Abstract
The development of safe live, attenuated Salmonella vaccines may be facilitated by detoxification of its lipopolysaccharide. Recent characterization of the lipid A 1-phosphatase, LpxE, from Francisella tularensis allowed us to construct recombinant, plasmid-free strains of Salmonella that produce predominantly 1-dephosphorylated lipid A, similar to the adjuvant approved for human use. Complete lipid A 1-dephosphorylation was also confirmed under low pH, low Mg2+ culture conditions, which induce lipid A modifications. lpxE expression in Salmonella reduced its virulence in mice by five orders of magnitude. Moreover, mice inoculated with these detoxified strains were protected against wild-type challenge. Candidate Salmonella vaccine strains synthesizing pneumococcal surface protein A (PspA) were also confirmed to possess nearly complete lipid A 1-dephosphorylation. After inoculation by the LpxE/PspA strains, mice produced robust levels of anti-PspA antibodies and showed significantly improved survival against challenge with wild-type Streptococcus pneumoniae WU2 as compared to vector-only immunized mice, validating Salmonella synthesizing 1-dephosphorylated lipid A as an antigen delivery system.
Keywords: Attenuated Salmonella, Dephosphorylation of Lipid A, LpxE, TLR4, PspA
Introduction
Recombinant attenuated Salmonella vaccines (RASVs) can deliver antigens from a variety of different pathogens, generating a range of immune responses including serum antibodies, mucosal IgA and a panoply of cell-mediated immune responses at local and distal sites (1–4). However, one problematic issue in the field has been that while candidate RASVs are adequately attenuated in animal models, when administered to humans, these vaccines can produce unwanted side effects, including fever and intestinal distress (5, 6). One possible cause of this fever is the lipid A component of lipopolysaccharide (LPS), also known as endotoxin (7). This could be of particular concern when using live strains exhibiting regulated delayed lysis in vivo to deliver a bolus of recombinant antigen and/or to confer complete biological containment (8).
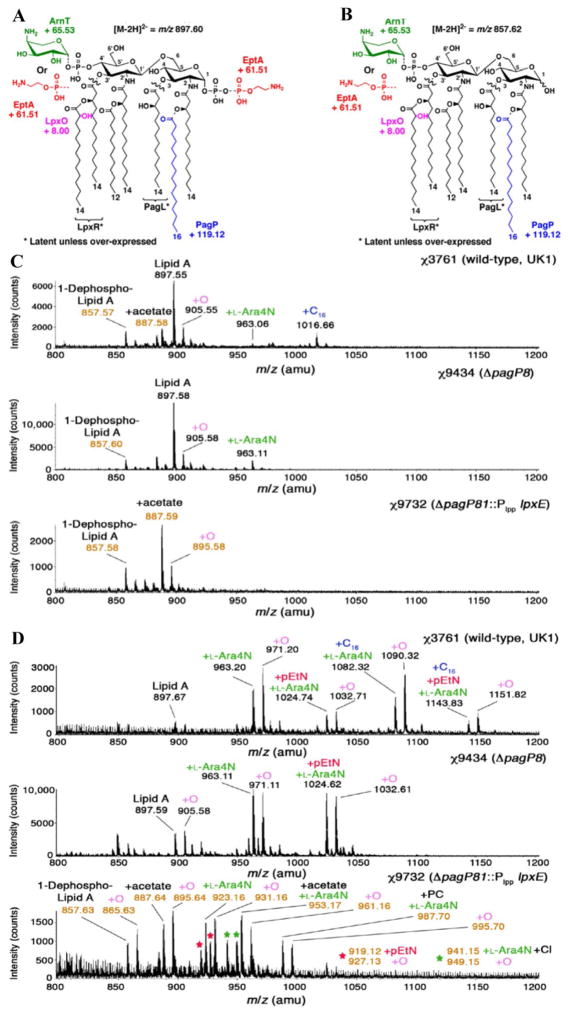
LPS, the major surface membrane component present in almost all gram-negative bacteria, consists of lipid A, a core oligosaccharide, and a highly variable and immunogenic O-antigen polysaccharide. Lipid A (Fig. 1A) is responsible for the toxicity of LPS (9, 10). Lipid A is detected by the toll-like receptor 4 (TLR4)/myeloid differentiation factor 2 (MD-2) receptor complex of the mammalian innate immune system (11–17). The structure-activity relationship of lipid A has been extensively studied, and factors governing its immunological activity have been identified. The total number and length of the acyl chains and two phosphate groups at the 1 and 4′ positions are critical factors for full lipid A activation of human TLR4/MD-2 (18–20). Hexa-acylated E. coli lipid A with both 1 and 4′ phosphate moieties and acyl chains from 12 to 14 carbons in length has optimal pro-inflammatory activity, whereas altering the number or length of the attached fatty acids or altering the charge of lipid A can reduce the magnitude of the signal (18, 19, 21). The recent TLR4-MD-2-LPS crystal structure shows that the 1- and 4′-phosphate groups interact with a cluster of positively charged residues from dimeric TLR4 and MD-2 (20). Removal of the 1- or 4′-phosphate not only weakens the ligand affinity but may also induce structural rearrangement of the TLR4 MD-2 multimer (20).
Figure 1.
Lipid A structure of wild-type and lpxE-expressing Salmonella. (A) Covalent modifications of Salmonella lipid A. LpxR and PagL catalyze the removal of the 3′-acyloxyacyl and the 3-hydroxymyristoyl chains from lipid A, respectively, although these modifications are not seen in laboratory growth conditions. The lipid A species can be identified by ESI-MS in the negative ion mode, with unmodified lipid A as the [M-2H]2-peak at m/z 897.60. Various modifications shift the peak by the indicated m/z values. The addition of palmitate (+C16) to the 2 position R-3-hydroxymyristoyl chain catalyzed by PagP is indicated in blue. Other covalent lipid A modifications include the hydroxylation of the 3′ secondary myristoyl chain by LpxO (+O, pink) the addition of L-Ara4N to the 4′ phosphate by ArnT (+L-Ara4N, green), and the addition of pEtN to the 1 phosphate by EptA (+pEtN, red). (B) structure of 1-dephosphorylated lipid A. Heterologous expression of the F. tularensis lpxE leads to nearly quantitative 1-dephosphorylation of all Salmonella lipid A species, specifically shifting the lipid A [M-2H]2− peak by m/z −39.98. (C) Lipid A profiles from ESI-MS analysis of χ3761(wild-type UK-1), χ9434(ΔpagP8), and χ9732(ΔpagP81::Plpp lpxE), grown in LB. Lipid A peaks are indicated with black m/z values, while 1-dephospho-lipid A peaks are indicated with orange m/z values. In each case, peaks labeled with +O are consistent with hydroxylated versions of the adjacent peak. For 1-dephospho-lipid A, peaks consistent with non-covalent acetate adducts are also detected. (D) ESI-MS analysis of lipid A purified from mutant strains χ3761(parent strain), χ9434 (ΔpagP8) and χ9732 (ΔpagP81::Plpp lpxE). Strains were grown at pH 5.8 in N-medium containing 10 μM Mg2+ at 37°C.
Monophosphoryl lipid A (MPL) is used clinically as a vaccine adjuvant in Europe and Australia (22) and was recently approved for use in the United States. As an adjuvant, MPL improves vaccine efficacy, induces dendritic cell maturation, induces primarily a Th1 response, indirectly reduces the threshold for activation of Th1 cells, and upregulates MHC class II molecules, CD80, and CD86 (23–26). Lipid A activates both the TLR4–TRIF and TLR4–MyD88 pathways, while MPL selectively activates the TLR4–TRIF signaling pathway, leading to significantly lower secretion of pro-inflammatory cytokines, such as IL-6, IL-1β and IFN-γ than wild-type lipid A, but robust induction of G-CSF, MCP-1, and IP-10 (15). The MPL vaccine adjuvant therefore maintains or enhances immuno-stimulatory benefits, but possesses reduced toxicity (21).
LpxE, an inner membrane phosphatase from Francisella tularensis subspecies novicida, strain Utah 112, can selectively remove the 1-phosphate group of lipid A in living cells of E. coli and Salmonella (Fig. 1B) (27), generating a close analog of MPL that remains covalently linked to LPS. In previous studies, lpxE was expressed from a multicopy plasmid, a method not ideal for use in vaccine strains due to potential stability issues and because target antigen genes are typically expressed from multicopy plasmids. In this study, we identified a unique chromosomal location for lpxE insertion that supports levels of lpxE transcription to provide levels of LpxE adequate for nearly complete 1-dephosphorylation of the lipid A in Salmonella. In addition, we demonstrate that lpxE expression from this chromosomal location in live Salmonella is attenuating. Our ultimate goal is to modify live attenuated Salmonella vaccine strains to produce dephosphorylated lipid A as an additional safety feature. Therefore, we introduced our optimal lpxE construct into an attenuated Salmonella strain. We found that chromosomal lpxE expression in a vaccine strain carrying additional attenuating deletions does not result in loss of efficacy when used to deliver a heterologous antigen.
Materials and Methods
Bacterial strains, plasmids, media, and growth conditions
S. Typhimurium cultures were routinely grown at 37°C in LB broth (28) or LB agar with or without 0.1% arabinose, nutrient broth (Difco) or in N minimal medium (29), pH 5.8, supplemented with 0.1% casamino acids, 38 mM glycerol and 10 μM MgCl2. DAP was added to a concentration of 50 μg/ml for the growth of Δasd strains (30). LB agar containing 5% sucrose was used for sacB gene-based counter selection in allelic exchange experiments. S. pneumoniae WU2 was cultured on brain heart infusion agar containing 5% sheep blood or in Todd-Hewitt broth plus 0.5% yeast extract. MOPS minimal medium (31) with/without 10 μg/ml p-aminobenzoic acid was used to confirm the phenotype of ΔpabA ΔpabB mutants.
Plasmids and mutant strain construction
DNA manipulations were carried out as described (32). Transformation of E. coli and S. enterica was performed by electroporation. Transformants were selected on LB agar plates containing appropriate antibiotics. Selection for Asd+ plasmids were done on LB agar plates. The primers used in this paper are listed in Supplemental Table 1. For construction of the ΔpagL7 mutation, which deletes the entire pagL open reading frame, the S. Typhimurium χ3761 (33) genome was used as template for cloning. A 350-bp DNA fragment containing the region upstream of the pagL gene (from ATG start codon, but not including ATG) was PCR amplified using primers PagL-Del1 and PagL-SbfI2 (Supplemental Table 1); another 350-bp DNA fragment containing the region downstream of pagL gene (from TAA stop codon, but not including TAA) was PCR amplified using primers PagL-SbfI3 and pagL-del4. The two PCR fragments were purified in agarose gels, combined at a 1:1 molar ratio and joined by PCR using primers pagL-Del1 and pagL-Del4. The resulting PCR product was digested with KpnI and XmaI and ligated to KpnI-XmaI-digested pRE112 (34), resulting in plasmid pYA4284. The same strategy is used to construct pYA4288 and pYA4287, which were used to delete the entire pagP and lpxR open reading frames, respectively. There is an SbfI site at the point of each deletion in all three plasmids. The Plpp promoter from E. coli was amplified by Plpp-FSbfI and Plpp-R. The lpxE gene from pXYW-1 (pACYC184 carrying a 2.5-kb F. tularensis genomic DNA fragment containing lpxE) (27) was amplified using primers LpxE-F1 and LpxE-RsbfI. The two PCR fragments were purified from agarose gels, combined at a 1:1 molar ratio and joined by PCR using primers Plpp-FSbfI and LpxE-RSbfI. The resulting PCR product was digested with SbfI and ligated with SbfI-digested, shrimp alkaline phosphatase-treated pYA4284 (ΔpagL7), pYA4288 (ΔpagP8), or pYA4287 (ΔlpxR9). Candidate plasmids were screened by PCR to verify the orientation of the insert. The resulting plasmids were pYA4291 (ΔpagL72::Plpp lpxE), pYA4473 (ΔpagP82::Plpp lpxE), and pYA4474 (ΔlpxR92::Plpp lpxE). The same strategy was used to construct suicide plasmids pYA4294, pYA4295 and pYA4296 for insertion of Plpp lpxE (codon-optimized) (Table 1).
Table 1.
Strains and plasmids used in this work.
| Strain or plasmid | Description (phenotype information)a | Source or derivative |
|---|---|---|
| S.Typhimurium | ||
| χ3761 | Wild type, UK-1 (Virulent parent strain) | (33) |
| χ9437 | ΔpagL72::Plpp lpxE (native lpxE) | χ3761 |
| χ9701 | ΔpagP82::Plpp lpxE (native lpxE) | χ3761 |
| χ9703 | ΔlpxR92::Plpp lpxE (native lpxE) | χ3761 |
| χ9440 | ΔpagL71::Plpp lpxE (codon-optimized lpxE) | χ3761 |
| χ9732 | ΔpagP81::Plpp lpxE (codon-optimized lpxE) (produces 1-monophosphoryl lipid A) | χ3761 |
| χ11092 | ΔlpxR91::Plpp lpxE (codon-optimized lpxE) | χ3761 |
| χ9704 | ΔpagL7 ΔpagP82::Plpp lpxE ΔlpxR9 | χ3761 |
| χ9705 | ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9 (produces 1-monophosphoryl lipid A) | χ3761 |
| χ9434 | ΔpagP8 | χ3761 |
| χ9485 | ΔpagL7 ΔpagP8 ΔlpxR9 | χ3761 |
| Vaccine strains | ||
| χ9241 | ΔpabA1516 ΔpabB232 ΔasdA16 ΔaraBAD23 ΔrelA198::araC PBAD lacI TT (attenuated vaccine strain) | (44) |
| χ9844 | ΔpagP8 | χ9241 |
| χ9845 | ΔpagP81::Plpp lpxE (produces 1-monophosphoryl lipid A) | χ9241 |
| χ9846 | ΔpagL7 ΔpagP8 ΔlpxR9 | χ9241 |
| χ9881 | ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9 (produces 1-monophosphoryl lipid A) | χ9241 |
| E. coli | ||
| χ7232 | endA1 hsdR17 (rK−, mK+) supE44 thi-1 recA1 gyrA relA1 Δ(lacZYA-argF) U169 λ pir deoR (φ80dlac (lacZ)M15) | (35) |
| χ7213 | thi-1 thr-1 leuB6 glnV44 tonA21 lacY1 recA1 RP4-2-Tc::Mu λ pir ΔasdA4 Δzhf-2::Tn10 | (35) |
| S. pneumoniae WU2 | Wild-type virulent, encapsulated type 3 | (46) |
| Plasmids | ||
| pRE112 | sacB mobRP4 R6K ori CmR | (34) |
| pYA4284 | pagL7 deletion | pRE112 |
| pYA4288 | pagP8 deletion | pRE112 |
| pYA4287 | lpxR9 deletion | pRE112 |
| pYA4291 | pagL deletion, and Plpp lpxE (native) insertion | pRE112 |
| pYA4473 | pagP deletion, and Plpp lpxE (native) insertion | pRE112 |
| pYA4474 | lpxR deletion, and Plpp lpxE (native) insertion | pRE112 |
| pYA4528 | Plpp lpxE insertion into downstream of bcfH gene | pRE112 |
| pYA4294 | pagL deletion, and Plpp lpxE (codon-optimized) insertion | pRE112 |
| pYA4295 | pagP deletion, and Plpp lpxE (codon-optimized) insertion | pRE112 |
| pYA4296 | lpxR deletion, and Plpp lpxE (codon-optimized) insertion | pRE112 |
| pXYW-1 | lpxE in pWSK29a | (27) |
| pYA3493 | Plasmid Asd+; pBRori β-lactamase signal sequence for periplasmic secretion | (43) |
| pYA4088 | 852 bp DNA encoding the α-helical region of PspA from amino acid 3 to amino acid 285 in pYA3493 | (44) |
Strains carrying lpxE produce some level of 1-monophosphoryl lipid A. See text for details.
The mutations were introduced into S. Typhimurium by allelic exchange by conjugation with E. coli strain χ7213 (35) harboring suicide vectors, pYA4284, pYA4288, pYA4287 to generate the ΔpagL7, ΔpagP8 and ΔlpxR9 mutations, respectively. Plasmids pYA4291, pYA4473 and pYA4474 were used to generate strains χ9437 (ΔpagL72::Plpp lpxE), χ9701 (ΔpagP82::Plpp lpxE), and χ9703 (ΔlpxR92::Plpp lpxE), respectively. Plasmids pYA4294, pYA4295 and pYA4296 were used to generate χ9440 (ΔpagL71::Plpp lpxE), χ9732 (ΔpagP81::Plpp lpxE) and χ11092 (ΔlpxR91::Plpp lpxE), respectively.
Some mutations were also introduced into the attenuated S. Typhimurium vaccine strain χ9241 using the same methods. The presence of the ΔpabA1516 and ΔpabB232 mutations in strain χ9241 were verified by the inability of the strains to grow in MOPS minimal medium without p-aminobenzoate. The presence of the ΔasdA16 mutation was confirmed by inability to grow in media without DAP and by PCR. The ΔaraBAD23 mutation was verified by a white colony phenotype on MacConkey agar supplemented with 1% arabinose and by PCR. LPS profiles of Salmonella strains were examined by previously described methods (36).
Isolation of lipid A
Strains were grown in LB or N media modified to 10 μM Mg2+ and pH 5.8 (37). Typically, 200 mL cultures were inoculated from overnight cultures of like media to A600 0.02 and grown to A600 0.8–0.9 for LB and 0.4–0.6 for N medium. The cells were pelleted by centrifugation at 3,500 × g for 20 min at 4°C, washed with phosphate-buffered saline (PBS), and pelleted again. The cell pellets were resuspended in 20 mL of PBS and transferred to chloroform-safe Nalgene bottles. Chloroform and methanol were added to a final ratio of 1:2:0.8 (chloroform:methanol:PBS, v/v), forming a single-phase Bligh/Dyer mixture (38). The cell suspensions were agitated by stirring for 1 h at room temperature, followed by centrifugation at 2,500 × g for 20 min. The supernatants containing phospholipids were discarded, and the pellets were resuspended by vortexing in 40 mL of a single-phase Bligh/Dyer mixture and transferred to a 50-mL Pyrex tube with a Teflon-lined cap. The tubes were centrifuged again and the supernatants discarded. The air-dried pellets were resuspended in 25 mL of 50 mM sodium acetate pH 4.5 by vortexing and probe sonication (39). After sonication, the pH was adjusted to 4.5 with acetic acid if necessary. The tubes were then placed in boiling water for 30 min to release the lipid A from the LPS. After cooling and vortexing, the solutions were transferred to chloroform-safe Nalgene bottles. Chloroform and methanol were added to a final ratio of 2:2:1.8 (chloroform:methanol:aqueous sodium acetate, v/v), forming a two-phase Bligh/Dyer mixture (38). The mixture was vigorously shaken to extract the lipid A, and the bottles were centrifuged at 2,500 × g for 20 min at 20°C to separate the two phases. The lower (chloroform) phase from each bottle was carefully removed to a round bottom flask and dried down on a rotary evaporator. The remaining upper phase was extracted again with fresh pre-equilibrated lower phase from a two-phase Bligh/Dyer mixture (2:2:1.8, chloroform:methanol:PBS, v/v). After centrifugation, the lower phase was added to the same flask and dried down again. The dried lipid A species were redissolved in chloroform:methanol (2:1, v/v) by vortexing and sonication, transferred to a glass tube, dried down, sealed with a Teflon-lined cap, and stored at −80°C.
Mass spectrometry (MS) of lipid A
Isolation of lipid A is described in SI text. Spectra were acquired on an ABI QSTAR XL quadropole time-of-flight tandem mass spectrometer (ABI/MDS-Sciex, Toronto, Canada), equipped with an electrospray ionization (ESI) source. Spectra were acquired in the negative-ion mode and typically were the accumulation of 60 scans collected from m/z 200–2000. The dried lipid A species were prepared for MS by dissolving them in 1.5 mL of chloroform:methanol (2:1, v/v). An aliquot of 10–20 μL was diluted 10-fold in the same solvent and supplemented with 2 μL piperidine (final concentration 1%, v/v). Immediately after preparation, each sample was directly infused into the ion source at 5–6 μL/min. The negative ion ESI was carried out at −4200 V. Data acquisition and analysis were performed using the Analyst QS software (ABI/MDS-Sciex).
LPS purification and LPS concentration determination
For tissue culture experiments, LPS was prepared from 20 ml of bacterial culture with Tri-reagent (Sigma) as described previously (40). The samples were repurified using the DOC-phenol method to remove trace protein (41). LPS preparations were quantitated using the Kdo method according to published procedures (42). Briefly, 3-deoxy-D-manno-octulosonic acid (Kdo) is released from LPS after 0.5 M H2SO4 hydrolysis. Each LPS molecule contains 3 Kdo moieties. After determining the Kdo concentration, we then calculated the LPS concentration and then diluted the samples to the concentration appropriate for each experiment.
Determination of virulence in mice
Seven week old, female BALB/cmice were obtained from the Charles River Laboratories (Wilmington, MA). All animal procedures were approved by the Arizona State University Animal Care and Use Committees. Mice were acclimated for 7 days after arrival before starting the experiments. For determination of the 50% lethality dose (LD50), bacteria were grown statically overnight at 37°C in LB, diluted 1:50 into fresh LB media, and grown with aeration (180 rpm) at 37°C. When the cultures reached an OD600 = 0.8–0.9, they were harvested by room temperature centrifugation at 4,000 rpm, washed once, and normalized to the required inoculums density in BSG by adjusting the suspension to the appropriate OD600 value. Groups of five mice each were infected orally with 20 μL containing various doses of S. Typhimurium χ3761 or its derivatives, ranging from 1 × 103 CFU to 1 × 109 CFU. Oral infections were performed using a 20 μL pipette. Animals were observed for 4 weeks post infection, and deaths were recorded daily. Surviving mice in some groups were challenged with 1 × 109 CFU of wild type strain χ3761. Animals were observed for 4 weeks post-infection and deaths were recorded daily.
To evaluate colonization, mice were orally inoculated with 20 μl of BSG containing 1×109 CFU of each strain. At days 3 and 6 after inoculation, three animals per group were euthanized and Peyer’s patches (PP), spleen and liver samples were collected. Each sample was homogenized in BSG at a final volume of 1 ml. Dilutions of 10−1 to 10−6 (depending on the tissue) were plated onto MacConkey and LB agar to determine the number of viable bacteria. Twenty colonies from each animal were randomly selected to confirm genotypic markers by PCR. Each experiment was performed twice.
Cell line culture and LPS stimulation
The murine macrophage cell line RAW264.7 (ATCC, Rockville, MD) was maintained in DMEM (Invitrogen, San Diego, CA) supplemented with 10% FBS and 100 μg/mL each of gentamicin and penicillin. The human monocytic leukemia cell line Mono Mac 6 (MM6) (Lonza, Germany) was cultured in RPMI1640 containing sodium bicarbonate (2 g/L), insulin (10 μg/mL) and oxalacetic acid (1 mM), 100 μg/mL each of gentamicin and penicillin, glutamine (2 mM), nonessential amino acids for minimum essential medium (MEM; 1% v/v), sodium pyruvate (1 mM), folic acid (40 μg/mL) and 15% FBS. Cells were seeded in 96 well microtiter plates (2.5×105/well) in 150 μL of the above medium and cultured at 37°C with 5% CO2. After 6 h, various dilutions of LPS preparations were added in 16 μL (10 × dilution). 24 h later, culture supernatants were collected, centrifuged to remove contaminating cells and stored at −80°C until determination of cytokine content. All experiments were performed at least twice.
Cytokine assay
Cytokine concentrations (human IL6, mouse TNF-α or mouse multiple cytokines) were determined using the Bio-Plex Protein Array System (Bio-Rad) according to the manufacturer’s recommendations. Serum samples were diluted with specific serum dilution buffer (Bio-Rad). Peritoneal washes were centrifuged at 4,000 rpm for 10 min and the supernatants were assayed for cytokines. Samples were incubated with antibody-coupled beads for 30 min with continuous shaking. The beads were washed 3 times with 100 μL wash buffer to remove unbound protein and then incubated with biotinylated detection cytokine-specific antibody for 30 min with continuous shaking. The beads were washed three times and incubated with streptavidin-phycoerythrin for 10 min after incubation. The beads were washed three times in washing buffer, resuspended in 125 μL assay buffer, and the constituents of each well of microtiter plate were drawn up into the flow-based Bio-Plex suspension Array System. Cytokine concentrations were automatically calculated by Bio-Plex Manager software by using a standard curve derived from a recombinant cytokine standard, two readings were made on each bead set.
Rabbit ileal loop experiment
New Zealand White rabbits were fasted overnight and then anesthetized with isoflurane through an endotracheal tube, and the ileum was exposed and then ligated into several loops 3 to 5 cm long using 1-cm spacers. S. Typhimurium strains were injected into separate loops in a volume of 1 ml at a titer of 1 × 109 CFU.LB broth was injected into one of the loops as a control. The abdominal musculature was closed using 3-0 chromic gut sutures, and the skin was closed with 3-0 ethilon sutures. Rabbits were maintained in a thermal blanket at 37°C. After 8 h, each rabbit was euthanized with an overdose of sodium pentobarbital. The abdomen was reopened, and the fluid within the ligated loops was collected, the volume measured, and the bacterial content enumerated. The loops were fixed in 10% formalin and subjected to H&E staining histopathological examination.
Antigen preparation
rPspA protein was purified as described (43). S. Typhimurium LPS was obtained from Sigma. The rPspA clone was kind gift from Dr. Susan Hollingshead at the University of Alabama at Birmingham.
SDS-PAGE and western blot analyses
Protein samples were boiled for 5 min in loading buffer and separated by SDS-PAGE. For western blotting, proteins separated by SDS-PAGE were transferred electrophoretically to nitrocellulose membranes. The membranes were blocked with 3% skim milk in 10 mM Tris-0.9% NaCl (pH 7.4) and incubated with rabbit polyclonal antibody specific for PspA (44) or anti-GroEL (Sigma, St. Louis, MO) antibodies. The secondary antibody was an AP-conjugated goat anti-rabbit immunoglobulinG (IgG) (Sigma). Immunoreactive bands were detected by the addition of BCIP/NBT solution (Sigma). The reaction was stopped after 2 min by washing with large volumes of deionized water several times.
Immunogenicity of vaccine strains in mice
RASV strains were grown statically overnight in LB broth with 0.1% arabinose at 37°C. The following day, 2 mL of the overnight culture was inoculated into 100 ml of LB broth with 0.1% arabinose and grown with aeration at 37°C to an OD600 of 0.8 to 0.9. Cells were harvested by room temperature centrifugation at 4,000 rpm for 15 min and the pellet resuspended in 1 mL of BSG. Mice (n = 13 per group) were orally inoculated with 20 μl of BSG containing 1×109 CFU of each strain on day 0 and boosted at 5 weeks with the same dose of the same strain. Blood was obtained by mandibular vein puncture at biweekly intervals. Following centrifugation, the serum was removed from the whole blood and stored at −20°C.
Enzyme-linked immunosorbent assay (ELISA)
ELISA was used to assay serum antibodies against S. Typhimurium LPS, rPspA and whole cell bacterial suspensions (1 × 109 CFU/ml)as previously described (45). Color development(absorbance) was recorded at 405 nm using an automated ELISA plate (model SpectraMax M2e; Molecular Devices, CA). Absorbance readings 0.1 higher than PBS control values were considered positive reactions.
Pneumococcal challenge
We assessed the protective efficacy of the attenuated Salmonella expressing pspA at week 8 by intraperitoneal challenge of immunized mice with 4×104 CFU of S. pneumoniae WU2 (46) in 200 μl of BSG (47) The LD50 of S. pneumoniae WU2 in BALB/c mice (n = 13 per group) was 2×102 CFU by intraperitoneal administration (data not shown). Challenged mice were monitored daily for 30 days.
Statistical analysis
Numerical data were expressed as means ± SEM. A two way ANOVA analysis followed by Bonferroni’s multiple comparison test was used to evaluate differences in antibody titer data. One way ANOVA analysis followed by Dunnett’s multiple comparison test was used to evaluate cytokine level and colonization for multiple comparisons among groups. The median lethal dose (LD50) was estimated using a probit analysis based on the XLSTAT. The Kaplan-Meier method was used for survival, and differences were analyzed by the log-rank sum test. All analyses were performed using GraphPad PRISM 5.0. P < 0.05 was considered statistically significant.
Results
Francisella LpxE can efficiently remove the 1-phosphate group from Salmonella lipid A
To evaluate the effect of chromosomally-expressed lpxE in Salmonella, we inserted F. tularensis lpxE under constitutive transcriptional control of the strong E. coli promoter Plpp into several different positions of the Salmonella chromosome. Lipid A was isolated from each strain after mild acid hydrolysis at pH 4.5 to cleave the Kdo-lipid A linkage (48) and subjected to electrospray ionization mass spectrometry (ESI-MS). Consistent with previous reports, the lipid A of the wild-type strain contains predominantly hexa-acylated lipid A (Fig. 1A and supplemental Fig. 1A, [M-2H]2− species near m/z 897.6). Our initial results indicated that the amount of LpxE synthesized in each strain was not adequate to 1-dephosphorylate more than 50% of the lipid A in the cell (Fig. 1B and Supplemental Fig. 1A, [M-2H]2− species with m/z near 857.6). To reduce the levels of inflammatory lipid A further and increase the levels of 1-dephospho-lipid A, the lpxE sequence was codon-optimized for high-level expression in Salmonella. Three mutant strains expressing codon-optimized Plpp lpxE were constructed and designated χ9440 (ΔpagL71::Plpp lpxE), χ9732 (ΔpagP81::Plpp lpxE) and χ11092 (ΔlpxR91::Plpp lpxE). ESI-MS of the lipid A for the mutant strains demonstrated that codon-optimization led to more efficient lipid A 1-dephosphorylation than in isogenic strains expressing the native lpxE sequence (Supplemental Fig. 1B). The level of Plpp lpxE expression was dependent on the chromosomal location, because only strain χ9732 (ΔpagP81::Plpp lpxE) produced lipid A that was essentially completely 1-dephosphorylated (Fig. 1B and Supplemental Fig. 1B, [M-2H]2− species near m/z 857.6). Based on these results, the pagP81::Plpp lpxE cassette was chosen for further evaluation.
The structure of Salmonella lipid A is nearly identical to that of E. coli (9, 10). However, Salmonella lipid A can be covalently modified in response to environmental conditions. For example, the 4′-phosphate group can be covalently modified with a 4-amino-4-deoxy-L-arabinose (L-Ara4N) residue, and the 1′-phosphate can be modified with a phosphoethanolamine moiety in response to specific environmental signals (9, 10). In addition, the fatty acyl chains can be modified by hydroxylation of the 3′ secondary myristate chain by LpxO, the addition of a secondary palmitate chain at the 2-position by PagP, or the removal of the 3 or 3′ acyl chain(s) by PagL or LpxR, respectively (Fig. 1A) (10, 49). To evaluate the effect of deleting pagL, pagP and lpxR genes in vitro and in the presence or absence of lpxE, we constructed the following mutant strains: χ9434 (ΔpagP8) and χ9732 (ΔpagP81::Plpp lpxE), and triple mutant strains: χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9). As expected, the ΔpagP strains χ9434 (ΔpagP8) and χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) lack the palmitate-containing peak seen in the wild-type strain χ3761 (Fig. 1C, [M-H]− species near m/z 1016.66, and data not shown). Because LpxR and PagL are latent in normal laboratory growth conditions, no other differences were seen for χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) compared to χ3761. In χ9732 (ΔpagP81::Plpp lpxE), the four major peaks detected are consistent with MPL (m/z 857.6), LpxO-modified MPL (m/z 865.5) and their acetate adducts (m/z 887.6 and 895.6, respectively) (Fig. 1C). The lipid A structures in strains χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) are similar to those in strains χ9434 (ΔpagP8) and χ9732 (ΔpagP81::Plpp lpxE), respectively. The small MPL peak (m/z 857.6) seen in strains χ3761 (wild-type), χ9434 (ΔpagP8), and χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) is due to minor chemical 1-dephosphorylation as a result of the mild acid hydrolysis step employed to liberate lipid A from LPS by cleavage of the Kdo-lipid A linkage.
The phoPQ and pmrAB two-component systems play a key role in controlling the remodeling of lipid A (10). The phoPQ regulon (which includes pmrAB) is turned on during invasion of host tissues in response to conditions that can include low pH and/or a low concentration of Mg2+ (10) or sub-lethal concentrations of cationic peptides (50, 51). Among other modifications induced, the addition of phosphoethanolamine (pEtN) to the 1-phosphate by EptA is upregulated (10). It is possible that these PhoPQ-regulated modifications may interfere with the action of LpxE.
To evaluate whether LpxE can efficiently remove the 1-phosphate group from lipid A when the phoPQ regulon is induced, strains were grown in media at low pH and low Mg2+ concentration, conditions that upregulate phoPQ (52), and the lipid A analyzed. ESI-MS data for χ9732 (ΔpagP81::Plpp lpxE) showed that LpxE can efficiently remove the 1-phosphate from lipid A when the phoPQ regulon is activated (Fig. 1D). In addition to the major peaks seen in cells grown on LB medium, the peaks observed in the low pH, low Mg2+ medium are consistent with 1-dephospho-lipid A, modified by 4-amino-4-deoxy-L-arabinose (L-Ara4N, Fig. 1D). Lipid A modification by ArnT (adding L-Ara4N to the 4′ phosphate) and by EptA (adding phosphoethanolamine to the 1-phosphate) each take place on the periplasmic surface of the inner membrane, the same location as 1-dephosphorylation by LpxE (10). The prevalence of L-Ara4N-modified 1-dephospho-lipid A species suggests that either LpxE acts prior to lipid A modification by ArnT or efficiently utilizes modified lipid A as a substrate. More importantly, despite the upregulation of EptA, LpxE clearly acts prior to addition of pEtN to the 1-position, suggesting LpxE will function under the range of conditions experienced in the host.
Salmonella with 1-dephosphorylated lipid A is attenuated without loss of colonization efficiency
We next determined the role of the individual mutations in mouse virulence (Table 2). The oral 50% lethal dose (LD50) of wild-type strain, χ3761, 1.0 × 104 CFU, was similar to that previously observed (53). The ΔpagP8 mutant strain χ9434 (ΔpagP8) had the same oral LD50 as χ3761 (wild-type), extending the previous observation that a pagP mutant is unaltered for virulence in mice when introduced by the intraperitoneal route (54). The LD50 of χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) was increased 10-fold compared to the wild-type strain. However, the LD50 of χ9732 (ΔpagP81::Plpp lpxE) was approximately 105-fold greater than χ3761 (wild-type), although at the highest doses we observed mild to severe clinical manifestations of disease (scruffy coat, lethargy) from which some mice recovered (Table 2). Strain χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) was completely avirulent, and no disease symptoms were observed even at the highest dose, indicating an LD50 value at least 105-fold greater than the wild type.
Table 2.
Mouse survival after infection with the indicated Salmonella strains.
| Dose | χ3761 wild-type |
χ9434 ΔpagP8 |
χ9732e ΔpagP81::PlpplpxE (m-lipid A)a |
χ9485 ΔpagL7 ΔpagP8 ΔlpxR9 |
χ9705e ΔpagL7 ΔpagP81::PlpplpxE ΔlpxR9 (m-lipid A) |
|---|---|---|---|---|---|
| 1× 103 CFU | 4/5b | 6/7 | - | 2/2 | - |
| 1× 104 CFU | 2/5 | 3/7 | - | 6/7 | - |
| 1× 105 CFU | 0/5 | 0/7 | - | 3/7 | - |
| 1× 106 CFU | -c | 0/2 | 2/2 | 0/7 | 2/2 |
| 1× 107 CFU | - | - | 7/7 | - | 7/7 |
| 1× 108 CFU | - | - | 6/7 | - | 7/7 |
| 1× 109 CFU | - | - | 3/7 | - | 7/7 |
| LD50 (CFU)d | 0.9 × 104 | 0.9 × 104 | 0.66 × 109 | 5.7 × 104 | >1 × 109 |
1-monophosphoryl lipid A
Survivors/total number of mice
Dose not tested
LD50 data were from probit analyses
Surviving mice were challenged with 1 × 109 CFU of χ3761 thirty days after the initial inoculation. All challenged mice survived.
While expression of lpxE in strains χ9732 (ΔpagP81::Plpp lpxE) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) was attenuating, this phenotype was not due to a general growth defect, as each mutant strain had growth characteristics nearly identical to wild-type strain χ3761 when grown in LB medium (data not shown). Strains χ9732 (ΔpagP81::Plpp lpxE) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) exhibited an LPS profile in silver-stained SDS-PAGE gels similar to χ3761 (Supplemental Fig. 2A). In addition, χ9732 (ΔpagP81::Plpp lpxE) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) were 2-fold more sensitive to the bile salt deoxycholate and SDS than other strains (data not shown), which may affect their survival in the intestinal tract, but the strains remained resistant to ox bile (data not shown).
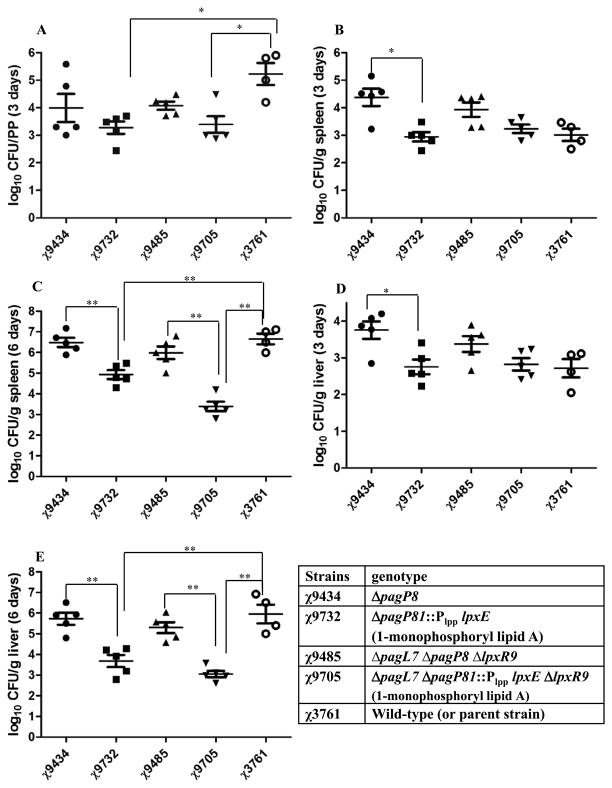
Because the ability to colonize lymphoid tissues (e.g. Peyer’s patches, spleen, liver) is an important attribute for live attenuated Salmonella vaccines (47, 55–57), we evaluated the effect of these mutations on tissue colonization. After oral dosing, each mutant strain was able to colonize mouse lymphoid tissues, although there were significant differences among some of the strains (Fig. 2). Notably, strain χ9434 (ΔpagP8) achieved higher titers than the other mutants in the spleen and liver at 3 days post-infection. The titer of strains χ9732 (ΔpagP81::Plpp lpxE) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) in spleen and liver did not increase at 6 days post infection, resulting in significantly lower numbers than strains χ9434 (ΔpagP8) and χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9).
Figure 2.
Bacterial burden in (A) Peyer’s patches (PP), (B, C) spleen and (D, E) liver of BALB/c mice (n = 4–5 each group). Groups of mice were orally inoculated with χ3761(wild-type UK-1), χ9434(ΔpagP8), χ9732(ΔpagP81::Plpp lpxE), χ9485(ΔpagL7 ΔpagP8 ΔlpxR9) and χ9705(ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9); 3–5 mice per group were euthanized, and spleen, liver and PP were collected, homogenized, and plated onto MacConkey and LB plates at 3 days and 6 days post inoculation. Salmonella colonies were counted and expressed as CFU per gram of PP, spleen, or liver. Significant differences in mean between groups were determined using one-way ANOVA analysis followed by Dunnett’s multiple comparison test. (* P < 0.05; ** P < 0.01).
Mice that survived inoculation with 1 × 106 to 1 × 109 CFU of the lpxE-expressing strains χ9732 (ΔpagP81::Plpp lpxE) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) were orally challenged with 1 × 109 CFU (1 × 105 LD50s) of the wild-type strain χ3761 thirty days after inoculation with the attenuated strains. All immunized mice survived challenge (Table 2). Thus the presence of LpxE attenuates the strains without compromising their ability to transiently colonize lymphoid tissues or their immunogenicity.
To evaluate the stability of the Plpp lpxE gene in vivo, mice were orally inoculated with approximately 1 × 109 CFU of either χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) or χ9732 (ΔpagP81::Plpp lpxE). After three days, spleens were harvested from the mice and colonizing Salmonella isolated. Spleen isolates were grown in LB and used to inoculate more mice. Our results indicated that the Plpp lpxE gene was stable in these strains after three mouse passages as determined by PCR analysis of 38 colonies followed by DNA sequence analysis of three PCR-positive colonies isolated after the third passage (data not shown).
Salmonella synthesizing 1-monophosphorylated LPS exhibits low endotoxic activity in vivo and in vitro
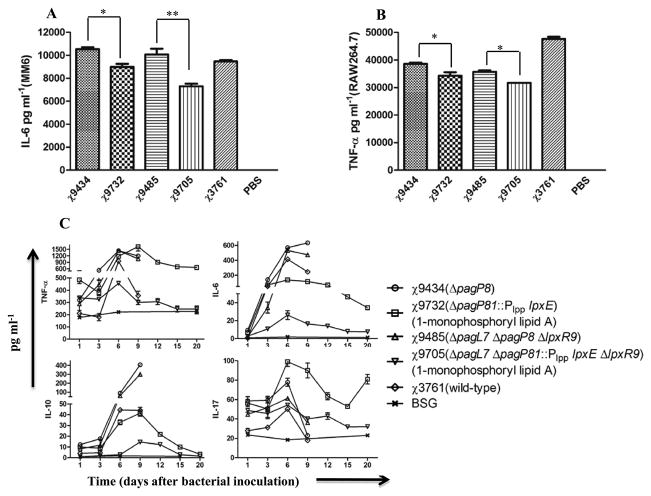
We determined the effect of modified lipid A on cytokine stimulation in tissue culture (Fig. 3A, 3B) and in animals (Fig. 3C). In tissue culture, 0.1 pmol/ml of LPS purified from strains expressing lpxE (χ9732 and χ9705) induced significantly lower levels of the pro-inflammatory cytokines IL-6 in the human cell line MM6 (Fig. 3A) and TNF-α in the mouse macrophage cell line RAW264.7 (Fig. 3B) than other strains. However, there were no differences in induction of either cytokine when cells were stimulated with 10 pmol/ml (data not shown). When sera from immunized mice were analyzed for cytokine production, we found that immunization with χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) induced lower levels of all cytokines tested except IL-17 (Fig. 3C).
Figure 3.
Cytokine concentrations in tissue culture supernatants from cells stimulated by LPS and in sera from immunized mice. Supernatants from Mono Mac 6 human monocyte cell line (MM6) and RAW264.7 murine macrophages were collected 24 h after stimulation with 0.1 or 10 pmol/ml LPS and tested for the presence of human IL-6 in MM-6 (A) and murine TNF-α in RAW264.7 (B), respectively. Data represent the mean cytokine concentration from two independent assays. P values for all cytokine analyses were determined using one-way ANOVA followed by Dunnett’s multiple comparison test. The multiple bioplex cytokine assay was used to detect and quantitate the amount of each cytokine in pooled sera collected from mice (n = 3 mice/group) inoculated with χ3761 and its derivatives on different days (C). All mice in groups inoculated with strains χ9434, χ9485 and χ3761 succumbed to the infection by day 10. In the group inoculated with χ9732, one mouse died on day 12. All mice inoculated with χ9705 survived for the duration of the experiment. The error bars represent the Mean ± SEM
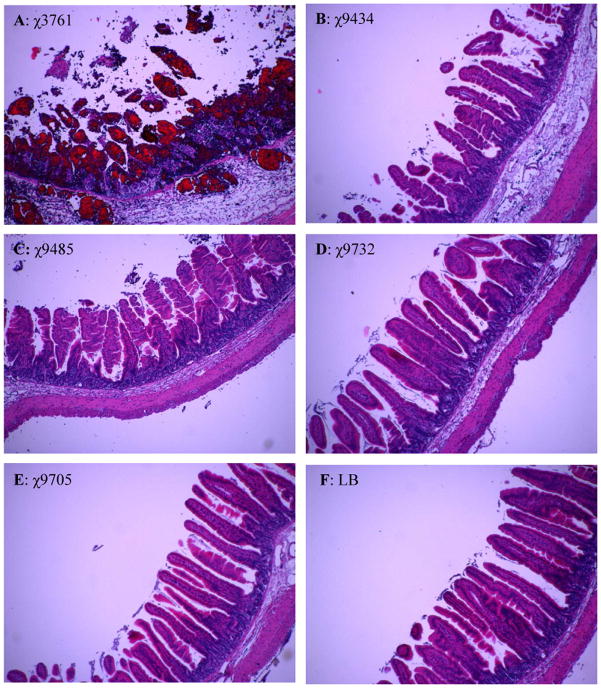
These mutant strains were also evaluated in rabbit ileal loops. Cells were introduced into ligated loops and incubated for 8 hours. Histological samples from loops infected with the wild-type strain χ3761 or mutant strains were stained with hematoxylin and eosin and examined microscopically (Fig. 4). The wild-type strain induced severe destruction of the mucosa including large areas of the necrotic epithelia, flattened villi, and heavy infiltration by polymorphomuclear leukocytes (PMN) (Fig. 4A and data not shown). In contrast, mutant strains χ9434 (ΔpagP8) and χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) induced some tissue destruction, although it was much milder than the wild-type strain (Fig. 4B and C). Loops injected with mutant strains χ9732 (ΔpagP81::Plpp lpxE) and χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) expressing lpxE were similar to the LB control loops, with no tissue destruction or PMN infiltration apparent (Fig 4D, 4E). These data are consistent with the mouse cytokine data which indicated that the 1-monophosphorylated LPS in Salmonella leads to a reduction in inflammatory responses after infection.
Figure 4.
S. Typhimurium mutants with LpxE expression decrease inflammation but still induce fluid secretion in rabbit ileal loops. Three - to six-cm-long rabbit ileal loops were injected with 109 CFU of S. Typhimurium strains for 8 h, and the fluid secretion and histopathological changes in the ileum were examined. Histopathological staining of rabbit ileal loops injected with S. Typhimurium strains or the L broth control (H & E stain, 40 ×), wild-type induced flattened villi, marked infiltration of PMN, and thickening of endothelium of blood vessels that accompanies PMN infiltration, but mutants with 1-monophosphorylated LPS did not. Inflammatory response: χ3761(wild-type UK-1) > χ9485(ΔpagL7 ΔpagP8 ΔlpxR9) > χ9434(ΔpagP8) > χ9732(ΔpagP81::Plpp lpxE) > χ9705(ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9).
Salmonella strains synthesizing monophosphoryl lipid A retain their ability to deliver a heterologous antigen
S. Typhimurium strain χ9241 (ΔpabA1516 ΔpabB232 ΔasdA16 ΔaraBAD23 ΔrelA198::araC PBAD lacI TT) is an attenuated vaccine strain that has been successfully employed to deliver the pneumococcal surface protein PspA and induce protective immunity against S. pneumoniae challenge (Table 1) (44, 53). Strain χ9241 carries the ΔrelA198::araC PBAD lacI TT deletion/insertion which provides arabinose-regulated delayed antigen synthesis (44). To evaluate the effect of lipid A modification on the efficacy of this strain, the single or triple mutations were introduced into χ9241 to yield strains χ9844 (ΔpagP8), χ9845 (ΔpagP81::Plpp lpxE), χ9846 (ΔpagL7 ΔpagP8 ΔlpxR9) and χ9881 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) (Table 1), and the expected lipid A modifications were confirmed by ESI-MS (data not shown). Subsequently, the Asd+ recombinant plasmid pYA3493 (vector control) or pYA4088, which encodes a recombinant pspA gene fused to DNA encoding the β-lactamase signal sequence (44), was introduced into each strain. In plasmid pYA4088, pspA expression is driven by the Ptrc promoter, and the bla signal sequence directs periplasmic secretion of PspA (Supplemental Fig. 2B).
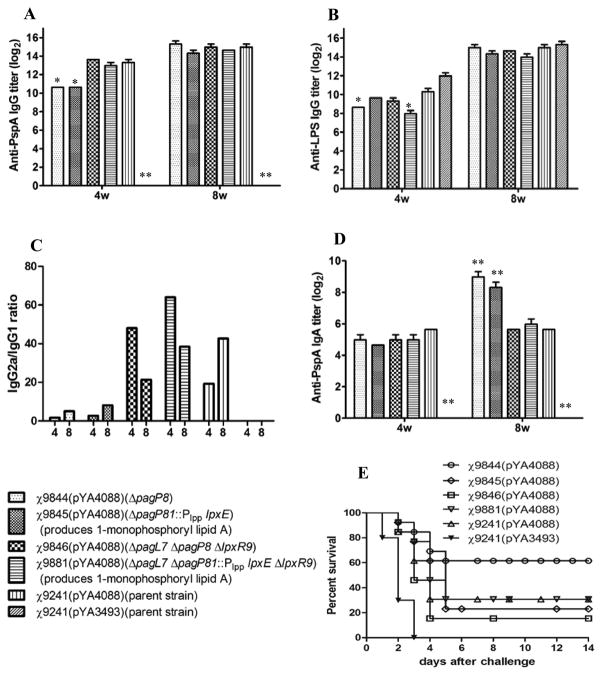
Groups of mice were orally inoculated with 1–2×109 CFU of each strain and boosted 5 weeks later with the same dose of the same strain. Consistent with the attenuation of χ9241, there were no significant adverse health effects on the inoculated mice. Blood was taken at various times, and serum IgG titers against PspA were measured (Fig. 5A). Serum IgG titers against PspA and S. Typhimurium LPS were below the limits of detection (<50) prior to immunization. Each strain synthesizing PspA triggered the production of significant levels of anti-PspA antibodies compared to the vector control strain χ9241(pYA3493) (P < 0.001). Importantly, the triple mutant strain expressing lpxE, χ9881(pYA4088), induced anti-PspA titers comparable to the parent strainχ9241(pYA4088). All the strains triggered the production of serum IgG antibodies against Salmonella LPS (Fig. 5B). The anti-LPS responses were similar for all strains except χ9844(pYA4088) (ΔpagP8) and χ9881(pYA4088) (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9), which induced significantly lower titers that the others at week 4 (Fig. 5B). By week 8, the anti-LPS IgG responses in all immunized mice were similar. Analysis of the ratios of IgG2a/IgG1 titers against PspA (Fig 5C) indicated that all strains induced a Th1 response typical of Salmonella (58). All strains expressing pspA elicited anti-PspA mucosal IgA responses significantly greater than the negative control strain χ9241(pYA3493) (Fig. 5D).
Figure 5.
ELISA measurements of serum IgG and mucosal IgA responses in immunized and control mice (n = 13 per group) and protection against S. pneumoniae challenge. (A) Total serum IgG specific for PspA, No immune responses were detected to PspA in mice immunized with the S. Typhimurium vaccine strain with the vector control plasmid, χ9241(pYA3493) (reciprocal titer <1:100); (B) anti-S. Typhimurium LPS serum IgG; (C) ratio of reciprocal anti-PspA IgG2a/IgG1 titers; (D) mucosal anti-PspA IgA. No anti-PspA IgG was detected in serum from mice immunized with the S. Typhimurium vaccine strain with the vector control plasmid, χ9241(pYA3493) (reciprocal titer <1:50). The data represent reciprocal antibody titers (mean ± SEM) in pooled sera or vaginal washes from mice orally immunized with attenuated Salmonella carrying either pYA4088 (PspA) or pYA3493 (control) and boosted 5 weeks later. * P < 0.01; ** P < 0.001 compared to mice immunized with χ9241(pYA4088). (E) Protection in orally immunized BALB/c mice challenged i.p. with 4×104 CFU of S. pneumoniae WU2–9 weeks after the first immunization. All vaccine groups were significantly different from the χ9241(pYA3493) control (P < 0.01), P values were determined using the log-rank test. There was no significant difference in protection among the other groups.
RASV synthesizing MPL and PspA induce protective immunity against Streptococcus pneumoniae challenge
To evaluate whether immunization elicited protective immunity, 9 weeks after the primary immunization, mice were challenged intraperitoneally with ~4×104 CFU of virulent S. pneumoniae strain WU2 (200 × LD50). Some mice in all groups immunized with strains expressing pspA survived challenge (Fig. 5E) while no mice inoculated with the control strain χ9241(pYA3493) survived challenge (P < 0.01). There was no statistical difference in the level of protection elicited by any of the strains expressing pspA.
Discussion
The potential usefulness of Salmonella as an antigen delivery vector is predicated on its ability to invade and transiently persist in host tissues, thereby stimulating robust mucosal, cellular and humoral immune responses. A virtual plethora of attenuating mutations and strategies have been described and shown to be effective at immunizing animals, particularly mice in the case of S. Typhimurium (1, 3). However, results in human trials using S. Typhi or S. Typhimurium as vectors have yet to demonstrate similar results, with vaccine strains being reactogenic and/or overattenuated, eliciting poor immune responses against vectored antigens. Rendering lipid A non-toxic may provide a means to safely increase the dose and/or reduce the level of attenuation to facilitate induction of a robust response to the vectored antigen. This may also provide an adequate level of safety to allow the use of live attenuated bacterial vaccines in infants and children, a target group that can benefit the most from this technology and for strains exhibiting regulated delayed lysis (8).
Salmonella lipid A is a mixture of closely related species that contain between 5–7 fatty acid moieties, and it may also be modified with other polar substituents (Fig. 1A). About 15% of Salmonella lipid A is hepta-acylated, while the most abundant species is hexa-acylated, as in E.coli (59). Dephosphorylation of the 1-phosphate group of lipid A is sufficient to reduce or eliminate its toxic effects (15, 60). The MPL used clinically consists primarily of 3-O-deacylated-1′-monophosphoryl lipid A (3D-MPL), which is obtained by sequential mild acid and mild base hydrolysis of Salmonella enterica serovar Minnesota R595 LPS (61). It is a mixture of penta- and hexa-acylated species. The hexa-acylated component of 3D-MPL lacks the hydroxymyristic acid moiety at position 3 and possesses a secondary palmitate chain on the 2 position R-3-hydroxymyristate chain (Fig. 1A). Initially, we attempted to generate 3D-MPL in S. Typhimurium by the combined over-expression of pagL, pagP and lpxE. However, we were unable to achieve PagP- and PagL-mediated lipid A modification above 50% of the total lipid A content under our standard laboratory growth conditions (data not shown). We then opted to eliminate pagL and pagP to engineer Salmonella synthesizing the 1′-monophosphoryl-hexa-acylated lipid A variant shown in Fig. 1B, which is also an excellent adjuvant.
In this report, we demonstrated that insertion of lpxE into the Salmonella chromosome resulted in dephosphorylation of the lipid A, although LpxE activity was dependent on the position of lpxE in the chromosome. These results are consistent with the observations of Beckwith et al. described over forty years ago in E. coli (62) and subsequently confirmed for Salmonella (63) demonstrating that the precise location in the bacterial chromosome can affect the level of gene transcription. Expression of codon-optimized lpxE inserted into chromosome at pagP resulted in complete removal of the lipid A 1′-phosphate group in living S. Typhimurium cells (Fig. 1) under a variety of growth conditions (Supplemental Fig 1B).
Expression of lpxE was attenuating for virulence (Table 2). This virulence reduction appears to be directly related to the production of detoxified lipid A, as a ΔpagP mutant was not attenuated. Evidence supporting this correlation comes from the finding that the mutants expressing lpxE induced lower levels of cytokine secretion compared with the parent strain in in vitro and in vivo models (Fig. 3, 4). Inoculation of mice with strain χ9705, in which 1′-dephosphorylation was essentially complete, resulted in lower induction levels of a number of pro-inflammatory cytokines including TNF-α and IL-6 (Fig. 3), while retaining overall immunogenicity (Table 2). It is difficult to compare these results directly to what occurs when humans are vaccinated with a live Salmonella vaccine for two reasons. First, since S. Typhi does not infect mice, it is not possible to generate meaningful cytokine data with S. Typhi vaccines in mice. Second, cytokine measurements in circulating human blood are not typically reported in trials with attenuated S. Typhi vaccines. However, in one study, peripheral blood monocytes were isolated from persons vaccinated with one of several S. Typhi vaccine strains and the levels of cytokines produced in response to S. Typhi flagella and LPS were measured (64). In typhoid patients, infected with S. Typhi, TNF-α levels ranging from 2609 to 6338 pg/ml and IL-6 levels ranging from 2416 to 7713 pg/ml of serum in the acute and convalescent phases, respectively, have been reported (65). These levels are substantially higher than those we observed in mice with any of our S. Typhimurium strains including the wild-type strain χ3761 (Fig. 3).
Although the cytokine levels in the tissue culture assays were higher than expected, the IL-6 levels we obtained for χ9705 LPS stimulation of MM6 cells was similar to those reported previously for MM6 cells exposed to MPL (66). In another study using MM6 cells, there was about a 3-fold difference in TNF-α production by wild-type lipid A and MPL (67). The lipid A preparation from parent strain χ3761 elicted nearly two-fold greater levels of TNF-α than the monophosphoryl lipid A from χ9705 (Fig. 3). The difference in results may be due to effects caused by other structural differences between MPL and the lipid A from χ9705.
Interestingly, triple mutant strain χ9705 was slightly more attenuated than χ9732 (ΔpagP81::Plpp lpxE), indicating that deletion of either pagL and/or lpxR, in the presence of ΔpagP81, reduced virulence. We observed a similar correlation when comparing strains χ9434 (ΔpagP8) and χ9485 (ΔpagL7 ΔpagP8 ΔlpxR9) that did not express lpxE (Table 2). While it is not clear whether deletion of pagL or lpxR, or both is required for this small decrease in virulence, we speculate that the pagL deletion is responsible. The actions of PagL and PagP serve to decrease the interaction of lipid A with TLR4, which has been suggested to enhance the ability of Salmonella to adapt to the host environment (68). Importantly, 1-dephosphorylated lipid A did not alter the immunogenicity of attenuated S. Typhimurium strain χ9241 expressing the pneumococcal antigen gene pspA (Fig. 5) indicating that this modification may be used in conjunction with other attenuating mutations to reduce reactogenicity and enhance the safety profile of the vaccine.
Our finding that the production of monophosphoryl lipid A that induces a limited immune response in the host, reduced the virulence of S. Typhimurium is in contrast to what happens in Yersinia pestis, in which the production of strongly stimulatory LPS results in a significant reduction in virulence (69, 70). The different outcomes are due to the different pathogenesis mechanisms utilized by the two pathogens. Y. pestis employs a weakly stimulatory LPS synthesized at 37 °C to escape host detection and killing by local inflammatory responses when it infects the mammalian hosts via the bite of infected fleas. For Salmonella, induction of a local inflammatory response early in infection seems to be part of its survival strategy, providing one mechanism (among many) to facilitate its invasion of the gut mucosa (71). It is clear from research done with Salmonella msbB mutants, which produce penta-acylated lipid A, have a reduced affinity to TLR4 resulting in attenuation (72, 73).
Our results demonstrate that production of 1′-monophosphoryl lipid A by an attenuated Salmonella strain does not diminish its ability to elicit an immune response against its own LPS (Fig. 5B), or a heterologous antigen, PspA (Fig. 5A). Attenuated Salmonella strain χ9241(pYA4088) and its derivative, χ9881(pYA4088) that produces 1′-monophosphoryl lipid A, both induced a strong Th1 response, as determined by the high ratio of IgG2 to IgG1 (Fig. 5C). This is consistent with observations by our group and others, that Salmonella typically induces a Th1-biased response (43, 53, 74), although a more balanced Th1/Th2 response can be obtained by altering the Salmonella genotype or immunization strategy (43, 45).
Although strain χ9705 (ΔpagL7 ΔpagP81::Plpp lpxE ΔlpxR9) produces nearly all of its lipid A lacking the 1′ phosphate group (Fig. 1) and is completely attenuated for virulence, production of monophosphoryl lipid A is not an acceptable attenuation strategy, as a single point mutation inactivating lpxE would render the strain as virulent as the wild-type parent (compare strains χ9485 and χ9706 in Table 2). We have based our approach on the fact that commercial monophosphoryl lipid A (MPL) has been proven safe and immunogenic for use as an adjuvant in humans. Thus, lpxE expression may enhance the safety of a Salmonella vaccine strain attenuated by other means, for example, when using the regulated delayed lysis in vivo attenuation to deliver a bolus of protective antigen and confer complete biological containment (8, 75). We also want to prevent unwanted side effects that can be caused by lipid A, such as the mild diarrhea or fevers experienced by some vaccinees that have been observed in clinical studies (5, 76–79) using attenuated S. Typhi vaccines. This type of modification, though helpful and necessary, is likely to be incremental, particularly when evaluated in a mouse model, where these types of side reactions are typically not seen with attenuated Salmonella strains.
There have been a number of recent improvements in the design of S. Typhi strains for antigen delivery, including the use of promoters that allow regulated antigen expression (80, 81), refinement of attenuating mutations (3, 82) and regulated delayed attenuation (83). Now, in addition, lipid A detoxification by lpxE provides a new and useful tool for improving live Salmonella vaccines to prevent typhoid and paratyphoid fever (84) and for antigen delivery, thus improving the safety of the vaccine without compromising immunogenicity. This may permit the use strains that are more aggressive for colonizing mucosal tissues and thereby enhancing immune responses without compromising safety.
Supplementary Material
Acknowledgments
This work was supported by grant 37863 from the Bill and Melinda Gates Foundation and by NIH grant GM-51796 to C. R. H. R. The mass spectrometry facility in the Department of Biochemistry of the Duke University Medical Center is supported by the LIPID MAPS Large Scale Collaborative Grant number GM-069338 from NIH.
We thank Jacquelyn A Kilbourne, Bronwyn Gunn and Heather Matthies for their expert technical assistance.
References
- 1.Atkins HS, Morton M, Griffin KF, Stokes MGM, Nataro JP, Titball RW. Recombinant Salmonella vaccines for biodefence. Vaccine. 2006;24:2710–2717. doi: 10.1016/j.vaccine.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 2.Lewis GK. Live-attenuated Salmonella as a prototype vaccine vector for passenger immunogens in humans: are we there yet? Expert Rev Vaccines. 2007;6:431–440. doi: 10.1586/14760584.6.3.431. [DOI] [PubMed] [Google Scholar]
- 3.Cheminay C, Hensel M. Rational design of Salmonella recombinant vaccines. Int J Med Microbiol. 2008;298:87–98. doi: 10.1016/j.ijmm.2007.08.006. [DOI] [PubMed] [Google Scholar]
- 4.Cardenas L, Clements JD. Oral immunization using live attenuated Salmonella spp as carriers of foreign antigens. Clin Microbiol Rev. 1992;5:328–342. doi: 10.1128/cmr.5.3.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tacket CO, Hone DM, Curtiss R, Kelly SM, Losonsky G, Guers L, Harris AM, Edelman R, Levine MM. Comparison of the safety and immunogenicity of ΔaroC ΔaroD and Δcya Δcrp Salmonella typhi strains in adult volunteers. Infect Immun. 1992;60:536–541. doi: 10.1128/iai.60.2.536-541.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tacket CO, Sztein MB, Wasserman SS, Losonsky G, Kotloff KL, Wyant TL, Nataro JP, Edelman R, Perry J, Bedford P, Brown D, Chatfield S, Dougan G, Levine MM. Phase 2 clinical trial of attenuated Salmonella enterica serovar Typhi oral live vector vaccine CVD 908-htrA in US volunteers. Infect Immun. 2000;68:1196–1201. doi: 10.1128/iai.68.3.1196-1201.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rietschel ET, Galanos C. Lipid A antiserum-mediated protection against lipopolysaccharide- and lipid A-induced fever and skin necrosis. Infect Immun. 1977;15:34–49. doi: 10.1128/iai.15.1.34-49.1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kong W, Wanda SY, Zhang X, Bollen W, Tinge SA, Roland KL, Curtiss R., III Regulated programmed lysis of recombinant Salmonella in host tissues to release protective antigens and confer biological containment. Proc Natl Acad Sci U S A. 2008;105:9361–9366. doi: 10.1073/pnas.0803801105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raetz CRH, Whitfield C. Lipopolysaccharide endotoxins. Annu Rev Biochem. 2002;71:635–700. doi: 10.1146/annurev.biochem.71.110601.135414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raetz CRH, Reynolds CM, Trent MS, Bishop RE. Lipid A modification systems in gram-negative bacteria. Annu Rev Biochem. 2007;76:295–329. doi: 10.1146/annurev.biochem.76.010307.145803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller SI, Ernst RK, Bader MW. LPS, TLR4 and infectious disease diversity. Nat Rev Microbiol. 2005;3:36–46. doi: 10.1038/nrmicro1068. [DOI] [PubMed] [Google Scholar]
- 12.Lu YC, Yeh WC, Ohashi PS. LPS/TLR4 signal transduction pathway. Cytokine. 2008;42:145–151. doi: 10.1016/j.cyto.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Miyake K. Roles for accessory molecules in microbial recognition by Toll-like receptors. J Endoxtin Res. 2006;12:195–204. doi: 10.1179/096805106X118807. [DOI] [PubMed] [Google Scholar]
- 14.Takeda K, Akira S. TLR signaling pathways. Semin Immunol. 2004;16:3–9. doi: 10.1016/j.smim.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 15.Mata-Haro V, Cekic C, Martin M, Chilton PM, Casella CR, Mitchell TC. The vaccine adjuvant monophosphoryl lipid A as a TRIF-biased agonist of TLR4. Science. 2007;316:1628–1632. doi: 10.1126/science.1138963. [DOI] [PubMed] [Google Scholar]
- 16.Kagan JC, Su T, Horng T, Chow A, Akira S, Medzhitov R. TRAM couples endocytosis of Toll-like receptor 4 to the induction of interferon-beta. Nat Immunol. 2008;9:361–368. doi: 10.1038/ni1569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Takeuchi O, Akira S. Pattern Recognition Receptors and Inflammation. Cell. 2010;140:805–820. doi: 10.1016/j.cell.2010.01.022. [DOI] [PubMed] [Google Scholar]
- 18.Rietschel ET. Bacterial endotoxin: molecular relationships of structure to activity and function. Faseb J. 1994;8:217–225. doi: 10.1096/fasebj.8.2.8119492. [DOI] [PubMed] [Google Scholar]
- 19.Rietschel ET. The chemical structure of bacterial endotoxin in relation to bioactivity. Immunobiology. 1993;187:169–190. doi: 10.1016/S0171-2985(11)80338-4. [DOI] [PubMed] [Google Scholar]
- 20.Park BS, Song DH, Kim HM, Choi BS, Lee H, Lee JO. The structural basis of lipopolysaccharide recognition by the TLR4-MD-2 complex. Nature. 2009;458:1191–U1130. doi: 10.1038/nature07830. [DOI] [PubMed] [Google Scholar]
- 21.Erridge C, Bennett-Guerrero E, Poxton IR. Structure and function of lipopolysaccharides. Microbes Infect. 2002;4:837–851. doi: 10.1016/s1286-4579(02)01604-0. [DOI] [PubMed] [Google Scholar]
- 22.Reed SG, Bertholet S, Coler RN, Friede M. New horizons in adjuvants for vaccine development. Trends Immunol. 2009;30:23–32. doi: 10.1016/j.it.2008.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Baldridge JR, Crane RT. Monophosphoryl lipid A (MPL) formulations for the next generation of vaccines. Methods. 1999;19:103–107. doi: 10.1006/meth.1999.0834. [DOI] [PubMed] [Google Scholar]
- 24.Wheeler AW, Marshall JS, Ulrich JT. A Th1-inducing adjuvant, MPL (R), enhances antibody profiles in experimental animals suggesting it has the potential to improve the efficacy of allergy vaccines. Int Arch Allergy Immunol. 2001;126:135–139. doi: 10.1159/000049504. [DOI] [PubMed] [Google Scholar]
- 25.Vernacchio L, Bernstein H, Pelton S, Allen C, MacDonald K, Dunn J, Duncan DD, Tsao G, LaPosta V, Eldridge J, Laussucq S, Arnbrosino DM, Molrine DC. Effect of monophosphoryl lipid A (MPL (R)) on T-helper cells when administered as an adjuvant with pneumocococcal-CRM197 conjugate vaccine in healthy toddlers. Vaccine. 2002;20:3658–3667. doi: 10.1016/s0264-410x(02)00413-9. [DOI] [PubMed] [Google Scholar]
- 26.Thompson BS, Chilton PM, Ward JR, Evans JT, Mitchell TC. The low-toxicity versions of LPS, MPL (R) adjuvant and RC529, are efficient adjuvants for CD4(+) T cells. J Leukoc Biol. 2005;78:1273–1280. doi: 10.1189/jlb.0305172. [DOI] [PubMed] [Google Scholar]
- 27.Wang XY, Karbarz MJ, McGrath SC, Cotter RJ, Raetz CRH. MsbA transporter-dependent lipid A 1-dephosphorylation on the periplasmic surface of the inner membrane - Topography of Francisella novicida LpxE expressed in Escherichia coli. J Biol Chem. 2004;279:49470–49478. doi: 10.1074/jbc.M409078200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bertani G. Studies on lysogenesis I.: The mode of phage liberation by lysogenic Escherichia coli. J Bacteriol. 1951;62:293–300. doi: 10.1128/jb.62.3.293-300.1951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shi YX, Latifi T, Cromie MJ, Groisman EA. Transcriptional control of the antimicrobial peptide resistance ugtL gene by the Salmonella PhoP and SlyA regulatory proteins. J Biol Chem. 2004;279:38618–38625. doi: 10.1074/jbc.M406149200. [DOI] [PubMed] [Google Scholar]
- 30.Nakayama K, Kelly SM, Curtiss R., III Construction of an Asd+ expression-cloning vector: stable maintenance and high level expression of cloned genes in a Salmonella vaccine strain. Nat Bio-technol. 1988;6:693–697. [Google Scholar]
- 31.Neidhardt FC, Bloch PL, Smith DF. Culture medium for enterobacteria. J Bacteriol. 1974;119:736–747. doi: 10.1128/jb.119.3.736-747.1974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sambrook J, Fritsch EF, Maniatis T. Molecular cloning: a laboratory manual. 2. Cold Spring Harbor Laboratory Press; Cold Spring Harbor, NY: 1989. [Google Scholar]
- 33.Hassan JO, Curtiss R., III Control of colonization by virulent Salmonella typhimurium by oral immunization of chickens with avirulent Δcya Δcrp Salmonella typhimurium. Res Microbiol. 1990;141:839–850. doi: 10.1016/0923-2508(90)90119-b. [DOI] [PubMed] [Google Scholar]
- 34.Edwards RA, Keller LH, Schifferli DM. Improved allelic exchange vectors and their use to analyze 987P fimbria gene expression. Gene. 1998;207:149–157. doi: 10.1016/s0378-1119(97)00619-7. [DOI] [PubMed] [Google Scholar]
- 35.Roland K, Curtiss R, III, Sizemore D. Construction and evaluation of a Δcya Δcrp Salmonella typhimurium strain expressing avian pathogenic Escherichia coli O78 LPS as a vaccine to prevent airsacculitis in chickens. Avian Dis. 1999;43:429–441. [PubMed] [Google Scholar]
- 36.Hitchcock PJ, Brown TM. Morphological heterogeneity among Salmonella lipopolysaccharide chemotypes in silver stained polyacrylamide gels. J Bacteriol. 1983;154:269–277. doi: 10.1128/jb.154.1.269-277.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Groisman EA, Kayser J, Soncini FC. Regulation of polymyxin resistance and adaptation to low-Mg2+ environments. J Bacteriol. 1997;179:7040–7045. doi: 10.1128/jb.179.22.7040-7045.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bligh EG, Dyer WJ. A rapid method of total lipid extraction and purification. Can J Biochem Phys. 1959;37:911–917. doi: 10.1139/o59-099. [DOI] [PubMed] [Google Scholar]
- 39.Gibbons HS, Reynolds CM, Guan ZQ, Raetz CRH. An inner membrane dioxygenase that generates the 2-hydroxymyristate moiety of Salmonella lipid A. Biochemistry. 2008;47:2814–2825. doi: 10.1021/bi702457c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yi EC, Hackett M. Rapid isolation method for lipopolysaccharide and lipid A from Gram-negative bacteria. Analyst. 2000;125:651–656. doi: 10.1039/b000368i. [DOI] [PubMed] [Google Scholar]
- 41.Hirschfeld M, Ma Y, Weis JH, Vogel SN, Weis JJ. Cutting edge: repurification of lipopolysaccharide eliminates signaling through both human and murine toll-like receptor 2. J Immunol. 2000;165:618–622. doi: 10.4049/jimmunol.165.2.618. [DOI] [PubMed] [Google Scholar]
- 42.Osborn MJ. Studies on gram-negative cell wall. 1. evidence for role of 2-Keto-3-deoxyoctonate in Lipopolysaccharide of Salmonella typhimurium. Proc Natl Acad Sci U S A. 1963;50:499–506. doi: 10.1073/pnas.50.3.499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kang HY, Srinivasan J, Curtiss R., III Immune responses to recombinant pneumococcal PspA antigen delivered by live attenuated Salmonella enterica serovar Typhimurium vaccine. Infect Immun. 2002;70:1739–1749. doi: 10.1128/IAI.70.4.1739-1749.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xin W, Wanda SY, Li Y, Wang S, Mo H, Curtiss R., III Analysis of type II secretion of recombinant pneumococcal PspA and PspC in a Salmonella enterica serovar Typhimurium vaccine with regulated delayed antigen synthesis. Infect Immun. 2008;76:3241–3254. doi: 10.1128/IAI.01623-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li Y, Wang S, Xin W, Scarpellini G, Shi Z, Gunn B, Roland KL, Curtiss R., III A sopB deletion mutation enhances the immunogenicity and protective efficacy of a heterologous antigen delivered by live attenuated Salmonella enterica vaccines. Infect Immun. 2008;76:5238–5246. doi: 10.1128/IAI.00720-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Briles DE, King JD, Gray MA, McDaniel LS, Swiatlo E, Benton KA. PspA, a protection-eliciting pneumococcal protein: Immunogenicity of isolated native PspA in mice. Vaccine. 1996;14:858–867. doi: 10.1016/0264-410x(96)82948-3. [DOI] [PubMed] [Google Scholar]
- 47.Nayak AR, Tinge SA, Tart RC, McDaniel LS, Briles DE, Curtiss R., III A live recombinant avirulent oral Salmonella vaccine expressing pneumococcal surface protein A induces protective responses against Streptococcus pneumoniae. Infect Immun. 1998;66:3744–3751. doi: 10.1128/iai.66.8.3744-3751.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou ZM, Lin SH, Cotter RJ, Raetz CRH. Lipid A modifications characteristic of Salmonella typhimurium are induced by NH4VO3 in Escherichia coli K12-detection of 4-amino-4-deoxy-L-arabinose, phosphoethanolamine and palmitate. J Biol Chem. 1999;274:18503–18514. doi: 10.1074/jbc.274.26.18503. [DOI] [PubMed] [Google Scholar]
- 49.Gibbons HS, Kalb SR, Cotter RJ, Raetz CRH. Role of Mg2+ and pH in the modification of Salmonella lipid A after endocytosis by macrophage tumour cells. Mol Microbiol. 2005;55:425–440. doi: 10.1111/j.1365-2958.2004.04409.x. [DOI] [PubMed] [Google Scholar]
- 50.Bader MW, Sanowar S, Daley ME, Schneider AR, Cho US, Xu WQ, Klevit RE, Le Moual H, Miller S. Recognition of antimicrobial peptides by a bacterial sensor kinase. Cell. 2005;122:461–472. doi: 10.1016/j.cell.2005.05.030. [DOI] [PubMed] [Google Scholar]
- 51.Bader MW, Navarre WW, Shiau W, Nikaido H, Frye JG, McClelland M, Fang FC, Miller SI. Regulation of Salmonella typhimurium virulence gene expression by cationic antimicrobial peptides. Mol Microbiol. 2003;50:219–230. doi: 10.1046/j.1365-2958.2003.03675.x. [DOI] [PubMed] [Google Scholar]
- 52.Vescovi EG, Soncini FC, Groisman EA. Mg2+ as an extracellular signal: environmental regulation of Salmonella virulence. Cell. 1996;84:165–174. doi: 10.1016/s0092-8674(00)81003-x. [DOI] [PubMed] [Google Scholar]
- 53.Kong Q, Liu Q, Roland KL, Curtiss R., III Regulated delayed expression of rfaH in an attenuated Salmonella enterica serovar Typhimurium vaccine enhances immunogenicity of outer membrane proteins and a heterologous antigen. Infect Immun. 2009;77:5572–5582. doi: 10.1128/IAI.00831-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Belden WJ, Miller SI. Further characterization of the PhoP regulon - identification of new PhoP-activated virulence loci. Infect Immun. 1994;62:5095–5101. doi: 10.1128/iai.62.11.5095-5101.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Coulson NM, Fulop M, Titball RW. Effect of different plasmids on colonization of mouse tissues by the aromatic amino acid dependent Salmonella typhimurium SL 3261. Microb Pathog. 1994;16:305–311. doi: 10.1006/mpat.1994.1031. [DOI] [PubMed] [Google Scholar]
- 56.Valentine PJ, Devore BP, Heffron F. Identification of three highly attenuated Salmonella typhimurium mutants that are more immunogenic and protective in mice than a prototypical aroA mutant. Infect Immun. 1998;66:3378–3383. doi: 10.1128/iai.66.7.3378-3383.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bumann D. Regulated antigen expression in live recombinant Salmonella enterica serovar typhimurium strongly affects colonization capabilities and specific CD4(+)-T-cell responses. Infect Immun. 2001;69:7493–7500. doi: 10.1128/IAI.69.12.7493-7500.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ramarathinam L, Niesel D, Klimpel G. Salmonella typhimurium induces IFN-gamma production in murine splenocytes. role of natural killer cells and macrophages. J Immunol. 1993;150:3973–3981. [PubMed] [Google Scholar]
- 59.Chan S, Reinhold VN. Detailed structural characterization of lipid A: electrospray ionization coupled with tandem Mass-Spectrometry. Anal Biochem. 1994;218:63–73. doi: 10.1006/abio.1994.1141. [DOI] [PubMed] [Google Scholar]
- 60.Morrison DC, Silverstein R, Luchi M, Shnyra A. Structure-function relationships of bacterial endotoxins - Contribution to microbial sepsis. Infect Dis Clin North Am. 1999;13:313–340. doi: 10.1016/s0891-5520(05)70077-5. [DOI] [PubMed] [Google Scholar]
- 61.Garcon N, Chomez P, Van Mechelen M. GlaxoSmithKline Adjuvant systems in vaccines: concepts, achievements and perspectives. Expert Rev Vaccines. 2007;6:723–739. doi: 10.1586/14760584.6.5.723. [DOI] [PubMed] [Google Scholar]
- 62.Beckwith JR, Signer ER, Epstein W. Transposition of Lac Region of E. coli. Cold Spring Harbor Symp Quant Biol. 1966;31:393–401. doi: 10.1101/sqb.1966.031.01.051. [DOI] [PubMed] [Google Scholar]
- 63.Schmid MB, Roth JR. Gene location affects expression level in Salmonella typhimurium. J Bacteriol. 1987;169:2872–2875. doi: 10.1128/jb.169.6.2872-2875.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sztein MB, Wasserman SS, Tacket CO, Edelman R, Hone D, Lindberg AA, Levine MM. Cytokine production patterns and lymphoproliferative responses in volunteers orally immunized with attenuated vaccine strains of Salmonella typhi. J Infect Dis. 1994;170:1508–1517. doi: 10.1093/infdis/170.6.1508. [DOI] [PubMed] [Google Scholar]
- 65.Keuter M, Dharmana E, Gasem MH, Vandervenjongekrijg J, Djokomoeljanto R, Dolmans WMV, Demacker P, Sauerwein R, Gallati H, Vandermeer JWM. Patterns of proinflammatory cytokines and Inhibitors during typhoid fever. J Infect Dis. 1994;169:1306–1311. doi: 10.1093/infdis/169.6.1306. [DOI] [PubMed] [Google Scholar]
- 66.Evans JT, Cluff CW, Johnson DA, Lacy MJ, Persing DH, Baldridge JR. Enhancement of antigen-specific immunity via the TLR4 ligands MPL adjuvant and Ribi.529. Expert Rev Vaccines. 2003;2:219–229. doi: 10.1586/14760584.2.2.219. [DOI] [PubMed] [Google Scholar]
- 67.Eperon S, DeGroote D, WernerFelmayer G, Jungi TW. Human monocytoid cell lines as indicators of endotoxin: Comparison with rabbit pyrogen and Limulus amoebocyte lysate assay. J Immunol Methods. 1997;207:135–145. doi: 10.1016/s0022-1759(97)00112-9. [DOI] [PubMed] [Google Scholar]
- 68.Kawasaki K, Ernst RK, Miller SI. Deacylation and palmitoylation of lipid A by Salmonellae outer membrane enzymes modulate host signaling through Toll-like receptor 4. J Endoxtin Res. 2004;10:439–444. doi: 10.1179/096805104225006264. [DOI] [PubMed] [Google Scholar]
- 69.Montminy SW, Khan N, McGrath S, Walkowicz MJ, Sharp F, Conlon JE, Fukase K, Kusumoto S, Sweet C, Miyake K, Akira S, Cotter RJ, Goguen JD, Lien E. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nat Immunol. 2006;7:1066–1073. doi: 10.1038/ni1386. [DOI] [PubMed] [Google Scholar]
- 70.Sun W, Six D, Kuang X, Roland KL, Raetz CRH, Curtiss R., III A live attenuated strain of Yersinia pestis KIM as a vaccine against plague. Vaccine. 29:2986–2998. doi: 10.1016/j.vaccine.2011.01.099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Haraga A, Ohlson MB, Miller SI. Salmonellae interplay with host cells. Nat Rev Microbiol. 2008;6:53–66. doi: 10.1038/nrmicro1788. [DOI] [PubMed] [Google Scholar]
- 72.Khan SA, Everest P, Servos S, Foxwell N, Zahringer U, Brade H, Rietschel ET, Dougan G, Charles IG, Maskell DJ. A lethal role for lipid A in Salmonella infections. Mol Microbiol. 1998;29:571–579. doi: 10.1046/j.1365-2958.1998.00952.x. [DOI] [PubMed] [Google Scholar]
- 73.Low KB, Ittensohn M, Le T, Platt J, Sodi S, Amoss M, Ash O, Carmichael E, Chakraborty A, Fischer J, Lin SL, Luo X, Miller SI, Zheng LM, King I, Pawelek JM, Bermudes D. Lipid A mutant Salmonella with suppressed virulence and TNF alpha induction retain tumor-targeting in vivo. Nat Biotechnol. 1999;17:37–41. doi: 10.1038/5205. [DOI] [PubMed] [Google Scholar]
- 74.Pasetti MF, Simon JK, Sztein MB, Levine MM. Immunology of gut mucosal vaccines. Immunol Rev. 2011;239:125–148. doi: 10.1111/j.1600-065X.2010.00970.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ameiss K, Ashraf S, Kong W, Pekosz A, Wu WH, Milich D, Billaud JN, Curtiss R., III Delivery of woodchuck hepatitis virus-like particle presented influenza M2e by recombinant attenuated Salmonella displaying a delayed lysis phenotype. Vaccine. 2010;28:6704–6713. doi: 10.1016/j.vaccine.2010.07.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Gilman RH, Hornick RB, Woodward WE, Dupont HL, Snyder MJ, Levine MM, Libonati JP. Evaluation of a UDP-glucose-4-epimeraseless mutant of Salmonella Typhi as a live oral vaccine. J Infect Dis. 1977;136:717–723. doi: 10.1093/infdis/136.6.717. [DOI] [PubMed] [Google Scholar]
- 77.Hohmann EL, Oletta CA, Killeen KP, Miller SI. phoP/phoQ-deleted Salmonella typhi (Ty800) is a safe and immunogenic single-dose typhoid fever vaccine in volunteers. J Infect Dis. 1996;173:1408–1414. doi: 10.1093/infdis/173.6.1408. [DOI] [PubMed] [Google Scholar]
- 78.Tran TH, Nguyen TD, Nguyen TT, Ninh TTV, Tran NBC, Nguyen VMH, Tran TTN, Cao TT, Pham VM, Nguyen TCB, Tran TDH, Pham VT, To SD, Campbell JI, Stockwell E, Schultsz C, Simmons CP, Glover C, Lam W, Marques F, May JP, Upton A, Budhram R, Dougan G, Farrar J, Nguyen VVC, Dolecek C. A randomised trial evaluating the safety and immunogenicity of the novel single oral dose typhoid vaccine M01ZH09 in healthy Vietnamese children. PLOS One. 2010;5:e11778. doi: 10.1371/journal.pone.0011778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tacket CO, Sztein MB, Losonsky GA, Wasserman SS, Nataro JP, Edelman R, Pickard D, Dougan G, Chatfield SN, Levine MM. Safety of live oral Salmonella typhi vaccine strains with deletions in htrA and aroC aroD and immune response in humans. Infect Immun. 1997;65:452–456. doi: 10.1128/iai.65.2.452-456.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Curtiss R, III, Xin W, Li YH, Kong W, Wanda SY, Gunn B, Wang SF. New technologies in using recombinant attenuated Salmonella vaccine vectors. Crit Rev Immunol. 2010;30:255–270. doi: 10.1615/critrevimmunol.v30.i3.30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang SF, Li YH, Scarpellini G, Kong W, Shi HY, Baek CH, Gunn B, Wanda SY, Roland KL, Zhang X, Senechal-Willis P, Curtiss R., III Salmonella vaccine vectors displaying delayed antigen synthesis in vivo to enhance immunogenicity. Infect Immun. 2010;78:3969–3980. doi: 10.1128/IAI.00444-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hindle Z, Chatfield SN, Phillimore J, Bentley M, Johnson J, Cosgrove CA, Ghaem-Maghami M, Sexton A, Khan M, Brennan FR, Everest P, Wu T, Pickard D, Holden DW, Dougan G, Griffin GE, House D, Santangelo JD, Khan SA, Shea JE, Feldman RG, Lewis DJA. Characterization of Salmonella enterica derivatives harboring defined aroC and Salmonella pathogenicity island 2 type III secretion system (ssaV) mutations by immunization of healthy volunteers. Infect Immun. 2002;70:3457–3467. doi: 10.1128/IAI.70.7.3457-3467.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Curtiss R, III, Wanda S-Y, Gunn BM, Zhang X, Tinge SA, Ananthnarayan V, Mo H, Wang S, Kong W. Salmonella enterica serovar Typhimurium strains with regulated delayed attenuation in vivo. Infect Immun. 2009;77:1071–1082. doi: 10.1128/IAI.00693-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Levine MM. Typhoid vaccines ready for implementation. N Engl J Med. 2009;361:403–405. doi: 10.1056/NEJMe0905519. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.