Abstract
Purpose
The aims of this systematic review were: 1) to analyze the content overlap between nurse and physician hospital-based handoff documentation for the purpose of developing a list of interdisciplinary handoff information for use in the future development of shared and tailored computer-based handoff tools, and 2) to evaluate the utility of the Continuity of Care Document (CCD) standard as a framework for organizing hospital-based handoff information for use in electronic health records (EHRs).
Methods
We searched PubMed for studies published through July 2010 containing the indexed terms: handoff(s), hand-off, handover(s), shift-report, shift report, signout, and sign-out. Original, hospital-based studies of acute care nursing or physician handoff were included. Handoff information content was organized into lists of nursing, physician, and interdisciplinary handoff information elements. These information element lists were organized using CCD sections, with additional sections being added as needed.
Results
Analysis of 36 studies resulted in a total of 95 handoff information elements. Forty-six percent (44/95) of the information overlapped between the nurse and physician handoff lists. Thirty-six percent (34/95) were specific to the nursing list and 18% (17/95) were specific to the physician list. The CCD standard was useful for categorizing 80% of the terms in the lists and 12 category names were developed for the remaining 20%.
Conclusion
Standardized interdisciplinary, nursing-specific, and physician-specific handoff information elements that are organized around the CCD standard and incorporated into EHRs in a structured narrative format may increase the consistency of data shared across all handoffs, facilitate the establishment of common ground, and increase interdisciplinary communication.
Keywords: Handoff(s), Hand-off, Handover(s), Shift-report, Signout, and Sign-out, Interdisciplinary, Electronic Health Records
1. Introduction
The handoff of patient responsibility from one clinician to another occurs frequently in the hospital setting. Evidence suggests that increasing the frequency of clinician handoffs is associated with increased patient complications and longer hospital stays [1]. The Joint Commission requires effective intra- and interdisciplinary communication and the standardization of handoff between clinicians [2].
Several institutions have developed their own electronic tools to support discipline-specific patient handoff [3-5], and evidence suggests that integrating such tools into electronic health records (EHRs) can improve communication among caregivers, and reduce errors [6]. While the federal financial incentives for Meaningful Use of EHRs in the United States are likely to accelerate EHR adoption in hospitals [7], commercial EHRs do not provide “off-the-shelf” support for patient-centered workflow activities such as handoff. Specifically, data that support these activities, such as patients' height, weight, allergies, active medications, and clinicians' to-do lists, are missing, inconsistent, or documented using unstructured text in many commercial EHR systems [8].
Beyond providing relevant, handoff-related information to clinicians, EHRs should also facilitate interdisciplinary communication, given the evidence regarding emergent communication patterns and the role of individual providers in the handoff process. A recent study demonstrated that the information flow for handoffs for each patient was not dominated or coordinated by one particular professional group, but rather, it exhibited patient-centered data or unique communication patterns and information coordination by two or more influential providers from nursing, medicine, or pharmacy [9]. Based on these findings, the investigators recommended using the EHR to support electronic handoff communication modules and asynchronous multi-professional communication logs [9]. The information exchanged during discipline-specific patient handoffs (e.g., nurse to nurse, physician to physician) may consist of patient-centered data that is critical to interdisciplinary information exchange. Furthermore, electronic tools that intelligently extract types of content from disparate parts of the EHR, based on a standard framework, may help to support the dialogue that occurs between clinicians to standardize the process of patient handoff and, where appropriate, enable data reuse of patient information that is needed in multiple places by multiple disciplines within the EHR. The development of an electronic handoff system that contains a minimum dataset of prompts, predefined fields, and structured headings for the entry of free-text data when appropriate, is a possible solution to avoid duplicate data entry, maintain continuity of care, and avoid errors caused by information gaps [10].
The literature related to discipline-specific clinical handoffs has greatly increased over the past few years and this is the first systematic review to explicitly analyze the overlapping and distinct information contained in nurse and physician handoffs. Therefore, the aims of this systematic review were: 1) to analyze the content overlap between nurse and physician hospital-based handoff documentation for the purpose of developing a list of interdisciplinary handoff information used in the future development of shared and tailored computer-based handoff tools, and 2) to evaluate the utility of the Continuity of Care Document (CCD) standard as a framework for organizing hospital-based handoff information for use in (EHRs.
1.1. Theoretical Framework
The purpose of handoff communication is to establish common ground, or mutual understanding, of patient information between clinicians that are transferring the responsibility for patient care, typically due to a shift change or a change in patient location [11]. The establishment of common ground during handoff occurs explicitly through conversations and implicitly through shared documentation. To date, most handoff studies have focused on intra-disciplinary communication because handoff communication is a recognized clinical communication process that occurs between members of a clinical discipline. However, the division of labor amongst members of the interdisciplinary team in the clinical setting, which enables efficiency and functioning of the system as a whole, is dependent on information exchange and the establishment of common ground between disciplines [12]. Therefore, the interdisciplinary handoff information conveyed during an intra-disciplinary handoff may support clinicians' division of labor by establishing common ground that enables a clinician to develop a discipline-specific plan of care that is aligned with the interdisciplinary team's overall plans of care.
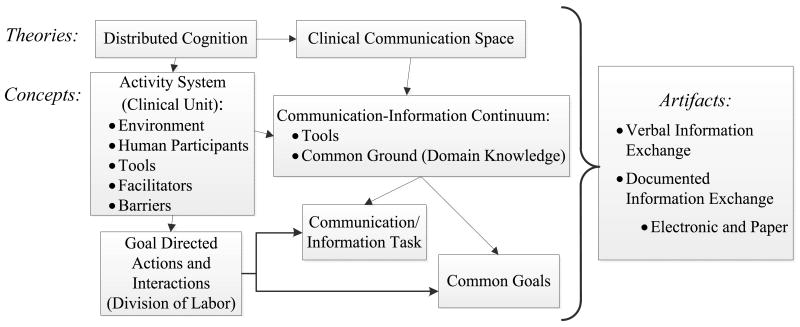
The integrated theoretical frameworks of distributed cognition and the clinical communication space have been used to analyze interdisciplinary information exchange and the establishment of common ground [13-16]. We used these integrated frameworks to inform our analysis of the verbal and documented information exchanged during handoffs and to highlight the potential role of an interdisciplinary handoff information element list for the purpose of standardizing hospital-based handoff (see Figure 1).
Figure 1.
Integrated Distributed Cognition and Clinical Communication Space Frameworks.
These integrated frameworks describe how common ground is established in the clinical setting through a process of information flow involving artifacts (e.g., electronic and paper-based documentation), communication between clinicians, and goal-directed actions and interactions within an activity system, such as a clinical unit [15]. The concept of “common ground” has been described as a means to facilitate effective informal communication, where interactivity and time pressure is high [13]; however, achieving common ground can be a challenge [13, 15]. Individuals may develop a mutual understanding or common ground during a face-to-face discussion; however, verbal communication is transient and must be documented to prevent information loss [15, 17]. When the information contained in an EHR is perceived as not sufficient, or is not updated, verbal discussions are the preferred method of information exchange between disciplines [16]. The clinical communication space framework suggests that the effectiveness of information exchange and the most appropriate method (e.g., an EHR versus a face-to-face discussion) is dependent on the level of common ground that has been established between clinicians. The distributed cognition framework characterizes clinicians' division of labor, gaps and overlaps in clinicians' domain knowledge (e.g., established common ground), the representation of information within artifacts such as EHR documentation, and patterns of communication and social interaction as essential elements to understand information exchange within an environment as a whole [18]. The integration of these two frameworks indicates that domain knowledge areas that overlap between nurses and physicians may be appropriate for data entry and display in interdisciplinary EHR tools and that such tools may facilitate the establishment of common ground and therefore improve interdisciplinary handoff communication.
2. Methods
To analyze the content overlap between nurse and physician hospital-based handoff and to develop a list of interdisciplinary handoff information elements, we searched PubMed for all published studies through July 2010 containing the indexed search terms: handoff(s), hand-off, handover(s), shift-report, shift report, signout, and sign-out. Two reviewers (S.C. and D.S.) independently analyzed the article abstracts for inclusion criteria and, in the instance of disagreement, held open discussions to reach a consensus. The inclusion criteria were original, hospital-based research studies that specifically investigated handoff content or structure which may have been verbal or documented for nurses or physicians, including the evaluation of computer or paper-based handoff tools. Non-acute care and hospital-based studies that were not focused on nursing or physician handoff were excluded. Additionally, handoff articles that focused only on theory (e.g., sociotechnical theory), professional practice issues, or general handoff mnemonics (e.g., SBAR - Situation, Background, Assessment, Recommendation) and did not include clinical elements of handoff content were excluded. The references of retrieved articles were analyzed for additional studies that met the inclusion criteria.
The reviewers (S.C. and D.S.) independently rated the studies using the Quality Scoring System for Evaluation of Handoff Research Studies guideline which was developed by Riesenberg et al. to allow for the standardized comparison of handoff study quality [19]. The guideline was developed for physician handoff studies; to use it for nursing handoff studies, we modified the item that asked if the study participants were clearly described to include a description of the number of nurses and the nurses' specialty (e.g., medical-surgical, critical care, oncology). In the case of disagreement over a study's quality score, the reviewers reached consensus through discussion. This scoring system has a total of 12 items and a maximum score of 16 points. The first two items rate the type of study design (1 to 3 points) and the total sample size (0 to 3 points). The remaining 10 items are binary (no = 0, yes = 1) and rate the quality of reporting and the internal validity of the study [19].
Next, each reviewer independently extracted all concepts or categories related to handoff information and handoff communication that were found in each study, and organized these into a comprehensive list of “handoff information elements”. Consensus was reached between the reviewers when disagreement occurred. Therefore, the list of handoff information elements was based on the findings of the reviewed handoff studies.
For all of the nursing-specific studies, the two reviewers collaboratively analyzed the collected handoff information elements and developed a comprehensive list that included all unique concepts or categories for nursing-specific handoff. This process was repeated for all of the physician-specific handoff studies. The resulting nursing-specific and physician-specific lists were analyzed for overlapping information elements to develop the interdisciplinary handoff element list. We categorized information elements as overlapping only if the information element was consistent in both groups' discipline-specific list of elements without further modification. For example, information elements that were at varying levels of granularity or otherwise required modification to fit both groups remained discipline specific to prevent information loss and ambiguity or the requirement of irrelevant documentation details. In the instances of disagreement, consensus was reached though discussion between the two reviewers. A search for a framework for inpatient handoff revealed small studies or anecdotal reports discussing numerous mnemonics that lacked scientifically rigorous research [20]. Therefore, we chose to explore and evaluate the appropriateness of various content-related data standards (CCD Health Information Technology Standards Panel (HITSP) C32, the Clinical Care Classification System, Systematized Nomenclature of Medicine--Clinical Terms (SNOMED-CT) and the Unified Medical Language System (UMLS)) were evaluated for their appropriateness as a categorization framework for inpatient nursing, physician and interdisciplinary handoff information elements. The CCD was evaluated, as opposed to other existing Clinical Document Architecture (CDA) constraints, such as the HITSP C48 “Referral Summary” or the Integrating the Healthcare Enterprise (IHE) Cross-Enterprise Document Sharing of Medical Summaries (XDS-MS), because of its intended purpose to support the aggregation and transfer of pertinent patient data from one provider to another. After a review of possibilities by the research team (S.C., D.S., D.V., P.S., S.B.) the CCD was selected as the foundation for the categorization based on its acceptance as a patient-centered electronic information exchange standard and relevance to continuity of care. We acknowledge that the CCD was developed for outpatient handoffs; however, given the lack of a validated framework for inpatient handoff, exploration of the CCD's generalizability to interdisciplinary inpatient handoff is worthwhile and informative. The CCD is a hybrid of the American Society for Testing and Materials International (ASTM) standard Continuity of Care Record (CCR) and the Health Level Seven (HL7) clinical documentation standard known as Clinical Document Architecture [21-23]. The CCD was developed as a documentation standard to organize information that supports care transitions in the outpatient setting or to facilitate information exchange during inter-institutional transfers. To evaluate the utility of the CCD standard as a framework for categorizing information elements from hospital-based handoff studies the two reviewers (SC and DS) coded the nursing-specific, physician-specific and interdisciplinary information elements according to each major CCD section as defined in the HL7 CCD standard [24] and personal information included in the CDA header [21]. Additional categories were added when the CCD framework was not sufficient and when an information element was judged as belonging to multiple categories.
3. Results
3.1. Handoff Literature Review and Interdisciplinary Handoff Element List Development
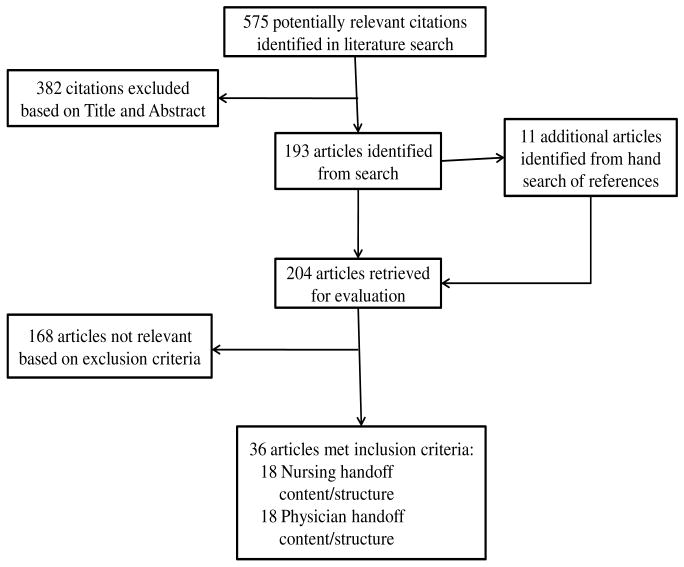
A total of 575 potentially relevant articles were retrieved from the literature search (see Figure 2). After reviewing each article's title and abstract 382 articles were excluded. Eleven additional articles were retrieved after reviewing the references of the remaining 193 articles. Based on our review of the remaining 204 articles, a total of 36 articles met our inclusion and exclusion criteria.
Figure 2.
The process used by the authors to select appropriate published studies about Nurses' and physicians' handoffs.
The range of scores for the Quality Scoring System for Evaluation of Handoff Research Studies was 4 to 13 out of a possible 16 points (see Tables 1 and 2). The range and average of quality scores for the nurse and physician articles were comparable (Nurse: range = 4 to 13, average = 9.6; Physician: range = 5 to 13, average = 10). Twenty-threeof the 36 studies were single group cross-sectional, single group post-test only, or qualitative studies (14 nursing studies, 9 physician studies). The remaining 4 nursing and 9 physician studies were single group pre- and post-test or cohort studies and one randomized control trial. Sample size accounted for the widest variability in quality scores, yet, is not an appropriate measure for qualitative studies.
Table 1. Nursing Handoff Studies.
| Paper | Study Methods | Sample and Size | Acute care setting | Score$ |
|---|---|---|---|---|
| Patterson, 1995 [25] | Cross-sectional survey | 197 surveys | All units, large medical center | 13 |
| Berkenstadt, 2008 [26] | Intervention: handoff checklist; interviews, observations | Pre: 5 interviews, 224 handoff observations, Post: 166 observations | Medical step-down unit | 12.5 |
| Miller, 2009[27] | Cohort comparison, content analysis | Cohort A:22 handoff observations, Cohort B: 23 observations | General medical, surgical, trauma intensive care units | 12.5 |
| Chaboyer, 2010 [28] | Observational, content analysis | 34 interviews, 532 handoff observations | Medical, surgical and rehabilitation | 12 |
| Lamond, 2000 [29] | Content analysis, multidimensional scalogram analysis | 60 audio-taped handoffs and formal written documents | Acute medical and acute surgical units from 2 hospitals | 11.5 |
| McFetridge, 2007 [30] | Interviews, focus groups, content analysis | 12 interviews, 2 focus groups, formal handoff document policies | Emergency department to intensive care | 11 |
| Welsh, 2010 [31] | Interviews, grounded theory | 20 interviews | General medicine, oncology, and surgical intensive care unit | 11 |
| McLane, 2009 [32] | Content analysis | 151 informal written handoff documents | Hematology, thoracic surgery, neurosurgery rehabilitation | 10.5 |
| Staggers, 2009 [33] | Observational, content analysis | 53 handoffs observed and audio-taped | Medical and surgical units in 3 acute care facilities | 10.5 |
| Currie, 2002 [34] | Cross-sectional survey | 28 surveys | Emergency department | 10 |
| Lally, 1999 [35] | Observational, thematic analysis | 6 handoff observations | General surgical and vascular surgery unit | 9.5 |
| Sexton, 2004 [36] | Observational, focus group, content analysis | 1 focus group, 23 audiotaped handoffs | General medical | 9 |
| Nelson, 2010 [37] | Intervention: computer-based handoff; survey, handoff duration time | Pre, Post, 6-months: 14 handoff durations each, survey unclear | Gastrointestinal surgical oncology unit | 8 |
| Fenton, 2006 [38] | Intervention: handoff guide; observations | Pre: 15 handoff observations; Post: 15 handoff observations | Geriatric rehabilitation unit | 7.5 |
| Block, 2010 [39] | Intervention: handoff card; random usage audits | Post: 13 audits of usage of formal handoff card | Labor and delivery | 7 |
| Sherlock, 1995 [40] | Observational, interviews, thematic analysis | 28 handoff observations, 3 interviews | General medical unit | 7 |
| Chaboyer, 2009 [41] | Intervention: Standard bedside handoff guideline; interviews, survey | Interview sample size unclear; 6 months post: 27 surveys | General medical and stroke/rehabilitation | 6 |
| Mascioli, 2009[42] | Interviews and surveys | Sample size unclear | Acute care nursing staff | 4 |
| Average Score | 9.6 | |||
Quality Scoring System for Handoff Research Studies, maximum score=16
Table 2. Physician Handoff Studies.
| Paper | Study Type | Sample and Size | Acute care setting | Score$ |
|---|---|---|---|---|
| Flanagan, 2009 [4] | Surveys, interviews, content analysis | 63 surveys; 18 interviews, 1264 formal computer-based handoff documents | General medicine and medical intensive care | 13 |
| Ye, 2007 [43] | Observational, post-handoff interviews, survey, content analysis | 914 handoffs observed; 707 post-handoff interviews, 50 surveys | Emergency department | 12 |
| Salerno, 2009 [44] | Intervention: computer-based handoff; survey | Pre: 186 surveys; Post: 130 surveys | General medicine units | 11.5 |
| Gakhar, 2010 [45] | Intervention: handoff curriculum and checklist; observations, surveys, and content analysis | Pre: 25 surveys, 100 handoff observations, 28 formal written sign-outs; Post: 12 surveys, 61 observations, 74 formal written sign-outs | Internal medicine and emergency medicine | 11.5 |
| Pickering, 2009 [46] | Intervention: Computer-based handoff; Handoff information recall score | Pre: 93 handoff information recall scores; Post: 42 information recall scores | Surgical/medical intensive care unit | 11.5 |
| Apker, 2009 [47] | Observational, discourse analysis | 15 audio-recorded telephone handoffs | Emergency department | 11 |
| Lee, 1996 [48] | RCT Intervention: Handoff card; survey | Intervention: 138 surveys; Control: 114 surveys | Cardiovascular medicine unit | 11 |
| Van Eaton 2004[49] | Iterative computer-based handoff system design, survey, focus groups | 31 surveys, focus groups with 28 residents | Resident inpatient and consult services | 11 |
| Kochendorfer 2010 [50] | Intervention: computer-based handoff; survey | Pre: 53 surveys; Post: 62 surveys | Internal Medicine | 11 |
| Horwitz, 2009 [1] | Observational, content analysis | 88 audio-taped handoffs, 84 interviews | Internal medicine residents | 10.5 |
| Chu, 2009 [51] | Intervention: Structured handoff; surveys | Pre: 72 surveys; Post: 65 surveys | General medicine unit | 10 |
| Frank, 2005 [52] | Documentation review | 74 typed sign-outs (Microsoft Word documents) | Pediatric | 9.5 |
| Ferran, 2008 [53] | Intervention: paper-based handoff sheet; audit content analysis | Pre: 48 formal written handoff sheets; Post: 55 formal written handoff sheets | Orthopedic surgery | 9.5 |
| Alem, 2008 [54] | Intervention: paper-based handoff toolkit; Pilot, observations, content analysis | Pilot: 15 handoff observations; Pre: 12 handoff observations; Post: 12 handoff observations | General medical and emergency department | 9.5 |
| Ram, 1992 [55] | Intervention: computer-based handoff; survey | Pre: 16 surveys; Post: 7 surveys; Cohort: 16 surveys | Family Practice Residency Inpatient Service | 8.5 |
| Nabors, 2010 [56] | Intervention: computer-based attending supervision of resident handoff; survey | Post: 24 residents surveys, 8 attending surveys | General medicine service | 8 |
| Solet, 2005 [57] | Observational, thematic analysis | 4 hospital resident handoff processes | Residency program in 4 acute care hospitals | 6 |
| Cheah, 2005 [10] | Intervention: computer-based handoff; survey, content analysis | Post: 14 surveys, 14 formal computer-based handoff documents | General surgical and vascular units | 5 |
| Average Score | 10 | |||
Quality Scoring System for Handoff Research Studies, maximum score=16
The analysis of the 36 nursing and physician handoff studies resulted in a total of 95 handoff information elements. The nursing list consisted of 78 of these handoff information elements and the physician list consisted of 61 of these handoff information elements. Therefore, there were 44 interdisciplinary (i.e., overlapping) information elements that were present in both the nursing and physician lists (see Tables 3 and 4). The elements that did not overlap are specified in Tables 3 and 4 as the nursing-only and physician-only data. Many of the information elements are at varying levels of detail due to the varying levels of detail reported in the literature and differences between nursing and physician handoff.
Table 3. Continuity of Care Document (CCD) Section Coding of Discipline Specific and Interdisciplinary Handoff Information Elements.
| CCD Sections | Nurse only data | Physician only data | Interdisciplinary data |
|---|---|---|---|
| 1. Personal Information | Patient name; Patient age; Patient date of birth; Patient sex | ||
| 2. Payers | Insurance status | ||
| 3. Advance Directives | Consent forms | Code status | |
| 4. Support | Family contact information | ||
| 5. Functional Status | Neurological status; Cardiovascular status; Respiratory status; Gastrointestinal status; Genitourinary status; Skin integrity; Activities of Daily Living; Hygiene/oral care; Mobilization precautions; Safety; Sleep; Psychological/emotional status | Physical exam findings; Baseline status | Diet; Mobility; Patient's condition; Condition/Plan of care trend; Specialty specific key physiologic parameters (e.g., critical care measurements, sepsis status, APACHE risk scale) |
| 6. Problems | Symptoms | Reason for admission/transfer; Active/Current problems/diagnosis | |
| 7. Social History | Occupation; Marital status; Smoking; Alcohol; Religion; Living situation | Patient race | Social concerns; Language/interpreter needed |
| 8. Alerts | Isolation status | Allergies | |
| 9. Medications | Medication times | Home medications | Active medication list; Antibiotics; Intravenous infusions |
| 10. Equipment | Lines and invasive devices; Telemetry | ||
| 11. Vital Signs | Patient height; Patient body mass index | Patient weight; Vital signs | |
| 12. Results | Blood type; Blood glucose | Cultures | Laboratory Data; Test/procedure results |
| 13. Procedures | Treatments and times; Wound care/dressing | Post-op day | Diagnostic/therapeutic procedures & dates |
| 14. Encounters | Admission information and date/hospital day | ||
| 15. Plan of care | Patient preferences | Need for and urgency of review; Prognosis; Rationale of primary team | Plan; Tasks/To-dos; Pending results and procedures; Discharge planning/Disposition; Advice/anticipatory guidance; Short-term concerns/clinical judgments/instincts/comments |
| 16. Health Care Providers | Team name/color; Medical Service | Clinicians involved in case; Physician contact information | |
| Total Information elements | 28 | 13 | 35 |
Table 4. Hospital Handoff (HH) Coding Developed for Discipline Specific and Interdisciplinary Handoff Information.
| HH codes developed for handoff information elements not present in any Continuity of Care Document Sections | |||
|---|---|---|---|
| HH Code | Nurse only data | Physician only data | Interdisciplinary data |
| 1. Admission demographics | Property accompanying patient | Patient's hospital MRN; Patient floor/bed number; Logistic/management issues | |
| 2. Fluid Balance | Intake and output/hydration status | ||
| 3. Education | Patient or family education | ||
| 4. Updates | Time handoff document updated | Significant events during last shift/overnight | |
| HH codes developed for handoff information elements present in multiple Continuity of Care Document Sections | |||
|---|---|---|---|
| HH Code | Nurse only data | Physician only data | Interdisciplinary data |
| 5. Pain management | Pain; Patient Controlled Analgesia/Epidural | ||
| 6. Orders | Physician orders; Protocols | ||
| 7. Psychosocial concerns | Psychosocial concerns | Sensitive or confidential information | |
| 8. Anticoagulation status | Anticoagulation status | ||
| 9. Prophylaxis | Prophylaxis | ||
| 10. Hospital course | Hospital course/summary/current history | ||
| 11. Past medical/surgical history | Past medical/surgical history | ||
| 12. Consultations | Consultations | ||
| Total Information Elements | 6 | 4 | 9 |
The purposes of the nursing studies ranged from explicitly examining handoff information content to studying the quality and effectiveness of the handoff process. Similarly, the methods used ranged from collecting and analyzing audio-recordings of nursing handoffs and the documentation referenced by nurses during a handoff to field observations of the handoff process. Studies that included the analysis of audio-recordings and documentation provided results that reflected a greater level of detail of the content discussed by nurses during handoff. Although the purpose of each study and data collection and analysis methods differed, results included two types of handoff information content: 1) general handoff information elements that include a breadth of possible patient information, such as problems, procedures, treatments, and clinical judgments, and 2) specific handoff information elements that may include in-depth knowledge about a patient problem or care issue, such as skin integrity, respiratory status, fluid intake and output and activities of daily living. However, the organization and level of detail of handoff information elements differed between the nursing studies. For example, Lamond et al., listed fluid input and fluid output as separate items; however, our analysis of all the nursing studies determined that fluid input and output was discussed during handoff as one clinical concept and, therefore, was included in the list as one information unit. Furthermore, many studies did not include definitions of handoff terms or used different terminology to categorize the same clinical concept. For example, the terms resuscitation status, code status and advance directives appeared in different nursing studies and were categorized as one handoff information unit, code status, in our list.
The purposes of the physician studies ranged from analyzing the type of information content handled by resident physicians during handoff for the purpose of developing a computer-based handoff system [49] to analyzing the accuracy of information contained in resident physicians' handoff sheets [52]. The results of the studies differed in their reported level of detail of handoff information; however, all of the physicians' studies included general (e.g., physical exam findings, symptoms, prognosis) and specific handoff information elements. Examples of some of the specific handoff information elements that differed from the nursing information elements were: insurance status, anticoagulation status, and prophylaxis. Different terms that reflected the same clinical concept were used in the physician literature, such as code status and advance directive, and if-then contingency planning and anticipatory guidance. However, the term to-do list was consistently used throughout the physician studies.
3.2. CCD Framework
Overall, 16 section codes from the CCD standard were useful for categorizing 80% (76/95) of all information elements (overlapping and discipline-specific) (see Table 3). A comparable 79% (35/44) of interdisciplinary elements and 80% (41/51) of all discipline-specific elements (i.e., nurse-only and physician-only) were captured by the CCD. Twelve new codes, referred to as Hospital Handoff (HH) codes, were developed to categorize the remaining 19 information elements that did not fit into the CCD standard or those that fit into multiple codes and were therefore too ambiguous to classify in the CCD (see Table 4). Interdisciplinary handoff information elements accounted for 46% of the total information elements (44/95) and were categorized into 15 codes from the CCD standard and 7 HH codes. The 34 nursing specific information elements (36% of total) were categorized into 9 codes from the CCD standard and 4 HH codes. Finally, the 17 physician specific information elements (18% of total) were categorized into 9 codes from the CCD standard and 4 HH codes (see tables 3 and 4). Family history and immunizations were the only CCD section standards that were not used.
The HH codes, admission demographics, fluid balance, education, and updates contain information that was not addressed in the major sections of the CCD, but existed in the hospital handoff literature (see Table 4). The information elements pain management, orders, psychosocial concerns, anticoagulation status, prophylaxis, hospital course, past medical/surgical history, and consultations each belonged to multiple CCD sections. Therefore, for consistency in categorizing the handoff information elements and preventing ambiguity in the coding, each of these elements was identified as a new HH section.
4. Discussion
This systematic review examined the content and structure of nurse and physician handoff information from peer reviewed publications. Eighteen nursing handoff studies and 18 physician handoff studies were reviewed. The nursing studies and the physician studies had a comparable range and mean of quality scores. A lack of standardization of key data elements required for information exchange and information overload have been cited as reasons that EHRs are less able to support coordination between clinicians and across settings [58]. There were 78 information elements identified in the nursing handoff list and 61 information elements in the physician handoff list. There were 44 information elements present in both, indicating a 46% overlap between nurse and physician handoff information elements for hospitalized patients. This suggests that a core set of data elements could be shared for patient handoff and interdisciplinary views within the EHR while also preserving discipline-specific handoff elements.
4.1. Interdisciplinary differences in handoff information
One challenge of standardizing handoff information, highlighted by the findings of this study, is the variation in clinical practice between disciplines and settings within the hospital. For example, physical exam findings was an information unit in the physician list; however, the nursing handoff element list contained more explicit categories that captured physical exam findings. These nursing list categories were: neurological status, cardiovascular status, respiratory status, gastrointestinal status, genitourinary status, and skin integrity. Attempting to structure the physical exam-related handoff information elements according to one standard for nurses and physicians may not ideally serve the needs of either discipline.
In addition to differences in the level of information granularity, some clinical concepts between disciplines fell into different categories or had different implications, especially related to the scope of clinical duties and responsibility. An example was the data element of Patient Controlled Analgesia in the nursing handoff element list. Patient controlled analgesia (PCA) delivers pain medication through an intravenous line when a patient pushes a button attached to the PCA pump, up to a maximum amount that is ordered by the physician and programmed into the PCA pump by the nurse. PCA did not appear explicitly in the physician handoff element list, although it may be mentioned in a discussion of the patient's medications. In contrast, for the nurse, a PCA is more than a pain intervention; the nurses' monitoring of the PCA pump's recorded history indicates if a patient's pain is adequately controlled by assessing the frequency with which the patient pushed the button for pain medication to be delivered compared to the maximum set amount. Furthermore, because the pain medication is a narcotic, it is required by protocol that during handoff, the out-going nurse and on-coming nurse verify and co-sign the documentation of PCA pump settings and the amount of pain medication remaining in the intravenous bag. Another example was that the request for the rationale by the primary team for a given clinical decision is an element of the physician handoff list and is not present in the nursing handoff list. However, other nursing literature suggests that when nurses were not aware of medical residents' rationale for care decisions they have purposefully delayed the implementation of the orders to allow time to assess that the order was entered as intended and was appropriate and safe [59, 60]. Therefore, the overlap between nurses and physicians regarding handoff information for hospitalized patients may be greater than is indicated by a literature review exclusively focused on handoff.
4.2. Interdisciplinary handoff element list and its role in establishing common ground
Verbal discussions (e.g., handoff) and documentation (e.g., in an EHR) are complementary tools to establish and maintain common ground in the clinical setting [13, 15, 16]. This study categorized information into an interdisciplinary list of handoff information elements that are essential to both nursing and physician handoff. These handoff information elements contain practical information (e.g., bed location), background information (e.g., reason for admission), planning information (e.g., to-do lists, discharge plan), and safety information (e.g., code status, allergies) that may be necessary for the establishment of common ground between disciplines. The process of entering and reviewing information in the patient chart enables clinicians to establish common ground, which is a pre-requisite for effective interdisciplinary communication [13]. Instead of relying solely on verbal discussions, the establishment of common ground could be augmented through the implementation of a standardized interdisciplinary handoff list in an EHR. This could facilitate interdisciplinary communication and decrease information loss, interruptions, and errors of omission [13, 61].
4.3. “Missing” inpatient handoff elements in the CCD standard
The CCD was designed primarily for the purpose of facilitating information transfer for inter-institutional handoffs or handoffs between outpatient healthcare providers [23]. Thus, as expected, we found that several of the information elements present in the nursing, physician, and interdisciplinary handoff lists either didn't fit into the standard CCD sections, or fit in to multiple sections and they were, therefore, too ambiguous to classify. The “HH” coded items shown in Table 4 did not fit neatly into the standard CCD sections, and they reveal insight into some of the unique handoff information needs that exist for hospital clinicians. Some of these items are understandably not typically part of the CCD as they refer to events and activities on a much finer temporal scale than would be necessary in the outpatient setting. Examples include continuous tallies of a patient's fluid status in terms of inputs and outputs, and significant events either from the previous night or over the entire hospital course.
Other items that didn't fit into the typical CCD sections were related to clinical characteristics of patients that, depending on the clinical problem, are less likely to be of immediate concern when handing off patients in the outpatient setting when patients are not acutely ill. Examples include anticoagulation status, prophylaxis (e.g., gastrointestinal or deep vein thrombosis), and pain management. Finally, the collaborative and interdisciplinary nature of hospital care requires that information regarding “who said what” is included at the time of handoff, hence the need to discuss physician orders (for nurses) or various consultants and their recommendations. In the outpatient setting, handoff is generally from one provider to another, which may explain why there is no specific section that corresponds to this type of information. Finally, there are administrative and institutional-specific types of information that are required given the complexity of the hospital setting. This information would not typically be contained in a CCD, such as the patient's floor and bed number, hospital-specific identification codes such as a Medical Record Number, and an inventory of personal property that arrived with the patient. The CCD standard covered 80% of all the information elements that are necessary for inpatient handoff, and, therefore, suggests that the addition of the new HH codes to the C83 HITSP CDA Content Modules and the extension of the CCD may be an important starting place for the development of a transition of care document standard for hospitalized patients. Alternatively, the development of a new constraint on CDA specified for “Inpatient Handoff” that uses the CDA elements that were covered by the CCD (80% of the inpatient handoff elements) plus the HH codes (20% of the inpatient handoff elements) may be appropriate. An inpatient handoff CDA constraint may simplify the delineation of required elements (i.e., interdisciplinary elements) versus optional elements (i.e., discipline or specialty specific elements), provide its own set of use cases, and facilitate the development of standards-based handoff modules for EHR vendors.
4.4. EHR support of overlapping interdisciplinary handoff information and the CCD standard
This study demonstrated considerable overlap between disciplines and suggests that a centralized interdisciplinary module in an EHR to support patient handoff is feasible. Furthermore, the CCD framework, with modifications for hospital-based handoff, may be useful to organize nursing, physician, and interdisciplinary handoff lists for the purpose of standardization. Given the demonstrated overlap of core concepts between the nursing and physician handoff elements it is logical to have this information centralized to decrease redundancy, information loss and propagation of information inaccuracy. Furthermore, having many clinicians looking at the same information may increase the quality, accuracy and interdisciplinary nature of clinical information. Specialized handoff applications in the EHR improve care transitions and it is recognized that specialized clinical units or services have distinct information needs [23]. For example, one interdisciplinary element was specialty specific key physiologic parameters which, in an intensive care unit, may include data such as hemodynamic measurements, mechanical ventilator settings, sepsis status, and the patient's APACHE risk score. EHRs with a custom handoff utility to support these specialty areas have been shown to improve workflow efficiency and improved patient care [3]. Therefore, such a module may be tailored to a specialty clinical unit or service, however, this does not address handoffs between units [62].
A challenge of standardizing handoff information is that there are many types and situational varieties of handoff. An EHR handoff tool based on a list of handoff elements that is organized using the CCD standard may automatically pull information from disparate parts of the EHR and allow clinicians to select and deselect categories, and to save their preferences. Based on the literature reviewed we recommend that the lists of nursing, physician, and interdisciplinary handoff elements and the extended CCD framework, or development of a new inpatient handoff CDA constraint, are used to standardize and organize handoff tools and to improve the establishment of common ground and interdisciplinary communication among nurses and physicians. When possible, these lists of handoff data elements should be automatically pulled from the EHR to ensure consistency of data across all handoffs. Handoff data elements that are amendable to structuring within the EHR (e.g., medications) may complement handoff elements specific to a discipline or setting that is more appropriately communicated in a narrative form (e.g., patient preferences). Therefore, a structured narrative, where unstructured text and coded handoff data elements are fused into a single document, may be appropriate to ensure data consistency for handoff documentation [63]. [63]
5. Conclusion
This systematic review examined handoff information and identified a 46% overlap between nurse and physician handoff lists for hospitalized patients. The CCD was useful for coding 80% of the hospital handoff information, and 12 hospital handoff codes were developed to categorize the remaining 20%. The different levels of granularity between disciplines for some handoff information indicates that standardizing all handoff information according to the same structure for nurses and physicians may not be appropriate. However, the interdisciplinary handoff element lists contained practical information, background information, planning information, and safety information that could be standardized and organized using the CCD framework in a centralized interdisciplinary EHR module. This may facilitate the establishment of common ground and interdisciplinary communication and decrease information loss, interruptions, and errors of omission [13, 61]. We recommend that the standardization of EHR handoff tools use the extended CCD sections and comprise interdisciplinary modules that incorporate the interdisciplinary handoff information elements into structured narrative documentation and that further research investigates the impact of providing standardized interdisciplinary handoff information to clinicians at the point of care.
Acknowledgments
Dr. Collins is supported by the National Library of Medicine (T15 LM 007079). The work was also supported by Wireless Informatics for Safe and Evidence-based APN Care (D11 HP07346) and the Center for Evidence-based Practice in the Underserved (P30NR010677).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Horwitz L, Moin T, Krumholz H, Wang L, Bradley E. What are covering doctors told about their patients? Analysis of sign-out among internal medicine house staff. Qual Saf Health Care. 2009;18:248–55. doi: 10.1136/qshc.2008.028654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arora V, Johnson J. A model for building a standardized hand-off protocol. Jt Comm J Qual Patient Saf. 2006;32:646–55. doi: 10.1016/s1553-7250(06)32084-3. [DOI] [PubMed] [Google Scholar]
- 3.Van Eaton EG, Horvath KD, Lober WB, Rossini AJ, Pellegrini CA. A randomized, controlled trial evaluating the impact of a computerized rounding and sign-out system on continuity of care and resident work hours. J Am Coll Surg. 2005;200:538–45. doi: 10.1016/j.jamcollsurg.2004.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Flanagan ME, Patterson ES, Frankel RM, Doebbeling BN. Evaluation of a physician informatics tool to improve patient handoffs. J Am Med Inform Assoc. 2009;16:509–15. doi: 10.1197/jamia.M2892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stein D, Wrenn J, Johnson S, Stetson P. Signout: a collaborative document with implications for the future of clinical information systems. AMIA Annu Symp Proc. 2007:696–700. [PMC free article] [PubMed] [Google Scholar]
- 6.Petersen L, Orav E, Teich J, O'Neil A, Brennan T. Using a computerized sign-out program to improve continuity of inpatient care and prevent adverse events. Jt Comm J Qual Improv. 1998;24:77–87. doi: 10.1016/s1070-3241(16)30363-7. [DOI] [PubMed] [Google Scholar]
- 7.National Research Council . Computational Technology for Effective Health Care: Immediate Steps and Strategic Directions. Washington, D.C.: The National Academies Press; 2009. [PubMed] [Google Scholar]
- 8.Brokel JM, Harrison MI. Redesigning care processes using an electronic health record: a system's experience. Jt Comm J Qual Patient Saf. 2009;35:82–92. doi: 10.1016/s1553-7250(09)35011-4. [DOI] [PubMed] [Google Scholar]
- 9.Benham-Hutchins MM, Effken JA. Multi-professional patterns and methods of communication during patient handoffs. Int J Med Inform. 2010;79:252–67. doi: 10.1016/j.ijmedinf.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 10.Cheah LP, Amott DH, Pollard J, Watters DA. Electronic medical handover: towards safer medical care. Med J Aust. 2005;183:369–72. doi: 10.5694/j.1326-5377.2005.tb07086.x. [DOI] [PubMed] [Google Scholar]
- 11.Groah L. Hand offs--a link to improving patient safety. AORN J. 2006;83:227–30. doi: 10.1016/s0001-2092(06)60243-3. [DOI] [PubMed] [Google Scholar]
- 12.Patel VL, Zhang J, Yoskowitz NA, Green R, Sayan OR. Translational cognition for decision support in critical care environments: a review. J Biomed Inform. 2008;41:413–31. doi: 10.1016/j.jbi.2008.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coiera E. When conversation is better than computation. J Am Med Inform Assoc. 2000;7:277–86. doi: 10.1136/jamia.2000.0070277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collins S, Bakken S, Vawdrey D, Coiera E, Currie L. Model development for EHR interdisciplinary information exchange of ICU common goals. Int J Med Inform. 2010 doi: 10.1016/j.ijmedinf.2010.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hutchins E. Cognition in the Wild. Cambridge, MA: MIT Press; 1995. [Google Scholar]
- 16.Collins S, Bakken S, Vawdrey D, Coiera E, Currie L. Discuss Now, Document Later: CIS/CPOE Perceived to be a ‘Shift Behind’ in the ICU. Stud Health Technol Inform. 2010;160:178–82. [PMC free article] [PubMed] [Google Scholar]
- 17.Hutchins E. How a cockpit remembers its speeds. Cognitive Science. 1995;19:265–288. [Google Scholar]
- 18.Zhang J, Patel VL, Johnson K, Smith J, Malin J. Designing Human-Centered Distributed Information Systems. IEEE Intelligent Systems. 2002;17:42–47. [Google Scholar]
- 19.Riesenberg LA, Leitzsch J, Massucci JL, Jaeger J, Rosenfeld JC, Patow C, Padmore JS, Karpovich KP. Residents' and attending physicians' handoffs: a systematic review of the literature. Acad Med. 2009;84:1775–87. doi: 10.1097/ACM.0b013e3181bf51a6. [DOI] [PubMed] [Google Scholar]
- 20.Riesenberg LA, Leitzsch J, Little BW. Systematic review of handoff mnemonics literature. Am J Med Qual. 2009;24:196–204. doi: 10.1177/1062860609332512. [DOI] [PubMed] [Google Scholar]
- 21.Dolin R, Alschuler L, Boyer S, Beebe C, Behlen F, Biron P, Shabo Shvo A. HL7 Clinical Document Architecture, Release 2. J Am Med Inform Assoc. 2006;13:30–9. doi: 10.1197/jamia.M1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.HL7 continuity of care document, a healthcare IT interoperability standard, is approved by balloting process and endorsed by healthcare IT standards panel. Available at http://www.hl7.org/documentcenter/public/pressreleases/20070212.pdf.
- 23.HITSP website . C32-HITSP summary documents using HL7 continuity of care document (CCD) component. 2009. In. [Google Scholar]
- 24.ASTM Standard E2369 . West Conshohocken, PA: ASTM International; 2005. ASTM E2369 - 05e1 Standard Specification for Continuity of Care Record (CCR) In. www.astm.org. [DOI] [Google Scholar]
- 25.Patterson P, Blehm R, Foster J, Fuglee K, Moore J. Nurse information needs for efficient care continuity across patient units. J Nurs Adm. 1995;25:28–36. doi: 10.1097/00005110-199510000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Berkenstadt H, Haviv Y, Tuval A, Shemesh Y, Megrill A, Perry A, Rubin O, Ziv A. Improving handoff communications in critical care: utilizing simulation-based training toward process improvement in managing patient risk. Chest. 2008;134:158–62. doi: 10.1378/chest.08-0914. [DOI] [PubMed] [Google Scholar]
- 27.Miller A, Scheinkestel C, Limpus A, Joseph M, Karnik A, Venkatesh B. Uni- and Interdisciplinary Effects on Round and Handover Content in Intensive Care Units. Human Factors. 2009;51:339–353. doi: 10.1177/0018720809338188. [DOI] [PubMed] [Google Scholar]
- 28.Chaboyer W, McMurray A, Wallis M. Bedside nursing handover: a case study. Int J Nurs Pract. 2010;16:27–34. doi: 10.1111/j.1440-172X.2009.01809.x. [DOI] [PubMed] [Google Scholar]
- 29.Lamond D. The information content of the nurse change of shift report: a comparative study. J Adv Nurs. 2000;31:794–804. doi: 10.1046/j.1365-2648.2000.01349.x. [DOI] [PubMed] [Google Scholar]
- 30.McFetridge B, Gillespie M, Goode D, Melby V. An exploration of the handover process of critically ill patients between nursing staff from the emergency department and the intensive care unit. Nurs Crit Care. 2007;12:261–9. doi: 10.1111/j.1478-5153.2007.00244.x. [DOI] [PubMed] [Google Scholar]
- 31.Welsh C, Flanagan M, Ebright P. Barriers and facilitators to nursing handoffs: Recommendations for redesign. Nurs Outlook. 2010;58:148–54. doi: 10.1016/j.outlook.2009.10.005. [DOI] [PubMed] [Google Scholar]
- 32.McLane S, Esquivel A, Turley JP. Developing a taxonomy and an ontology of nurses' patient clinical summaries. Stud Health Technol Inform. 2009;146:352–7. [PubMed] [Google Scholar]
- 33.Staggers N, Jennings BM. The content and context of change of shift report on medical and surgical units. J Nurs Adm. 2009;39:393–8. doi: 10.1097/NNA.0b013e3181b3b63a. [DOI] [PubMed] [Google Scholar]
- 34.Currie J. Improving the efficiency of patient handover. Emerg Nurse. 2002;10:24–7. doi: 10.7748/en2002.06.10.3.24.c1064. [DOI] [PubMed] [Google Scholar]
- 35.Lally S. An investigation into the functions of nurses' communication at the inter-shift handover. J Nurs Manag. 1999;7:29–36. doi: 10.1046/j.1365-2834.1999.00095.x. [DOI] [PubMed] [Google Scholar]
- 36.Sexton A, Chan C, Elliott M, Stuart J, Jayasuriya R, Crookes P. Nursing handovers: do we really need them? J Nurs Manag. 2004;12:37–42. doi: 10.1111/j.1365-2834.2004.00415.x. [DOI] [PubMed] [Google Scholar]
- 37.Nelson B, Massey R. Implementing an electronic change-of-shift report using transforming care at the bedside processes and methods. J Nurs Adm. 2010;40:162–8. doi: 10.1097/NNA.0b013e3181d40dfc. [DOI] [PubMed] [Google Scholar]
- 38.Fenton W. Developing a guide to improve the quality of nurses' handover. Nurs Older People. 2006;18:32–6. doi: 10.7748/nop.18.11.32.s24. quiz 37. [DOI] [PubMed] [Google Scholar]
- 39.Block M, Ehrenworth J, Cuce V, Ng'ang'a N, Weinbach J, Saber S, Milic M, Urgo J, Sokoli D, Schlesinger M. The tangible handoff: a team approach for advancing structured communication in labor and delivery. Jt Comm J Qual Patient Saf. 2010;36:282–7. 241. doi: 10.1016/s1553-7250(10)36044-2. [DOI] [PubMed] [Google Scholar]
- 40.Sherlock C. The patient handover: a study of its form, function and efficiency. Nurs Stand. 1995;9:33–6. doi: 10.7748/ns.9.52.33.s34. [DOI] [PubMed] [Google Scholar]
- 41.Chaboyer W, McMurray A, Johnson J, Hardy L, Wallis M, Sylvia Chu FY. Bedside handover: quality improvement strategy to “transform care at the bedside”. J Nurs Care Qual. 2009;24:136–42. doi: 10.1097/01.NCQ.0000347450.90676.d9. [DOI] [PubMed] [Google Scholar]
- 42.Mascioli S, Laskowski-Jones L, Urban S, Moran S. Improving handoff communication. Nursing. 2009;39:52–5. doi: 10.1097/01.NURSE.0000345252.78133.67. [DOI] [PubMed] [Google Scholar]
- 43.Ye K, McD Taylor D, Knott JC, Dent A, MacBean CE. Handover in the emergency department: deficiencies and adverse effects. Emerg Med Australas. 2007;19:433–41. doi: 10.1111/j.1742-6723.2007.00984.x. [DOI] [PubMed] [Google Scholar]
- 44.Salerno SM, Arnett MV, Domanski JP. Standardized sign-out reduces intern perception of medical errors on the general internal medicine ward. Teach Learn Med. 2009;21:121–6. doi: 10.1080/10401330902791354. [DOI] [PubMed] [Google Scholar]
- 45.Gakhar B, Spencer A. Using direct observation, formal evaluation, and an interactive curriculum to improve the sign-out practices of internal medicine interns. Acad Med. 2010;85:1182–8. doi: 10.1097/ACM.0b013e3181da8370. [DOI] [PubMed] [Google Scholar]
- 46.Pickering BW, Hurley K, Marsh B. Identification of patient information corruption in the intensive care unit: using a scoring tool to direct quality improvements in handover. Crit Care Med. 2009;37:2905–12. doi: 10.1097/CCM.0b013e3181a96267. [DOI] [PubMed] [Google Scholar]
- 47.Apker J, Mallak LA, Applegate EB, 3rd, Gibson SC, Ham JJ, Johnson NA, Street RL., Jr Exploring emergency physician-hospitalist handoff interactions: development of the Handoff Communication Assessment. Ann Emerg Med. 2009;55:161–70. doi: 10.1016/j.annemergmed.2009.09.021. [DOI] [PubMed] [Google Scholar]
- 48.Lee LH, Levine JA, Schultz HJ. Utility of a standardized sign-out card for new medical interns. J Gen Intern Med. 1996;11:753–5. doi: 10.1007/BF02598991. [DOI] [PubMed] [Google Scholar]
- 49.Van Eaton EG, Horvath KD, Lober WB, Pellegrini CA. Organizing the transfer of patient care information: the development of a computerized resident sign-out system. Surgery. 2004;136:5–13. doi: 10.1016/j.surg.2004.04.018. [DOI] [PubMed] [Google Scholar]
- 50.Kochendorfer K, Morris L, Kruse R, Ge B, Mehr D. Attending and resident physician perceptions of an EMR-generated rounding report for adult inpatient services. Fam Med. 2010;42:343–9. [PubMed] [Google Scholar]
- 51.Chu ES, Reid M, Schulz T, Burden M, Mancini D, Ambardekar AV, Keniston A, Albert RK. A structured handoff program for interns. Acad Med. 2009;84:347–52. doi: 10.1097/ACM.0b013e3181970829. [DOI] [PubMed] [Google Scholar]
- 52.Frank G, Lawler L, Jackson A, Steinberg T, Lawless S. Resident Miscommunication: Accuracy of the Resident Sign-out Sheet. Journal for Healthcare Quality Online. 2005 [Google Scholar]
- 53.Ferran NA, Metcalfe AJ, O'Doherty D. Standardised proformas improve patient handover: Audit of trauma handover practice. Patient Saf Surg. 2008;2:24. doi: 10.1186/1754-9493-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alem L, Joseph M, Kethers S, Steele C, Wilkinson R. Information environments for supporting consistent registrar medical handover. HIM J. 2008;37:9–25. doi: 10.1177/183335830803700102. [DOI] [PubMed] [Google Scholar]
- 55.Ram R, Block B. Signing out patients for off-hours coverage: comparison of manual and computer-aided methods. Proc Annu Symp Comput Appl Med Care. 1992:114–8. [PMC free article] [PubMed] [Google Scholar]
- 56.Nabors C, Peterson S, Lee W, Mumtaz A, Shah T, Sule S, Gutwein A, Forman L, Eskridge E, Wold E, Stallings G, Burak K, Karmen C, Behar C, Carosella C, Yu S, Kar K, Gennarelli M, Bailey-Wallace G, Goldberg R, Guo G, Frishman W. Experience with faculty supervision of an electronic resident sign-out system. Am J Med. 2010;123:376–81. doi: 10.1016/j.amjmed.2009.12.010. [DOI] [PubMed] [Google Scholar]
- 57.Solet DJ, Norvell JM, Rutan GH, Frankel RM. Lost in translation: challenges and opportunities in physician-to-physician communication during patient handoffs. Acad Med. 2005;80:1094–9. doi: 10.1097/00001888-200512000-00005. [DOI] [PubMed] [Google Scholar]
- 58.O'Malley A, Grossman J, Cohen G, Kemper N, Pham H. Are electronic medical records helpful for care coordination? Experiences of physician practices. J Gen Intern Med. 2010;25:177–85. doi: 10.1007/s11606-009-1195-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Baggs JG, Schmitt MH. Nurses' and Resident Physicians' Perceptions of the Process of Collaboration in an MICU. Research in Nursing and Health. 1997;20:71–80. doi: 10.1002/(sici)1098-240x(199702)20:1<71::aid-nur8>3.0.co;2-r. [DOI] [PubMed] [Google Scholar]
- 60.Lingard L, Espin S, Evans C, Hawryluck L. The rules of the game: interprofessional collaboration on the intensive care unit team. Critical Care. 2004;8:R403–R408. doi: 10.1186/cc2958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Collins S, Currie L, Patel VL, Bakken S, Cimino JJ. Multitasking by clinicians in the context of CPOE and CIS use. Medinfo. 2007;12:958–62. [PubMed] [Google Scholar]
- 62.Cohen M, Hilligoss P. The published literature on handoffs in hospitals: deficiencies identified in an extensive review. Qual Saf Health Care. 2010 doi: 10.1136/qshc.2009.033480. [DOI] [PubMed] [Google Scholar]
- 63.Johnson S, Bakken S, Dine D, Hyun S, Mendonça E, Morrison F, Bright T, Van Vleck T, Wrenn J, Stetson P. An electronic health record based on structured narrative. J Am Med Inform Assoc. 2008;15:54–64. doi: 10.1197/jamia.M2131. [DOI] [PMC free article] [PubMed] [Google Scholar]