Abstract
BACKGROUND AND OBJECTIVES:
Saudi Arabia has a high prevalence of hereditary hemoglobin disorders. Data has been collected by the Saudi Premarital Screening and Genetic Counseling Program on the prevalence of sickle cell disease and β-thalassemia but the outcomes were not quantified. We used six years of premarital screening data to estimate the burden of sickle disease and β-thalassemia over the program period and to assess the frequency of at-risk marriage detection and prevention.
DESIGN AND SETTING:
Retrospective review, premarital couples attending premarital and genetic counseling clinics with marriage proposals between 2004 and 2009.
METHODS:
Blood samples obtained from all couples with marriage proposals between 2004 and 2009 were tested for sickle cell disease and β-thalassemia. Test results were shared with all examinees and genetic counseling was offered for all at-risk couples. Marriage certificates were issued irrespective of the results and compliance with medical advice was voluntary.
RESULTS:
Out of all men and women examined, 70 962 (4.5%) and 29 006 (1.8%) were carriers or cases of sickle cell disease and β-thalassemia, respectively. While the prevalence of sickle cell disease was constant between 2004 and 2009 (average 45.1 per 1000 examined persons, P=.803), the prevalence of β-thalassemia steadily decreased from 32.9 to 9.0 per 1000 examined persons (P<.001). The frequency of at-risk couples decreased by about 60% between 2004 and 2009 (from 10.1 to 4.0 per 1000 examined persons, P<.001). The frequency of voluntary cancellation of marriage proposals among at-risk couples showed more than 5-fold increase between 2004 and 2009 (from 9.2% to 51.9%, P<.001). The eastern region had 58% of all detected at-risk marriages and showed the greatest decline in detection and increase in prevention over time compared to other regions of Saudi Arabia.
CONCLUSION:
Six years of premarital screening in Saudi Arabia markedly reduced the number of at-risk marriages, which may considerably reduce the genetic disease burden in Saudi Arabia in the next decades.
Inherited hemoglobin disorders (hemoglobinopathies) are predominantly single-gene autosomal recessive disorders that result in production of structurally abnormal hemoglobin variants (sickle-cell disease) or a reduction in the synthesis of structurally normal globin (β-thalassemia).1 Sickle-cell disease and β-thalassemia affect as much as 5% of the world's population, constituting a major public health problem in certain parts of the world including the Mediterranean area and the Middle East.2 Saudi Arabia is well-known for its high prevalence of hereditary blood disorders. In a study conducted in Saudi Arabia and published in June 2007, 4.20% of the participants had sickle cell trait, 0.26% had sickle cell disease, and 3.22% had b-thalassemia trait, while 0.07% had β-thalassemia disease.3 Certain cultural factors in Saudi Arabia, including the high frequency of consanguineous marriages (exceeding 55%), the large family size, and the high paternal and maternal ages may contribute to the high prevalence of sickle-cell disease and β-thalassemia in Saudi Arabia.4–6
Premarital screening for genetic diseases is superior to neonatal screening since the former is primary prevention while the latter is secondary or tertiary prevention.7 Premarital screening can potentially reduce the burden of inherited hemoglobin diseases by reducing the number of high-risk marriages.8,9 This was proven to be beneficial in nearby countries with similar endemicity levels of hemoglobinopathies.10–12 Because of the burden on the healthcare system and effect on the quality of life in patients with sickle-cell disease or β-thalassemia, premarital genetic screening was mandated in Saudi Arabia in 2004.13 All couples with marriage proposals have to be tested for both diseases and get the appropriate counseling (if required) before completing their marriage proposal. The compliance with the counseling recommendation was left voluntary. The outcome of this national program had yet been quantified. We used 6 years of premarital screening data to estimate the burden of sickle-cell disease and β-thalassemia over the program period and to assess the frequency of at-risk marriage detection and prevention.
METHODS
The current report used the national data of the Saudi Premarital Screening and Genetic Counseling (PMSGC) Program. The Saudi population was 22.7 million at the start of the program in 2004 and it reached 25.4 million by 2009.14 The annual number of marriages was close to a quarter of a million at the start of the program, including all 13 administrative regions of Saudi Arabia.
The program was stipulated by law in December 2003 and implemented in February 2004. The mandatory nature of the program was preceded by national debates at the scientific, social, and religious levels and was followed by widespread media advertising. The main program objective was to reduce the prevalence of sickle-cell disease and β-thalassemia by a reduction of the number of at-risk marriages. The program infrastructure consisted of 150 health care reception clinics, 70 laboratories, and 78 genetic counseling clinics covering the country 13 administrative regions.
By late 2003, comprehensive PMSGC program guidelines were distributed to all workers in the program. According to these guidelines, couples with marriage proposals had to report to the nearest health care clinic to apply for premarital certificates. At the health care clinics, the program staff collected basic demographic information, a blood sample (in EDTA anticoagulant), and offered educational materials about the program to the applying couples. Blood samples were then sent to the designated laboratory for testing for sickle cell disease and β-thalassemia using hemoglobin electrophoresis. Other blood tests included a complete blood count, a peripheral blood film, a reticulocyte count, and a sickling test. The results were interpreted in accordance with standard laboratory diagnostic protocols.15,16
Test results were shared with examined couples before issuing the premarital compatibility certificates. The test results sort the individuals of potential couples into free (healthy), carriers (carrying the trait) and cases (having the disease) as regards the genetic make-up of sickle-cell disease and/or β-thalassemia. A safe marriage was declared when both or at least one of the couple were healthy. At-risk marriage was declared when both couples were carriers or cases (or one was a case and the other was a carrier) of sickle-cell disease and/or β-thalassemia. Couples with safe marriage test results were issued instant compatibility certificates while at-risk couples were asked to attend personal genetic counseling meetings before issuing incompatibility certificates. During these meetings the counselors explained to the couple members the potential hazards of their proposed marriages and the voluntary nature of their compliance. The program staff followed-up (by phone call) with at-risk couple members and the Ministry of Justice (responsible for issuing marriage certificates) to verify the marriage proposals among at-risk couples.
It was the responsibility of the 150 health care clinics to collect and manage their own local laboratory data. Each of the 20 health regions were required to collect data from their respective health care clinics and fax standard monthly reports to the Directorate General of Noncommunicable Disease of the Ministry of Health in Riyadh. Aggregate data were used to construct a central database that was used for the current analysis. The prevalence of carriers and/or cases of sickle-cell disease and/or β-thalassemia were expressed per 1000 examined persons and plotted over time. Similarly the frequency of at-risk couples (incompatible certificates per 1000 examined persons and per 100 positive results) and the frequency of voluntary cancellation of marriage proposals (percentage) among at-risk couples were plotted over time. Carrier-case ratio was defined as the ratio of carriers to cases among those who had any positive results for sickle-cell disease and/or β-thalassemia. Significant increasing or decreasing trends were tested using the Extended Mantel-Haenszel chi square test for linear trend. Regional differences in frequency were tested using the chi square test. All P values were two-tailed. A P value <.05 was considered as significant. OpenEpi (version 2.2, Atlanta, GA, USA) and Microsoft Office Excel (2003) were used for all statistical analyses.
RESULTS
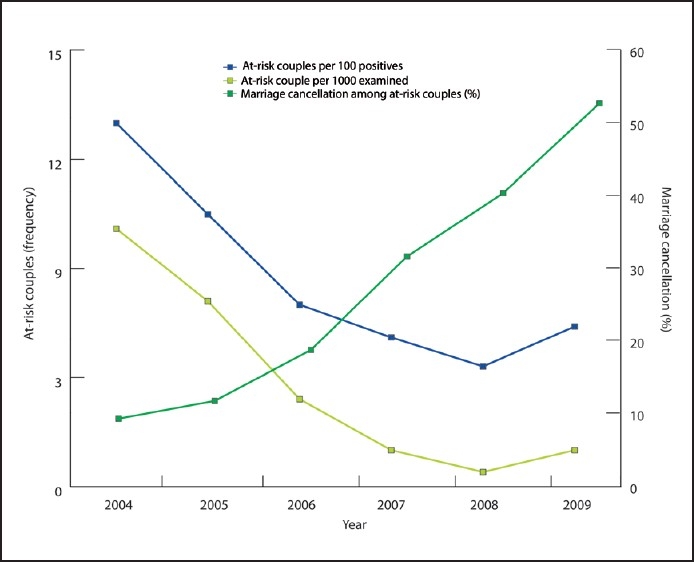
The annual number of men and women examined in the PMSGC program ranged between approximately 242 000 in 2004 and 296 000 in 2009 (Table 1). This represented an annual frequency of 10.9 marriage proposals per 1000 Saudi population. Of 1 572 140 men and women examined between 2004 and 2009, 70 962 (4.5%) were positive (carriers or cases) for sickle cell disease and 29 006 (1.8%) were positive (carriers or cases) for β-thalassemia. The annual prevalence of sickle cell disease was 45.1 (42.4 for carriers and 2.7 for cases) per 1000 examined persons (Table 2). The annual prevalence of β-thalassemia was 18.5 (18.0 for carriers and 0.5 for cases) per 1000 examined persons. While the prevalence of sickle cell disease was constant over the program period (range between 44.2 and 47.1 per 1000 examined persons, P for trend =.803), the prevalence of β-thalassemia steadily decreased from 32.9 to 9.0 per 1000 examined persons between 2004 and 2009, respectively (P for trend <.001,Figure 1).
Table 1.
Premarital Genetic Screening Program between 2004 and 2009 by year in Saudi Arabia
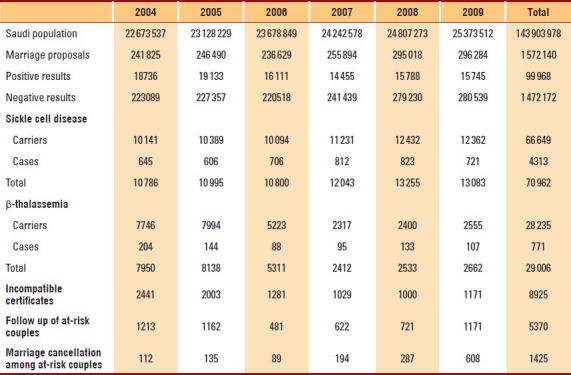
Table 2.
Premarital Genetic Screening Program between 2004 and 2009 by year in Saudi Arabia
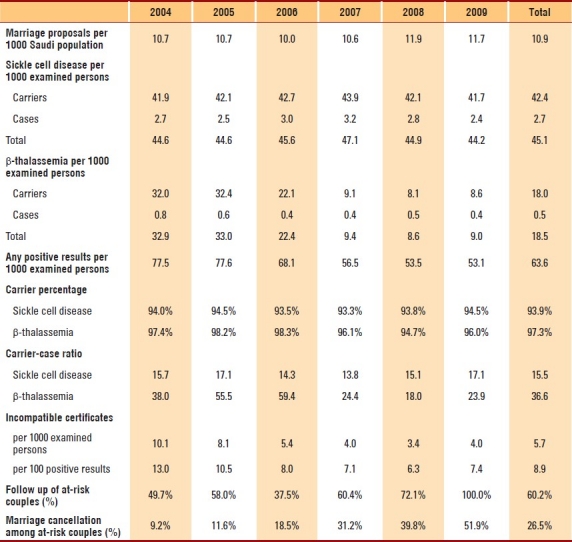
Figure 1.
Annual prevalence of sickle cell disease and β-thalassemia among examined persons in the Premarital Genetic Screening Program between 2004 and 2009 by year in Saudi Arabia.
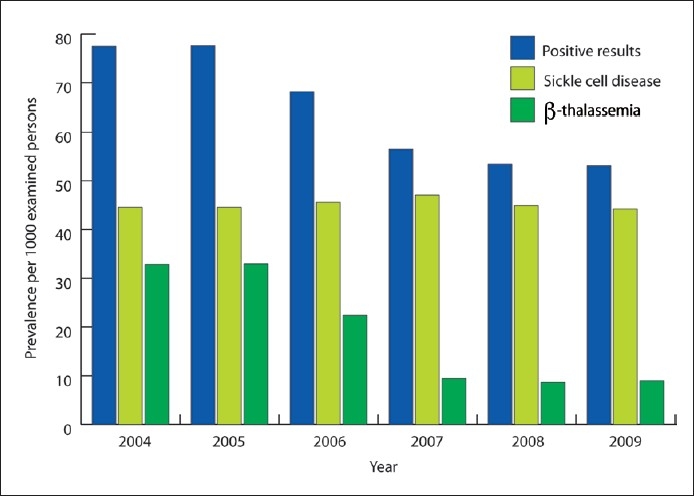
Between 2004 and 2009, a total of 8925 incompatibility certificates were issued because both couples were carriers or cases (or one was a case and the other was a carrier) of sickle-cell disease and/or β-thalassemia (Table 1). The annual frequency of incompatibility certificates was 5.7 per 1000 examined persons and 8.9 per 100 positive results (Table 2). The frequency of at-risk couples (incompatible certificates) decreased by about 60% between 2004 and 2009 (from 10.1 to 4.0 per 1000 examined persons, respectively, P for trend <.001, Figure 2). This represented a 43.1% reduction of issuing incompatibility certificates per 100 positive results (Figure 2). Out of the 8925 who had been issued incompatibility certificates between 2004 and 2009, the staff of PMSGC program was able to follow up the decision of 5370 (60.2%) at-risk couples. Out of the 5370 at-risk couples followed, 1425 (26.5%) cancelled their marriage proposals. The frequency of voluntary cancellation of marriage proposals among followed at-risk couples showed more than a 5-fold increase between 2004 and 2009 (from 9.2% to 51.9%, respectively, P for trend <.001).
Figure 2.
Annual frequency of at-risk couples and frequency of marriage cancellation among at-risk couples in the Premarital Genetic Screening Program between 2004 and 2009 by year in Saudi Arabia.
Compared to other regions of Saudi Arabia, the eastern region had more than a 5-fold higher annual prevalence of positive results for sickle-cell disease and β-thalassemia (193.1 vs 38.1 per 1000 examined persons, P<.001) and about a 7-fold higher annual frequency of issuing incompatibility certificates (20.0 vs 2.9 per 1000 examined persons, P<.001). Moreover, the Eastern region had better overall follow-up of the decision of at-risk couples (68.6% Vs 48.5%, P<.001) and had a lower overall marriage cancellation (22.6% vs 34.3%). Between 2004 and 2009, the eastern region, which had 58% of all detected at-risk marriages, showed a greater decline in issuing incompatible certificates (79% vs 28%, Figure 3) as well as a greater increase in marriage cancellation among followed at-risk couples (8.0 folds vs 1.7 fold) compared to other regions (Figure 4).
Figure 3.
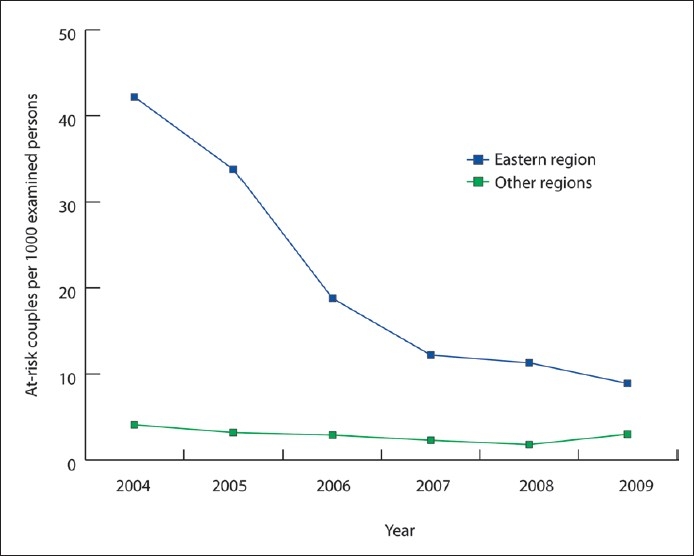
Annual frequency of at-risk couples in the Premarital Genetic Screening Program between 2004 and 2009 by year and geographic regions of Saudi Arabia.
Figure 4.

Annual frequency of marriage cancellation among at-risk couples in the Premarital Genetic Screening Program between 2004 and 2009 by year and geographic regions of Saudi Arabia.
DISCUSSION
The current article reports the impact of six years of national premarital screening and genetic counseling on the prevalence of sickle-cell disease and β-thalassemia as well as the frequency of at-risk marriages in Saudi Arabia. To our knowledge, this is the first study to examine the detection and prevention of at-risk marriages at a national level. Mandating the premarital screening for inherited hemoglobinopathies was long awaited in Saudi Arabia and was preceded by religious and scientific debate.17–20 In this highly conservative population, premarital screening in Saudi Arabia is practically the main preventive measures against inherited hemoglobinopathies.9 Neonatal screening may be of limited importance as it represents only secondary or tertiary prevention.
As expected, the current study showed that Saudi Arabia has a high prevalence of sickle-cell disease (4.5%) and β-thalassemia (1.8%). The majority of these positive results were carriers (93.9% of sickle-cell disease and 97.3% of β-thalassemia). An earlier report covering the first 2 years of the PMSGC program showed a similar prevalence of sickle-cell disease (4.2% carriers and 0.26% cases), but a considerably higher prevalence of β-thalassemia (3.2% carriers and 0.07% cases).16 This can be explained by the considerable reduction (more than 70%) of the prevalence of β-thalassemia in the current study after the second year of the program.
The study shows clearly the success of the PMSGC program in reducing the detection and prevention of at-risk marriages. Detection of at-risk marriages was reduced by about 60% (from 10.1 in 2004 to 4.0 in 2009 per 1000 examined persons). This was mainly driven by a more than 70% reduction of the prevalence of β-thalassemia during the same period. However, It is not clear why sickle-cell disease was essentially constant over the program period.
The completion of 48% of at-risk marriages in 2009 indicates the huge cultural challenges that remain to be addressed by the counselors. Even years after program implementation, the knowledge of premarital screening was good but not adequate.21–23 In the current report, the overall marriage cancellation among at-risk marriages was 26.5% and increased to more than 50% in 2009. In a recent survey (2008), more than 60% of the participants were in favor of canceling at-risk marriages.23 However, in another study among 129 at-risk candidates identified in premarital screening, only 2% cancelled their marriage proposals. In almost half of cases, cultural pressure was the main reason to proceed with marriage.24 An earlier report covering the first 2 years of the PMSGC program showed that only 10% of at-risk couples cancelled their marriage proposals.16 Genetic counseling obtained towards the end of marriage process is not likely to be effective. It has been proposed that screening singles on admission to university prior to any commitment may be preferable than screening immediately before the marriage certificate is issued.22
The Eastern region that had 58% of all detected at-risk marriages during the program period had a lower overall cancellation of at-risk marriages compared to other regions (22.6% vs 34.3%). This may be explained by the fact that cancellation of at-risk marriages at the beginning of the program implementation (2004) was lower in the Eastern region compared to other regions (5% vs 21%). This probably masked the improvement of at-risk marriage prevention in the Eastern region compared to other regions (8.0 fold vs 1.7 fold). Another potential explanation is the higher positivity of sickle-cell disease and/or β-thalassemia in Eastern region compared to other regions (19.3% vs 3.8%), which could make it difficult for at-risk couples to find an alternative socially and suitably safe match.
In addition to the huge efforts already accomplished by the Saudi MOH to prevent at-risk marriages for sickle-cell disease and β-thalassemia, additional efforts are underway. These include increasing the number of specialized health care reception clinics to cover more regions25 as well as connecting all clinics in the country by a state-of-art web-based database software that will enhance instant rate calculation and research. This will overcome the limitation of aggregate data as seen in the current study because there was no access to raw or individual data for analysis. Saudi MOH may enhance the effects of counseling by encouraging couples to seek testing earlier in the marriage process, engage religious figures in counseling, include program information in high school curriculum, allow singles to voluntarily seek genetic testing, and finally augment the help of community figures to publicize the program in media and religious gatherings.
In conclusion, six-year of premarital screening and genetic counseling in Saudi Arabia markedly reduced the number of at-risk marriages, which may considerably reduce the genetic disease burden in Saudi Arabia over the coming decades.
REFERENCES
- 1.Milunsky A, Milunsky J. Genetic Disorders and the Fetus: Diagnosis, Prevention and Treatment.6th ed. Wiley-Blackwell. (6th ed) 2010 [Google Scholar]
- 2.WHO. Fact sheet: Sickle-cell disease and other haemoglobin disorders. 2006. Aug, URL: http://www.who.int/mediacentre/factsheets/fs308/en/index.html .
- 3.Alhamdan NA, Almazrou YY, Alswaidi FM, Choudhry AJ. Premarital screening for b-thalassemia and sickle cell disease in Saudi Arabia. Genet Med. 2007;9:372–7. doi: 10.1097/gim.0b013e318065a9e8. [DOI] [PubMed] [Google Scholar]
- 4.El-Mouzan MI, Al-Salloum AA, Al-Herbish AS, Qurachi MM, Al-Omar AA. Regional variations in the prevalence of consanguinity in Saudi Arabia. Saudi Med J. 2007;28:1881–4. [PubMed] [Google Scholar]
- 5.el-Hazmi MA, al-Swailem AR, Warsy AS, al-Swailem AM, Sulaimani R, al-Meshari AA. Consanguinity among the Saudi Arabian population. J Med Genet. 1995;32:623–6. doi: 10.1136/jmg.32.8.623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Al-Gazali L, Hamamy H, Al-Arrayad S. Genetic disorders in the Arab world. BMJ. 2006;333:831–4. doi: 10.1136/bmj.38982.704931.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tamhankar PM, Agarwal S, Arya V, Kumar R, Gupta UR, Agarwal SS. Prevention of homozygous beta b-thalassemia by premarital screening and prenatal diagnosis in India. Prenat Diagn. 2009;29:83–8. doi: 10.1002/pd.2176. [DOI] [PubMed] [Google Scholar]
- 8.Alswaidi FM, O′Brien SJ. Premarital screening programmes for haemoglobinopathies, HIV and hepatitis viruses: review and factors affecting their success. J Med Screen. 2009;16:22–8. doi: 10.1258/jms.2008.008029. [DOI] [PubMed] [Google Scholar]
- 9.Meyer BF. Strategies for the prevention of hereditary diseases in a highly consanguineous population. Ann Hum Biol. 2005;32:174–9. doi: 10.1080/03014460500075217. [DOI] [PubMed] [Google Scholar]
- 10.Karimi M, Jamalian N, Yarmohammadi H, Askarnejad A, Afrasiabi A, Hashemi A. Premarital screening for beta-thalassaemia in Southern Iran: options for improving the programme. J Med Screen. 2007;14:62–6. doi: 10.1258/096914107781261882. [DOI] [PubMed] [Google Scholar]
- 11.Keskin A, Turk T, Polat A, Koyuncu H, Saracoglu B. Premarital screening of beta-b-thalassemia trait in the province of Denizli, Turkey. Acta Haematol. 2000;104:31–3. doi: 10.1159/000041066. [DOI] [PubMed] [Google Scholar]
- 12.Al-Arrayed S, Hafadh N, Al-Serafi S. Premarital counselling: an experience from Bahrain. East Mediterr Health J. 1997;3:415–9. [Google Scholar]
- 13.El-Hazmi MA. Pre-marital examination as a method of prevention from blood genetic disorders.Community views. Saudi Med J. 2006;27:1291–5. [PubMed] [Google Scholar]
- 14.Saudi Ministry of Health. A Review of Health Situation, The Annual Health statistics book. 2004. URL: http://www.moh.gov.sa/statistics/index.html .
- 15.Wild BJ, Bain BJ. Dacie & Lewis practical hematology. 9th edition. London: Churchill Livingstone; 2001. Investigation of abnormal hemoglobins and b-thalassemia; pp. 231–68. [Google Scholar]
- 16.Al-Odaib AN, Abu-Amero KK, Ozand PT, Al-Hellani AM. A new era for preventive genetic programs in the Arabian Peninsula. Saudi Med J. 2003;24:1168–75. [PubMed] [Google Scholar]
- 17.Al-Khaldi YM, Al-Sharif AI, Sadiq AA, Ziady HH. Attitudes to premarital counseling among students of Abha Health Sciences College. Saudi Med J. 2002;23:986–90. [PubMed] [Google Scholar]
- 18.Albar MA. Counselling about genetic disease: an Islamic perspective. East Mediterr Health J. 1999;5:1129–33. [PubMed] [Google Scholar]
- 19.Albar MA. Ethical considerations in the prevention and management of genetic disorders with special emphasis on religious considerations. Saudi Med J. 2002;23:627–32. [PubMed] [Google Scholar]
- 20.Samavat A, Modell B. Iranian national thalassaemia screening programme. BMJ. 2004;329:1134–7. doi: 10.1136/bmj.329.7475.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Al-Aama JY. Attitudes towards mandatory national premarital screening for hereditary hemolytic disorders. Health Policy. 2010 doi: 10.1016/j.healthpol.2010.02.009. [DOI] [PubMed] [Google Scholar]
- 22.Al-Aama JY, Al-Nabulsi BK, Alyousef MA, Asiri NA, Al-Blewi SM. Knowledge regarding the national premarital screening program among university students in western Saudi Arabia. Saudi Med J. 2008;29:1649–53. [PubMed] [Google Scholar]
- 23.Al Sulaiman A, Suliman A, Al Mishari M, Al Sawadi A, Owaidah TM. Knowledge and attitude toward the hemoglobinopathies premarital screening program in Saudi Arabia: population-based survey. Hemoglobin. 2008;32:531–8. doi: 10.1080/03630260802508384. [DOI] [PubMed] [Google Scholar]
- 24.Al Sulaiman A, Saeedi M, Al Suliman A, Owaidah T. Postmarital follow-up survey on high risk patients subjected to premarital screening program in Saudi Arabia. Prenat Diagn. 2010;30:478–81. doi: 10.1002/pd.2507. [DOI] [PubMed] [Google Scholar]
- 25.Al-Shahrani M. Steps toward the prevention of hemoglobinopathies in the kingdom of Saudi Arabia. Hemoglobin. 2009;33(Suppl 1):S21–4. doi: 10.3109/03630260903346437. [DOI] [PubMed] [Google Scholar]


