boys and girls? J Child Psychol Psychiatry. 2007;48:831–839. doi: 10.1111/j.1469-7610.2007.01750.x. [DOI] [PubMed] [Google Scholar]
- 37.Barkley RA, Fischer M, Edelbrock CS, Smallish L. The adolescent outcome of hyperactive children diagnosed by research criteria: I. An 8-year prospective follow-up study. J Am Acad Child Adolesc Psychiatry. 1990;29:546–557. doi: 10.1097/00004583-199007000-00007. [DOI] [PubMed] [Google Scholar]