Abstract
Objectives
Examining the impact of homebound status of older persons in Israel on mortality, mental health, and function, future homebound status, and institutionalization.
Design
Cross-sectional and longitudinal analysis using existing datasets of a national survey.
Participants
Analyzed sample was drawn from a representative cohort of older persons in Israel including 1191 participants (age; M=83.10, SD=5.3) in the first wave of the Cross-Sectional and Longitudinal Aging Study (CALAS) and 621 participants in the second wave of the study.
Measurements
Homebound status, health, function, environment, mental health, distal events, mortality. Instruments included Activities Daily Living (ADL), Instrumental Activities of Daily Living (IADL), Orientation-Memory-Concentration Test, and Center for Epidemiological Studies Depression Scale. Mortality data were recorded from the Israeli National Population Registry.
Results
Homebound participants had a significantly higher risk for mortality than their non-homebound counterparts, even after controlling for background variables, health and function (risk ratio=1.33, confidence interval 1.08-1.63). In cross-sectional analysis, homebound status was related to depressed affect even after controlling for demographics, health and function. In longitudinal analysis, homebound status predicted future depressed affect, ADL and IADL difficulties when controlling for demographics and health, but only IADL prediction was statistically significant when baseline levels of the outcome variable were entered into the regression.
Conclusion
The results highlight the detrimental effects of homebound status, thus underscoring the importance of improving prevention of this state, of interventions to assist those who are homebound, and of future research to examine the efficacy and coverage of services to this population.
Keywords: older persons, homebound status, mental health, mortality, depressed affect
INTRODUCTION
Being homebound has been reported to be significantly associated with more depressive symptoms, higher prevalence of cognitive impairments, and greater functional limitations, in comparison with persons who went outdoors more often.1-4 Cohort studies1-3, 5indicate that homebound older people are less healthy and more disabled than their counterparts. According to longitudinal data4 a lower frequency of going outdoors is linked to greater incident disability and lower recovery of persons aged 65 or older at two-year follow-up. Kono, Kai, Sakato, and Rubenstein6 reported that the functional capacity of participants who went outdoors less than once a week decreased over time more than it did in older persons who went outdoors more frequently. Finally, cross-sectional findings indicated that lower mobility among older persons, as measured by the Life Space Assessment (LSA), was associated with depression, cognitive impairment, lower self-perception of health, taking more medications, and having more comorbidity and more symptoms.7
The goal of the current study is to examine the impact of homebound status on mortality, mental health, and function, future homebound status, and institutionalization, in a cohort of older persons in Israel for which data of 3.5 year functional follow-up as well as 20 year mortality follow-up were available. Understanding the consequences of homebound status will inform the need for intervention and policy for homebound persons.
Homebound status isolates a person and restricts access to goods and services. Thus, it may affect the function and mental health of the homebound person. In our conceptual model, demographics, health, function, mental health, environment, and distal events all serve as predictors of homebound status which in turn, affects mortality, function, and mental health outcomes. In this paper we address the right side of the model, i.e., outcomes of homebound status, whereas in a companion paper (unpublished manuscript, Tel Aviv University, Israel) we examine the predictors.
The specific question is: What is the impact of being homebound, that is, how do outcomes of mortality, mental health, functional status, future homebound status and institutionalization differ among those who were homebound and those who were not?
METHODS
Participants and Procedure
The sample included participants from the Cross-Sectional and Longitudinal Aging Study (CALAS). The CALAS is a multidimensional survey of a random sample of the older Jewish population in Israel, stratified by age group (75-79, 80-84, 85-89, 90-94), gender, and place of birth (Asia-Africa, Europe-America, Israel). This study examines two waves of data collection, the first collected during 1989-1992 and the second during 1993-1994, with an average of 3.5 years between them. More information regarding the CALAS appears in various publications.8-15
Interviews were conducted in participants’ homes after they had signed informed consent. The CALAS was approved for ethical treatment of human participants by the Institutional Review Board of the Chaim Sheba Medical Center in Israel.
The present analyses include 1191 self-respondent participants aged 75-94. The mean age was 83.10 (SD=5.3). The longitudinal analyses included all of the participants from the first wave of the CALAS who were alive and located at the second wave of data collection (n=721), of whom 621 were able to provide self report.
Measures
Background
Socio-demographics included gender, age, place of birth (Israel, Middle East/North Africa, or Europe/America), marital status, having children, education (number of years of education), and financial status (whether the participant had income additional to the basic National Insurance pension).
Homebound Status
In line with Ganguli et al.,3 being homebound was defined as going out of the house once a week or less, and was measured by asking participants how often they went outside of their homes (more than once a week, or once a week or less).
Health
Subjective health (terrible, okay, good, or excellent); Medications: all medications taken by participants as inspected and counted by the interviewer (range 0–8); BMI - the interviewer measured the weight and height of the participants, and their Body Mass Index was calculated (< 22 = underweight, 22-25, 25-30, >30 = obese).16 Comorbidity was assessed by the number of diseases the participant had been diagnosed with from a list of 18 chronic diseases (e.g., diabetes, cancer; range: 0-18).
Function
ADL (Activities of Daily Living)17 was assessed by asking respondents to rate their difficulty in performing seven different vital activities (crossing a small room, washing, dressing, eating, grooming, transferring, and toileting) on a scale from “no difficulty” (0) to “complete disability” (3). The sum score ranged from 0 to 21. Cronbach’s alpha coefficient of this measure was 0.88. IADL (Instrumental Activities of Daily Living)18 is a scale which consists of seven items, each rating the difficulty of performing different activities (preparing meals, daily shopping, shopping for clothes, doing light housekeeping, doing heavy housework, taking the bus, and doing laundry) on a scale similar to that used for ADL (range: 0-21). Alpha coefficient of this measure was 0.87. Cognitive difficulties were measured by the Orientation-Memory-Concentration (OMC) Test.19Seven items tested basic cognitive functions such as knowing the current date and time, remembering a name and an address, and counting backwards. Errors were multiplied by prefixed weights and added up (range: 0-28). Alpha coefficient was 0.73.
Environment
Having stairs and/or an elevator. The respondents were asked if they could enter their home without climbing any stairs and whether they had an elevator in their building. These two questions were combined to calculate the variable of “having stairs and/or no elevator”.
Mental Health
Depressed affect was measured by the Center for Epidemiological Studies Depression Scale (CESD).20 Respondents rated the frequency of experiencing 20 depressive symptoms in the past month on a scale from 0 (not at all) to 3 (almost every day). The items expressed negative affect, lack of well-being, psychosomatic reactions, and interpersonal distress. The score was the respondents’ mean rating after reversing four positive items (range: 0-3). Alpha coefficient was 0.88. Item 10 was removed from the analysis and was treated as a separate variable that measures loneliness. Loneliness was measured through a single question asking whether the respondent had felt lonely in the last month. The score ranged from 0 to 3 (no, sometimes, most of the time, or almost everyday).
Distal Events
Number of traumatic events was assessed by asking participants whether they had experienced any traumatic events which influenced their lives (range 0-3).
Mortality Follow-up
Mortality data within 20 years from the date of the first interview were recorded from the Israeli National Population Registry. Of the original sample, 59 participants were still alive at the 20-year follow up.
Statistical Analysis
The impact of homebound status on 20 year mortality was tested using Cox regression models. In order to examine whether homebound status had an effect beyond that of the variables which may cause homebound status, three models were examined: 1) homebound status alone as a predictor of mortality; 2) examining the impact of homebound status on mortality after controlling for stratification variables (age, gender, origin); 3) demographics, health and function were entered prior to examining the impact of homebound status.
Impact of homebound status on future mental health, function, institutionalization, and homebound status. The role of homebound status at wave 1 in predicting institutionalization and homebound status at wave 2 was examined using chi-square analyses. The impact of homebound status on depressed affect, ADL and IADL was examined using linear regression analyses in order to control for background and health variables at wave 1. Two models were analyzed for each dependent variable, the first controlling for demographic and health variables, and the second controlling for function variables in addition to those of demographic and health. Finally, because wave 1 sample was larger than wave 2 sample, thus providing more power to the analysis, we examined the association of homebound status at wave 1 with concurrent depressed affect at wave 1, while controlling for background and health variables.
RESULTS
As explicated in a companion paper (unpublished manuscript, Tel Aviv University, Israel), homebound and non-homebound participants differed on demographic, health and functional variables at wave 1 of the CALAS. Specifically, homebound participants, in comparison to non-homebound participants, were significantly older (M= 85.05 vs. 82.62, SD=5.23 and 5.23, respectively), more likely to be female (68% vs. 39%), and more likely to be born in Israel (32% vs. 30%) or in the Middle East/North Africa (38.5% vs. 31%) than in Europe (29.5% vs. 39%). Homebound persons (in the CALAS cohort) presented higher levels of depressed affect than their counterparts, were more lonely, encountered significantly more difficulties in ADLs and in IADLs, and performed significantly worse on the OMC test. They had more children, attained lower levels of education, and were worse off financially. They took significantly more medications, reported a worse subjective health, and were more likely to be either obese or underweight in comparison to their non-homebound counterparts.
In terms of mortality, homebound participants had a significantly higher risk for mortality than their counterparts (risk ratio [RR]=1.64, confidence interval [CI]:1.42-1.90, χ2= 40.35, p < .001, -2 log likelihood= 14082.49). Controlling for the stratification variables of the sample did not change the impact of homebound status on mortality (Table 1). Furthermore, after controlling for background, health, and function variables, homebound status remained a significant predictor of mortality (RR= 1.33, CI=1.08-1.63; Table 1). The findings concerning the relationship between homebound status and 20 year mortality are illustrated in the survival curves in Figure 1.
Table 1.
Cox Regression Predicting Mortality in 20 Years from Date of First Interview by Homebound Status
| Impact after controlling for survey stratification variables | Impact after controlling for background, health and function variables | |||
|---|---|---|---|---|
| Exp(b) | CI | Exp(b) | CI | |
| Background | ||||
| Age | 1.07*** | 1.05-1.08 | 1.05*** | 1.04-1.07 |
| Gender (female=0, male=1) | 1.32*** | 1.17-1.50 | 1.58*** | 1.33-1.88 |
| Origin (east) | .88 | .76-1.02 | .77** | .64-.93 |
| Origin (west) | 1.15 | .99-1.33 | 1.06 | .91-1.02 |
| Years of education | 1.00 | .99-1.02 | ||
| Additional income | .87* | .75-1.00 | ||
| Marital status | .92 | .79-1.08 | ||
| Had children | .65** | .52-.84 | ||
| Health | ||||
| Comorbidity | 1.03 | .99-1.06 | ||
| Function | ||||
| ADL | 1.07** | 1.03-1.11 | ||
| IADL | 1.03** | 1.01-1.04 | ||
| Cognitive difficulties | 1.01 | .99-1.02 | ||
| Environment | ||||
| Having stairs and no elevator | 0.93 | .80-1.08 | ||
| Mental health | ||||
| Depressive affect | .97 | .81-1.18 | ||
| Distal events | ||||
| Traumatic events | .98 | .90-1.06 | ||
| χ2 of step | χ2= 152.52*** | χ2= 78.20*** | ||
| -2 log likelihood | 13970.32 | 10811.55 | ||
| Homebound (vs. non-homebound) | 1.68*** | 1.44-1.97 | 1.33** | 1.08-1.63 |
| χ2 of step | χ2 = 39.80*** | χ2= 7.16** | ||
| -2 log likelihood | 13930.53 | 10804.195 | ||
p < .05,
p < .01,
p < .001.
Figure 1.
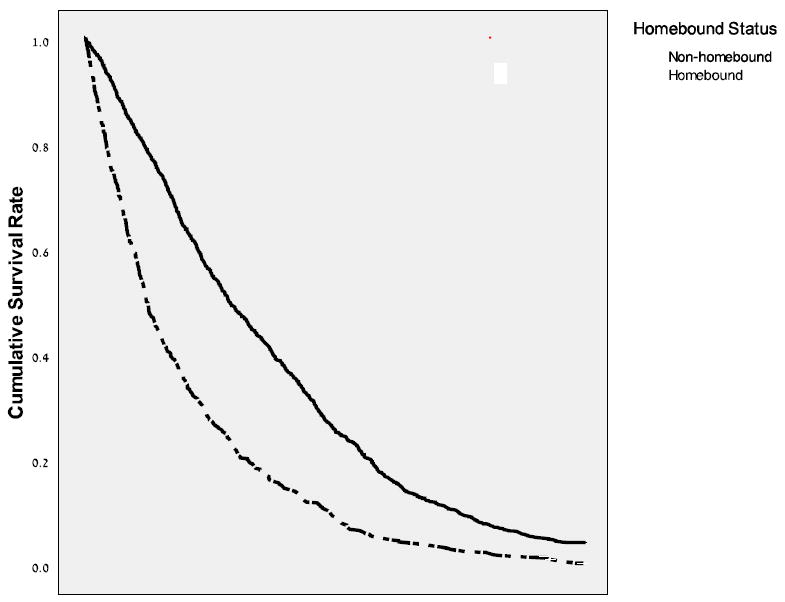
Cumulative Survival Rates by Years, for Homebound vs. Non-Homebound Participants (N=1191)
Self-respondent participants who were homebound at wave 1 were less likely than their non-homebound counterparts to be self-respondent at wave 2 (71.3% vs. 82.3%, χ2 (1) =7.85; p < .01), and were more likely to be homebound also at wave 2 (67% vs. 21%, χ2 (1) =90; p < .001). Additionally, although they had higher rates of institutionalization as compared to non-homebound participants, this difference only approached statistical significance (p =.07).
An examination of wave 1 predictors of depressed affect and functional status at wave 2 (Table 2) shows that homebound status is a significant predictor of depressed affect and worse function at wave 2 even when controlling for demographics and health at wave 1. When controlling also for ADL, IADL, depressed affect and cognitive difficulties at wave 1, the impact on depressed affect is no longer statistically significant and the impact on ADL only approaches significance. However, the impact of homebound status on IADL remains highly significant even after controlling for IADL at wave 1 and other function assessments (Table 2).
Table 2.
Longitudinal Prediction of the Impact of Homebound Status: Multiple Regression Results (Standardized Beta Coefficients) Predicting Depressed Affect and Functional Status at Wave 2 by Homebound Status after Controlling for Demographic and Health variables (Model 1), and Demographics, Health, and Function Variables (Model 2), at Wave 1.
| Dependent var. | Depressed Affect | ADL | IADL | |||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Demographics | ||||||
| Age | -.026 | -.040 | .146* | .071+ | .246*** | .168** |
| Gender | -.152** | -.113* | -.016 | .004 | -.091 | -.058 |
| Origin (east) | .137** | .078 | -.013 | -.046 | .029 | -.015 |
| Origin (west) | .092* | .058 | -.008 | -.008 | -.055 | -.059 |
| Marital status | -.018 | .016 | -.036 | -.003 | .012 | .049 |
| Years of education | -.157*** | -.106* | -.047 | -.007 | -.038 | .018 |
| Additional income | -.008 | .035 | -.018 | -.022 | .000 | .008 |
| Had children | -.032 | -.029 | -.034 | -.044 | -.050 | -.059 |
| Health | ||||||
| Comorbidity | .266*** | .110** | .163*** | .063 | 1.53*** | .046 |
| Function | ||||||
| ADL | .008 | .139** | .036 | |||
| IADL | .038 | .308*** | .390*** | |||
| Cognitive difficulties | .009 | .066 | .060 | |||
| Environment | ||||||
| Having stairs and no elevator | -.047 | -.012 | -.021 | |||
| Mental health | ||||||
| Depressed affect | .346*** | -.014 | .086* | |||
| Distal events | ||||||
| Traumatic events | .036 | -.010 | -.062 | |||
| Homebound status | .081* | .020 | .218*** | .075+ | .267*** | .110** |
| R2 of demographics | .117*** | .117*** | .063*** | .063*** | .139*** | .139*** |
| R2 of health Wave 1 | .042*** | .042*** | .030*** | .030*** | .027*** | .027*** |
| R2 of function Wave 1 | .112*** | .163*** | .200*** | |||
| R2 of homebound Wave 1 | .006* | 0 | .042*** | .004 | .063*** | .009** |
| R2 | .165 | .271 | .135 | .260 | .229 | .375 |
Note. n =621.
p < .05,
p < .01,
p < .001
1 > p > 0.5
Since the sample size of wave 2 was much smaller than that of wave 1, the lack of impact on depressed affect at wave 2 could be attributed to a low power. In order to understand whether homebound status was an independent predictor of depressed affect at time 1, we undertook a cross-sectional regression (using forced entry) explaining depressed affect at wave 1 by all demographics, health and function at wave 1. In the cross sectional analysis (N=1191) homebound status was a significant predictor of depressed affect even after controlling for demographic, health, and functional variables (ADL, IADL and cognitive difficulties) as well as distal (past trauma) and environmental variables (results available from authors). Significant predictors included older age, being of eastern or western origin, not married, less education, less financial resources, more comorbidity, ADL and IADL difficulties, having experienced significant past trauma, and homebound status (results available from authors).
DISCUSSION
A unique finding in this study involves the relation between homebound status and mortality risk. As far as we know, the current study is the first to report mortality risk of homebound status. We measured the impact of homebound status by analyzing 20-year mortality rate, and found that homebound status of older persons was related to increased long term mortality, even beyond the predictive effects of the demographic, health and function risk factors. Additional outcomes of mental health and function were measured using CESD, ADL and IADL.
Homebound status was associated with low levels of mental health. Previous findings support this concern as homebound persons were found to be more depressed than other old-old persons.3, 21 In this paper, homebound status was related to higher levels of depressed affect at wave 2, change from self-report status at wave 1 to proxy report status at wave 2, and a greater likelihood of being homebound at wave 2. Homebound status was a longitudinal predictor of depressed affect when controlling for demographics and health, but did not remain a significant predictor when depressed affect at time 1 was controlled for. However, in relation to depressed affect at wave 1, homebound status was a significant concurrent predictor even after controlling for background, health and functional status variables. It is therefore possible that a larger longitudinal sample is needed to establish the influence of homebound status on depression. Similarly, trauma was only predictive of depressed affect in the cross sectional data. This could be due to the lower power of the longitudinal data or to the fact that only those who had survived the trauma until at least age 75 were included in the study.
The finding of homebound persons being more depressed than non-homebound persons is especially interesting since in a companion paper (unpublished manuscript, Tel Aviv University, Israel) on the predictors of homebound status, depressed affect was found to be a significant predictor of homebound status in a multi-variate cross-sectional analysis. This raises the notion of a possible vicious cycle, where more depressed persons are more likely to become homebound, a condition which further aggravates their depressed affect. Similarly, the relationship between homebound status and functional status also emerges as bi-directional; Functional status predicts homebound status in a multi-variate analysis controlling for confounding variables (unpublished manuscript, Tel-Aviv University, Israel) and homebound status appears to affect future functional status even when taking background, health and baseline functional status into account. Nonetheless, current longitudinal findings may be limited in inferring causality due to having only two time points. Future studies should examine more points in time and examine models of recursive vs. one-direction effects. Another possible avenue for future research involves multi-dimensional conceptualizations of being homebound, exploring the combined effect of capacity, volition, and resources, as well as actual activity.
The study underscores the general low level of mental health of the homebound population. As this finding is corroborated by previous evidence from other countries,2, 3 it may be that the low rates (3%) of depression reported in one study among homebound older persons in Israel22 may involve under-detection, be due to the different age groups under study and the use of a non-representative sample, or be due to a different definition of homebound status relating to home confinement which precludes access to the family physician in the clinic. Our finding of elevated depressed affect among the homebound underlines the importance of providing homebound older persons with resources to allow them to get out of the house and calls attention to the need for health and social agencies to address the pain, depressed affect, and general low mental health of those persons. Finally, studies are needed to examine different psychosocial and environmental interventions which address both the mental health and mobility of homebound persons.
Acknowledgments
The two waves of the Cross-Sectional and Longitudinal Aging Study (CALAS) were funded by grants from the U.S. National Institute on Aging (R01-5885-03 and R01-5885-06) to the Department of Clinical Epidemiology at the Chaim Sheba Medical Center.
Sponsor’s role Funding sources had no role in study design; in subject recruitment; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Author contributions Prof. Cohen-Mansfield designed the study, and directed it, including statistical analysis and write-up. Prof. Dov Shmotkin consulted regarding the data analysis and participated in the write-up. Prof. Haim Hazan participated in the write-up. All authors have contributed in a meaningful manner.
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
References
- 1.Lindesay J, Thompson C. Housebound elderly people: Definition, prevalence and characteristics. Int J Geriatr Psychiatry. 1993;8:231–237. [Google Scholar]
- 2.Farquhar M, Bowling A, Grundy E, et al. Elderly housebound: Changes over time. Nurs Stand. 1993;8:26–31. doi: 10.7748/ns.8.1.26.s31. [DOI] [PubMed] [Google Scholar]
- 3.Ganguli M, Fox A, Gilby J, et al. Characteristics of rural homebound older adults: A community-based study. J Am Geriatr Soc. 1996;44:363–371. doi: 10.1111/j.1532-5415.1996.tb06403.x. [DOI] [PubMed] [Google Scholar]
- 4.Fujita K, Fujiwara Y, Chaves PHM, et al. Frequency of going outdoors as a good predictors for incident disability of physical function as well as disability recovery in community-dwelling older adults in rural Japan. J Epidemiol. 2006;16:261–270. doi: 10.2188/jea.16.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inoue K, Matsumoto M. Homebound status in a community-dwelling elderly population in Japan. Asia Pac J Public Health. 2001;13:109–115. doi: 10.1177/101053950101300209. [DOI] [PubMed] [Google Scholar]
- 6.Kono A, Kai I, Sakato C, et al. Frequency of going outdoors: A predictor of functional and psychosocial change among ambulatory frail elders living at home. J Gerontol A Biol Sci Med Sci. 2004;59:M275–280. doi: 10.1093/gerona/59.3.m275. [DOI] [PubMed] [Google Scholar]
- 7.Allman RM, Sawyer P, Roseman JM. The UAB Study of Aging: Background and insights into life-space mobility among older Americans in rural and urban settings. Aging Health. 2006;2:417–429. [Google Scholar]
- 8.Ben-Ezra M, Shmotkin D. Predictors of mortality in the old-old in Israel: The Cross-Sectional and Longitudinal Aging Study. J Am Geriatr Soc. 2006;54:906–911. doi: 10.1111/j.1532-5415.2006.00741.x. [DOI] [PubMed] [Google Scholar]
- 9.Benyamini Y, Blumstein T, Lusky A, et al. Gender differences in the self-rated health-mortality association: Is it poor self-rated health that predicts mortality or excellent self-rated health that predicts survival? Gerontologist. 2003;43:396–405. doi: 10.1093/geront/43.3.396. [DOI] [PubMed] [Google Scholar]
- 10.Blumstein T, Shmotkin D, Eyal N, et al. A longitudinal evaluation of medication use among the old-old population in Israel. Res Aging. 2008;30:55–73. [Google Scholar]
- 11.Shmotkin D, Blumstein T, Modan B. Beyond keeping active: Concomitants of being a volunteer in old-old age. Psychol Aging. 2003;18:602–607. doi: 10.1037/0882-7974.18.3.602. [DOI] [PubMed] [Google Scholar]
- 12.Shmotkin D, Blumstein T, Modan B. Tracing long-term effects of early trauma: A broad-scope view of Holocaust survivors in late life. J Consult Clin Psychol. 2003;71:223–234. doi: 10.1037/0022-006x.71.2.223. [DOI] [PubMed] [Google Scholar]
- 13.Walter-Ginzburg A, Blumstein T, Chetrit A, et al. Social factors and mortality in the old-old in Israel: The CALAS study. J Gerontol B Psychol Sci Soc Sci. 2002;57:S308–S318. doi: 10.1093/geronb/57.5.s308. [DOI] [PubMed] [Google Scholar]
- 14.Walter-Ginzburg A, Shmotkin D, Blumstein T, et al. A gender-based dynamic multidimensional longitudinal analysis of resilience and mortality in the old-old in Israel: The Cross-sectional and Longitudinal Aging Study (CALAS) Soc Sci Med. 2005;60:1705–1715. doi: 10.1016/j.socscimed.2004.08.023. [DOI] [PubMed] [Google Scholar]
- 15.Walter-Ginzburg A, Guralnik JM, Blumstein T, et al. Assistance with personal care activities among the old-old in Israel: A national epidemiological study. J Am Geriatr Soc. 2001;49:1176–1184. doi: 10.1046/j.1532-5415.2001.49234.x. [DOI] [PubMed] [Google Scholar]
- 16.Alfaro-Acha A, Ostir GV, Markides KS, et al. Cognitive status, body mass index, and hip fracture in older Hispanic adults. J Am Geriatr Soc. 2006;54:1251–1255. doi: 10.1111/j.1532-5415.2006.00820.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Katz S, Downs T, Cash H, Grotz R. Progress in development of the index of ADL. Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 18.Lawton M, Brody E. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- 19.Katzman R, Brown T, Fuld P, et al. Validation of a short orientation-memory-concentration test of cognitive impairment. Am J Psychiatry. 1983;140:734–739. doi: 10.1176/ajp.140.6.734. [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 21.Choi NG, McDougall GJ. Comparison of depressive symptoms between homebound older adults and ambulatory older adults. Aging Ment Health. 2007;11:310–322. doi: 10.1080/13607860600844614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vinker S, Naker S, Weingarten MA. Network motIGPR. Home visits to the housebound patient in family practice: a multicenter study Israeli General Practice Research Network. Isr Med Assoc J. 2000;2:203–206. [PubMed] [Google Scholar]


