Abstract
BACKGROUND AND OBJECTIVES:
Childhood and adolescent anxiety is generally associated with a varied somatic symptom pattern thought to reflect autonomic system activity. Few studies have examined the autonomic characteristics of generalized anxiety disorder (GAD). This omission is at odds with contemporary models of autonomic cardiovascular control. The current study aimed to find differences in autonomic functions between children with a diagnosis of childhood anxiety disorder and a control group using a case-control design.
DESIGN AND SETTING:
A cross sectional experimental study conducted in the years 2004-2005 in the psycho-physiology lab of a tertiary care multi-speciality teaching hospital.
METHODS:
Assessments were carried out using a semistructured interview, K-SADS (Schedule for Affective Disorders and Schizophrenia for Children and Adolescents); STAIC (State and Trait Anxiety Inventory for Children); CDRS (Childhood Depression Rating Scales); SCARED (Self-Report for Childhood Anxiety–Related Disorders). Autonomic reactivity was tested using the standard battery of tests.
RESULTS:
There were differences between 34 children and adolescents (age range, 8-18 years) with a diagnosis of childhood anxiety disorder and a control group of 30 age- and sex-matched subjects from a nearby school in autonomic activity and reactivity between individuals with anxiety disorder and non-anxious control subjects. Our finding is suggestive of autonomic rigidity or diminished physiologic flexibility in children with anxiety disorder
CONCLUSIONS:
The study is probably the first of its kind to look into the issue in detail using a detailed battery of the autonomic function tests, and the results are of help in better understanding the condition. The result of the present experiment supports differences in autonomic activity and reactivity between individuals with anxiety disorder and non-anxious control subjects.
The aggregate anxiety disorders constitute the set of most prevalent psychiatric disorders in children and adolescents, with estimates of point prevalence ranging from 3% to 13%.1 Generalized anxiety disorder has been noted to be common in children and adolescents, with a prevalence of 3.6% to 7.3% in a community sample.1 Studies conducted in the USA and Europe, including Scandinavia, largely support the view that social phobia ranks among the most prevalent of the anxiety disorders in the general population.2 Estimates range from fairly low lifetime rates of 1% to 4% in studies conducted in the early 1980s to considerably higher estimates of 7% to 16% in later studies utilizing DSM-III-R criteria. Anxious children often present with physical complaints rather than overt worries or psychic anxiety. Anxiety is generally associated with a variety of somatic symptom patterns thought to reflect autonomic system activity. Traditionally, cardiovascular symptoms such as increased heart rate and palpitations have been the hallmark of anxiety.3 These physiological concomitants of anxiety could be of help in assessment and hence the management of childhood and adolescent anxiety disorders.
The symptoms can be difficult to assess and diagnose accurately. Frequently, the nonspecific presentation leads to extensive, intrusive and unnecessary workups. Relatively few studies have examined the autonomic characteristics of generalized anxiety disorder (GAD). One problem with the studies that have examined autonomic characteristics of anxiety has been their failure to address the well-documented complexity and specificity of autonomic nervous system (ANS) activity.
Even the broad distinction between the two categories of ANS—sympathetic nervous system (SNS) and parasympathetic nervous system (PNS), is often overlooked, as evidenced by the DSM-III R criteria of autonomic hyperactivity. As such, there has been a near-exclusive focus on sympathetic dysfunctions in ANS theories of panic susceptibility. By comparison, the potential role of the parasympathetic system has been overlooked. This characterization may reflect the tendency of past theoretical models to link global ANS disturbances to anxiety and the widespread usage in the literature of nonspecific construct such as “autonomic arousal” or “autonomic hyperactivity.” This omission is at odds with contemporary models of autonomic cardiovascular control, which emphasize the ongoing interplay of both sympathetic and parasympathetic (vagal) activities.
Young people can present with a pattern of anxiety symptoms that are somewhat different from those typically seen in adults. The most troublesome aspect of this difference is that children with anxiety disorders may not report any worries or anxieties, but may have pronounced physical symptoms. From the cardiovascular perspective, a sense of palpitations, tachycardia, increased blood pressure and flushing or pallor may be seen in cases of anxiety disorders. Young children with GAD may feel sick after a news report of a disaster.4 Our study aimed at finding the differences in the autonomic functions between a study group and a control group among children and adolescents and hence to find a correlation between clinical parameters and autonomic dysfunction.
METHODS
The study was carried out at the All India Institute of Medical Sciences (AIIMS), a top-level medical institute in the country. The subjects were recruited from the Child Guidance Clinic of the institute, and the assessments were carried out at the Autonomic Functions Laboratory in the Department of Physiology at the same institute. The sample consisted of two groups, which were drawn nonrandomly as a sample of convenience. The reason for employing this methodology was to ensure that the selected subjects were assessed properly and the assessors were not overburdened with the case load. This was based on the fact that a large number of cases are seen in the Child Guidance Clinic of the institute, which, being the primary institute, draws patients from all across the country. However, it was ensured that the assessor (author RS) would take up the first possible patient meeting the inclusion and exclusion criteria and providing valid informed consent. This ensured the absence of any possible selection bias in terms of factors such as gender, severity of condition, socio-demographic variables, or other factors. Moreover, attempts were made to adequately match the controls to the cases to have a comparable group. The study group was comprised of 34 subjects (children and adolescents) with a diagnosis of childhood anxiety disorder in the age range of 8 to 18 years. The control group consisted of 30 age- and sex-matched subjects recruited from a nearby primary school. The subjects with comorbid diagnosis of other psychiatric disorders, like bipolar disorder, conduct disorder, mental retardation, schizophrenia disorder, delusional disorder and any severe medical illness (organic brain disease and epilepsy), were excluded.
The assessments were carried out using a semistructured interview using K-SADS (Schedule for Affective Disorders and Schizophrenia for Children and Adolescents); STAIC (State and Trait Anxiety Inventory for Children); CDRS (Childhood Depression Rating Scales); and SCARED (Self-Report for Childhood Anxiety–Related Disorders), which assessed similarities or discrepancies, if any, in the reporting of symptoms between parents and respective children. The study was carried out in two sessions for the study group. Session I was an assessment of the study and control groups using the rating scales. After fulfilling the inclusion and exclusion criteria, a complete psychiatric and medical history was taken, and a mental status examination was performed on the subjects. This was followed by a general physical examination. After this, a diagnosis was reached using DSM-IV-TR. The findings, including the diagnosis, were discussed with the consultant psychiatrist. This was followed by completing a semistructured pro forma sheet. The semistructured pro forma sheet included details about education, birth and developmental history; family history; past history of psychiatric and medical illnesses; and psychosocial stressors.
The second session was an evaluation of the study group (comprising those who were assessed in Session I) for autonomic function. Before the test patients were advised to refrain from food, tea, coffee or any other beverages 2 hours prior to the test. The entire range of tests was carried out in an air-conditioned laboratory (22°C±2°C) in supine and sitting positions, between 9 AM and 4 PM. Autonomic reactivity tests included resting blood pressure (BP) and respiration. Resting BP was measured using a standard mercury sphygmomanometer, after the patient had rested for at least 15 minutes. The resting respiratory rate was also estimated during this period.
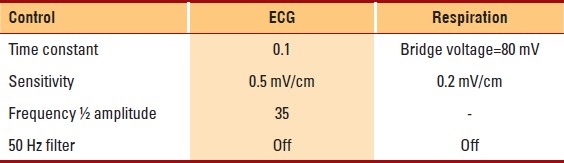
All the subjects underwent a battery of tests aimed at assessing their autonomic reactivity. The tests were performed with the patient seated comfortably, and continuous ECG and respiratory (stethograph) recordings were taken. Blood pressure was monitored (using a manometric cuff) at intervals throughout the procedure. Verbal directions were given to the patients, and they were under continuous supervision during the tests. ECG and respiratory tracings were obtained via a Polywrite (Recorders and Medicare, Chandigarh, India). The tests were carried out in the order mentioned below. Adequate time was given between two consecutive tests for the BP and heart rate to normalize before the next test was started. Table 1 lists the amplifier settings for the recording procedure.
Table 1.
Amplifier settings for recording ECG and respiration
In the lying-to-standing (LST) difference of BP test, the subjects were asked to rest in a supine position for 15 minutes. After rest, BP was recorded as basal BP. The subjects were instructed to stand up within about 3 seconds. BP was again recorded immediately on standing up and at 2 minutes thereafter. In the deep breathing test (DBT), the subjects were advised to inspire 6 breaths in 1 minute, comprised of 5 seconds of inspiration and 5 seconds of expiration. The average of the maximum RR intervals on the ECG during expiration divided by the average of the minimum RR intervals during inspiration gave the expiration:inspiration (E:I) ratio. The difference between the maximum and minimum heart rate gave the ΔHR. In very young children who were unable to follow the above procedure, the values were calculated from a single breath cycle. For the Valsalva maneuver (VM), the subjects were instructed to blow out into a mercury manometer (forced expiration from the chest) at a pressure of 40 mm Hg, in a closed system, for 15 seconds.
In the handgrip test (HGT), the subjects were directed to grip the handgrip dynamometer with their dominant hand and contract maximally. The maximum value of these readings was taken as the maximum voluntary contraction (MVC). The subjects were then asked to continually press the dynamometer at 30% of the MVC, up to 4 minutes. Blood pressure recordings were carried out before the start of the contraction and at 1st, 2nd and 4th minutes, in the contralateral arm. The resulting heart rate changes were monitored during the procedure via polygraph tracings. For the cold-pressor test (CPT), the subjects were directed to immerse their hand (up to the wrist) in water at 10°C for 1 minute. The blood pressure and heart rate were monitored before the procedure and at 1 minute, before retracting the hand from the cold water.
The ratio between maximum RR interval around the 30th beat to the minimum RR interval around the 15th beat is 30:15, when the patient stands up from lying posture. The DBT, VM and the (30: 15 ratio) heart rate changes due to LST provided a measure of the parasympathetic reactivity; while the HGT, CPT and the BP changes due to LST provided a measure of the sympathetic reactivity.
The equipment used for the study included Polywrite (manufactured by Recorders and Medicare Systems, India); handgrip dynamometer (Jetter and Scheerer, Germany); manometer locally assembled in the Autonomic Function Laboratory; standard mercury sphygmomanometer; strain gauge type of volume transducer (Model Vt. 159) (manufactured by INCO, India).
Data was analyzed using the SPSS-10 software (Chicago, IL, USA). Descriptive statistical measures were performed and compared group-wise for all of the variables, including the sociodemographic and clinical variables. The Nevrokard Heart rate reserve (HRV) analysis system, v 6.4, manufactured by Medistar, Slovenia; Biopac system MP150/ Acquknowledge 3.5; and MatLab v6.5 developed by MathWorks Inc., Japan, were used for analysis of the heart rate variability. In case of continuous variables, the t test for normal distribution was done. To compare the categorical variables, the chi-square test was done. To quantify the association between two variables, the Pearson correlation coefficient was used for normally distributed measures.
RESULTS
Of 76 children and adolescents who took part in the study, 39 had childhood anxiety disorders and 37 without anxiety disorders comprised the control group. Those with childhood anxiety disorders compared for their autonomic characteristics with 30 subjects of the control group, who were matched for age and sex with the subjects of the study group. There were no significant differences between the study and the control groups in terms of the sociodemographic profile (Table 2). The study group was comprised of 15 subjects with a rural background, while the control group all had an urban background. However, available epidemiological studies from India have reported comparable rates of psychiatric disorders among children and adolescents from both rural and urban settings.5 The psychiatric diagnoses of subjects in the study group included GAD, separation anxiety disorder (SAD) and social phobia (Table 3). The assessments by C-GAS, STAIC (state and trait anxiety), CDRS-R are shown in Tables 4 through Table 7. In the SCARED scale the mean (standard deviation) of the parent version was 25.53 (4.65) vs. 22.53 (4.65) for the child version as assessed in the study group, and the difference was statistically significant (P<.05).
Table 2.
Sociodemographic profile of the study and control groups
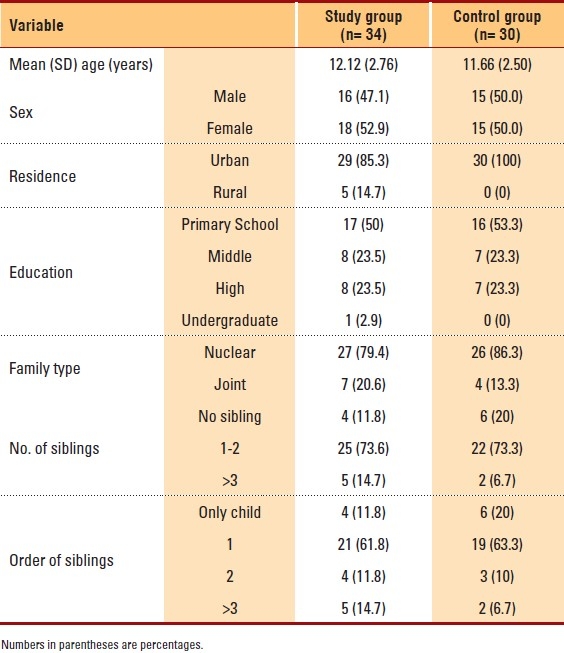
Table 3.
Diagnosis of anxiety disorder in the study subjects on the basis of gender
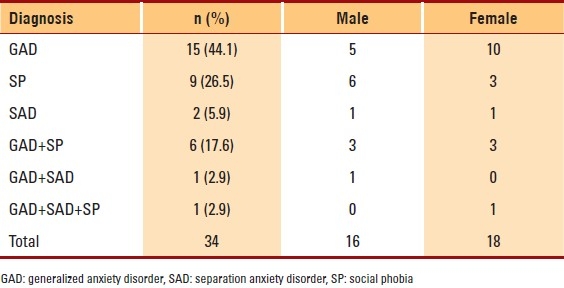
Table 4.
Comparison of the level of functioning between the 2 groups on C-GAS
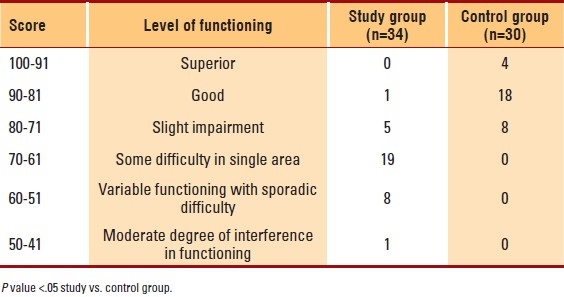
Table 7.
Comparative distribution of the likelihood of depression in subjects of the study group and control group on CDRS-R
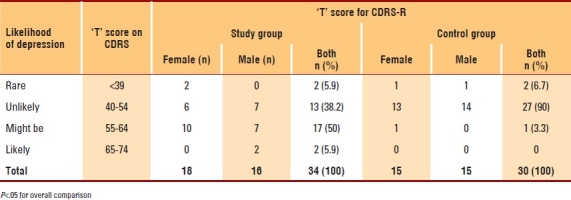
Table 5.
Comparative distribution of normalized ‘T’ scores of state anxiety on STAIC in subjects of study group and control group
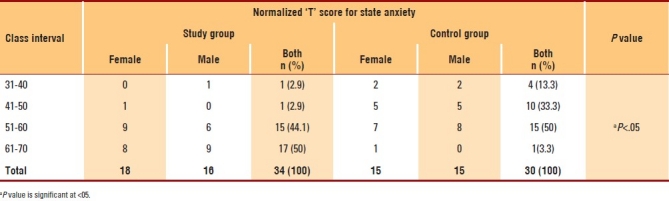
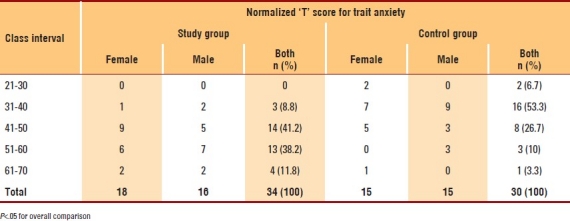
Table 6.
Comparative distribution of normalized ‘T’ scores of trait anxiety on STAIC in subjects of study group and control group
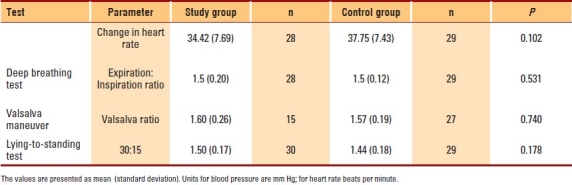
For comparisons of sympathetic activity (Table 8), in the handgrip test, the rise in diastolic blood pressure (DBP) was found to be statistically significant between the two groups. In lying-to-standing test, the fall in systolic blood pressure was more in the anxiety group, which was found to be statistically significant. In the cold-pressor test, the rise in diastolic blood pressure was statistically comparable between both the groups, though it was slightly higher in the control group. In all the tests for parasympathetic reactivity, the two groups were statistically comparable (Table 8). The delta heart rate in deep breathing test of the control group was higher than that of the anxiety group (Table 9). Two of the patients in the study group and one of the patients in the control group could not perform the tests. The E:I ratios of the two groups were almost similar. For this parameter also, the data is available for 28 children from the anxiety group and 29 children from the control group. The 30:15 ratios of the RR interval in the lying-to-standing test were also comparable in both the groups. The data is available for all the anxiety group children and 29 of the control group children. In Valsalva maneuver, values in both the groups were comparable.
Table 8.
Comparison of sympathetic reactivity in study and control groups
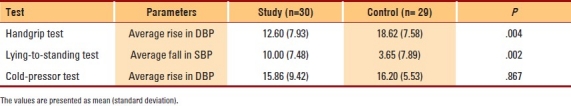
Table 9.
Comparison of parasympathetic reactivity between the study and control groups
DISCUSSION
Anxiety disorders in youth are receiving increasing attention. Such attention is understandable considering that it has been estimated that between 10% and 20% of youngsters display anxiety and anxiety-related symptoms. Anxiety disorder constitutes the set of most prevalent psychiatric disorders in children and adolescents. This can affect the developmental process and school performance and result in strained relationship with peers and family members. This study is probably the first one to aim at exploring the clinical characteristics of childhood anxiety disorders attended to in a tertiary-care hospital.
Anxiety is often accompanied by somatic manifestations that suggest morbid changes in autonomic nervous system (ANS) activity, such as rapid heart rate (HR), shortness of breath and sweating. Autonomic characteristics of depression and panic disorder have been studied extensively;5 however, relatively few studies have examined the autonomic characteristics of anxiety disorder, especially in children and adolescents. Exploration of the autonomic characteristics of children diagnosed with anxiety disorders compared with healthy age- and sex-matched controls would also help determine whether any correlation exists between the autonomic profile and the clinical anxiety status of affected subjects vis-à-vis healthy controls.
Thirty-four children and adolescents (age range, 8-18 years) diagnosed with anxiety disorders were enrolled for the study and assessed, and they constituted the study group. The majority of the subjects in the study group had 1 to 2 siblings (25 subjects, 73.6%) and 21 subjects (61.8%) were the oldest in the family. The majority of the patients (85.3%) were from an urban setting, which may be due to the fact that the study was conducted in an urban setting. Another reason might be that patients in the urban setting have more awareness about, and accessibility to, treatment centers and thus seek treatment.
In terms of a single psychiatric diagnosis, GAD was the most common diagnosis (15 subjects, 44.1%), followed by SP (9 subjects, 26.5%) and SAD (2 subjects, 5.9%). In the present study, the gender differences in prevalence of a sole diagnosis of GAD were not significant. This is similar to the finding from a previous clinic-based study, where no significant differences were noted with regard to gender.6 The differences were statistically significant between the two groups (P< .05) on the scores of K-SADS (Schedule for Affective Disorders and Schizophrenia) and C-GAS (Children's Global Assessment Scale). These differences highlight the dysfunction and disability that are caused by psychiatric disorders in the study subjects.
The assessments using the STAIC to study the differences between the study group and control group on state and trait anxiety measures show that the differences were statistically significant. This would be expected since the study group comprised subjects with a diagnosis of anxiety disorder, which would therefore result in higher ratings on the STAIC in study subjects compared to controls. The assessments using the CDRS to study the differences between the study group and control group on the likelihood of depression show that the differences were statistically significant. As discussed earlier, depression was reported to be present in 9 (26.5%) subjects of the study group, using the K-SADS. There was a high level of concordance between depression scores on K-SADS and CDRS. This significant difference was expected since the study group comprised subjects with a diagnosis of depressive disorder, which would therefore result in higher ratings on the CDRS in study subjects compared to controls.
The mean score for subjects' reporting of anxiety compared to parents' reporting of anxiety implied low concordance between the parents' reporting of anxiety and the subjects′ self-reporting. Such a finding has been noted in a previous study.7 The reason for this disparity in the reporting may be that children report a fewer number of cognitive symptoms and show more of internalizing phenomenon, thus not communicating their problems to their parents.
Anxiety is generally associated with a variety of somatic symptom patterns thought to reflect autonomic nervous system activity. Relatively few studies have examined the autonomic characteristics of GAD. Only one review has commented on SP, mentioning that the patients have sympathetic arousal even when they are not exposed to the phobic situation.8 Despite extensive literature search, no study reporting the autonomic characteristics of separation anxiety disorder could be found.
To the best of our knowledge, this is the first study in children and adolescents in which a complete battery of autonomic functions tests was employed. The result of the present experiment supports differences in substantial autonomic activity and reactivity between individuals meeting DSM-IV-TR criteria for anxiety disorder and non-anxious control subjects, as described below. The study group was characterized by statistically significant findings in the form of decreased sympathetic reactivity, sympathetic activity and parasympathetic activity when compared to the control group. However, no change in parasympathetic reactivity was observed between the two groups.
There were significant differences (P=.004) in sympathetic reactivity as measured by the handgrip test. The rise in diastolic blood pressure (DBP) was less in the handgrip test in the study group in comparison to the control group. The sympathetic reactivity as measured by the lying-to-standing test showed that the fall in systolic blood pressure (SBP) was more in the study group in comparison to the control group and this difference was clinically significant (P= .002).
In the current study, there were no significant differences in the parasympathetic reactivity between the control and anxiety groups, thus implying that in the study group, comprising anxiety disorder patients, parasympathetic reactivity (heart rate response to given perturbation) essentially remained within normal range. This was similar to the finding of a previous study, which also reported no difference in vagal tone (parasympathetic reactivity) in adults with GAD, with mean (SD) age of 32.2 (SD±6.7) years; compared to controls, with mean (SD) age of 29.7 (SD±4.6) years.9
The sympathetic inhibition found in the current study group was similar to that found in a previous study (Saric et al., 2004) on GAD patients in the adult population (36 years [range, 19-55]). The study assessed skin conductance and inter-beat intervals in 40 GAD patients and compared these findings with those of 20 controls. Our finding is suggestive of autonomic rigidity or diminished physiologic flexibility in anxiety disorder children. This loss of variability in autonomic control system in general has recently been linked with a number of diseases and dysfunctions, among which anxiety disorder can be included.
There was no correlation between state and trait anxiety scores on STAIC scale and the autonomic function parameters. Similarly there was no correlation between depression rating scores on Childhood Depression Rating Scale — Revised (CDRS-R) and autonomic parameters. No correlation between child-reporting scores and parent-reporting scores on SCARED (Self-Report for Childhood Anxiety–Related Disorders) and autonomic parameters. Thus there was no correlation at all between the clinical profile and the autonomic function parameters.
Previous studies have also noted a discrepancy between the clinical profile measuring the psychological perception and the physiological changes as measured by autonomic function tests. To explain this counterintuitive set of results, three hypotheses, namely, the Variability Hypothesis, the Expectation Hypothesis and the Attention Hypothesis, have been proposed. Another explanation could also be that strong emotional experiences that initially trigger autonomic responses subsequently elicit similar somatic sensations, even in the absence of physiological responses. However, a study by Watkins et al in 1998 on adults with anxiety found an association between trait anxiety score and vagal control of the heart in terms of parasympathetic activity.10 In this study, stepwise increase in trait anxiety scores was associated with reduced vagal control of the heart. In the present study, the negative results may also be attributed to the low power of the study.
Clinical implications
Anxiety disorders during childhood and adolescence are associated with significant morbidity. They not only affect the development of patients in the developmental stages of their life but also have a bearing on the future occurrence of the psychiatric morbidity. These disorders need to be studied in greater detail, including the assessment of the associated physiological changes. The study is probably the first of its kind to look into the issue in detail using a detailed battery of the autonomic function tests, and the results are of help in better understanding of the condition. The study provides information on the status of autonomic functions, governed by both the sympathetic and the parasympathetic systems, in childhood anxiety disorders. The role of the parasympathetic system in these disorders has not been explored, which would be of help in understanding this rather under-researched area. The result of the present experiment supports differences in substantial autonomic activity and reactivity between individuals meeting DSM-IV-TR criteria for anxiety disorder and non-anxious control subjects. This loss of variability in autonomic control system has been linked with a number of diseases and dysfunctions. Since the current study suggests similar results, it would be of great importance to include childhood anxiety disorders in the list of these diseases and dysfunctions. This would alert the clinicians to be vigilant for the same in their patients and thus take necessary interventional steps to avoid, or lower the intensity of, the possible adverse outcomes.
Limitations
The study used a sample of convenience for logistical reasons, as explained earlier. This would mean that certain cases would have been missed in between. Moreover, this is unlikely to have an adverse impact on the findings since an adequately matched control group was chosen and the assessor chose the first suitable subject meeting the study criteria on every clinic day. This prevented the possibility of the selection being biased by the severity of disorder or other potential confounders. There is also a need of following up these individuals and then subjecting them to the battery of tests once the clinical symptoms remit, to observe the impact of the therapeutic interventions. This could not be achieved in the current study due to time constraints.
However, taking a sample of convenience results in not only selection bias, but also ascertainment bias causing distortion in the found results and hence can affect the reliability of the obtained results.
Author contributions
Rajiv Sharma had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Rajesh Sagar was involved in conceptualisation of the study, study design, review of manuscript. KK Deepak was involved in conceptualisation of the study, study design, review of manuscript. Manju Mehta was involved in conceptualisation of the study, study design, review of manuscript. Yatan Pal Singh Balhara was involved in preparation of manuscript, review of literature and editing.
REFERENCES
- 1.Kashani JH, Orvaschel H. Anxiety disorders in Mid-Adolescence: A community sample. Am J Psychaitry. 1998;145:960–4. doi: 10.1176/ajp.145.8.960. [DOI] [PubMed] [Google Scholar]
- 2.Furmark T. Social phobia: Overview of community surveys. Acta Psychiatr Scand. 2002;105:84–93. doi: 10.1034/j.1600-0447.2002.1r103.x. [DOI] [PubMed] [Google Scholar]
- 3.Thayer JF, Friedman BH, Borkovec TD. Autonomic characteristics of generalized anxiety disorder and worry. Biol Psychiatry. 1996;39:255–66. doi: 10.1016/0006-3223(95)00136-0. [DOI] [PubMed] [Google Scholar]
- 4.Varley CK, Smith CJ. Anxiety disorders in the child and teen. Pediatr Clin N Am. 2003;50:1107–38. doi: 10.1016/s0031-3955(03)00070-1. [DOI] [PubMed] [Google Scholar]
- 5.Srinath S, Girimaji SC, Gururaj G, Seshadri S, Subbakrishna DK, Bhola P, et al. Epidemiological study of child and adolescent psychiatric disorders in urban and rural areas of Bangalore, India. Indian J Med Res. 2005;122:67–79. [PubMed] [Google Scholar]
- 6.Friedman BH, Thayer JF, Borkovec TD, Cheek M, Muth ER, Tyrrell RA, et al. Heart rate variability in generalized anxiety disorders. SPR Abstracts. 1993 [Google Scholar]
- 7.Treadwell KR, Kendall PC. Self-talk in youth with anxiety disorders: States of mind, content specificity, and treatment outcome. J Consult Clin Psychol. 1996;64:941–50. doi: 10.1037//0022-006x.64.5.941. [DOI] [PubMed] [Google Scholar]
- 8.Kendall PC, Pimentel SS. On the physiological symptom constellation in youth with generalized anxiety disorder (GAD) J Anxiety Disord. 2003;17:211–21. doi: 10.1016/s0887-6185(02)00196-2. [DOI] [PubMed] [Google Scholar]
- 9.Hoehn-Saric R, Masek BJ. Effects of naloxone on normals and chronically anxious patients. Biol Psychiatry. 1981;16:1041–50. [PubMed] [Google Scholar]
- 10.Watkins LL, Grossman P, Krishnan R, Sherwood A. Anxiety and vagal control of heart rate. Psychosom Med. 1998;60:498–502. doi: 10.1097/00006842-199807000-00018. [DOI] [PubMed] [Google Scholar]


